The word pancreas derives from the Greek words “pan” meaning “all “and “kreas” meaning “meat “ since it was thought to be made of muscle. It is however not a muscle but an elongated glandular structure that is soft and fleshy, and is situated in the retroperitoneum behind the stomach and the duodenum. It secretes pancreatic enzymes into the duodenum which aid in the digestion of fat and proteins, and it is a key player in the control of glucose metabolism which it accomplishes by secreting insulin into the circulation. It thus functions
as both an as an exocrine gland (secretes into ducts) and an endocrine gland (secretes into the circulation).The pancreas was known as the “hermit of the abdomen” since it was considered for many years a mysterious and lonely figure that lay deep in the abdomen. Over the years, knowledge of the function of the pancreas evolved, but it is only in recent years with the advent of and advances in angiography, ultrasound, CT and MRI that it’s in vivo structure has become understood. It is well connected to many organs, and is central to many functions and structures. Together with the“all meat” misnomer its status as “ hermit of the abdomen” are mere historic curiosities at this time.
In this section we present a perspective of the gland by exploring the principles that govern the gland hoping to give a perspective of its common structural and functional features. We explore the variety of classifications of the gland which gives us a perspective of where it lies in respect to the other structures. The historical perspective, gives us a sense of the evolution of our knowledge base, lest we take that for granted. We conclude with some general comments oclassifications advance the knowledge of structure and function, the basics structure and function of the anatomy and we add to that an overview of the gland at large including the physiology histology, diagnostic arts and therapy.
The Pancreas |
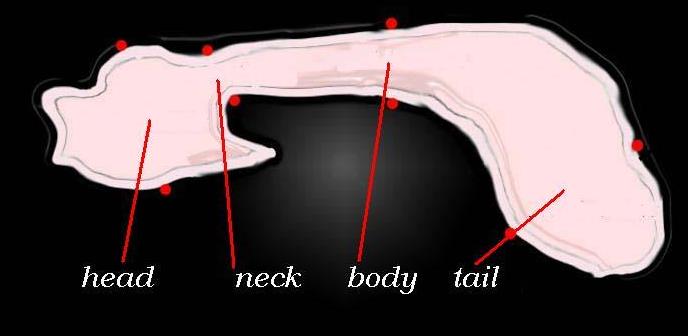
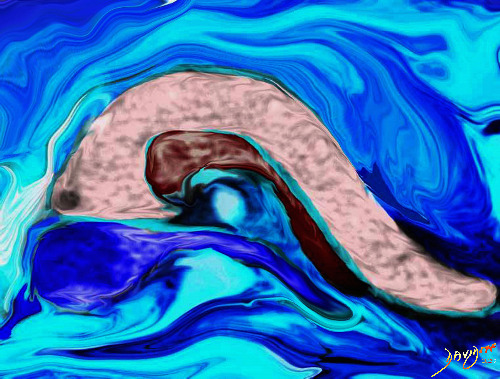
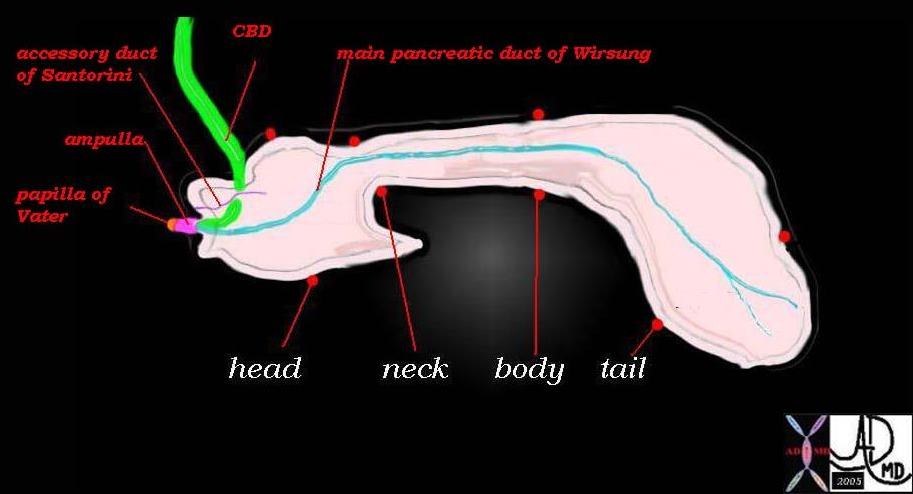
| This drawing reveals the major anatomic components of the pancreas, including the head, neck, body and tail, the ductal system (main duct of Wirsung, accessory duct of Santorini) the confluence of the bile duct and the pancreatic duct in the ampulla, and finally the papilla which is the common entrance of the main duct and the bile duct in the duodenum.
Courtesy Ashley Davidoff 41394size002b09 |
Principles
As a Gland
Since the pancreas is a gland it is, like all glands, composed of epithelial cells that are specialised to synthesise and secrete active substances that contribute to funcionality in the body. It has both the endocrine type of gland that secretes insulin and glucagon into the blood and an exocrine portion that secretes digestive proenzymes (zymogens) into the ducts.
