-
Buzz
- Like sarcoid
- lymphatics and lymph nodes
- primary and secondary behave same way
- different
- age
- location
- Like sarcoid

Ashley Davidoff MD TheCommonVein.net lungs-0752
TB of the lung is an infection caused by mycobacterium TB with two phases – an activation phase and a reactivation phase adenopathy a
Inhaled droplets of Mycobacterium
- Immediate clearance of the organism
- Primary disease: immediate onset of active disease
- Latent infection
-

Position of Disease
Upper and mid lung field distribution
Ashley Davidoff MD TheCommonvein.net lungs-0772 - Reactivation disease: onset of active disease many years following a period of latent infection
- Consolidation
- Cavitation
- Miliary
key Dx feature upper or Rt middle lobe involvement initial exudative phase, vol loss instead of exp hypersensitivity rxn causes chronic inflam phase caseation necrosis after 6 wks
Radiology
Primary tuberculosis demonstrates
lymphadenopathy,
consolidation, (CAVITATION UNCOMMON)
pleural effusion, and
miliary nodules
middle lobes
upper portion of lower lobes or lower portion of upper lobes
Ghon lesion, sometimes called Ghon focus,
initial tuberculous granuloma formed during primary infection and is not radiologically visible unless it calcifies – this occurs
represents a tuberculous caseating granuloma (tuberculoma) and represents the sequelae of primary pulmonary tuberculosis infection.
