Sickle Cell Disease (SCD) can have significant impacts on the lungs and chest, leading to both acute and chronic complications. The lung involvement in SCD is a major contributor to morbidity and mortality, especially as patients age. Below is an overview of how SCD affects the lungs and chest.
- Acute Complications
- Acute Chest Syndrome (ACS):
- Pulmonary Embolism (PE):
- Pneumonia
- Rib or Vertebral Infarction
-
Chronic Complications:
- Pulmonary Hypertension
- Chronic Hypoxemia
- Obstructive Sleep Apnea
- Pulmonary Hypertension
Acute Complications:
- Acute Chest Syndrome (ACS):
- Definition: ACS is one of the most serious and potentially life-threatening complications in SCD. It is defined by the presence of new pulmonary infiltrates on imaging (such as a chest X-ray) along with symptoms like fever, chest pain, hypoxemia (low oxygen levels), and respiratory distress.
- Causes:
- Pulmonary infection (bacterial or viral)
- Fat embolism from necrotic bone marrow
- Vaso-occlusion of pulmonary vasculature
- Hypoventilation (due to rib infarction or splinting from pain)
- Presentation: Patients may experience fever, dyspnea (shortness of breath), chest pain, coughing, and a rapid drop in oxygen saturation.
- Treatment: ACS requires prompt treatment, including oxygen therapy, antibiotics, bronchodilators, blood transfusion, and in severe cases, mechanical ventilation.
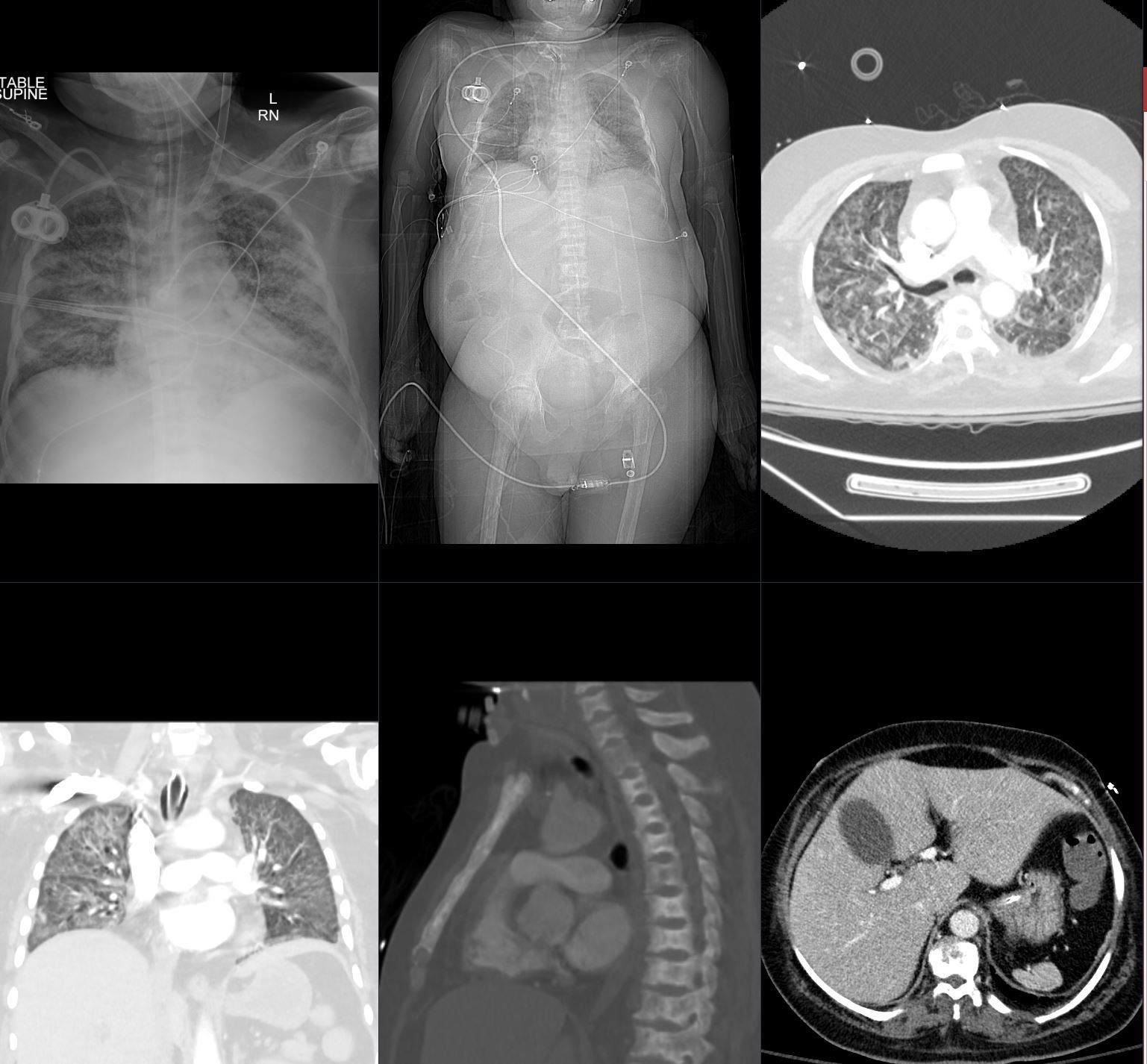
