- This is a 70 yo F former smoker with PMH significant for difficult to treat seropositive RA (has failed multiple agents; currently on upadacitinib), T2DM, HTN, CKD, COVID-19
- brief hospitalization 1 year ago and
- up to 2 lpm supplemental O2)3 months ago
- dyspnea on exertion following COVID-19 admission4
- PFTs revealed
- moderate reduction in DLCO and
- reduction in FVC compared to prior.
- FEMALE ON METHOTREXATE (RA) WITH NEW BROWNISH PRODUCTIVE COUGH, BILATERAL RHONCHI, ? PNEUMONIA
There are no focal consolidations or pleural effusions although there are slightly increased interstitial markings that are chronic.
CXR Follicular Bronchiolitis Nodular Interstitial Process

70-year-old female former smoker with long standing history of RA presents with chronic dyspnea. Frontal and lateral views of the chest reveals a coarsened nodular interstitial pattern. LVH is suggested on the lateral examination.
Ashley Davidoff MD TheCommonVein.net 132Lu 136650c

70-year-old female former smoker with long standing history of RA presents with chronic dyspnea. Frontal view of the chest reveals a coarsened nodular interstitial pattern with magnified views showing the micronodularity in the lower panels.
Ashley Davidoff MD TheCommonVein.net 132Lu 136650c01
HRCT
bilateral subpleural and peribronchovascular reticulations/interstitial thickening,
subpleural cystic remodeling in the anterior lobes,
bronchiectasis,
mosaicism, and
possible early cysts in the lower lobes.
The fibrotic changes have mildly progressed over 4years.
suggestive of constrictive bronchiolitis/OP,
follicular bronchiolitis, and
LIP among others. ),
Follicular Bronchiolitis, (BALT), Centrilobular Nodules, Air Trapping, Ground Glass Opacities (GGO) in Upper Lobes

70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the aortic arch reveals centrilobular nodules, ground-glass opacities, and mosaic attenuation (likely due to air trapping in this context) and bronchial wall thickening. In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136652
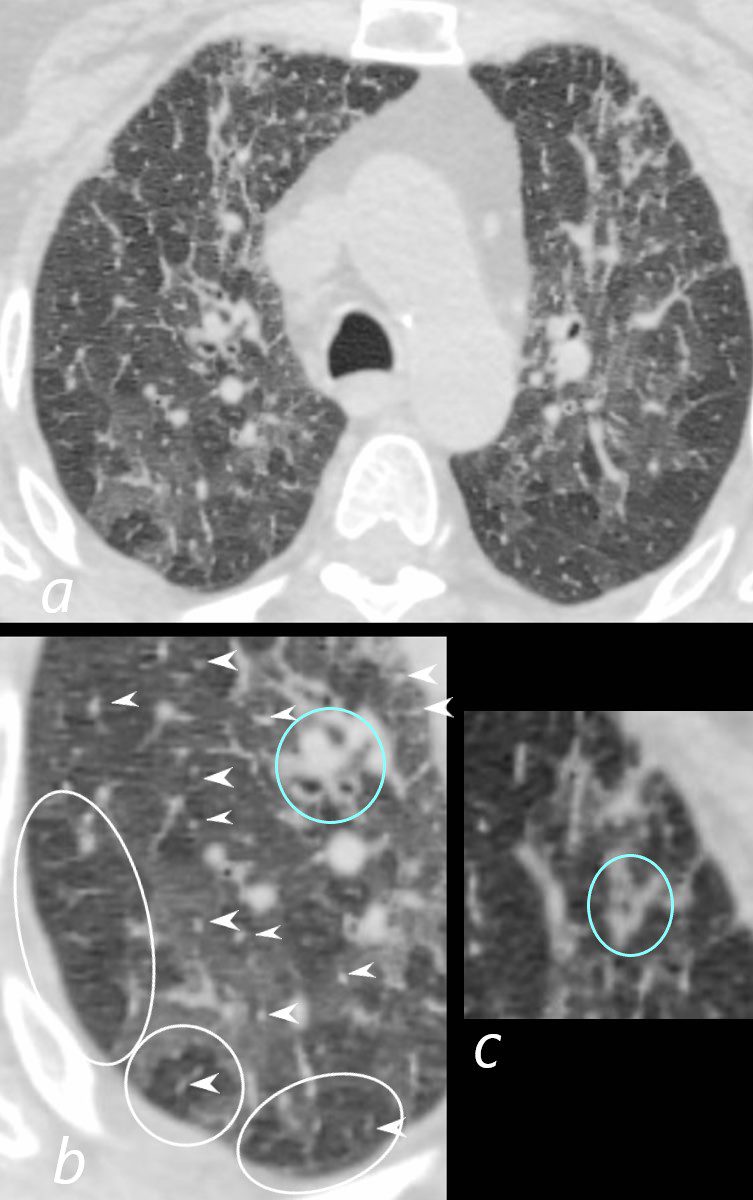
