40 y/o M with PMH of MDD, Covid PTSD, +PPD (treated), and bilateral pulmonary sequestration
Bilateral lower lobe extralobar sequestration
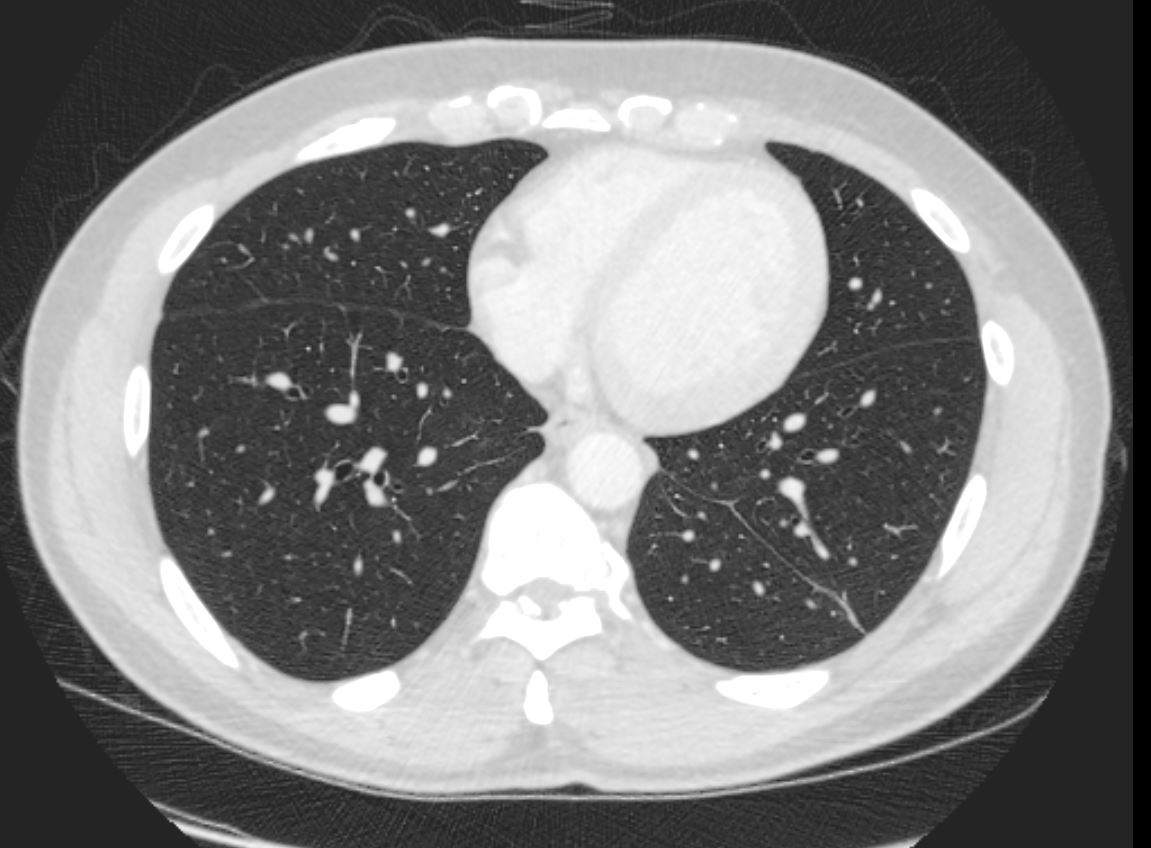