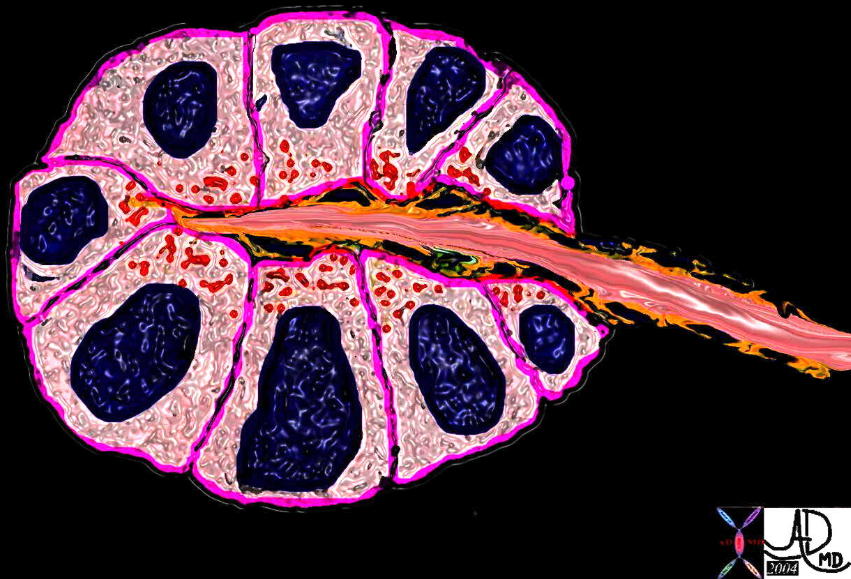 The pancreas consists of two types of glands. The exocrine type is demonstrtaed above consisting of an epithelium in the form of a rosette that secretes functional material into a duct. The rosette of gland is rounded in 3D in the form of an acinus. 39939b04 Courtesy Ashley Davidoff MD
The pancreas consists of two types of glands. The exocrine type is demonstrtaed above consisting of an epithelium in the form of a rosette that secretes functional material into a duct. The rosette of gland is rounded in 3D in the form of an acinus. 39939b04 Courtesy Ashley Davidoff MD
As an endocrine gland, the pancreas is endowed with a rich blood supply since it has to secrete the hormones it produces into the circulation in order for the hormones to have a rapid effect. The islets of Langerhans secrete insulin into the blood stream, very soon after ingestion of a meal in order to control blood sugar and intracellular glucose concentrations. The endocrine cells called the islets of Langerhans represent only 1-2% of the tissue volume of the pancreas, but play a vital role in body function and well being. They are most numerous in the tail of the pancreas.
As a serous exocrine gland, the pancreas has to have an accompanying ductal system. The epithelial cells secrete a fluid containg the enzymes into the pancreatic duct which is a tube and as such, is subject to the the laws that govern flow in a tube. Some of the factors that need consideration relating to flow include the radius of the tube, the pressure differences between the upstream side and the downstream side of the tube, viscocity of the medium that is being transported and the friction that occurs between the fluid being transported and the lining of the tube. The pancreatic fluid has a relatively low viscocity, and is rich in sodium and bicarbonates. The bicarbonates neutralise the acid in the gastric juices that enter the small bowel as chyle in order to optimise the PH for enzyme function. About one litre of fluid is produced and transported per day.
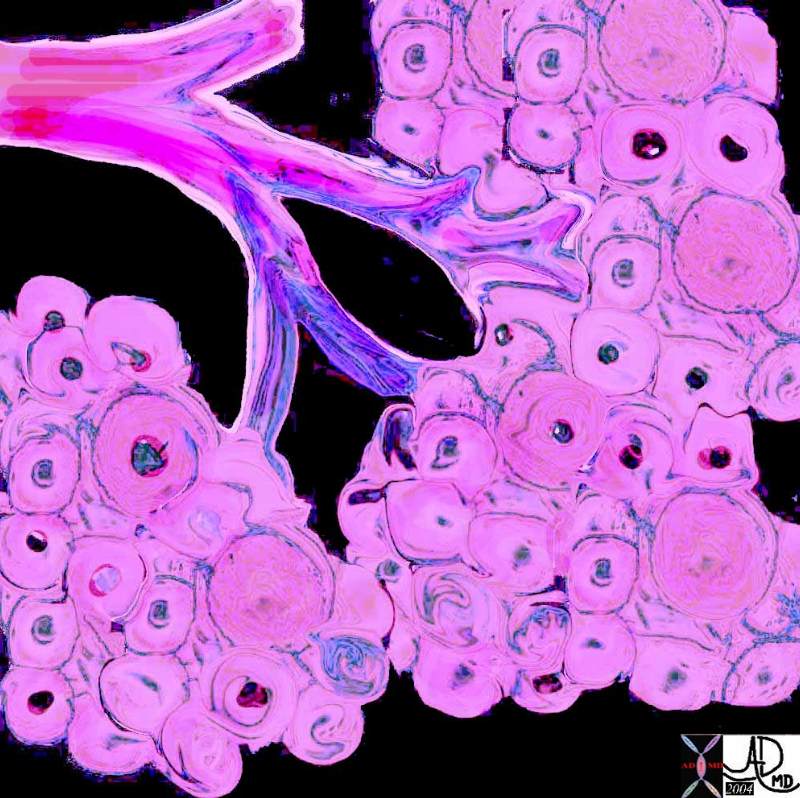 The pancreas has an exocrine and endocrine component. The exocrine compnent is demonstrated above in 3D with acini in “cluster of grapes” formation subtended by a duct. Courtesy Ashley Davidoff MD 32645a06
The pancreas has an exocrine and endocrine component. The exocrine compnent is demonstrated above in 3D with acini in “cluster of grapes” formation subtended by a duct. Courtesy Ashley Davidoff MD 32645a06
As an endocrine gland the pancreas secretes its hormones directly into the blood stream with almost immediate effect on the body. For this aspect to function optimally there has to be a rich blood supply to and from the gland. The pancreas has an exteremely rich blood supply supplied by both the celiac axis and the SMA.