ARDS Sickle Cell Crisis
The CXR and CT in this 26 year old male in sickle cell crisis shows diffuse and symmetrical ground glass changes with subpleural sparing best observed in images b and d. The bony changes are characterized by bilateral avascular necrosis of the hips (b) and diffuse sclerosis with fish mouth deformity of the thoracic and lumbar spine (e). The spleen is extremely small but still perfusing (e)
Ashley Davidoff TheCommonVein.net b11662-01L
Diffuse Ground Glass Changes and Subpleural Sparing
ARDS Sickle Cell Crisis
The CXR in this 26 year old male in sickle cell crisis shows diffuse and symmetrical ground glass changes with subpleural sparing
Ashley Davidoff TheCommonVein.net b11662-02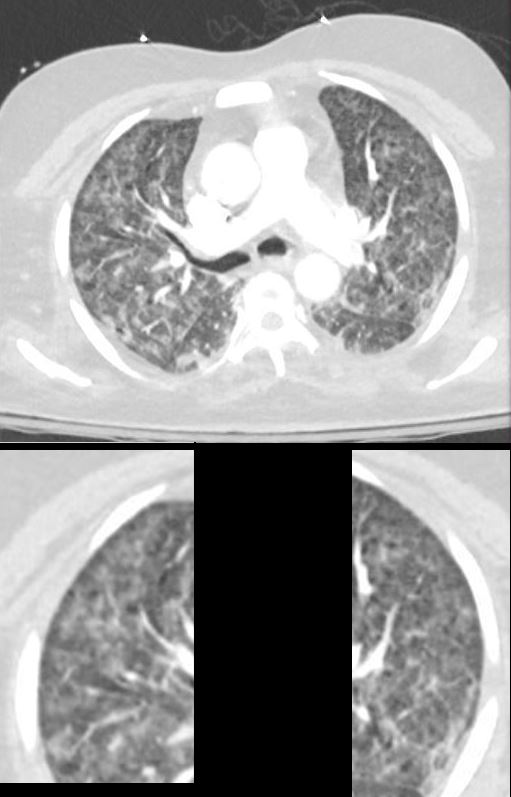
Diffuse Ground Glass Changes and Subpleural Sparing
ARDS Sickle Cell Crisis
The CXR in this 26 year old male in sickle cell crisis shows diffuse and symmetrical ground glass changes with subpleural sparing
Ashley Davidoff TheCommonVein.net b11662-03
- Pulmonary Embolism (PE):
- Increased Risk: SCD patients are at higher risk for pulmonary embolism due to the hypercoagulable state induced by chronic hemolysis and inflammation.
- Presentation: Sudden onset of chest pain, dyspnea, and hypoxemia may suggest PE.
- Diagnosis and Treatment: Imaging, such as a CT pulmonary angiogram, can confirm PE, and treatment usually involves anticoagulation therapy.
