Etymology:
The term “Batwing Pattern” refers to the characteristic appearance of bilateral perihilar opacities on a chest X-ray, resembling the shape of a bat’s wings.
Also Known As (AKA):
Butterfly pattern, angel wing pattern.
What is it?
The Batwing Pattern is a radiographic sign typically indicative of pulmonary edema, where fluid accumulates in the lung interstitium and alveoli, leading to characteristic imaging findings.
Characterized by:
Bilateral, symmetrical perihilar opacities that extend outward from the hilum, often sparing the peripheral lung fields. This pattern is most commonly associated with cardiogenic pulmonary edema.[1-3]
Anatomically Affecting:
Primarily affects the perihilar regions of the lungs, extending to the central alveolar spaces.
Pathophysiology:
Pulmonary edema results from increased hydrostatic pressure in the pulmonary capillaries, leading to fluid leakage into the interstitial and alveolar spaces. This can be due to left-sided heart failure, fluid overload, or increased capillary permeability.[1-3]
Causes:
? Most Common Causes:
Cardiogenic pulmonary edema due to left-sided heart failure.[1-3]
? Other Causes:
? Infection:
Severe pneumonia leading to non-cardiogenic pulmonary edema.[1]
? Inflammation:
Acute respiratory distress syndrome (ARDS).[1-2]
? Neoplasm:
Lymphangitic spread of carcinoma.[2]
? Mechanical Trauma:
Post-obstructive pulmonary edema following upper airway obstruction.[1]
? Metabolic:
Uremic pulmonary edema.[1]
? Circulatory:
Pulmonary veno-occlusive disease.[1]
? Immune:
Autoimmune diseases causing capillary leak syndrome.[1]
? Infiltrative:
Sarcoidosis with pulmonary involvement.[1]
? Iatrogenic:
Fluid overload from excessive intravenous fluids.[1]
? Idiopathic:
Idiopathic pulmonary fibrosis with acute exacerbation.[1]
Histopathology:
Histopathological findings in pulmonary edema include alveolar flooding with proteinaceous fluid, interstitial edema, and the presence of hemosiderin-laden macrophages in chronic cases.[1-2]
Imaging Radiology:
? Applied Anatomy to CT:
? Parts: Perihilar regions, central alveolar spaces.
? Size: Variable, depending on the extent of edema.
? Shape: Bilateral, symmetrical opacities resembling bat wings.
? Position: Central, perihilar distribution.
? Character: Ground-glass opacities, interstitial thickening, and alveolar consolidation.[1-3]
? Time: Acute or subacute presentation.
? CXR:
Bilateral perihilar opacities with sparing of the peripheral lung fields.[1]
? MRI:
Less commonly used but can assess fluid distribution and cardiac function.[1]
? Other:
Lung ultrasound can show B-lines indicative of interstitial fluid.[6]
Labs:
Blood tests for cardiac biomarkers (e.g., BNP), renal function, and inflammatory markers.[1]
Pulmonary Function Tests (PFTs):
Typically not useful in the acute setting of pulmonary edema but may show restrictive patterns in chronic cases.[1]
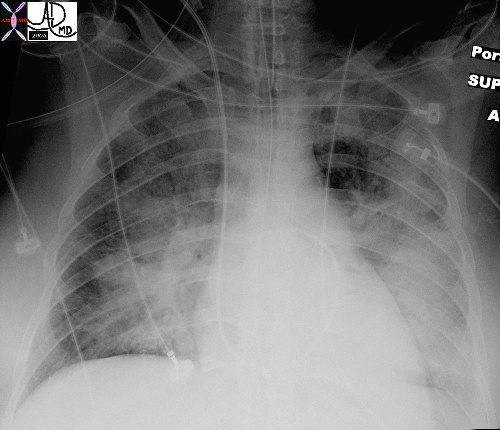
In this patient with acute congestive cardiac failure the consolidation that has hilar distribution has reminded radiologists of bat wings and butterfly wings and is caused by alveolar edema. As a result of the fluid in the alveoli, gas exchange across the respiratory membrane is reduced resulting in a decrease in oxygen saturation, and thus requiring intubation to improve the gas exchange process. Note the endotracheal tube as well as the central venous line that is used to assess the heart pressure and monitor the congestion.
