A bulla is an air-filled space within the lung parenchyma that is greater than 1 cm in diameter and has a thin wall (<1 mm). It results from the destruction of alveolar walls due to processes such as emphysema or other parenchymal damage. Bullae are commonly subpleural and are considered a form of emphysematous change.
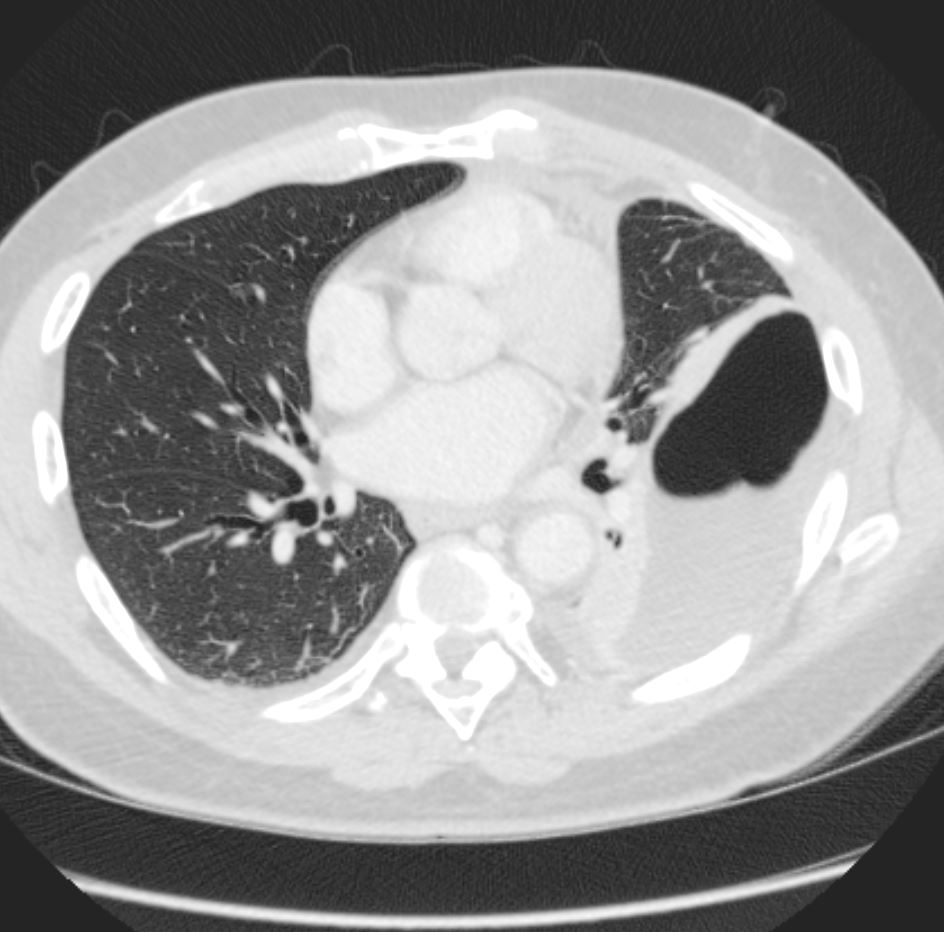
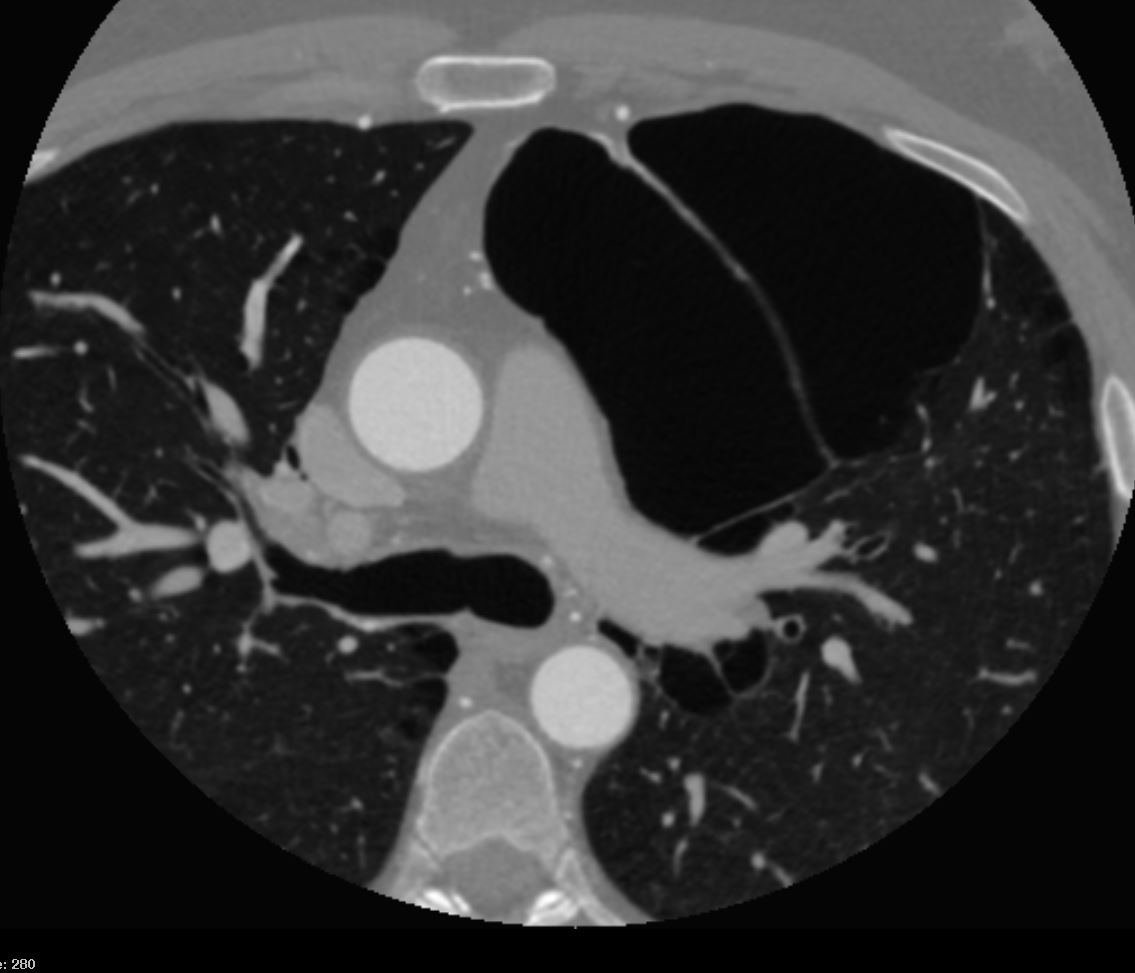
CT scan in the axial and coronal plains in a 55 year old male shows a combination of blebs bulla and paraseptal emphysema most prominent in the apex of the right upper lobe
Ashley Davidoff MD TheCommonVein.net 136929

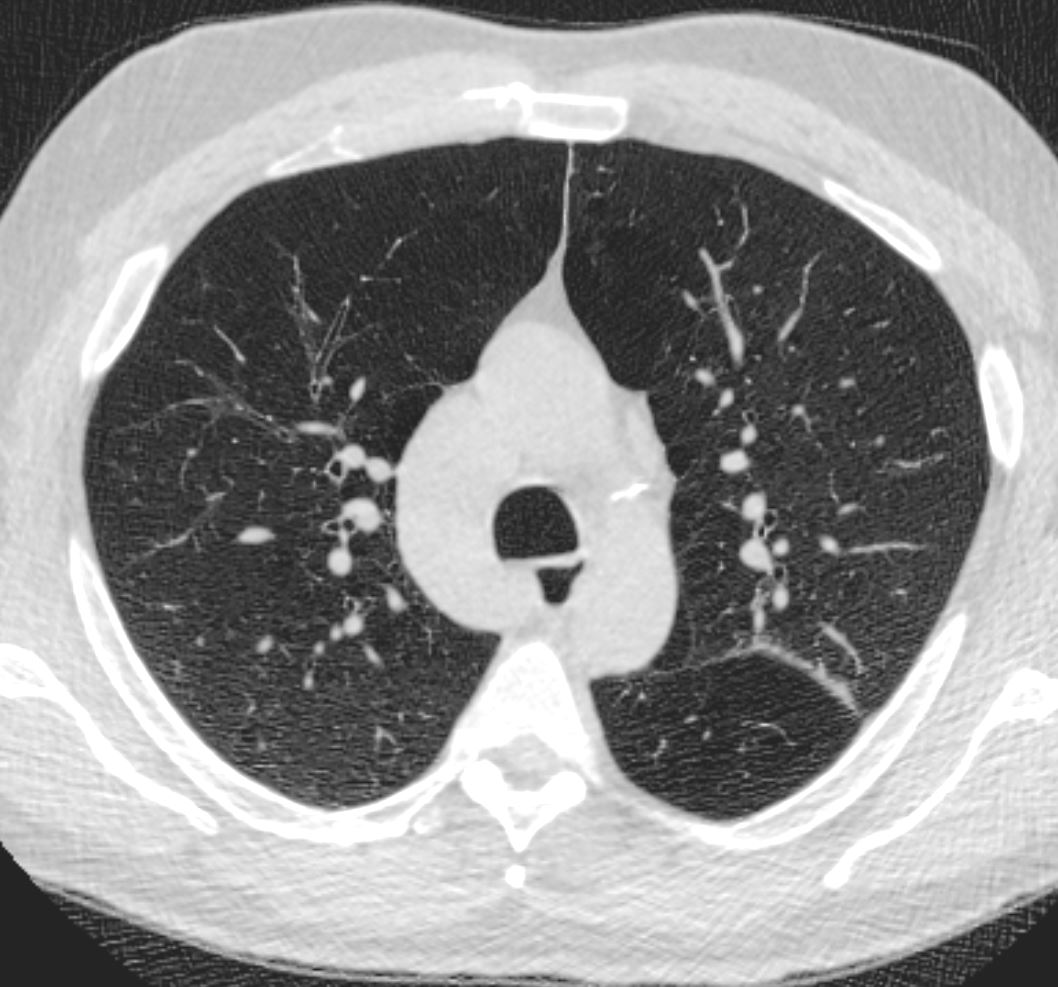
CT scan in the axial plane of a 64- year-old man with emphysema shows bilateral apical bullous lung disease,
Ashley Davidoff MD TheCommonVein.net 136440

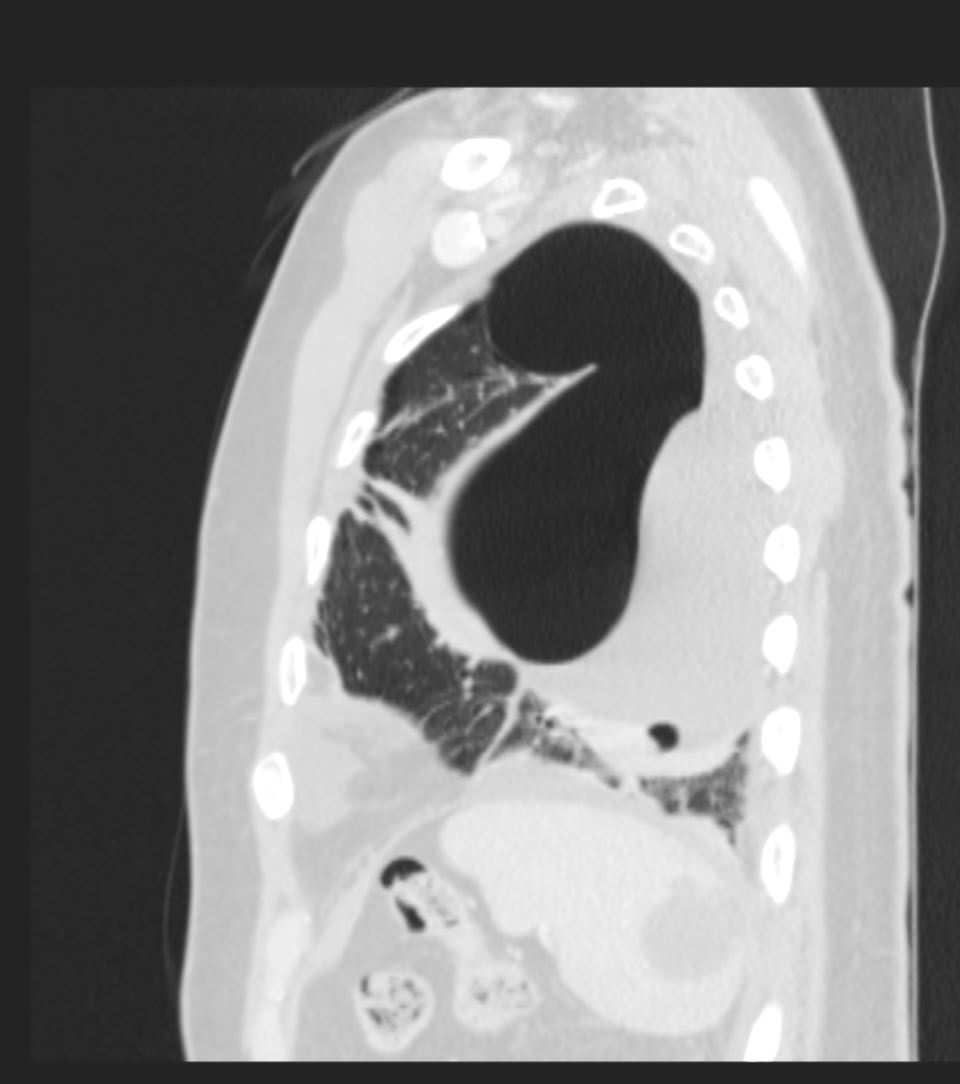
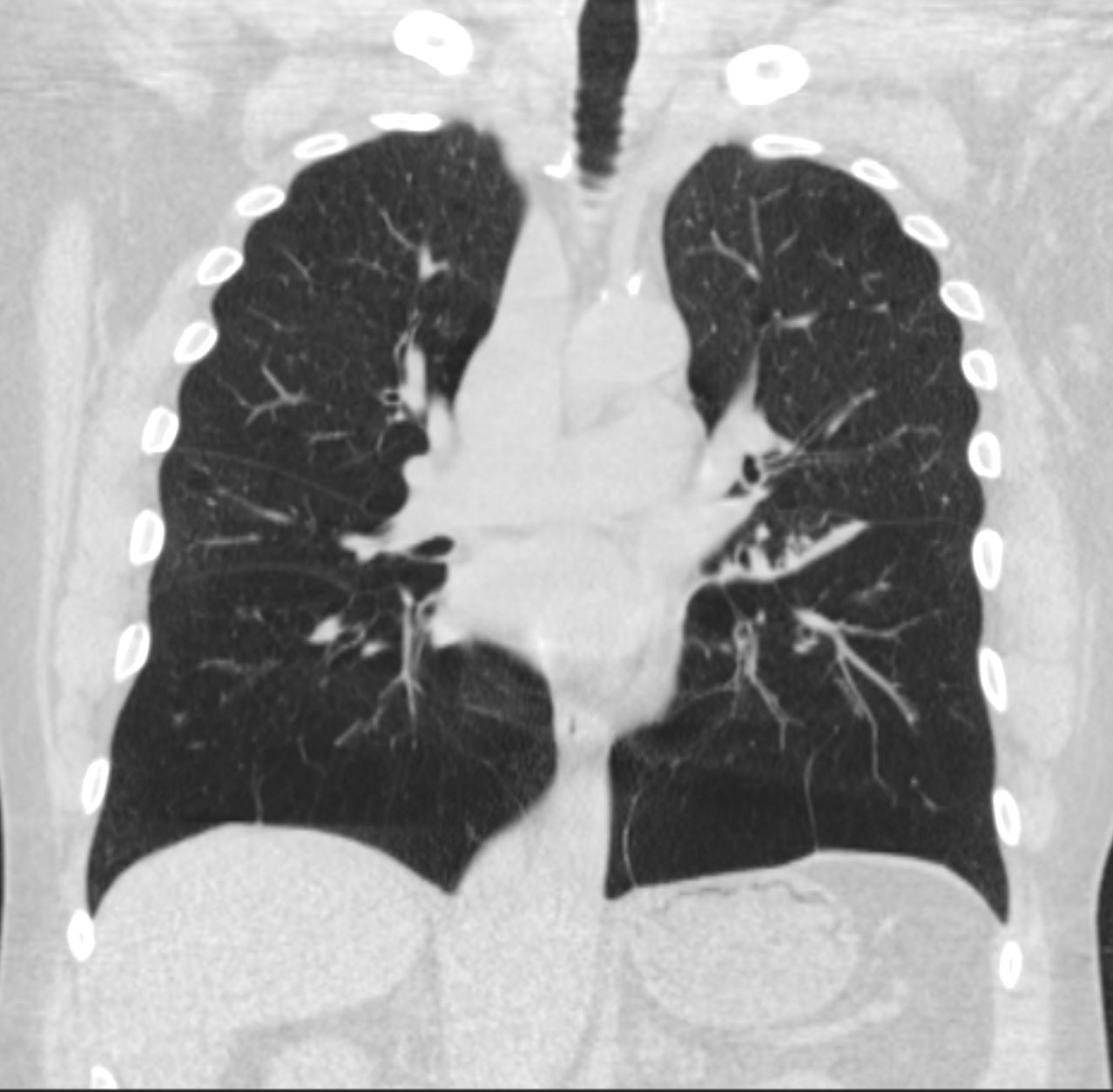