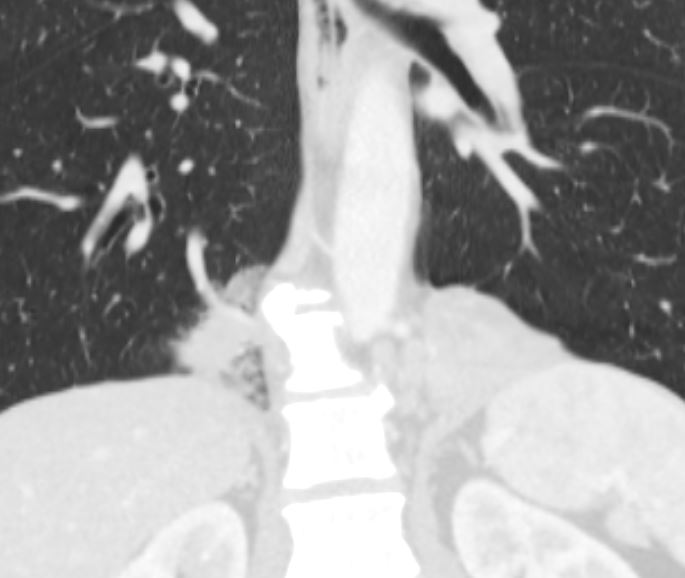
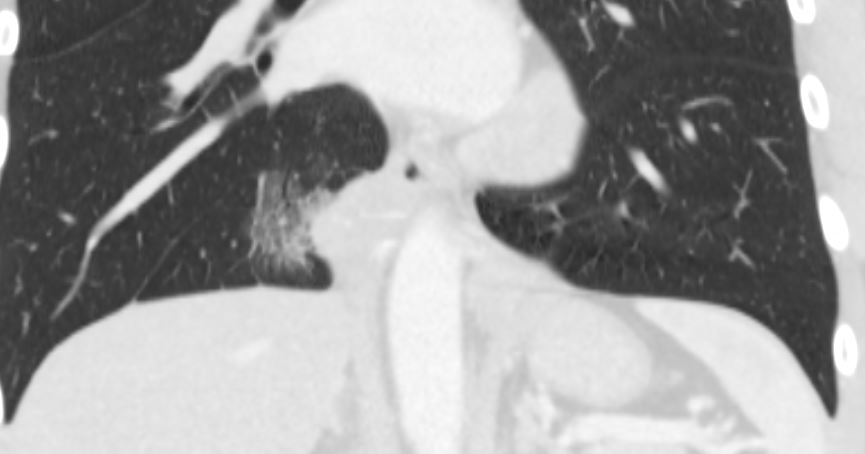
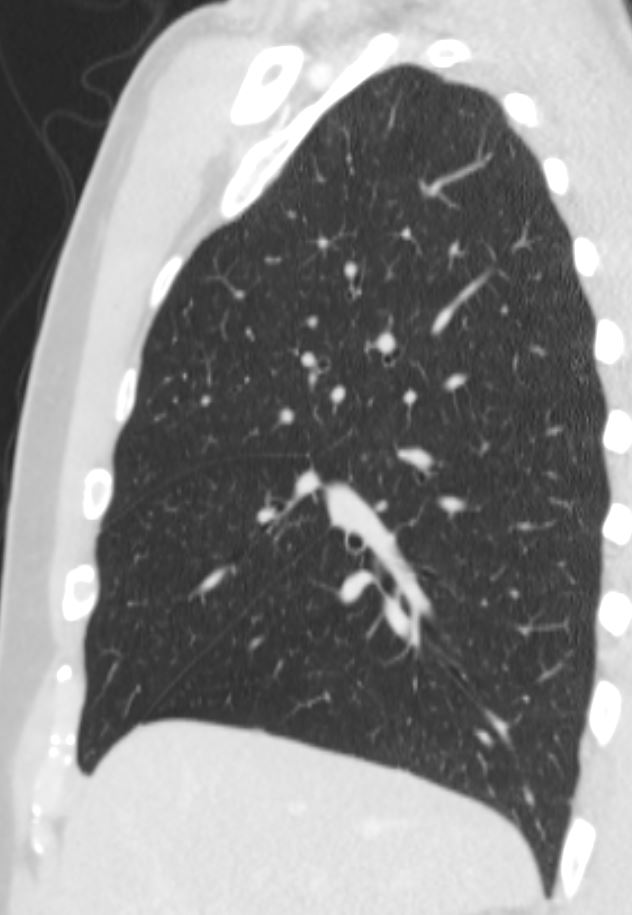
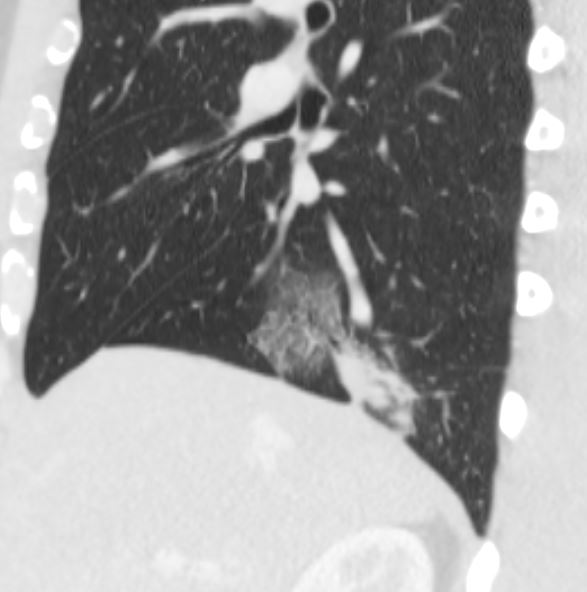
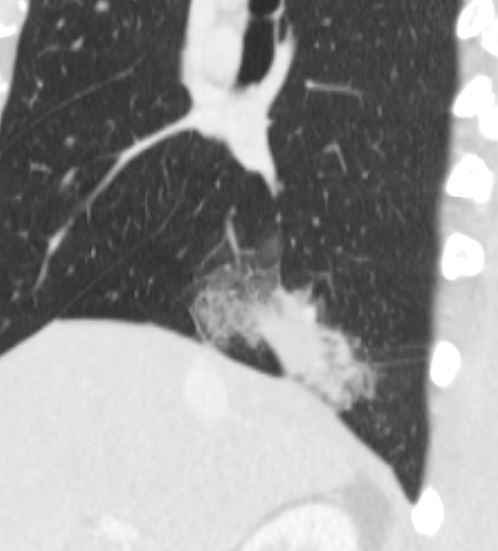