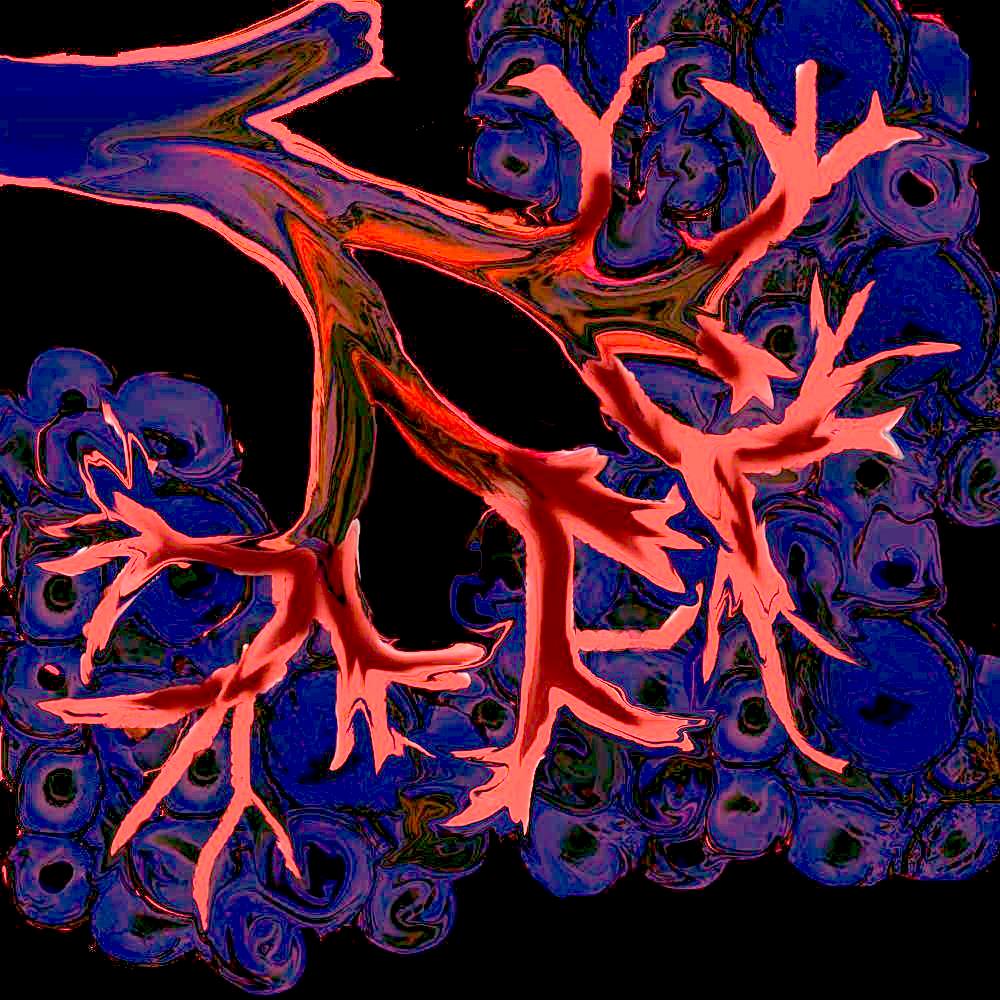
 This 3D rendition of an endocrine gland shows an example of the structure of endocrine the acini of the islets of Langerhans surrounded by a rich network of blood vessels into which the hormones will be secreted. Courtesy Ashley Davidoff MD 32164b02
This 3D rendition of an endocrine gland shows an example of the structure of endocrine the acini of the islets of Langerhans surrounded by a rich network of blood vessels into which the hormones will be secreted. Courtesy Ashley Davidoff MD 32164b02
In diseases such as cystic fibrosis the fluid being transported is significantly thickened and forms inspissated concretions that not only are slow to move but may eventually be unmovable, limiting upstream flow and causing obstruction. In diseases where the tube is damaged and narrowed such as in carcinoma of the pancreas, or pancreatitis, the resulting stricture will inhibit flow and the upstream part will be dilated and the downstream portion decompressed.
PRINCIPLES
As a tubular structure
The pancreas consists of a system of glands and their subtending tubes. At the terminal end of the tube is an epithelial layer anatomically designed in clusters of grape formation to increase the surface area available for rapid and efficient production and transport of enzymes and serous fluid.
Tubular systems are universal throughout the body. The arterial, venous, lymphatic, ductal, gastrointestinal, and genitourinary systems are classical examples.
Flow will only occur when a pressure difference exists between the two sides of the tubes. The velocity of flow relates to diameter, resistance, friction, and pressure. Velocity of flow will also depend on whether the flow is laminar or turbulent, and whether the fluid medium being transported is thick or thin. Frictional considerations between the fluid medium and the lining are essential to velocity of flow. In the small bowel for example the contents are relatively thick and the surface of the lining is thrown into folds. This combination is designed for slow flow, and optimises the duration of contact of the fluid with the surface lining. In the arterial system on the other hand, velocity of flow and speed of delivery is essential. Although blood is relatively viscous (for example compared to the serous secretions of the pancreas for example) the endothelium is smooth and thus friction is limited and flow therefore as rapid as is necessary.