CT scan in the coronal plane of a 64- year-old man with emphysema shows bilateral apical bullous lung disease, magnified in the lower image
Ashley Davidoff MD TheCommonVein.Net 136439c

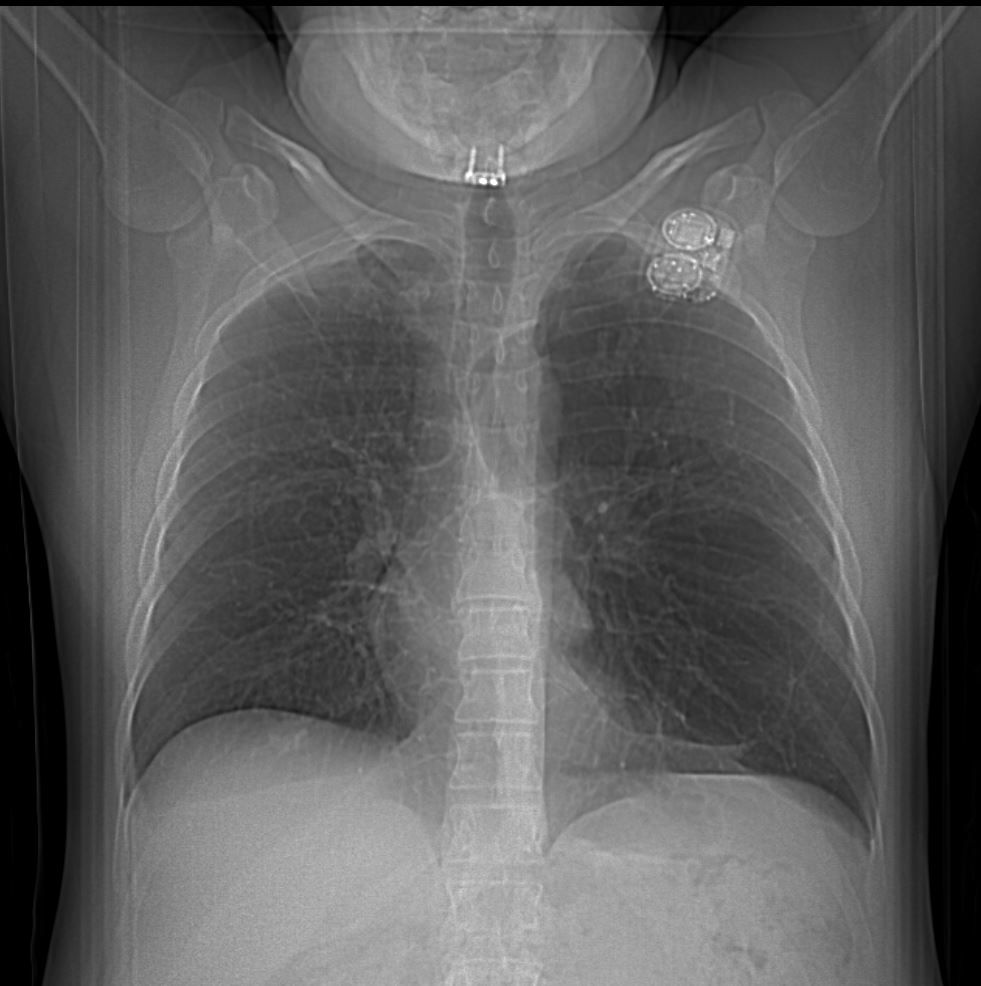
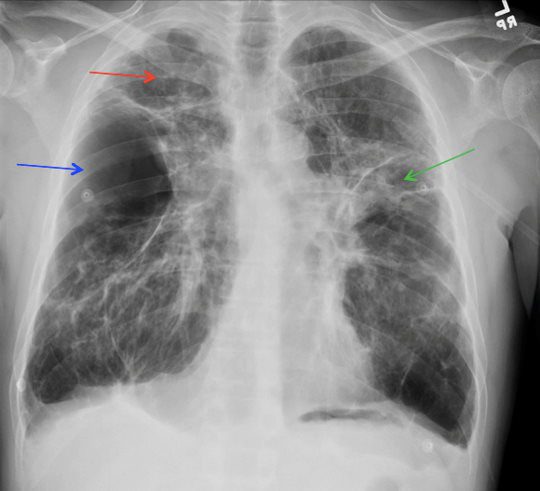
28-year-old male presents for follow up post bullectomy after having a spontaneous pneumothorax. He has a narrow A-P diameter and an asthenic build and the surgical sutures are noted in the left apex of the lung (b, arrowhead)
Ashley Davidoff MD TheCommonVein.net 136231c
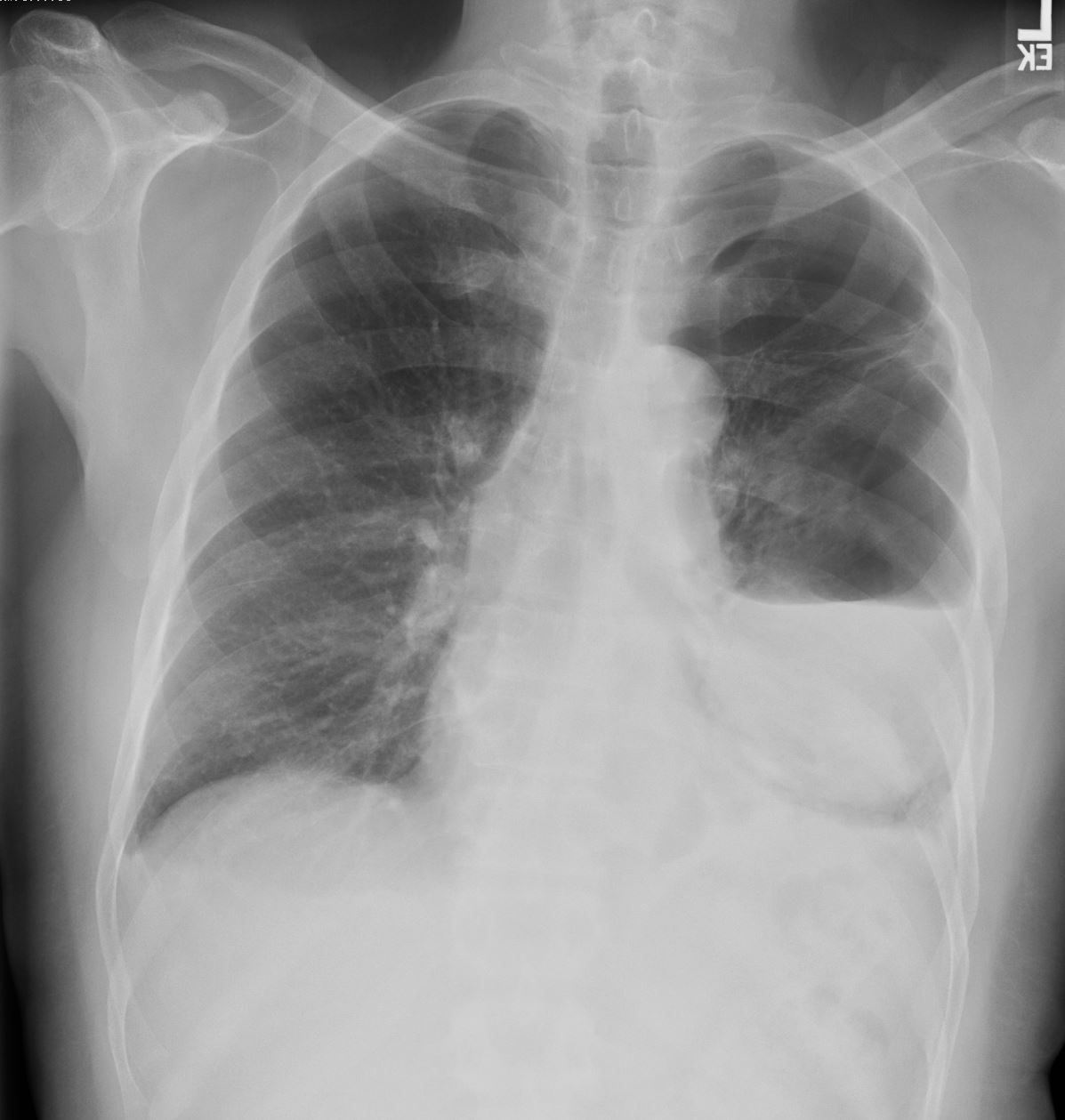
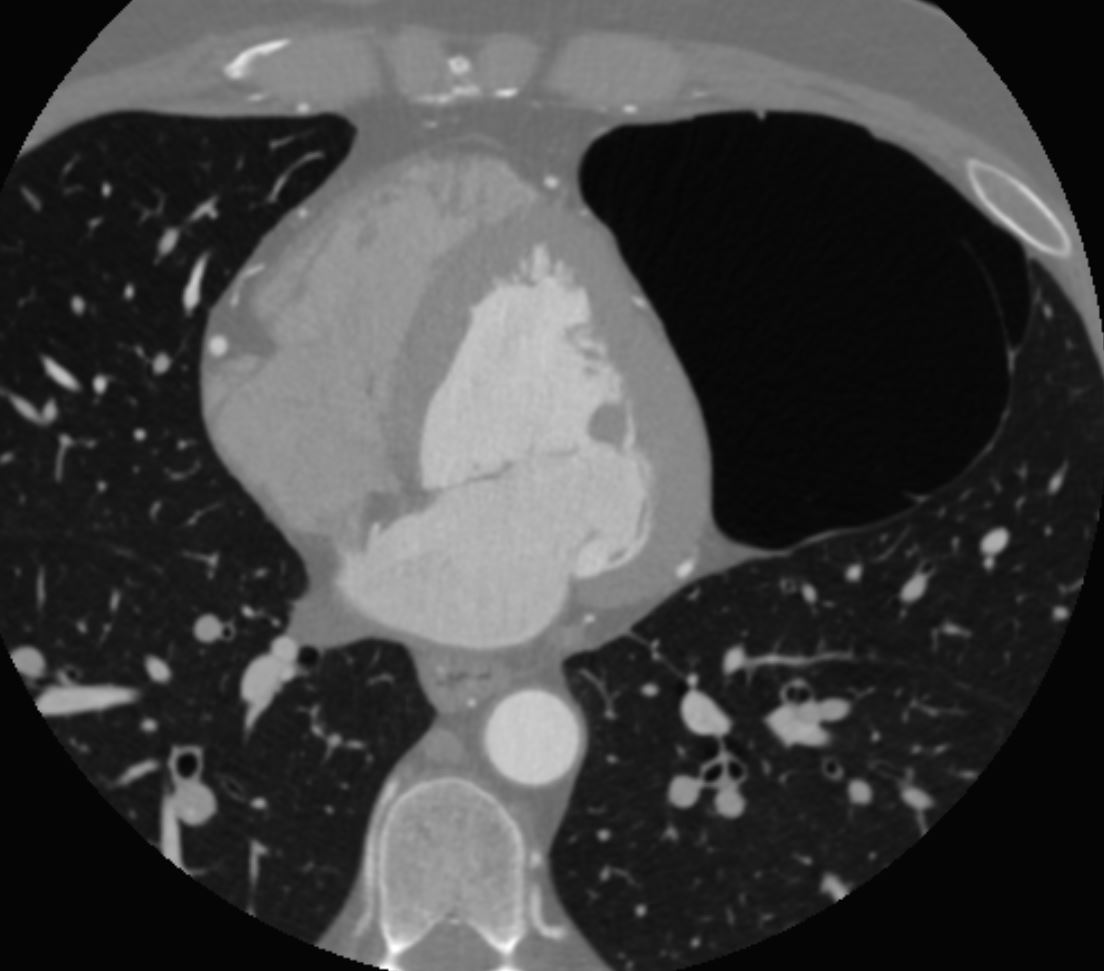
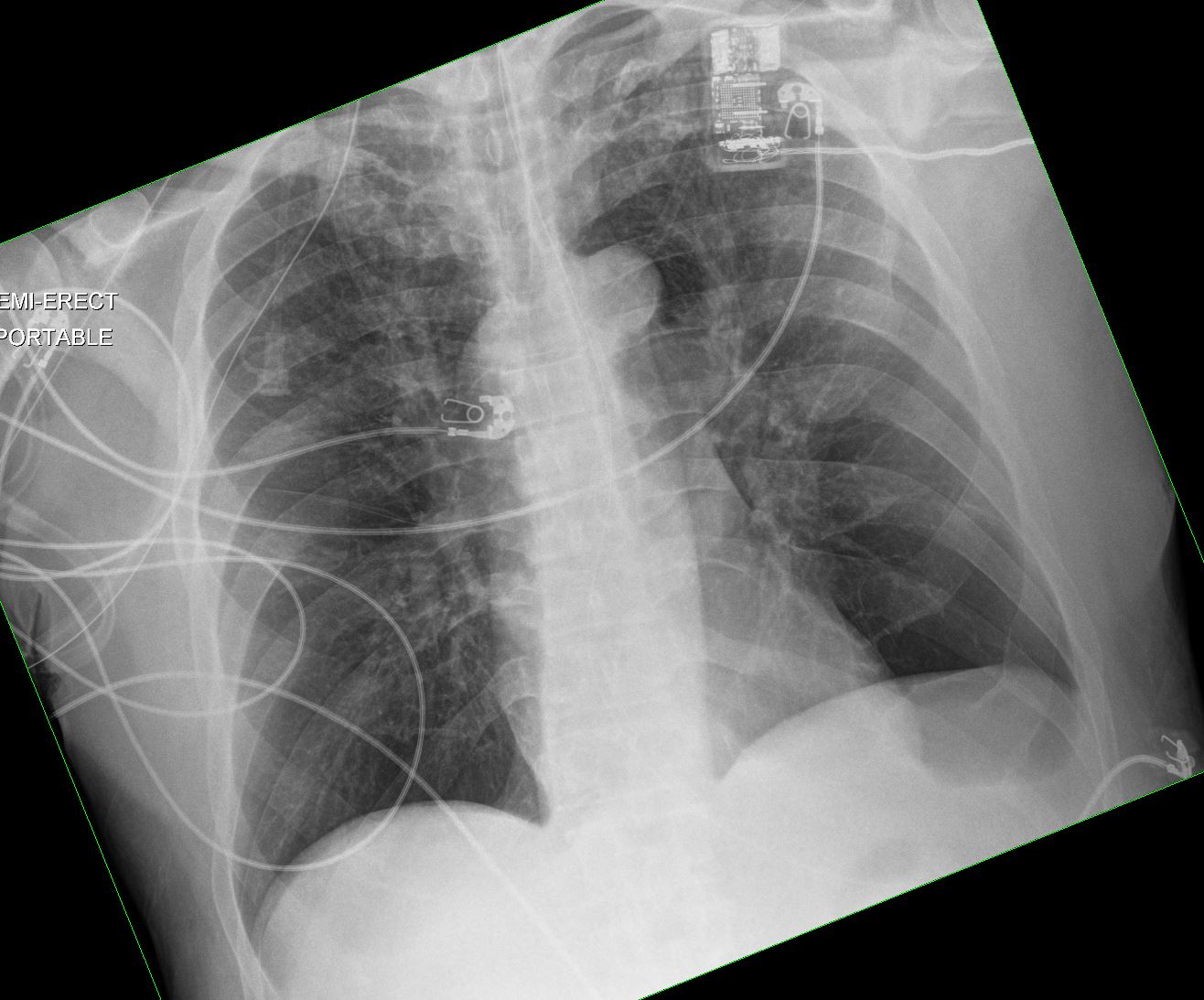
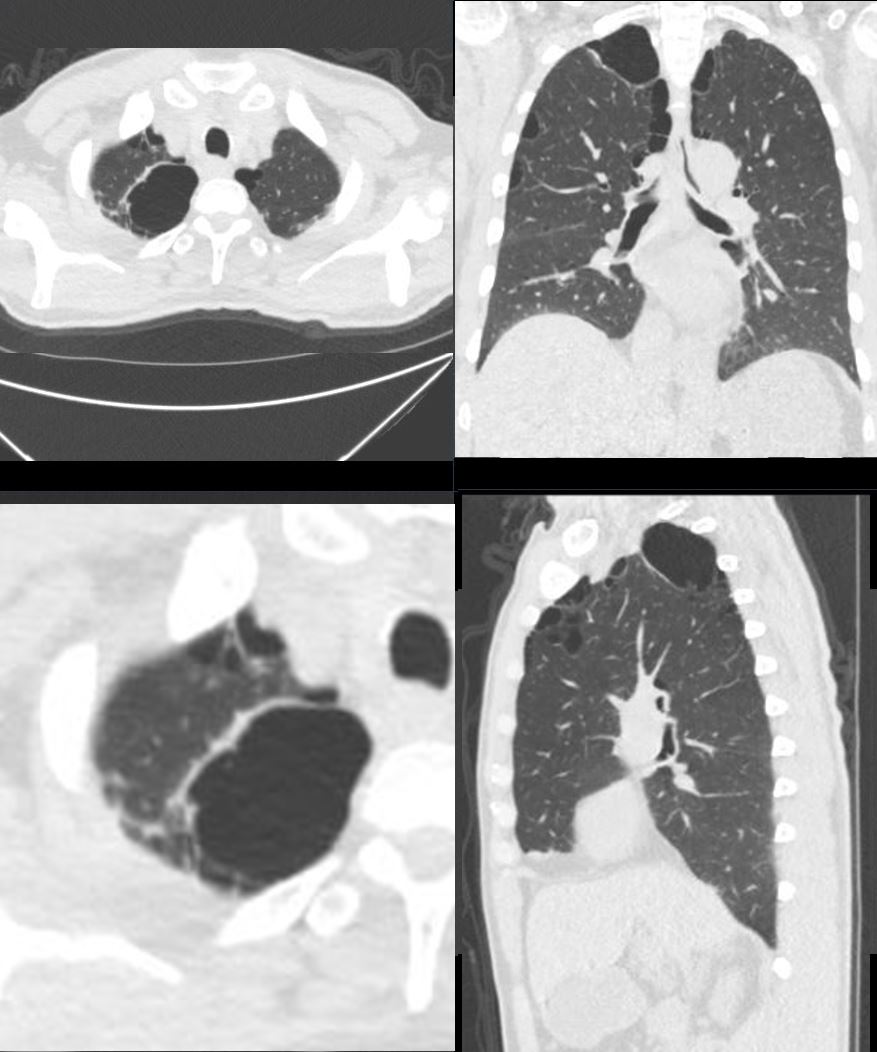
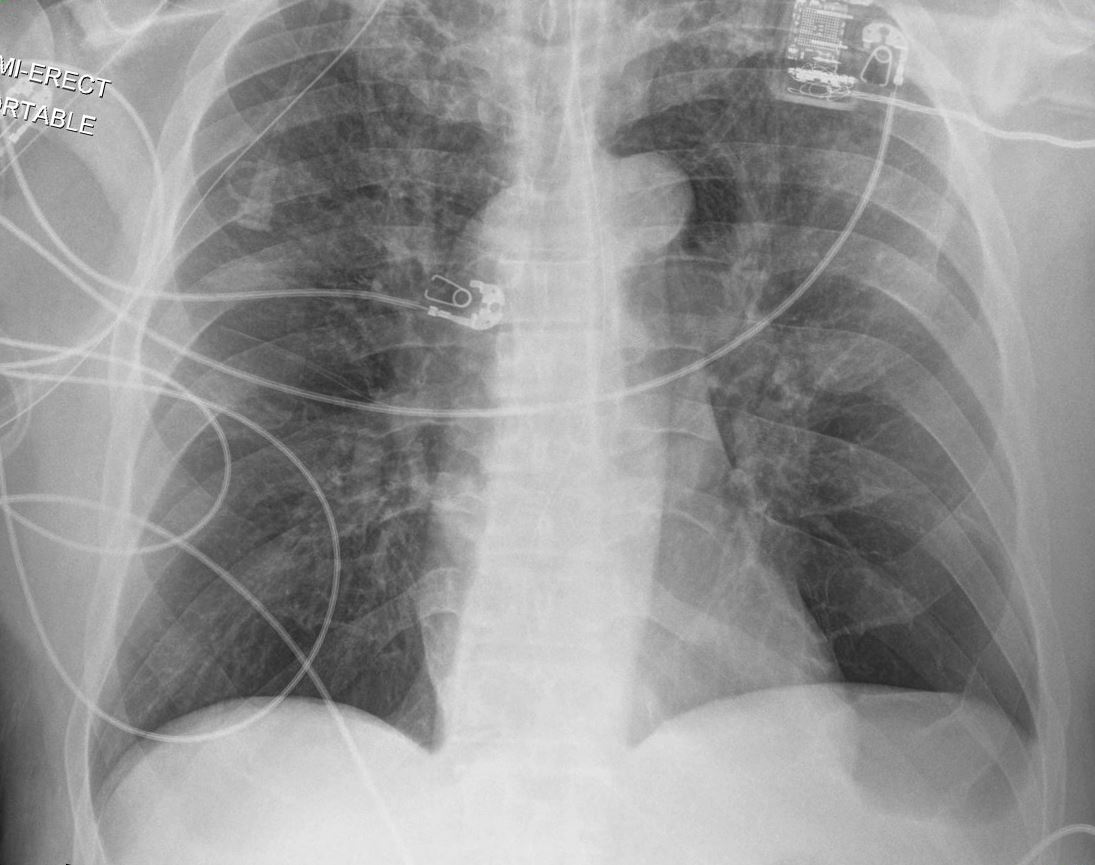
65-year-old male with emphysema of the lungs presents with a cough, fever and leukocytosis.