Ghon complex.
is a Ghon focus alongside ipsilateral mediastinal lymphadenopathy
Ranke complex
is calcified Ghon complex (Ghon lesion and ipsilateral lymph node) representing a progression of the Ghon complex
radiologically detectable
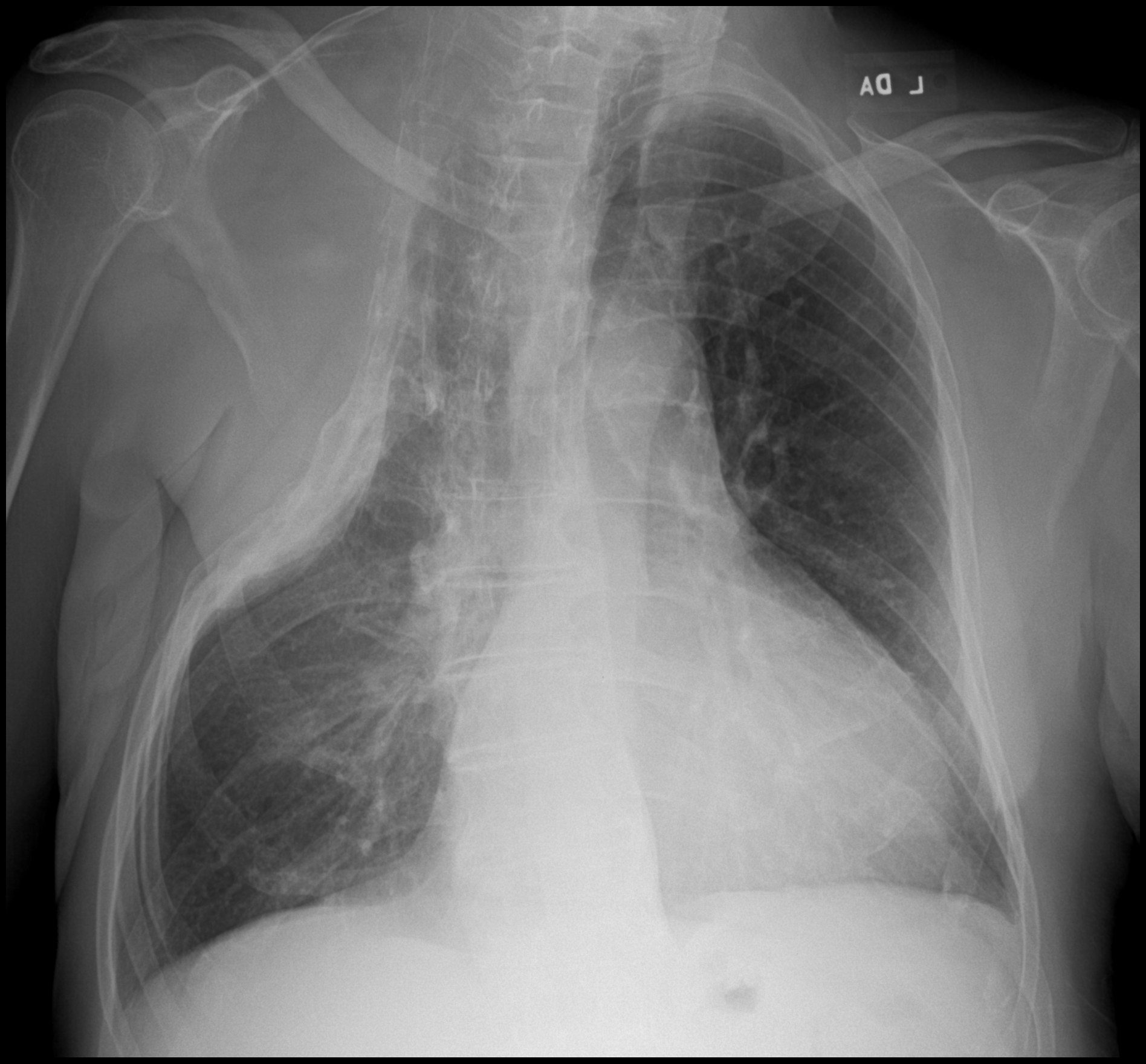
- 30 year old Female with Positive Sputum
- multiple tree-in-bud opacities and nodules
- measuring up to 8 mm in
- peribronchial vascular distribution in the
- left upper lobe the,
- lingula,
- left lower lobe,
- withslight surrounding groundglass.
- several bilateral calcified granulomas.
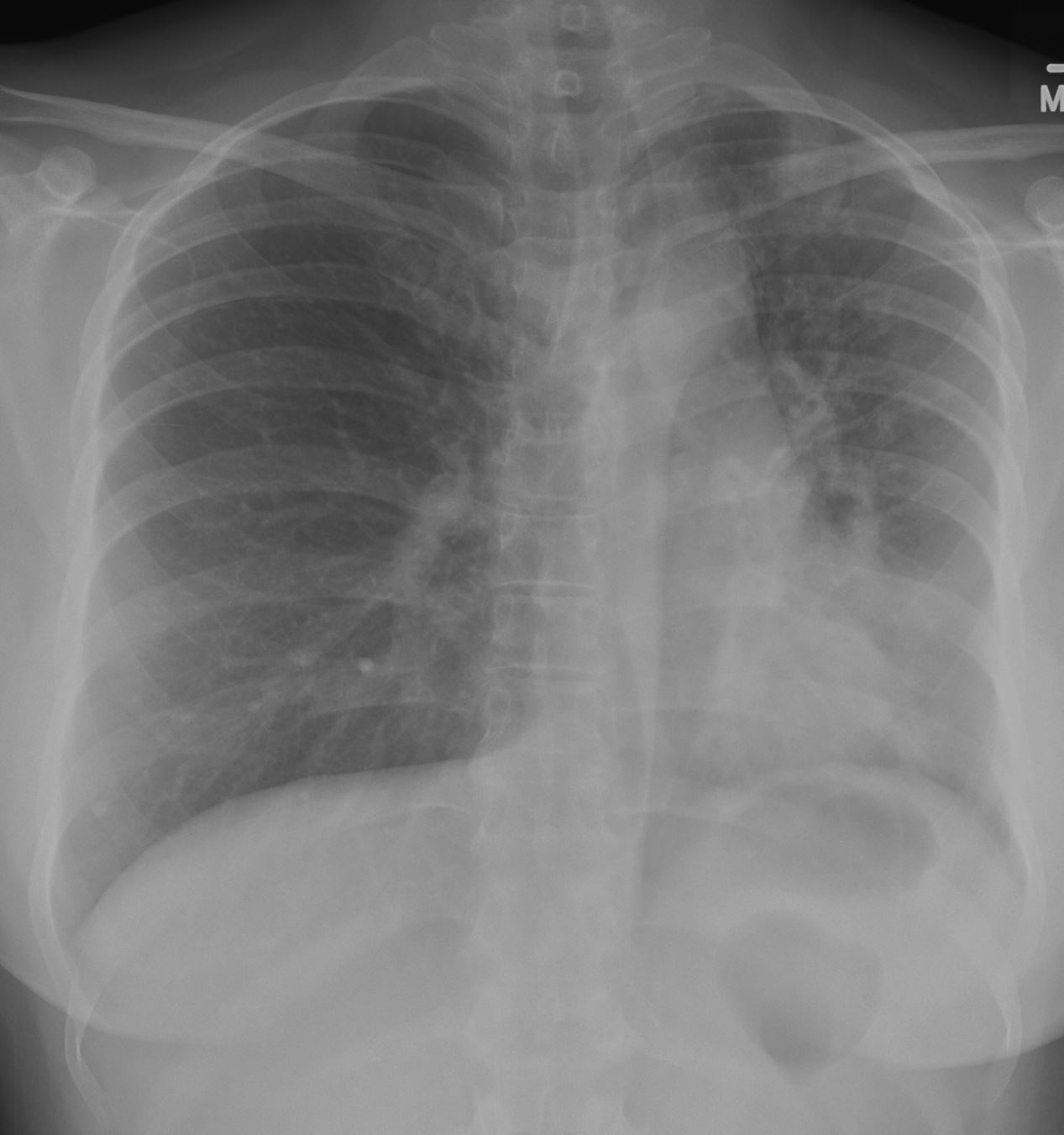
- CXR showed
-
Acute on Latent TB 46 f with positive sputum LUL nodules tree in bud and GGO on CT
CXR shows volume loss with tracheal shift mild elevation of the left hemidiapgragm left lower lobe, lingular and less obvious left upper lobe infiltrate and granulomas right base
Ashley Davidoff MD TheCommonVein.net
Acute on Latent TB 46f with positive sputum LUL nodules tree in bud and GGO on CT Lateral CXR shows mild elevation of the left hemidiapgragm subsegmental left lower lobe, lingular and lreticulonodular changes in the anterior segment of the LUL and lingula
Ashley Davidoff MD TheCommonVein.net3 Months Later on Treatment
-
46-f-acute-on-latent-TB-LUL-nodules-GGO-LL-infiltrate-volume-loss-granulomas-right-base-CXR-003-4mths-later-post-RX-hilum-retracted.jpg