Ashley Davidoff MDTheCommonVein.net 42073b01
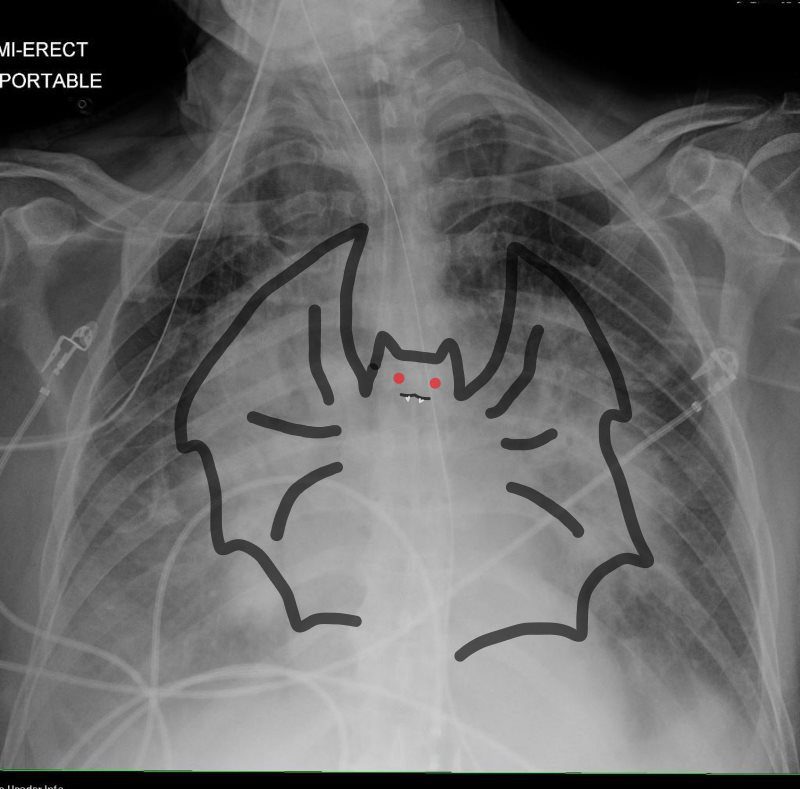
In this patient with acute congestive cardiac failure the consolidation that has hilar distribution has reminded radiologists of bat wings and is caused by alveolar edema. As a result of the fluid in the alveoli, gas exchange across the respiratory membrane is reduced and required intubation to improve the gas exchange process. Note the endotracheal tube as well as the central venous line that is used to assess the heart pressure and monitor the congestion.
Ashley Davidoff MD
TheCommonVein.net 42073b01
Memory Image Neelou Etesami MS4 PhD
References
- Clinical and Radiologic Features of Pulmonary Edema. Gluecker T, Capasso P, Schnyder P, et al. Radiographics : A Review Publication of the Radiological Society of North America, Inc. 1999 Nov-Dec;19(6):1507-31; discussion 1532-3. doi:10.1148/radiographics.19.6.g99no211507.
- CT Signs and Patterns of Lung Disease. Collins J. Radiologic Clinics of North America. 2001;39(6):1115-35. doi:10.1016/s0033-8389(05)70334-1.
- Radiographic Features of Cardiogenic Pulmonary Oedema in Cats With Left-Sided Cardiac Disease: 71 Cases. Diana A, Perfetti S, Valente C, et al Journal of Feline Medicine and Surgery. 2022;24(12):e568-e579.
- Chest CT Signs in Pulmonary Disease: A Pictorial Review. Raju S, Ghosh S, Mehta AC. 2017;151(6):1356-1374. doi:10.1016/j.chest.2016.12.033.
- Hydrostatic Pulmonary Edema: Evaluation With Thin-Section CT in Dogs. Scillia P, Delcroix M, Lejeune P, et al. 1999;211(1):161-8. doi:10.1148/radiology.211.1.r99ap07161.
- Ultrasound of Extravascular Lung Water: A New Standard for Pulmonary Congestion., Picano E, Pellikka PA. European Heart Journal. 2016;37(27):2097-104. doi:10.1093/eurheartj/ehw1647.Diseases Involving the Lung Peribronchovascular Region: A CT Imaging Pathologic Classification. Le L, Narula N, Zhou F, et al 2024;166(4):802-820. doi:10.1016/j.chest.2024.05.033.
- Lung Morphology and Surfactant Function in Cardiogenic Pulmonary Edema: A Narrative Review. Nugent K, Dobbe L, Rahman R, Elmassry M, Paz P. Journal of Thoracic Disease. 2019;11(9):4031-4038. doi:10.21037/jtd.2019.09.02.
- .Radiographic Appearance of Presumed Noncardiogenic Pulmonary Edema and Correlation With the Underlying Cause in Dogs and Cats. Bouyssou S, Specchi S, Desquilbet L, Pey P. Veterinary Radiology & Ultrasound : The Official Journal of the American College of Veterinary Radiology and the International Veterinary Radiology Association. 2017;58(3):259-265. doi:10.1111/vru.12468.
- CT Approach to Lung Injury. Marquis KM, Hammer MM, Steinbrecher K, et al. Radiographics : A Review Publication of the Radiological Society of North America, Inc. 2023;43(7):e220176. doi:10.1148/rg.220176.
- Idiopathic Pulmonary Fibrosis (An Update) and Progressive Pulmonary Fibrosis in Adults: An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Raghu G, Remy-Jardin M, Richeldi L, et al. American Journal of Respiratory and Critical Care Medicine. 2022;205(9):e18-e47. doi:10.1164/rccm.202202-0399ST.
- Diagnosis and Evaluation of Hypersensitivity Pneumonitis: CHEST Guideline and Expert Panel Report. Fernández Pérez ER, Travis WD, Lynch DA, et al. 2021;160(2):e97-e156. doi:10.1016/j.chest.2021.03.066.