Frontal CXR in semi-upright position, shows a pigtail catheter in the large right apical abscess within a giant apical bulla with persistent fluid as evidenced by ground glass curtain of fluid bilaterally. Hyperinflation with resultant small heart is noted.
Ashley Davidoff MD TheCommonVein.net 259Lu 117505.8

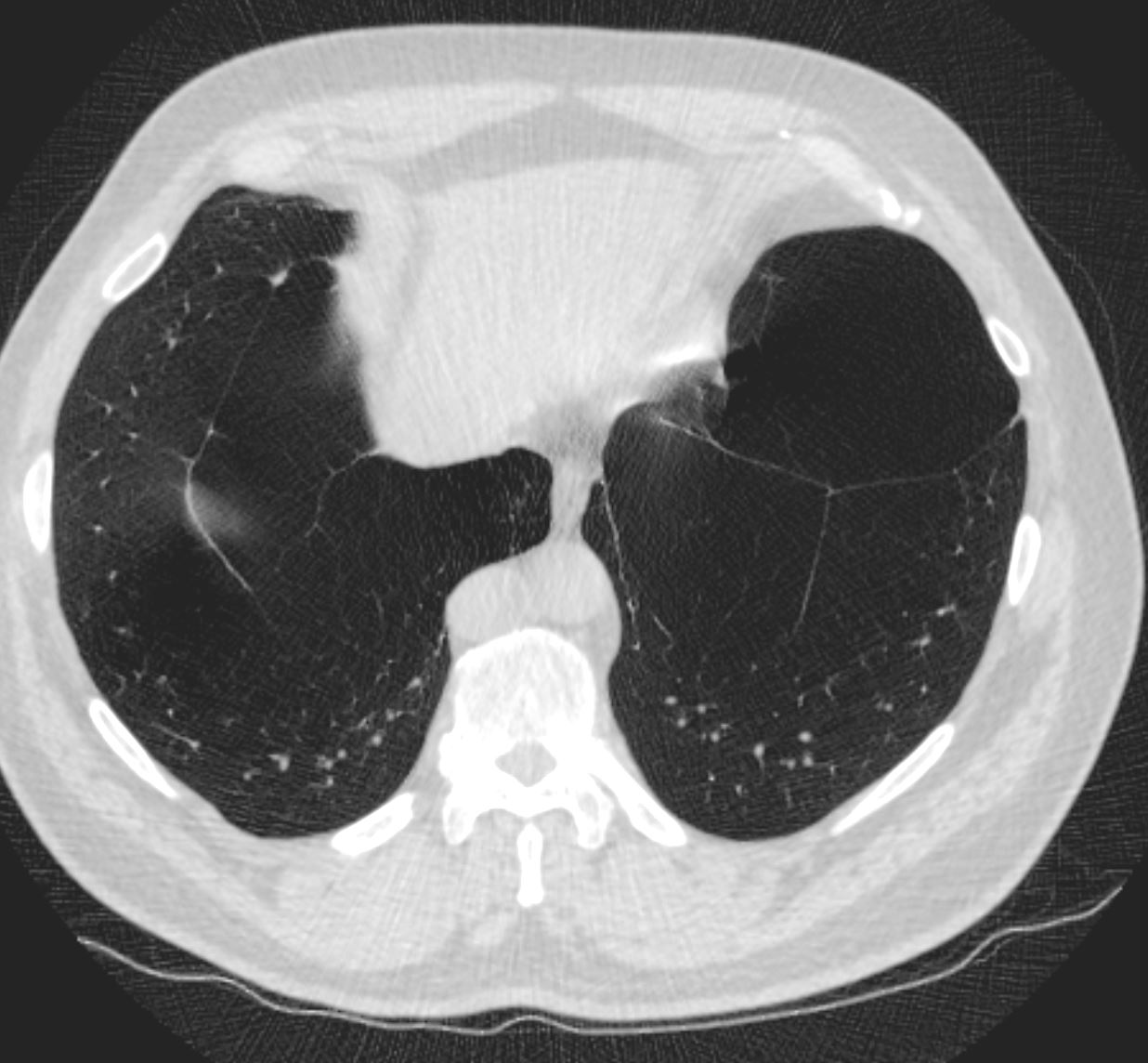
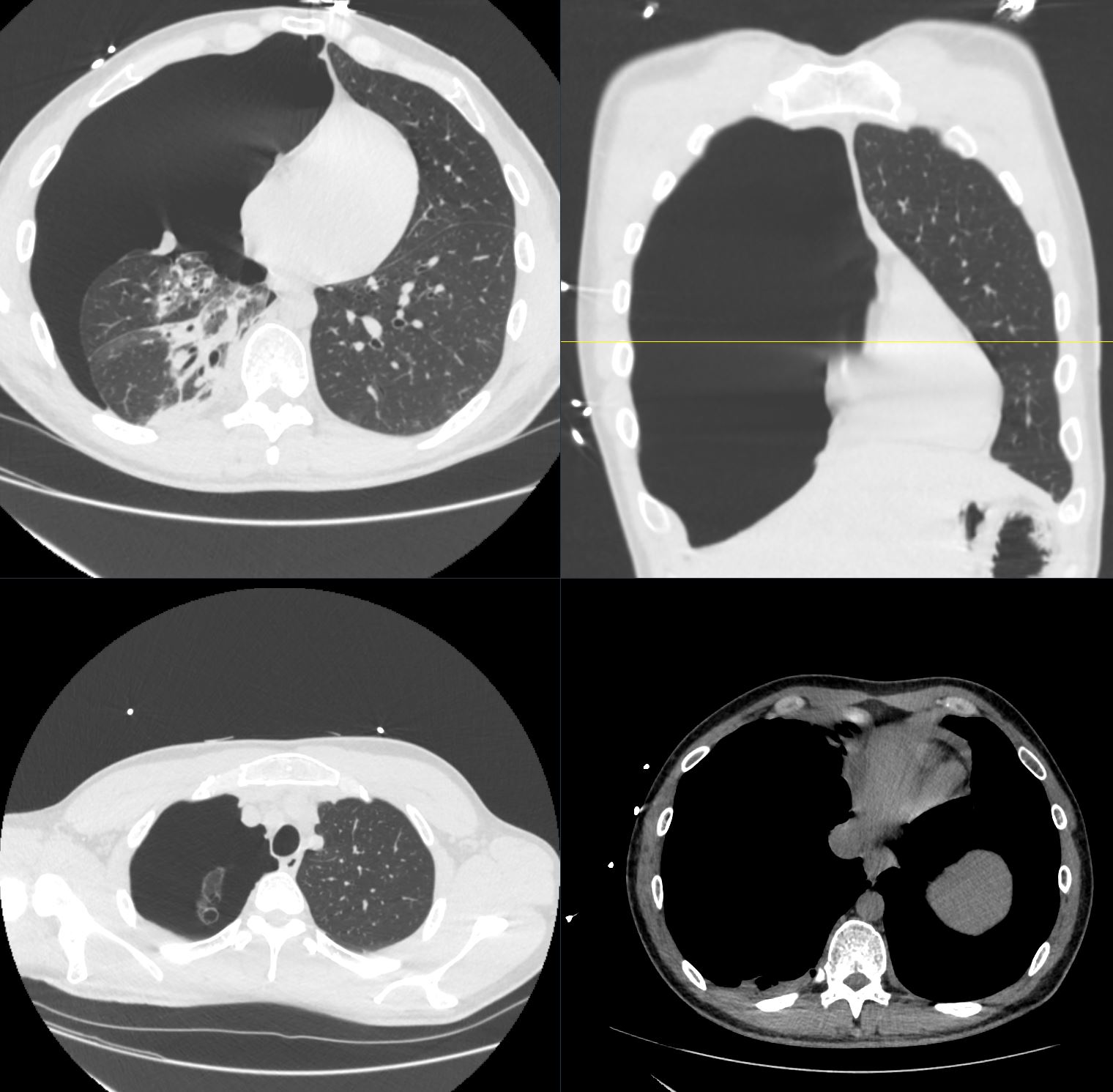
65-year-old male with emphysema of the lungs presents with a cough, fever and leukocytosis. CT in the axial plane shows extensive apical bullous lung disease. There is a large right upper lobe bulla with an air fluid level, and a smaller left upper lobe bulla with an air fluid level. The bulla in the left upper lobe, cause compressive atelectasis of a segment of the left upper lobe.
Ashley Davidoff MD TheCommonVein.net 259Lu 117474
Courtesy Maegan Lu, Jonathan Scalera, MD
CT scan shows basilar bullous lung disease, with only minimal centrilobular emphysematous changes in the upper lobes