When flow is laminar, it will be governed by Poiseuille’s law which states that laminar flow is directly proportional to the driving pressure. Thus if the driving pressure is doubled, the flow rate will be doubled, as long as the the radius remains constant. The radius of the tube, however, is very important and relates to the velocity to the 4th power. Hence if the radius of a tube is increased by 2cms, the velocity will increase by a factor of 16, as long as all the factors remain constant including the presence of laminar flow. As velocity increases, however, the flow tends to become turbulent. Flow tends to be laminar when the tubes are small and turbulent when the tubes are large or when there are irregularities in the walls.
 This diagram illustrates the tubular and branching pattern of a ductal system that extends from the secondary duct into the terminal ductules. Courtesy Ashley Davidoff MD 32645b04b04
This diagram illustrates the tubular and branching pattern of a ductal system that extends from the secondary duct into the terminal ductules. Courtesy Ashley Davidoff MD 32645b04b04
Thus flow in the pancreatic duct tends to be laminar and relatively slow compared to the circulation and controlled by the needs of digestion and the outlet valve at the ampulla.
Resistance of flow in most systems in the body depends on sympathetic tone of the smooth muscle. In health this tone is well balanced with the needs of the person. However, if the tone is patholically increased then flow becomes aberrant .
The pancreatic system is beautifully designed to enable rapid and efficient delivery of pancreatic enzymes in response to a reflex that identifies fat protein or carbohydrates in the stomach. Tactile stimuli, chemical stimuli, and autonomic nervous stimuli excite the glands to produce the serous fluid with appropriate enzymes.
APPLICATIONS TO DISEASES
When there is malignant transformation of the cells in the pancreas, the liklihood of developing an adenocarrcinoma originating in the exocrine portion is much higher than from the endocrine portion since the exocrine portion is so dominant by shher volume. As stated, 98% of the cellular volume of the pancreas is exocrine and only 2% endocrine.
Adenocarcinoma of the pancreas shows characteristic desmoplastic response. This fibrotic response results in encasement of ducts arteries veins and lymphatics.
APPLICATION TO IMAGING
One of the main distinguishing features that separates endocrine tumors from exocrine tumors of the pancreas on CT, MRI or angiography, is tumor vascularity. Since the endocrine system is so intimately related to the vascular system, it is not surprising that these tumors are hypervascular. They also tend to be larger when identified because their re;lative lack of scirrhous reaction. Additionally since the islets are more promoinent in the tail of the pancreas, the tumors tend to be more common in the tail.
The exocrine tumors on the other hand, are hyporvascular lesions showing characteristic scirrhous reaction. Encasement around bile duct, pancreatic duct, arteries, veins and nerves is not uncommon.

In this ERCP the main pancreatic duct and the secondary branches are dilated due to an outflow tract obstruction. A dialted duct is not an uncommon finding and usually indictates an obstruction from pancreatitis or from carcinoma. 05008 Courtesy Ashley Davidoff MD
CLASSIFICATION
Structural Considerations:
The pancreas is part of the gastrointestinal system and is considered a major accessory gland of the gastrointestinal system.
It is of course part of the endocrine system as well. At a macroscopic level it has a head, neck, body and tail.
At an anatomic level the main components are the head with uncinate process, the neck which is a small section, the body and the tail. 41394size002b03 Courtesy Ashley Davidoff MD
At a histological level excocrine performing cells are considered as a compound tubuloalveolar gland with serous secretion. Structurally, the exocrine pancreas is classified as a compound serous acinar gland.
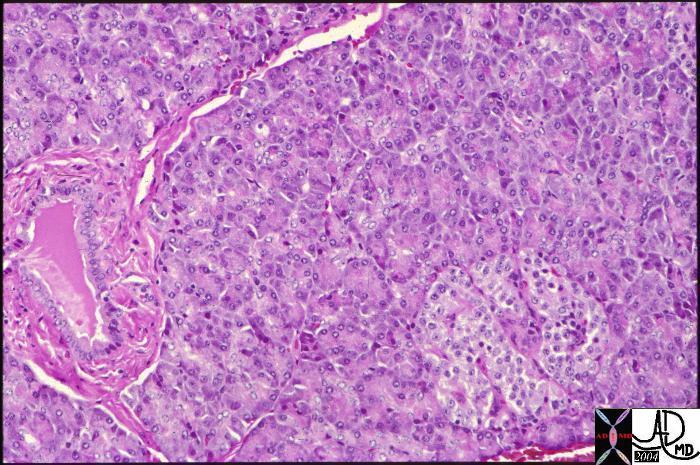
Normal histology of the pancreas showing the islet of Langerhans in the right lower corner of the image with the remaining glandular tissue being the exocrine portion of the gland. A duct can be seen in the left lower quadrant. The islets only make up about 2% of the gland. Courtesy Barbara Banner 15282
The islet cells are classified according to the type of cell that is present
The three primary cell types within the pancreatic islets are
(1) beta cells (60%), which produce and secrete insulin, as well as amylin, C peptide, proinsulin, and preproinsulin;
(2) a cells (25%), which synthesize glucagon;
(3) d cells (10%), which synthesize somatostatin; and
(4) other cells (5%) pancreatic polypeptide, D1, and enterochromaffin.
Classification – Functional Considerations:
The gland can be classified as a combination of an exocrine gland and an exocrine gland. Other members of the endocrine system include the pituitary thyroid parathyroid ovary and testis.
The pancreas is responsible for 50% digestion of the carbohydrates, 50% digestion of the protein and 90% of lipids.