Acute on Latent TB following 3 months treatment
CXR is significantly improved with resolution of infiltrates in the left lower lobe and lingula and with retraction of the left hilum and crowding of the markings in the LUL . There is persistent volume loss with elevation of the left hemidiaphragm and rightward deviation of the trachea . Granulomas noted atthe right base Ashley Davidoff MD TheCommonVein.net
Acute on Latent TB following 3 months treatment
CXR significantly improved with resolution of infiltrates in the left lower lobe and lingula
Ashley Davidoff MD TheCommonVein.net
-
- multiple tree-in-bud opacities and nodules
CT showed
Postprimary tuberculosis
(aka – reactivation TB and secondary TB)
consolidations that are predominant in the apical and upper lung zones,
nodules, and
cavitation
-
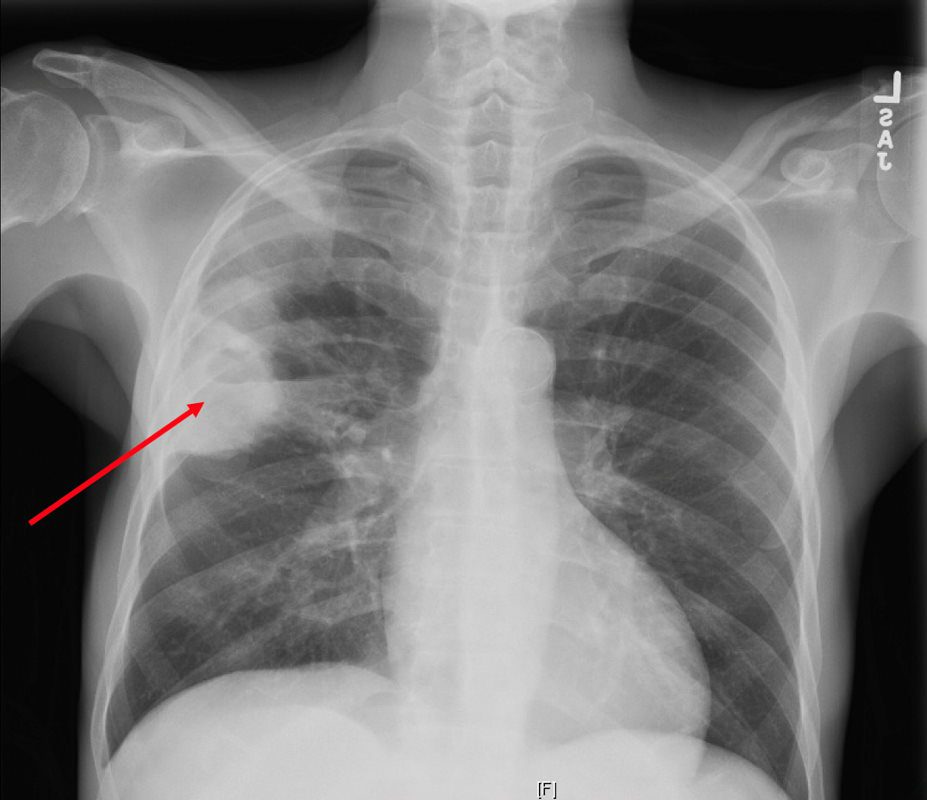
Reactivation TB
CXR reveals a dense consolidation in the right upper lobe (red arrow) with questionable air-fluid level. No pneumothorax. No pleural effusions. Differential includes right upper lobe pneumonia or tuberculosis. CT is recommended for further evaluation if there is concern for a cavity.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