- Pneumonia:
- Higher Susceptibility: People with SCD are prone to infections, particularly pneumonia, due to functional asplenia (loss of spleen function) and immune dysfunction.
- Bacterial and Viral Pneumonia: Both bacterial and viral infections can lead to pneumonia, often precipitating or mimicking Acute Chest Syndrome.
- Rib or Vertebral Infarction:
- Bone Pain and Chest Pain: Vaso-occlusion can lead to infarction of the ribs or vertebrae, causing severe chest or back pain. This can make breathing painful and lead to hypoventilation, contributing to ACS.
Chronic Complications:
- Pulmonary Hypertension (PH):
- Definition: Pulmonary hypertension is a chronic increase in pressure in the pulmonary arteries. It occurs in up to 30% of adults with SCD and is associated with worse survival.
- Causes:
- Chronic hemolysis leading to increased free hemoglobin, which scavenges nitric oxide (NO), a vasodilator, leading to pulmonary vasoconstriction.
- Chronic hypoxia and inflammation.
- Presentation: Symptoms include exertional dyspnea, fatigue, and in severe cases, right heart failure.
- Diagnosis: Echocardiography and right heart catheterization can confirm the diagnosis.
- Treatment: Oxygen therapy, pulmonary vasodilators, and management of underlying SCD complications may be used.
- Restrictive Lung Disease:
- Cause: Recurrent episodes of ACS and chronic lung damage can lead to fibrosis, resulting in restrictive lung disease (reduced lung volumes and compliance).
- Presentation: Patients may have progressive shortness of breath and decreased exercise tolerance.
- Diagnosis and Treatment: Pulmonary function tests (PFTs) show a reduced lung capacity. Treatment focuses on preventing further damage and optimizing lung function.
- Chronic Hypoxemia:
- Cause: Chronic vaso-occlusion and lung damage, along with anemia, can lead to persistent low oxygen levels in the blood.
- Consequences: Chronic hypoxemia contributes to the development of pulmonary hypertension and right heart strain.
- Obstructive Sleep Apnea (OSA):
- Increased Risk: People with SCD have a higher prevalence of OSA due to factors such as adenotonsillar hypertrophy (enlargement) and obesity.
- Impact: OSA can worsen nocturnal hypoxemia, increasing the risk of complications like ACS and pulmonary hypertension.
- Treatment: Continuous Positive Airway Pressure (CPAP) or other interventions for OSA can improve oxygenation during sleep.
Vaso-Occlusive Crises (VOC) and Chest Pain:
- VOC in the Chest: Vaso-occlusion can affect the ribs, causing acute rib infarction, which leads to significant chest pain. This pain can mimic pneumonia or ACS, and patients may breathe shallowly (splinting), leading to hypoventilation and worsening lung function.
- Pain Management: Adequate pain control is crucial to prevent hypoventilation and subsequent complications.
Surgical Considerations:
- Cholecystectomy: Many SCD patients develop gallstones and may require gallbladder surgery. Post-operative pulmonary complications are a concern, especially ACS, and patients should receive appropriate perioperative management, including incentive spirometry to prevent atelectasis (lung collapse).
Preventive Measures for Lung Complications:
- Hydroxyurea Therapy: Reduces the frequency of painful crises and ACS episodes by increasing fetal hemoglobin (HbF) levels and decreasing vaso-occlusion.
- Chronic Transfusion Therapy: Used in some patients to reduce the risk of recurrent ACS and stroke by lowering the proportion of sickled red blood cells.
- Vaccination and Prophylaxis: Routine vaccinations, especially for pneumococcal infections, and antibiotic prophylaxis (e.g., penicillin) are important in reducing the risk of pneumonia.
- Pulmonary Rehabilitation: For patients with chronic lung disease, pulmonary rehabilitation can help improve lung function and quality of life.
Summary:
In Sickle Cell Disease, the lungs and chest are often affected by both acute and chronic complications, with Acute Chest Syndrome being the most dangerous acute event, and pulmonary hypertension and chronic lung disease contributing to long-term morbidity. Early recognition and prompt treatment of these conditions, along with preventive care, are critical in improving outcomes for individuals with SCD.