Factors Stimulating Pancreatic Function
Cholecystokinin (CCK,) produced by small intestinal cells
is released upon entry of food into stomach
particularly in response to amino acids, and fat. The CCK targets pancreas and gallbladder
Secretin, is produced by small intestinal cells and is secreted in response to duodenal chyme with acid. Secretin targets the pancreas which responds by producing fluid rich in (HCO-3) which neutralises the acid in the duodenum.
It may also inhibit GI motility.
Somatostatin is produced by pancreatic and small intestinal cells
It is released by endocrine cells It inhibits gastrin secretion, increases the release of GIP, secretin, and motilin. In addition it inhibits gastric acid release, gastric motility, pancreatic exocrine secretions and gall bladder secretions.
Production And Function Of The Digestive Juices Produced By The Pancreas
Enzymes produced for Protein Digestion
The pancreatic proteases include trypsinogen, chymotrypsinogen, procarboxypeptidases, proelastase, collagenase. They are secreted in vesicles and must be activated. Trypinsogen is converted to trypsin by enteropeptidase (enterokinase) and by free trypsin. Peptide bonds are hydrolyzed into mono, di and some tri peptides so that they can be absorbed. On the brush border of the small intestine there are aminopeptidases which serve to hydrolyse the peptides further.
Enzymes produced for Carbohydrate Digestion
Pancreatic alpha amylase hydrolyzes alpha 1-4 bonds and alpha dextrinase to 1-6 branches
On the brush border of the small intestine there are other enzymes (isomaltase, maltase, sucrase, lactase) which serve to hydrolyse the carohydrates further.
Enzymes produced for Lipid Digestion
Pancreatic lipase hydrolyzes triglcerides (TG) to yield monoglycerides (MG), free fatty acids (FFA) and glycerol
Phospholipase and cholesterol esterase
Bile required and sometimes pancreatic colipase (binds TG and pancreatic lipase displacing bile)
HISTORICAL ASPECTS
In this section we explore the evolution of pancreatic knowledge with particular emphasis on structure, from the time of antiquity to the current day.
6000BC
There is a beautiful aboriginal rock painting in the Kakadu National Park, in the Northern Territory of Australia that depicts the earliest knowledge of anatomy. The image is of the bones and a series of triangles and diamond shapes. The pancreas was obviously far from the minds of these people – or so we think.
300-400 BC
5,600 years later the credit for the discovery of the pancreas is given to Herophilus, a Greek anatomist and surgeon, who was born in 336 BC in Chalcedon (now Kadiköy, Turkey) on the Asiatic side of the Bosporus river. Herophilus was one of the founders of the ancient schools of Medicine in Alexandria, Egypt. He may have been the first to have performed dissections of human bodies before public audiences, and thus is considered the father of scientific anatomy. He accurately described the eye, brain, liver, and pancreas, though the name “pancreas” only seemed to have evolved later.
The pancreas appears in Aristotle’s Historia Animalium, in which he refers to “another to the so-called pancreas” suggesting that not only was the organ known to Aristotle, (384-322 BC) but the name was already established. In the English translation of chapter 4 by Wentworth Thompson of Historia Animalium the word pancreas seems to be mentioned in context …”Again, other veins branch off from the big vein; one to the omentum, and another to the pancreas, from which vein run a number of veins through the mesentery. All these veins coalesce in a single large vein, along the entire gut and stomach to the oesophagus; about these parts there is a great ramification of branch veins.”
Historically however Ruphos an anatomist who lived in the first or second century AD has been given the credit for assigning the name to the pancreas. He was a surgeon of Ephesus in Asia Minor which today is the Asian portion of Turkey. The name “pancreas” means “all meat” or “all flesh” in Greek.
100-200 AD
Galen (Claudius Galenus 138-201 AD), , known as the the “Physician to the Gladiators” of Rome, and the Roman Emperor, tried to understand the function of the ‘kallikreas’ and his best guess was that it was a cushion for the stomach and a protection to the large blood vessels lying immediately behind it.
300 AD
In Judaic culture, the talmud, which is the written interpretation of rabbinic discussions on Jewish law, ethics, and customs, has a reference to the pancreas. At the time of writing in the 4th century there appears to have been recognition of the pancreas. It was referred to very briefly as the “finger of the liver.” The rabbis understood the anatomy of animals because of their strict techniques involved in animal slaughter and meticulous inspection of each of the organs to ensure halthy food. This practice resulted in a more than superficial knowledge of internal anatomy of the animals.
1200-1300
Attention to anatomy in Western culture only surfaced again with the publication in Bologna in 1316 of the Anothomia of Mundinus (1270-1326) in which Mundinus had once again started to perform human dissection.
1400 AD
da Vinci (1452-1519) was a keen observer of biology, but unlike Vesalius who lived in the next century as a dedicated anatomist, da Vinci spread his genius across many fields. As far as can be seen from da Vinci’ drawings and his commentaries, he seemed to have had no knowledge of the pancreas as a discrete structure in the body. He could have missed the pancreas because dissection of his human specimens may have been delayed resulting in autolysis of the gland.
da Vinci certainly knew of the splenic artery since there is a tiny drawing and a description of the atherosclerotic process of the splenic artery among his works. So we know he was in the anterior pararenal space during his dissections, but he just did not comment on the pancreas.