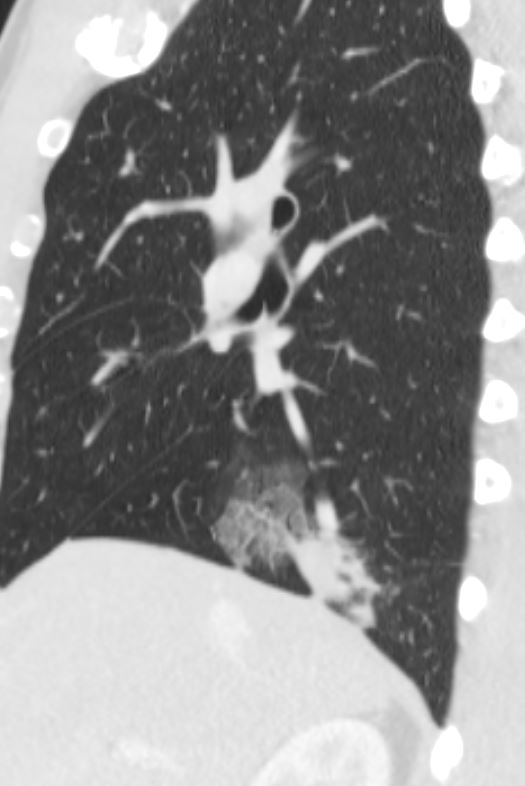
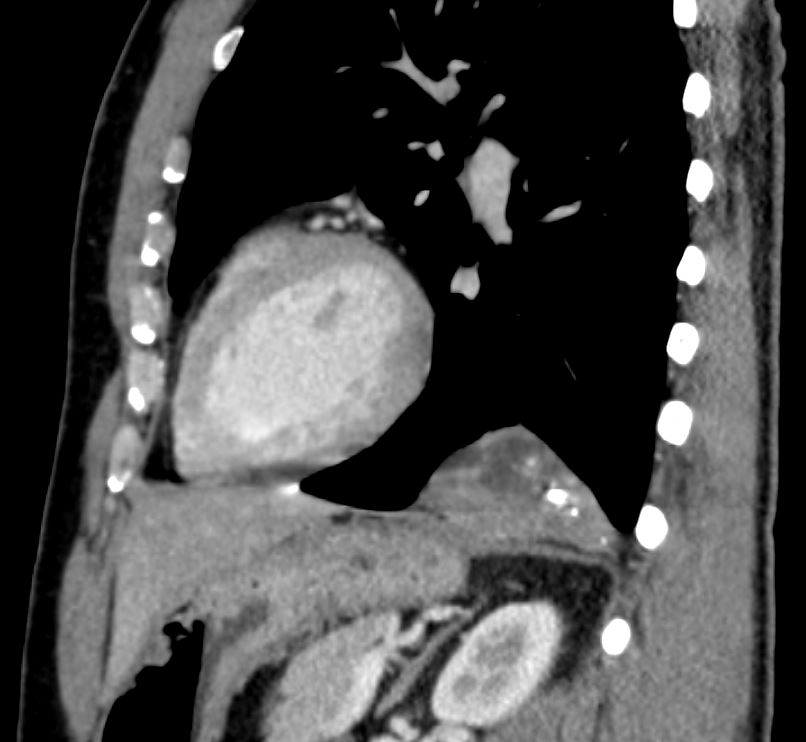
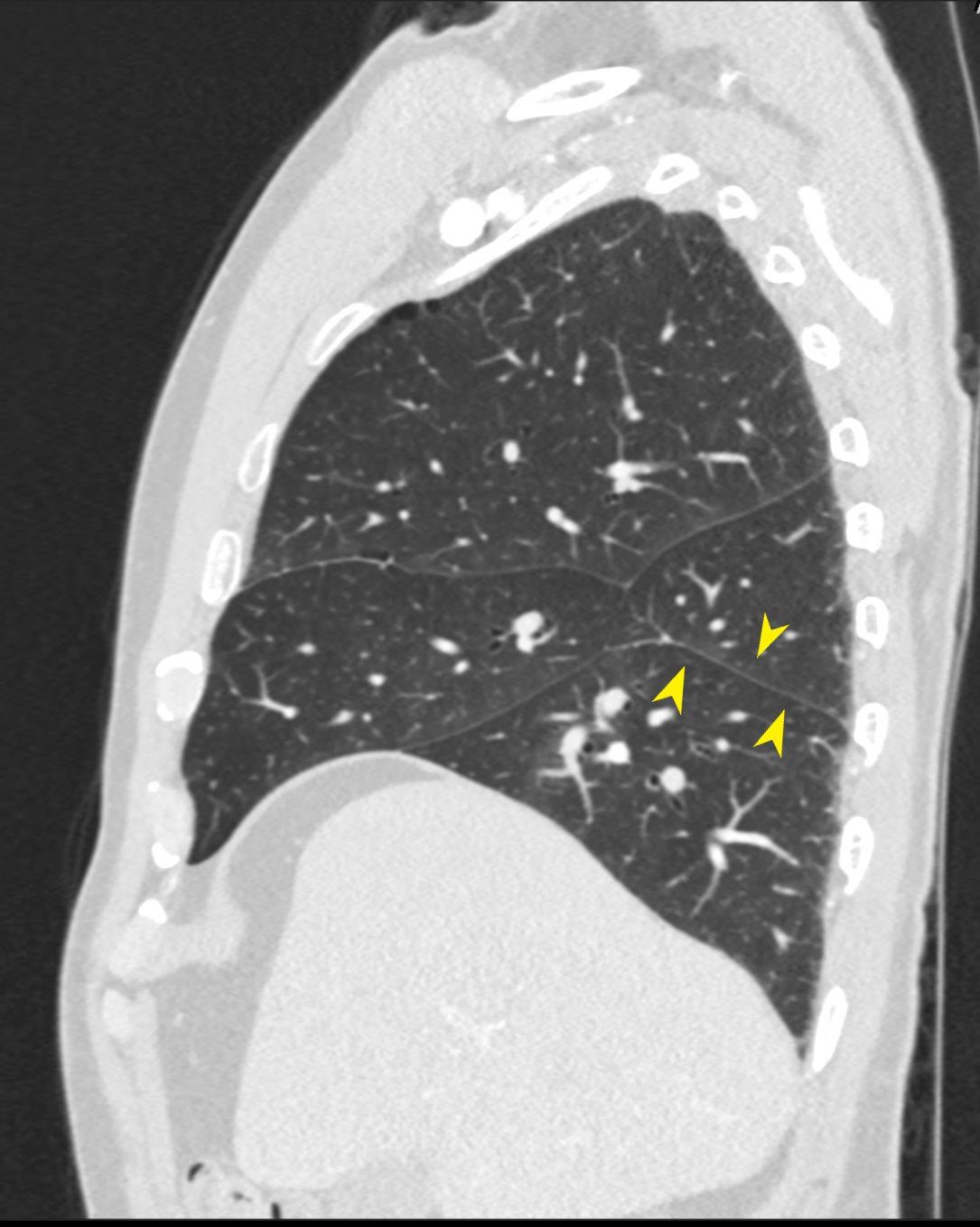
This is a 47-year-old gentleman with a diagnosis of a lung sequestration for which he has had what appears to be recurrent pneumonia, mostly on the left side. On the CAT scan, there is a collapsed portion of the left lower lobe that is receiving its blood supply from the descending aorta.