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the aortic arch reveals centrilobular nodules (b, white arrowheads) , ground-glass opacities, and mosaic attenuation (b, white rings) likely due to air trapping in this context, and bronchial wall thickening (b, c teal rings). There is some irregular thickening of the interlobular septa. In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136652cL
Bronchial Wall Thickening Follicular Bronchiolitis,

70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the carina reveals centrilobular nodules, ground-glass opacities, and mosaic attenuation (likely due to air trapping in this context) and bronchial wall thickening . In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136654
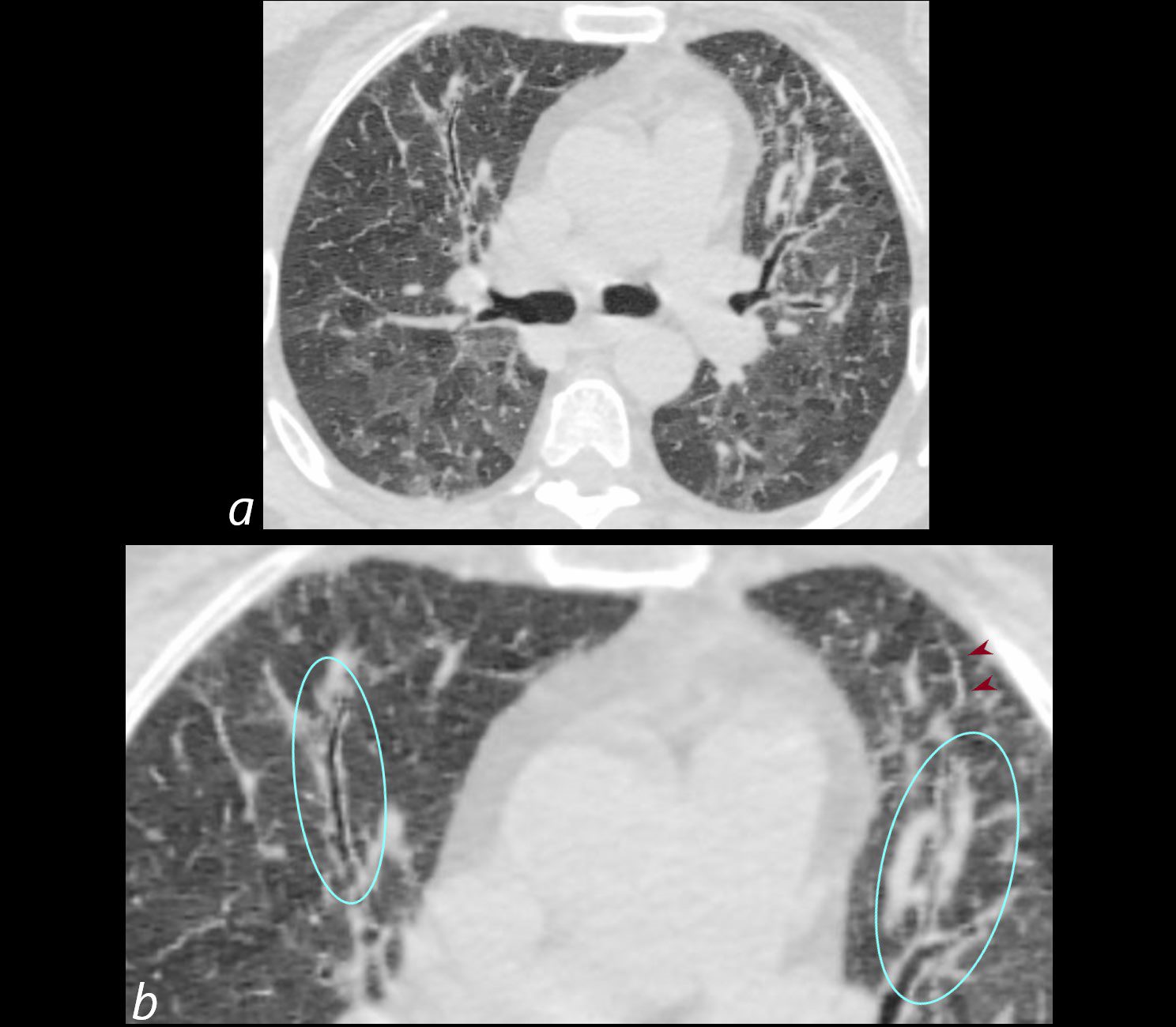
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the carina reveals centrilobular nodules, ground-glass opacities, and mosaic attenuation (likely due to air trapping in this context) and bronchial wall thickening . Bronchial wall thickening (b, maroon arrowheads) and irregular septal thickening (b maroon arrowheads) are noted.
In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136654cL
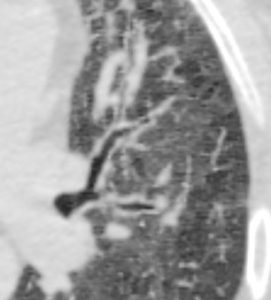