 This is a drawing of the “meseraic vessels” – presumably the celiac axis. Da Vinci was able to interview and perform an autopsy on a centenarian. He describes the dessicated and tortuos state of the vessels of this patient accurately depicting the atherosclerotic process. He describes the narrowed lumen and the consequences of poor blood flow.The translation of da Vinci’s text accompanying this one inch image is remarkably insightful and pioneering. (see atherosclerosis hisrorical da Vinci) 13045b
This is a drawing of the “meseraic vessels” – presumably the celiac axis. Da Vinci was able to interview and perform an autopsy on a centenarian. He describes the dessicated and tortuos state of the vessels of this patient accurately depicting the atherosclerotic process. He describes the narrowed lumen and the consequences of poor blood flow.The translation of da Vinci’s text accompanying this one inch image is remarkably insightful and pioneering. (see atherosclerosis hisrorical da Vinci) 13045b
1500 AD
Berengario da Carpi (1460-1530) an Italian physician and anatomist, was a professor at the University of Bologna from 1502 to 1527. He produced an extensive commentary on the Anothomia in 1521. It is the first anatomical text to contain illustrations and woodcuts based on human dissections, of which Berengario performed many. He was the the first to describe the heart valves. He probably was also the first to consider that the pancreas was a gland rather than an organ. (Dittrich )
His other claim to fame was his innovation in his use of mercurial ointment in the treatment of syphilis.
Andreas Vesalius (1515-1564) was born in Brussels, and educated in Paris and Padua as an anatomist and surgeon. Many consider Vesalius the true father of anatomy. He emphasised that the study of anatomy should come from direct observation from the human body and not learned from animals (which had been the habit of Galen) nor only from books (which had been the habit of others for so many years) . Vesalius’s brought a number of radical changes to the study of anatomy, but despite his open minded approach, and his disagreement with Galen on at least 200 other anatomic issues, he continued to follow Galenic theory that the pancreas functioned as a support structure for the stomach and mesenteric vessels. There was therefore no significant advancement on pancreatic knowledge in his time. His illustrated book De Hummani Corporis Fabrica was published in 1543. In plate 54 he noted that the “glandular” bodies arising in it” inferring that the pancreas arose in the the omentum and transverse mesocolon. The pancreas was regarded as several glands probably beacause it was broken up by the dissection of the vessels that course in and around it. In plate 56 there is a diagram of the greater omentum and transverse mesocolon where there is an elevation thought to be a representation of the pancreas and labelled with an “L”.
1600
Nicholaes Tulp (1606-1699) a surgeon, anatomist and the mayor of Amsterdam was the first to observe the effects pancreatitis at autopsy. He and his students are the subject of a very famous painting by Rembrandt called the Anatomy Lesson of Dr Tulp painted in 1632. The group portrait of Tulp, appointed ‘praelector anatomiae’ of the guild of surgeons, and seven of the guild’s members. Alberti in 1578, and Schenck in 1600 were others who recognised diseases in the pancreas including inflammatory diseases and tumors of the pancreas. (Sachs)

(1593-1674) by Rembrandt Harmenszoon van Rijn (1606-1669) Dr Tulp was one of the first to identify the anatomical changes of pancreatitis in a post mortem. In this particular painting he is dissecting the upper limb of a criminal who had been hanged for his crime. Aris Kindt had been hanged for armed robbery. Immediately after the execution, his body was taken to the Anatomy Theatre of the Guild of Surgeons. 54466 code historical reference Thre is a great explanation of this image at http://www.ohsu.edu/library/images/hom/rutkow122.jpg
1632 The Anatomy Lecture of Dr. Nicolaas Tulp (1593-1674) by Rembrandt Harmenszoon van Rijn (1606-1669) Dr Tulp was one of the first to identify the anatomical changes of pancreatitis in a post mortem. In this particular painting he is dissecting the upper limb of a criminal who had been hanged for his crime. Aris Kindt had been hanged for armed robbery. Immediately after the execution, his body was taken to the Anatomy Theatre of the Guild of Surgeons. 54466 code historical reference Thre is a great explanation of this image at http://www.ohsu.edu/library/images/hom/rutkow122.jpg
In 1642, a German émigré to Italy and prosector Johann Georg Wirsüng, discovered the pancreatic duct when he was a medical student in Padua, Italy. He questioned it’s nature and function and observed that there was never blood within it. He engraved a drawing of the duct on a copper plate and made seven copies, distributing the plates to other well known anatomists in Europe with the question as to whether it was an artery or a vein. Wirsüng was murdered by a student the year after his discovery. (Howard ) It was rumored that he was murdered by a his jealous mentor Johann Wesling, but Wesling was subsequently acquitted of the crime. Wirsung’s diagram of the duct resides in the University of Gottingen.
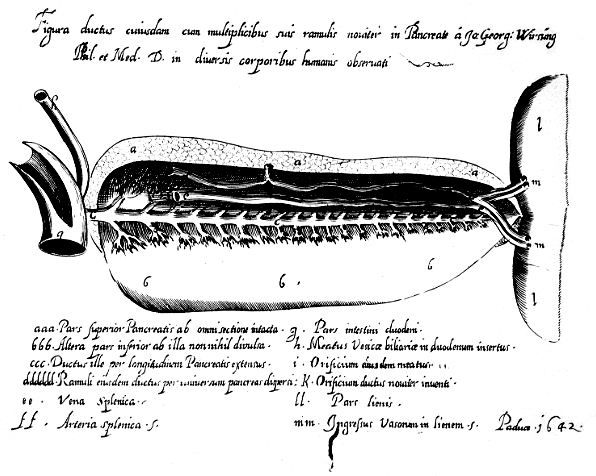
54476
At about the same time in England, in the middle of the 17th century, Thomas Wharton an anatomist, was also focused on the glands of the body, culminating in a Latin treatise Adenographia published in 1656. The work covered a description of the glands of the body providing the first thorough account and focus on the presence and importance of the glands. More importantly he distinguished them from the other viscera. He was able to classify the glands into excretory, reductive, or nutrient types. Wharton noted the superficial similarity between the pancreas and the submaxillary salivary glands. He discovered the duct of the submandibular salivary gland, which was subsequently called Whartons duct. He did not take the obvious next step to find the duct of the pancreas.