Ashley DAvidoff MD TheCommonVein.net
61M-COPD-Bulla-base-false-neg-PTX-001b
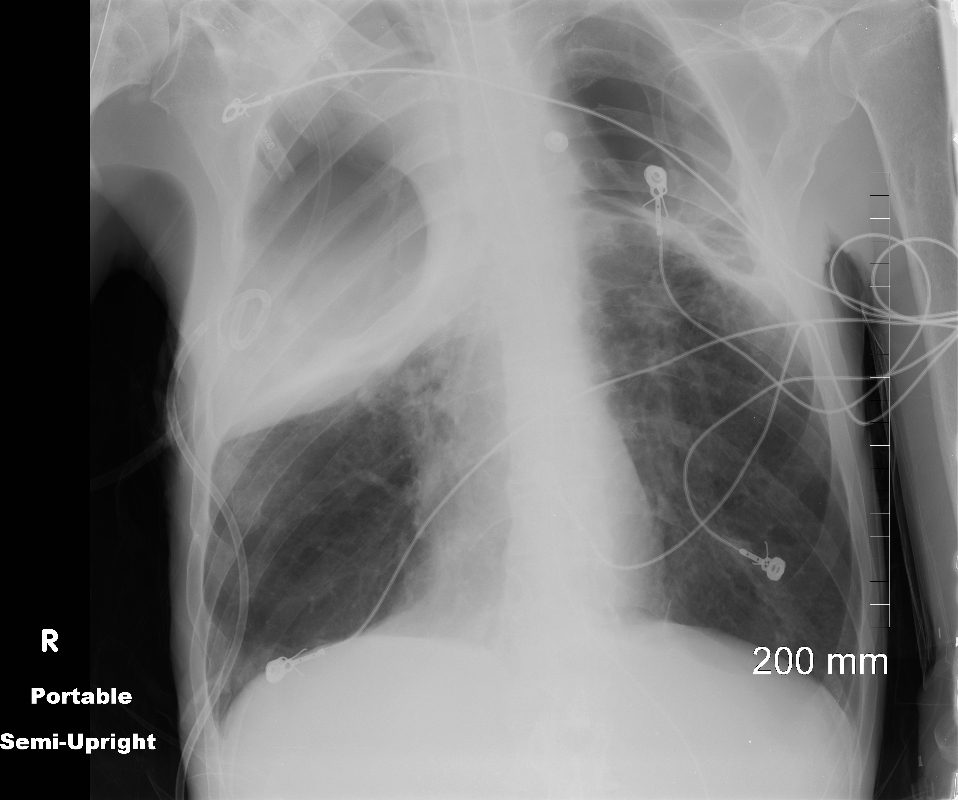
Bulla Masquerading as a Deep Sulcus Sign
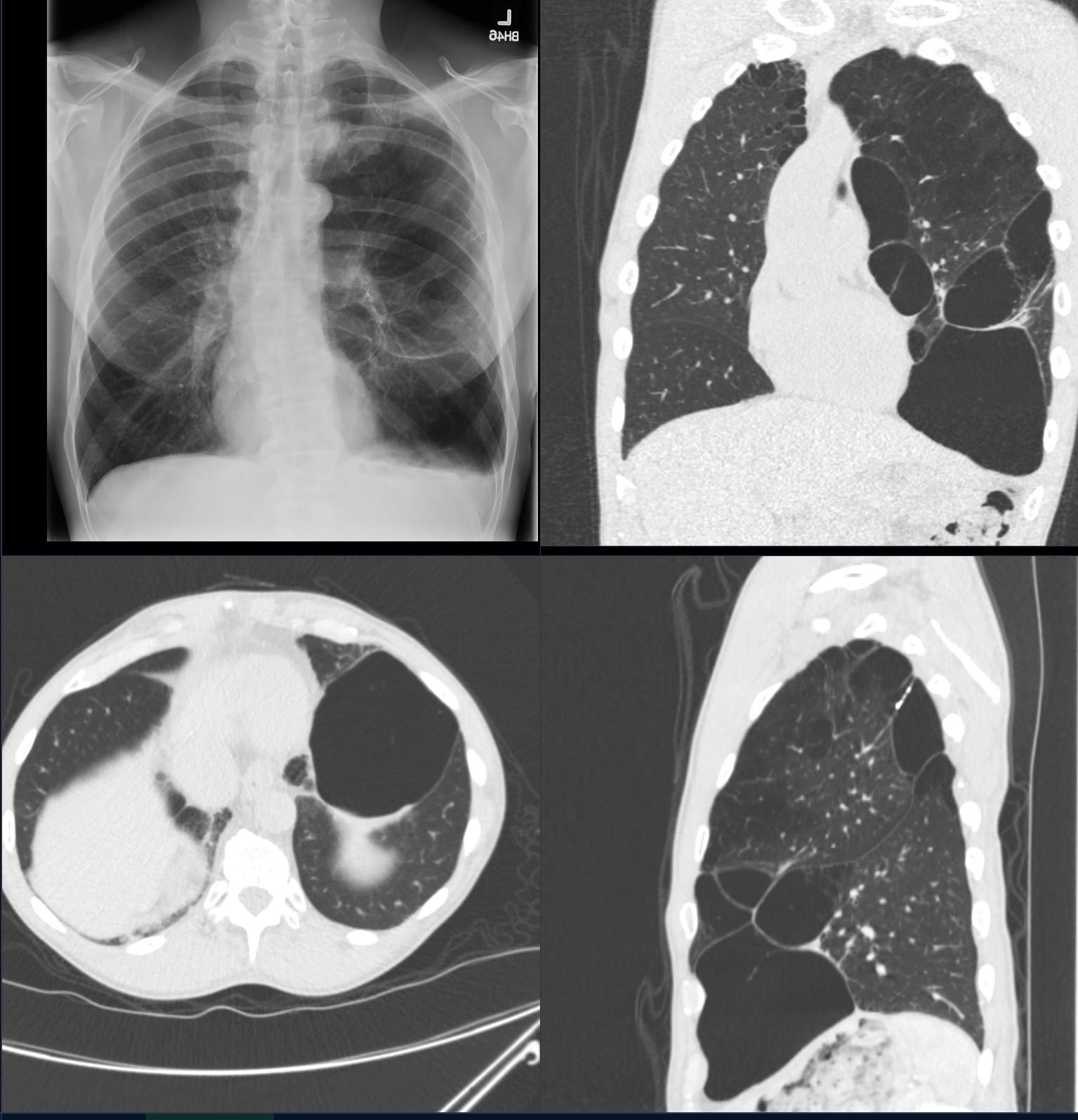
CXR top left shows a lucency at the left base with flattening of the diaphragm masquerading as a deep sulcus sign – and since this is an upright exam, could reflect a loculated pneumothorax. CT scan in the coronal, sagittal and axial planes confirm the presence of a large multiloculated bulla
Ashley Davidoff MD TheCommonVein.net b11534
Ruptured Bulla and Tension Pneumothorax
CT scan in the axial and coronal planes show a right sided tension pneumothorax caused by the rupture of an apical bulla. There is total atelectasis of the right lung compression of the right sided heart structures and leftward shift of the mediastinal structures
Ashley Davidoff MD TheCommonVein.net b11585
Radiological Features
- Chest X-Ray (CXR):