CXR from 14 years ago shows an ovoid retro cardiac soft tissue density abutting the diaphragm in the left lower lobe
Ashley Davidoff TheCommonVein.net 139147 111Lu

CXR from 14 years ago shows an ovoid retro cardiac soft tissue density abutting the diaphragm in the left lower lobe
Ashley Davidoff TheCommonVein.net 139148 111Lu

Scout films of the CT scan shows similar ovoid retro cardiac soft tissue density abutting the diaphragm in the left lower lobe
Ashley Davidoff TheCommonVein.net 139149 111Lu
Ashley Davidoff TheCommonVein.net 139153 111Lu

Ashley Davidoff TheCommonVein.net 139154 111Lu

Ashley Davidoff TheCommonVein.net 139155 111Lu
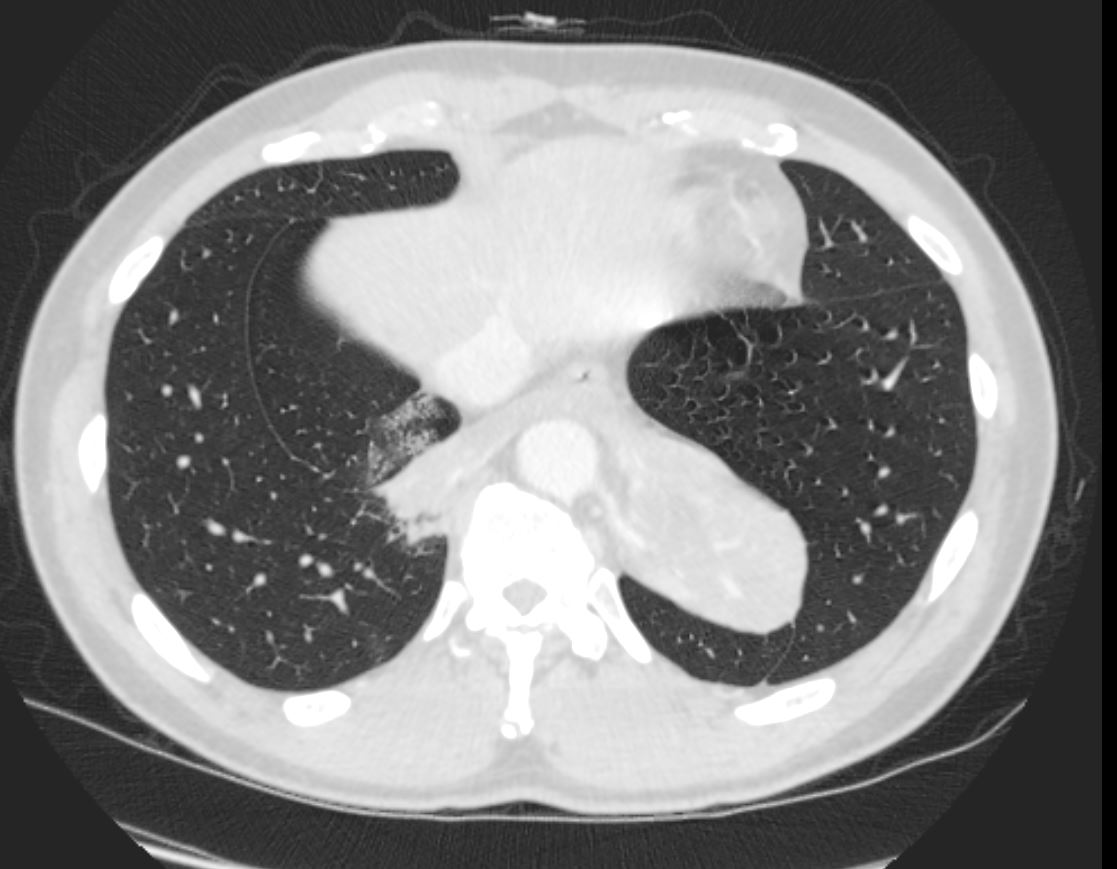
Axial CT scan through the lower chest shows 2 fissures in the left lung. The normal oblique fissure is seen anteriorly and the fissure/pleura posteriorly noted as a component of the extralobar sequestration.
Ashley Davidoff TheCommonVein.net
139150 111Lu
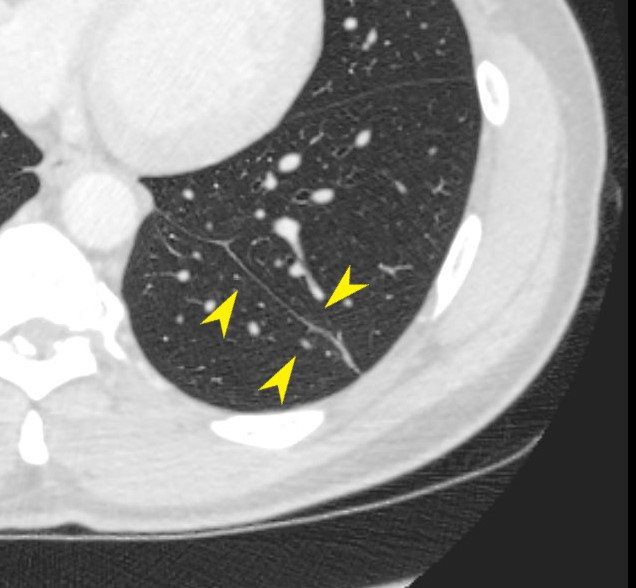
Axial CT scan through the lower chest shows 2 fissures in the left lung. The normal oblique fissure is seen anteriorly and the fissure/pleura posteriorly noted as a component of the extralobar sequestration.
Ashley Davidoff TheCommonVein.net
139152 111Lu