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the superior lingula bronchus shows prominent segmental and segmental bronchial wall thickening together with mosaic attenuation and ground glass opacities (GGO’s)
Ashley Davidoff MD TheCommonVein.net 132Lu 136656

70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the lower lung fields reveals centrilobular nodules, ground-glass opacities, and mosaic attenuation (likely due to air trapping in this context). In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136657
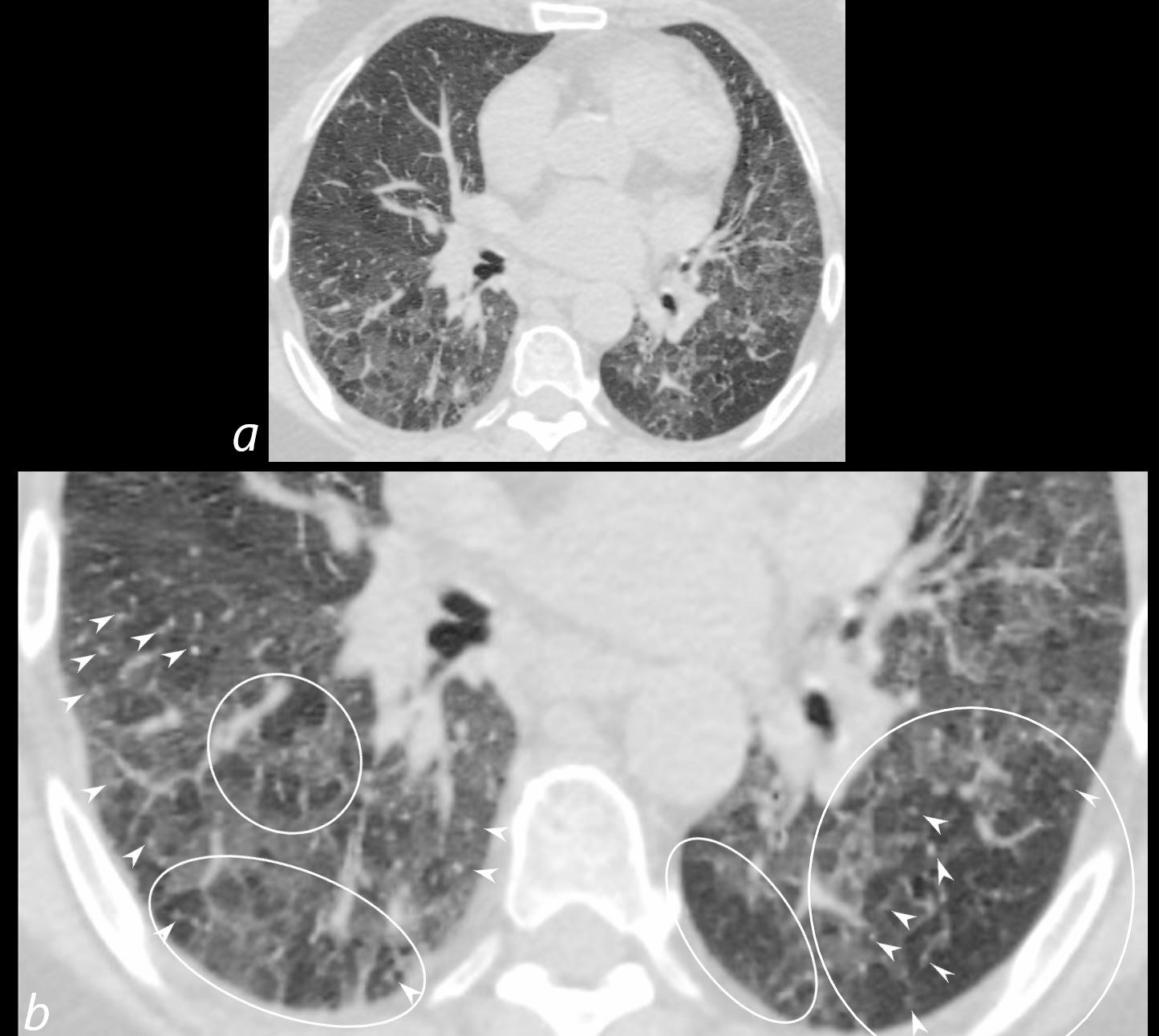
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the lower lung fields reveals centrilobular nodules (b white arrowheads), ground-glass opacities, and mosaic attenuation (b, white rings) likely due to air trapping in this context.
In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136657cL

70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the lower lung fields reveals centrilobular nodules, ground-glass opacities, and mosaic attenuation (likely due to air trapping in this context). In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136659