CTPA reveals a large consolidation in the right upper lobe and superior segment of the right lower lobe spans approximately 8.8 x 5.6 x 9.4 cm and extends to the pleura. There are multiple internal cavitations (red arrows) with air-fluid levels. These large predominately right upper lobe cavitary lesions are consistent with clinical concern for tuberculosis pneumonia, however follow-up with chest CT in 3 months post-treatment is recommended to exclude other less likely causes of cavitary lesions, such as malignancy.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
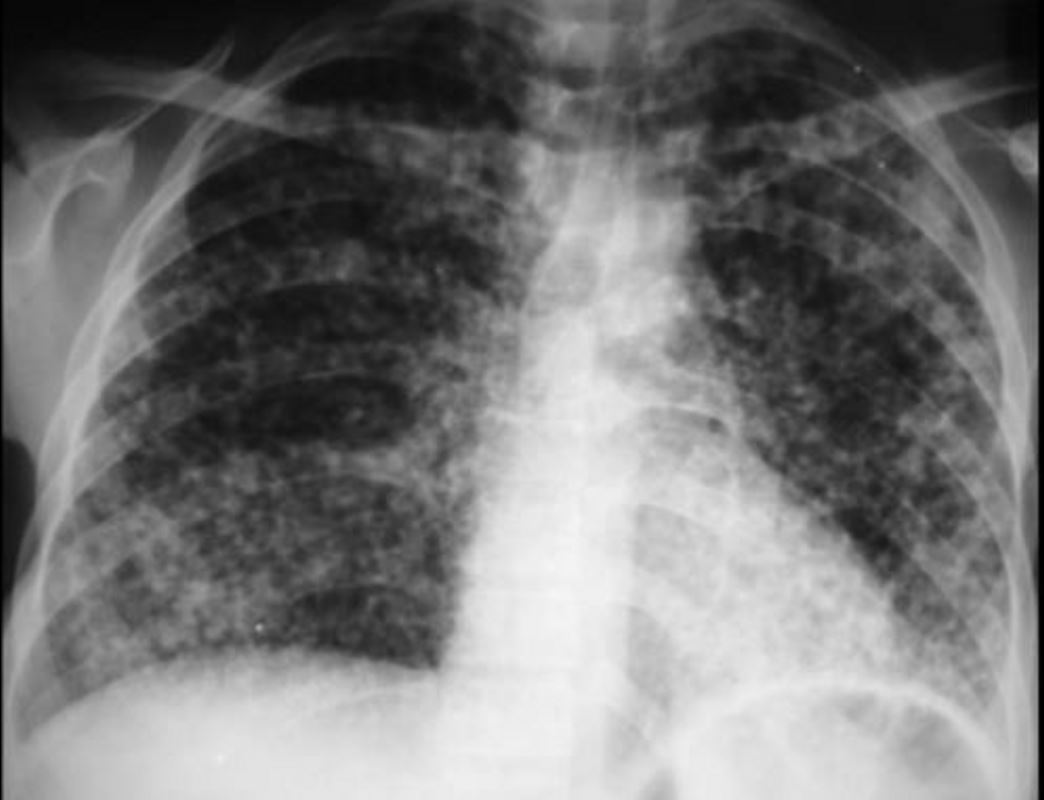
Miliary TB
CTPA reveals innumerable punctate nodules in a randomly distribution (red arrows). There are areas of groundglass opacity predominantly in a central peribronchial vascular distribution in both lungs. No pneumothorax. Differential of innumerable punctate nodules is consistent with miliary TB.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
CT reveals bulky conglomerate lymphadenopathy with central hypodensity (red arrow) in right levels IV, VI, supraclavicular region and partially visualized within the upper mediastinum. Differential includes infection, such as mycobacterial, or malignancy.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS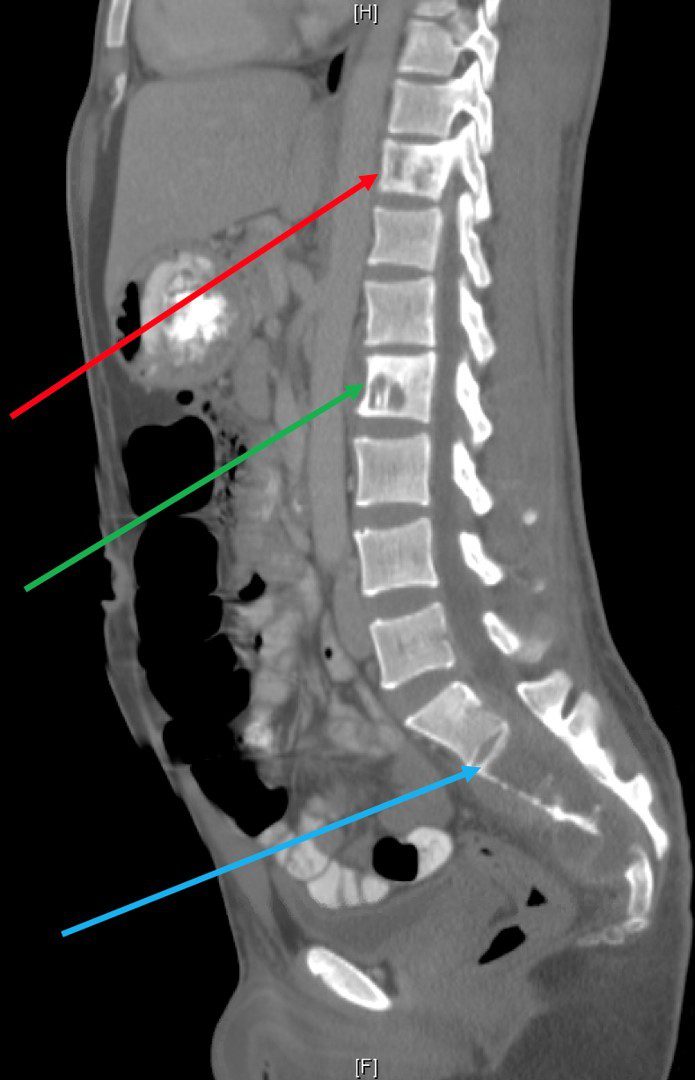
CT ?CAP in the sagittal projection shows extensive lytic lesions of the T11 (red arrow) and L2 (green arrow) vertebral bodies. In addition, there is an extensive lytic lesion from S2 inferiorly (blue arrow) with an associated soft tissue mass. There are no additional lesions in the thoracic or lumbar spine. These findings may represent metastatic disease, or possibly an infectious etiology such as tuberculosis.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MSActive TB
-
- as primary tuberculosis, developing shortly after infection,
- or postprimary tuberculosis
- Stability of radiographic findings for 6 months distinguishes inactive from active disease
- Primary Active
-
-
- lymphadenopathy,
- consolidation,
- pleural effusion, and
- miliary nodules
-
-
- Reactivation
- consolidations that are predominant in the apical and upper lung zones,
- nodules
- tree in bud
- cavitation
-
Primary Active and Reactivation
miliary tuberculosis is evenly distributed throughout both lungs
Courtesy https://www.slideshare.net/
82 year old man s/pthoracoplasty for treatment of right upper lobe TB. Associated finding is left ventricular enlargement
Ashley Davidoff MD
References and Links
- Radiographics
- Nachiappan, A.C et al Pulmonary Tuberculosis: Role of Radiology in Diagnosis and Management RadioGraphicsVol. 37, No. 1 2017
- Rossi, SE et al Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview RadioGraphicsVol. 25, No. 3 2005
-
Bhalla, A S et al Chest tuberculosis: Radiological review and imaging recommendation Indian J Radiol Imaging. 2015 Jul-Sep; 25(3): 213?225.
- Radiopaedia
-
TCV