- Appearance:
- A hyperlucent, air-filled space with no visible lung markings inside.
- Thin, imperceptible walls (if visible, suggests a thicker-walled cavity).
- Typically located in the upper lobes or subpleural regions.
- Complications:
- Large bullae may mimic a pneumothorax (known as a “vanishing lung” phenomenon).
- Appearance:
- Computed Tomography (CT):
- Appearance:
- Thin-walled air-filled space (>1 cm).
- Often subpleural, but can be central or paraseptal.
- Adjacent lung parenchyma may show emphysematous changes (e.g., centrilobular emphysema).
- Size and Location:
- Variable sizes; bullae may be solitary or multiple.
- Large bullae (>5 cm) are sometimes referred to as giant bullae.
- Associated Findings:
- Evidence of adjacent parenchymal destruction or fibrosis.
- Possible compression of adjacent lung tissue or mediastinal structures in giant bullae.
- Appearance:
- Magnetic Resonance Imaging (MRI):
- Rarely used but can confirm the presence of air-filled spaces.
- Ultrasound:
- Rarely used in routine evaluation.
- May show absence of normal lung sliding if a bulla is suspected near the pleura.
Common Causes
Bullae are typically associated with conditions that result in alveolar wall destruction:
- Primary Causes:
- Emphysema:
- Centrilobular or paraseptal emphysema commonly leads to bullae formation.
- Congenital Bullae:
- Occur in rare conditions such as congenital lobar emphysema.
- Emphysema:
- Secondary Causes:
- Chronic Obstructive Pulmonary Disease (COPD):
- Strongly linked to bullae, especially in smokers.
- Infections:
- Post-tubercular or fungal infections may leave bullae as residual lesions.
- Trauma:
- Barotrauma from mechanical ventilation or blunt chest trauma.
- Fibrosis-Related Diseases:
- Paraseptal bullae near fibrotic lung tissue (e.g., in idiopathic pulmonary fibrosis).