70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the lower lung fields reveals centrilobular nodules, ground-glass opacities, and mosaic attenuation (likely due to air trapping in this context). In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136660
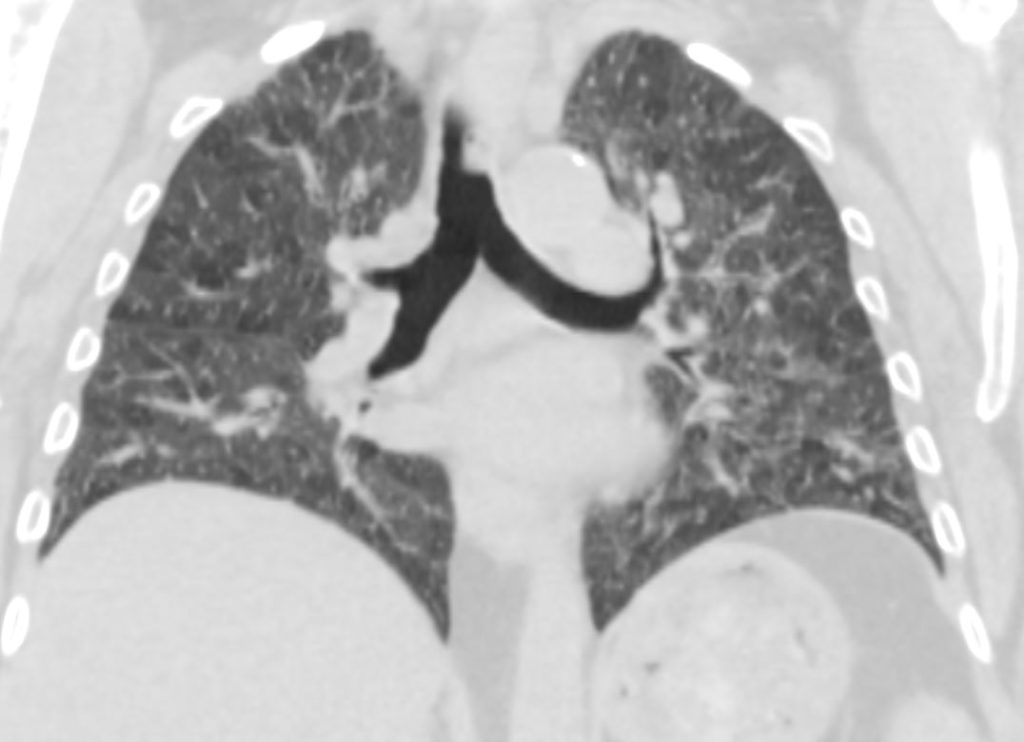
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
CT in the coronal plane of the chest at the level of the carina reveals bilateral diffuse changes in the lungs characterized by centrilobular nodules, ground-glass opacities, mosaic attenuation (likely due to air trapping in this context) and irregular thickening of the interlobular septa.
In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136661
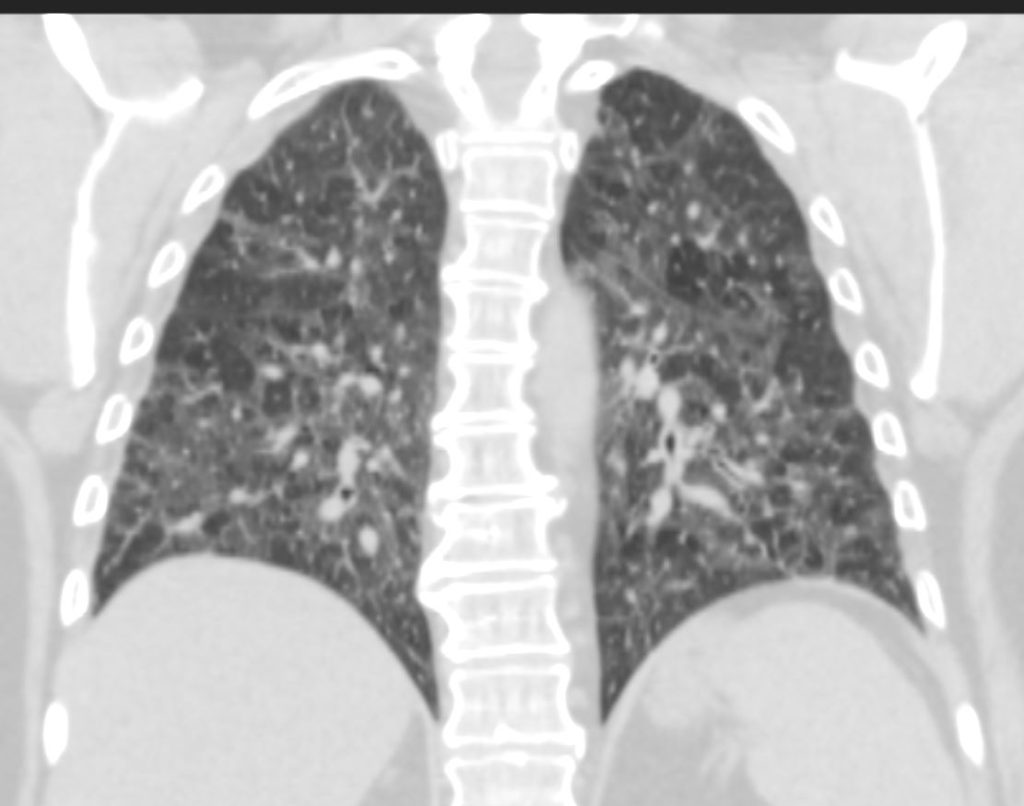
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
CT in the coronal plane of the chest at the level of the spine reveals bilateral diffuse changes in the lungs characterized by centrilobular nodules, ground-glass opacities, mosaic attenuation (likely due to air trapping in this context) and irregular thickening of the interlobular septa.