It would have been unlikely that Wharton was consulted by Wirsung about the nature of the bloodless tube of the pancreas since he would undoubtedly have known the answer. Not only had he noted the similarity of the structure of the pancreas with the salivary glands but also had discovered the duct of the submandibular gland. It did not take too much longer to understand the nature of the bloodless duct since de Graaf in 1664 in Holland had isolated the duct in the dog and was gaining early insight into pancreatic function.
54479a
web copyright unknown ref Graaf
Reignier de Graaf (1641-1673) of Holland wrote a treatise in latin which was later translated into English It was called Tractatus Anatomico-Medicus De Succo Pancreatico, – A physical and anatomical treatise on the nature and office of the pancreatic juice. It is one of the, if not the earliest works on pancreatic secretion. It seems that de Graaf and Wharton independantly came to the conclusion that the pancreas was a gland rather than an organ. This conceptual change, was an important step in the biological knowledge of the glands. De Graaf’s first work was originally published in Latin in 1664. He used the hollow quill of a goose feather to cannulate the pancreatic duct of a dog in 1663. He was the first to isolate and collect the secretions of the pancreas and gall bladder. Apparently he deduced that pancreatic juice was acidic based on his observation upon tasting it, that it was “insipid” with “acid-salt” flavor. He also collected the pancreatic juice of a sailor who died suddenly and noted that it was similar in character to the dogs juices.
Both de Graaf and his teacher Sylvius suggested that the pancreatic juice was linked to digestion and that it was required to identify the useful nutritional elements from the non essential elements; In later years he focused on the generative organs and as a result of this work, the Graafian follicle was named after him.
De Graaf was instrumental in introducing Anton van Leeuwenhoek, a fellow townsman to the attention of the Royal Society in London as a maker of exceptional microscopes. This was a turning point in Leeuwenhoek’s career who did not specifically study the pancreas but his discovery later created opportunity for others to discover the acini and Langerhans cells. Moyse, a student in Paris, described the histology of the exocrine pancreas, more than 70 years later, while Langerhans identified the Langerhans cells almost 200 years later.
In 1654 Francis Glisson, (1597-1677 ) published the first book devoted exclusively to the anatomy of the liver. Glisson injected coloured liquids enabling him to outline the vessels of the liver. He was thus able to identify and be the first to describe sphincter of the bile duct (1681) which was later rediscovered by Oddi in 1869 and is known today as the sphincter of Oddi.
In 1673, the Swiss physician Johann Conrad Brunner, while still a student in Paris, came near to discovering pancreatic diabetes after he noted that an experimental dog became thirsty and polyuric after a pancreatectomy. His book ‘Experimenta nova circa pancreas’ was published in 1683.
The term “diabetes mellitus” was coined in 1674 by the Oxford physician Thomas Willis, personal physician to King Charles II. Mellitus is Latin for honey, which is how Willis described the taste of the urine of diabetics (“as if imbued with honey and sugar”). Thomas Willis also described the arteries at the base of the brain.
1700AD
During the next 150 years, knowledge of the pancreas seemed to have been relatively dormant except for two discoveries in the structure of the pancreas. The first related to the papilla the small nipple-like protuberance representing the covered entrance of the the common channel of the pancreatic and bile duct as they enter the duodenum. This was named by Abraham Vater of Germany who noted the papilla in 1720. Although he was given the honor there were others who recognised the papilla before him including Brunner (1683). (Sachs)
Giovanni Santorini (1681-1737) of Italy studied medicine at Bologna, Padua, and Pisa, receiving the doctorate in 1701. One of his teachers was Marcello Malpighi (1628-1694). Santorini described the pancreatic accessory duct in 1724.
1800 AD.
Claude Bernard (1813-1878) was a French physiologist who heralded in a new era in the understanding of pancreatic physiology by strict adherence to the disciplines of experimental physiology. As a result of his work he established general physiology as a distinct discipline.
1800 AD.
Claude Bernard (1813-1878) was a French physiologist who heralded in a new era in the understanding of pancreatic physiology by strict adherence to the disciplines of experimental physiology. As a result of his work he established general physiology as a distinct discipline.
The two diagrams show the book cover of Claude Bernard’s book on expiremetal medicine and an etching by R. de Los Rios, after a painting by Leon Augustin L’hermitte, 1889. reference UTMB.edu
In 1847 Claude Bernard began a series of experiments that involved feeding famished rabbits high protein diets. On the basis of these experiments he was able to deduce that the secretions of the pancreas changed th ingested fat into fatty acids and glycerine. He attributed the reactions to an enzyme that was later called ‘pancreatic lipase’
There is a single reference that notes that he bathed a candle in pancreatic juice and noted that it dissolved again confirming the lipolyticnature of the pancreatic juices.
Despite the advancements made in physiology, it was not until 1852, almost 70 years after the introduction of Leeuwenhoek’s microcopes, that a student in Paris named D. Moyse, pioneered the knowledge of pancreatic acinar histology.