CT scan shows ovoid left retro cardiac consolidation with arterial supply from the aorta and a second branch originating from the left side of the aorta and crossing the midline to supply the right sided smaller sequestration.
Ashley Davidoff TheCommonVein.net 139156 111Lu

Ashley Davidoff TheCommonVein.net 139157 111Lu

Ashley Davidoff TheCommonVein.net 139158 111Lu

Ashley Davidoff TheCommonVein.net 139150 111Lu

Ashley Davidoff TheCommonVein.net 139160 111Lu

Ashley Davidoff TheCommonVein.net 139160 111Lu

Ashley Davidoff TheCommonVein.net 139160 111Lu


Ashley Davidoff TheCommonVein.net 139166 111Lu



Ashley Davidoff TheCommonVein.net 139174 111Lu
CT Scan
PAth
LEFT LOWER LOBE SEGMENT, LUNG
Final Diagnosis
LEFT LOWER LOBE SEGMENT, LUNG
able to identify the abnormal part of the left lower lobe. This was obvious rather than a left lower lobe lobectomy we decided to simply remove this abnormal part of the lung as the rest of the left lower lobe appeared normal. There was some soft adhesions that were taken down with electrocautery. This abnormal part of the left lower lobe was densely adherent to the surrounding structures including the diaphragm and the descending aorta. The adhesions to the diaphragm was taken down with electrocautery. We then worked along the descending aorta. There was some adherent split thickness tissues in which we knew there would be a small branch coming off of the descending aorta. We were able to get around this and divided this entire tissue, likely included the branch off of the ascending aorta with a vascular stapler.
The specimen consists of a lobectomy specimen consisting of left lower lobe of lung measuring 9.0 x 6.5 x 3.5 cm and weighing 92.2 grams with a 5 cm staple line. A bronchial stump margin is identified measuring 0.8 cm in diameter. The visceral pleura
are tan-pink, smooth, and glistening. The specimen is sectioned to reveal a tan-white and not aerated lung parenchyma with focal hemorrhage. The main bronchus is filled with tan white viscous material. No additional masses are seen. No peribronchial
lymph nodes are identified.
Lung with bronchopneumonia in the background of chronic interstitial fibrosis. excision demonstrates patchy intra-alveolar fibrinopurulent exudate with predominant neutrophil in a background of relatively uniform alveolar septal thickening with marked fibrosis, interstitial chronic inflammation and occasional
clusters of foreign body multinucleated giant cells. No increased eosinophils, vasculitis, or granulomas is seen.
Discussion
Bilateral sequetrations
- Most intralobar PS are unilateral, and
- bilateral PS are very rare.
- PS was first described by
- Rokitanski and Rektorzik in 1861,
- 1946 when Pryce2 made it known as a clinical entity.
- 1972, Felson et al.
- reported a case of bilateral PS confirmed by pathological
- 1977, Karp et al. described another case in a 13-year-old girl
- PS was first described by