- Chronic Obstructive Pulmonary Disease (COPD):
- Rare Associations:
- Birt-Hogg-Dubé Syndrome:
- Autosomal dominant disorder associated with bullae and spontaneous pneumothorax.
- Marfan Syndrome:
- Connective tissue disorders predisposing to bullae formation.
- Birt-Hogg-Dubé Syndrome:
Differential Diagnosis
Bullae must be distinguished from other radiological entities:
- Cysts:
- Have thicker walls and may contain fluid or solid components.
- Cavities:
- Often irregular with thicker walls, associated with necrosis or infection (e.g., tuberculosis, abscess).
- Pneumatoceles:
- Transient, thin-walled air spaces seen in trauma or infections like staphylococcal pneumonia.
- Pneumothorax:
- Hyperlucency without a wall and no visible lung markings, often with pleural line displacement.
Complications
- Spontaneous Pneumothorax:
- Rupture of a bulla can lead to air escaping into the pleural space.
- Infection:
- Superinfection of a bulla can result in an abscess or empyema.
- Respiratory Compromise:
- Large bullae can compress adjacent lung tissue, reducing functional lung capacity.
Management
- Observation:
- Small, asymptomatic bullae usually require no intervention.
- Medical Therapy:
- Smoking cessation and bronchodilators in cases of underlying COPD or emphysema.
- Surgical Treatment:
- Bullectomy:
- Indicated for symptomatic or complicated bullae (e.g., recurrent pneumothorax or compression).
- Lung Volume Reduction Surgery (LVRS):
- For giant bullae causing severe respiratory compromise.
- Bullectomy:
Clinical Relevance
- Bullae are often incidental findings on imaging but may have significant clinical implications if they rupture or cause compression.
- Identifying and distinguishing bullae from other similar-appearing lesions on imaging is critical for appropriate management.