The “batwing pattern” (or “butterfly pattern”) refers to a specific radiologic appearance on chest X-rays, where there is bilateral, perihilar alveolar edema with a shape resembling a bat’s wings or a butterfly. This pattern is characterized by central alveolar opacities that extend outward toward the lungs’ periphery, often sparing the outermost edges.
The alveolar pattern is a radiological term used to describe a
specific appearance on chest X-rays or CT scans that indicates the
filling of the alveoli with material such as fluid, pus, blood, or cells.
This pattern typically appears as areas of increased opacity
(whiteness) with ill-defined, fluffy borders that may merge with
adjacent lung tissue, often creating a “cloud-like” or “patchy”
appearance. Common causes of an alveolar pattern include
pneumonia (where pus fills the alveoli), pulmonary edema (fluid in
the alveoli), pulmonary hemorrhage (blood filling the airspaces),
and alveolar proteinosis (accumulation of proteinaceous material).
The pattern may also show characteristics like air bronchograms,
where air-filled bronchi are visible against the opaque alveolar
background, helping to differentiate it from other types of lung
pathology. (Etesami)
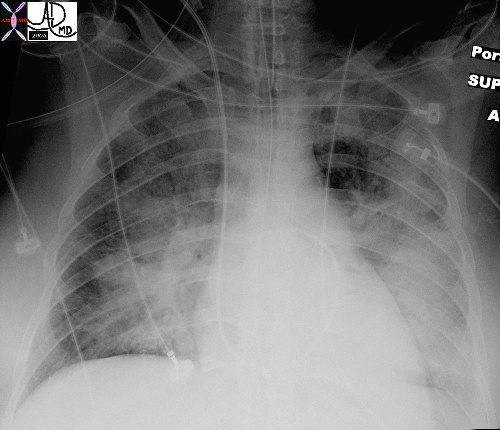
In this patient with acute congestive cardiac failure the consolidation that has hilar distribution has reminded radiologists of bat wings and butterfly wings and is caused by alveolar edema. As a result of the fluid in the alveoli, gas exchange across the respiratory membrane is reduced resulting in a decrease in oxygen saturation, and thus requiring intubation to improve the gas exchange process. Note the endotracheal tube as well as the central venous line that is used to assess the heart pressure and monitor the congestion.
Ashley Davidoff MDTheCommonVein.net 42073b01
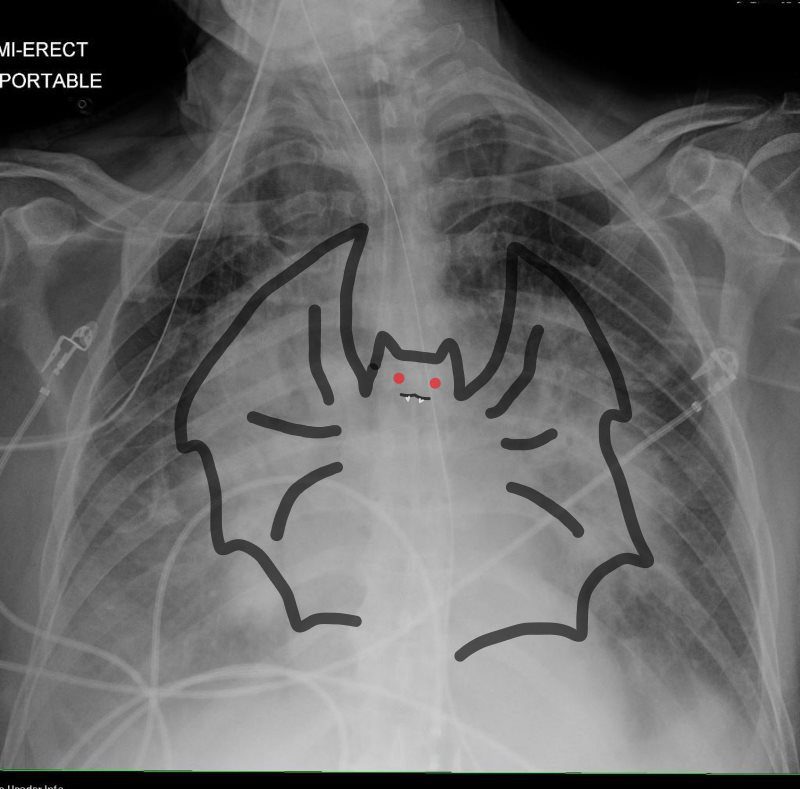
In this patient with acute congestive cardiac failure the consolidation that has hilar distribution has reminded radiologists of bat wings and is caused by alveolar edema. As a result of the fluid in the alveoli, gas exchange across the respiratory membrane is reduced and required intubation to improve the gas exchange process. Note the endotracheal tube as well as the central venous line that is used to assess the heart pressure and monitor the congestion.
Ashley Davidoff MD
TheCommonVein.net 42073b01
Memory Image Neelou Etesami MS4 PhD
Association with Heart Failure and Other Causes of Alveolar Edema
The batwing pattern is most commonly associated with cardiogenic pulmonary edema due to heart failure, where increased hydrostatic pressure in the pulmonary capillaries causes fluid to leak into the alveolar spaces. However, the pattern itself does not exclusively indicate heart failure and can be seen in various causes of alveolar edema.
Conditions That Can Produce a Batwing Pattern
While cardiogenic pulmonary edema is the most common, several other conditions can also lead to a batwing pattern:
- Non-Cardiogenic Pulmonary Edema:
- Acute Respiratory Distress Syndrome (ARDS): Can cause diffuse alveolar edema, sometimes with a similar central distribution.
- Fluid Overload: Excessive fluid administration can lead to pulmonary edema with a similar radiologic appearance.
- Renal Failure: Fluid retention due to renal dysfunction can lead to pulmonary edema that may display a batwing pattern.
- Infections:
- Pneumonia: Although more commonly peripheral or lobar, certain viral or atypical pneumonias can sometimes present with a bilateral perihilar pattern resembling bat wings.
- Pulmonary Hemorrhage:
- In cases of diffuse alveolar hemorrhage (e.g., Goodpasture syndrome, systemic lupus erythematosus), blood can fill the alveolar spaces and create a similar central pattern.
Key Point
While the batwing pattern is strongly associated with cardiogenic pulmonary edema, it can be seen in other forms of alveolar edema or alveolar filling processes. Therefore, while it suggests the possibility of heart failure, it does not specifically confirm it, and clinical correlation is essential for accurate diagnosis.
The alveolar pattern is a radiological term used to describe a
specific appearance on chest X-rays or CT scans that indicates the
filling of the alveoli with material such as fluid, pus, blood, or cells.
This pattern typically appears as areas of increased opacity
with ill-defined, fluffy borders that may merge with
adjacent lung tissue, often creating a “cloud-like” or “patchy”
appearance. Common causes of an alveolar pattern include
pneumonia (where pus fills the alveoli), pulmonary edema (fluid in
the alveoli), pulmonary hemorrhage (blood filling the airspaces),
and alveolar proteinosis (accumulation of proteinaceous material).
The pattern may also show characteristics like air bronchograms,
where air-filled bronchi are visible against the opaque alveolar
background, helping to differentiate it from other types of lung
pathology.