In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136663
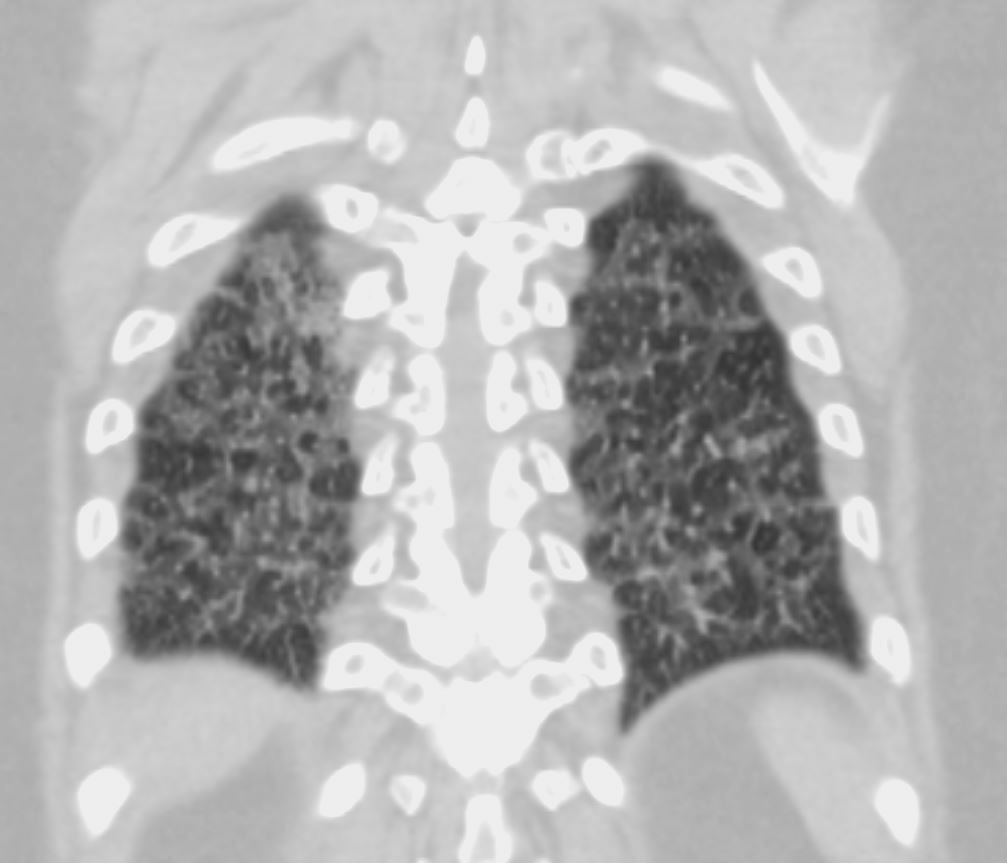
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
CT in the coronal plane of the chest at the level of the spine reveals bilateral diffuse changes in the lungs characterized by centrilobular nodules, ground-glass opacities, mosaic attenuation (likely due to air trapping in this context) and irregular thickening of the interlobular septa.
In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136664
modification of the immunosuppressive regimen to one with lung effect (potentially low dose prednisone and MMF or rituximab); however, given that patient’s RA has been extremely difficult to control, the fact that the CT had demonstrated only mild progression in the fibrotic changes,
start nintedanib for progressive fibrosing ILD.