Rugerio Oddi (1864-1913) was an Italian anatomist and surgeon of Perugia who described the sphincter bearing his name in 1869. He struggled wih addictions throughout his life and was dismissed from his post as head of the Physiology Institute at the University of Genoa because of impropriety with drugs and finacial issues. Glisson had described the sphincter in 1681 but it may have been too early for the field to grasp and understand the context and importance and thus Oddi was given the honor of having his name associated with the sphincter.
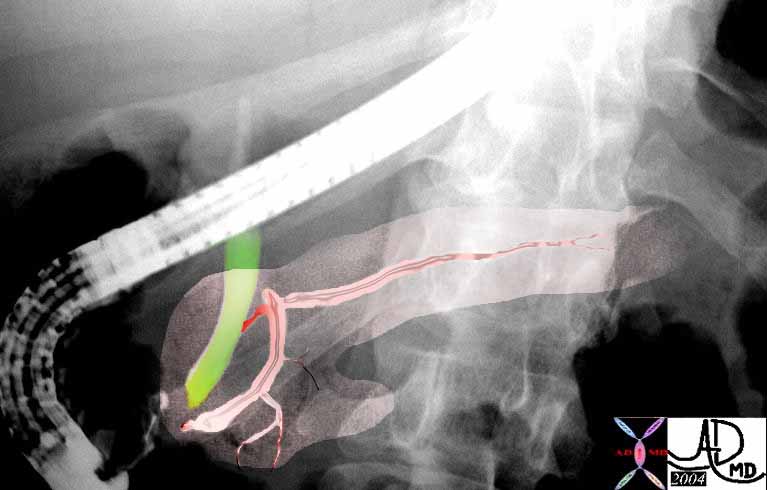 This ERCP shows the region of the The sphincter of Oddi which controls flow of pancreatic duct (pink) and bile duct (green) just before the common entrance into the duodenum at the ampulla. 39962b04 Courtesy Ashley Davidoff MD
This ERCP shows the region of the The sphincter of Oddi which controls flow of pancreatic duct (pink) and bile duct (green) just before the common entrance into the duodenum at the ampulla. 39962b04 Courtesy Ashley Davidoff MD
Alberti, Schenck and Tulp had noted post mortem changes in the diseased pancreas in late 16th and early 17th century and after Claude Bernard’s work on the lipolytic function (1847) the pathology of fat necrosis in acute pancreatitis was recognised by W. Balser in 1882, while autodigestion was a process recognised by H. Chiari in 1896.
In 1869, at an inaugral dissertation of his doctorate degree, Paul Langerhans, (1847-1888), presented his work on the islets of the pancreas subsequently known as the “islets of Langerhans” which represent only 2% of the cellular population of the pancreas. His work was conducted at the Berlin Institute of Pathology, under Rudolph Virchow. Langerhans, a physician, pathologist and anatomist, was innovative in the use of special stains which enabled visualisation of structural detail not before appreciated. The special stains allowed him to recognise the dendritic cells in the skin which now bear his name, and subsequently the islets. Identification of the islets opened up the door (or gates) to a huge field of knowledge relating to glucose metabolism and diabetes.
.
A picture of Paul Langerhans who discovered the islets of Langerhans while working in Berlin under Virchow Image from Historical Medical Personalities
| Langerhans contracted tuberculosis of the lung which forced him to emigrate to Madeira in Portugal where he continued with unbridled intellectual enthusiasm and he changed the course of his academic direction by exploring marine fauna of fthe Portuguese coast . He eventually died in Madeira of a renal infection at the age of 41 years in 1888.
Claude Bernard had laid the foundation of experimental physiology of the pancreas in 1847, and subsequent collaborators in Johann Nepomuk Eberle (1798-1834) of Bavaria, Alexander Danilevsky of St. Petersburg (in 1862), and Willy Kuhne (1837-1900), of Amsterdam advanced our knowledge of the pancreatic digestive enzymes.
This image of Ludwig Courvoisier (1843-1918), who was a surgeon who described ‘Courvoisier’s law’ – ‘if in the presence of jaundice the gallbladder is palpable, then the jaundice is unlikely to be due to a stone.’ This was first published in his book ‘The pathology and surgery of the gallbladder’ in Leipzig in 1890. 54478 Origin of this photo from surgical tutor.org a free on line resource and may be subject to copyright
In 1889 as the 19th century was closing, Oskar Minkowski, (1858-1931) a German internist and physiologist and Joseph von Mering (1849-1908) a pharmacist, were debating about whether pancreatic enzymes play a role in the digestion of fat. It was Joseph von Mering who suggested the idea of the pancreatectomy and thought it impossible, while Minkowski a German internist and physiologist became surgeon and removed the pancreas. Actually Johann Conrad Brunner in 1673 had already observed that pancretectomy had resulted in polyuria and polydypsia. Carl Gussenbauer (1842–1903), was a surgeon who pioneered pancreatic surgery. In 1882 he performed external drainage for a pancreatic cyst. Gussenbauer initiated the modern era of pancreatic surgery. Würzburg, Germany
PICTURE OF ROENTGEN Wilhelm Roentgen more than anybody else is responsible for initiating the work that subsequently opened up the in vivo secrets of the structural makeup of the pancreas. Image may be subject to copyright web 1900 AD The connection between cholelithiasis and acute pancreatitis (E.L. Opie and W. St. Halsted 1901) laid the foundation for 20th century research. In 1902, W.B. Bayliss and E.H. Starling, of London England discovered secretin, which stimulates pancreatic enzyme secretion. References of Historical Aspects John M. Howard, M.D.
|