Etymology
- The term “tracheobronchial” is derived from the Greek words “trachea” (rough) and “bronchos” (windpipe), reflecting the structure?s function as a conduit for air to and from the lungs.
AKA
- Airway tree
What is it?
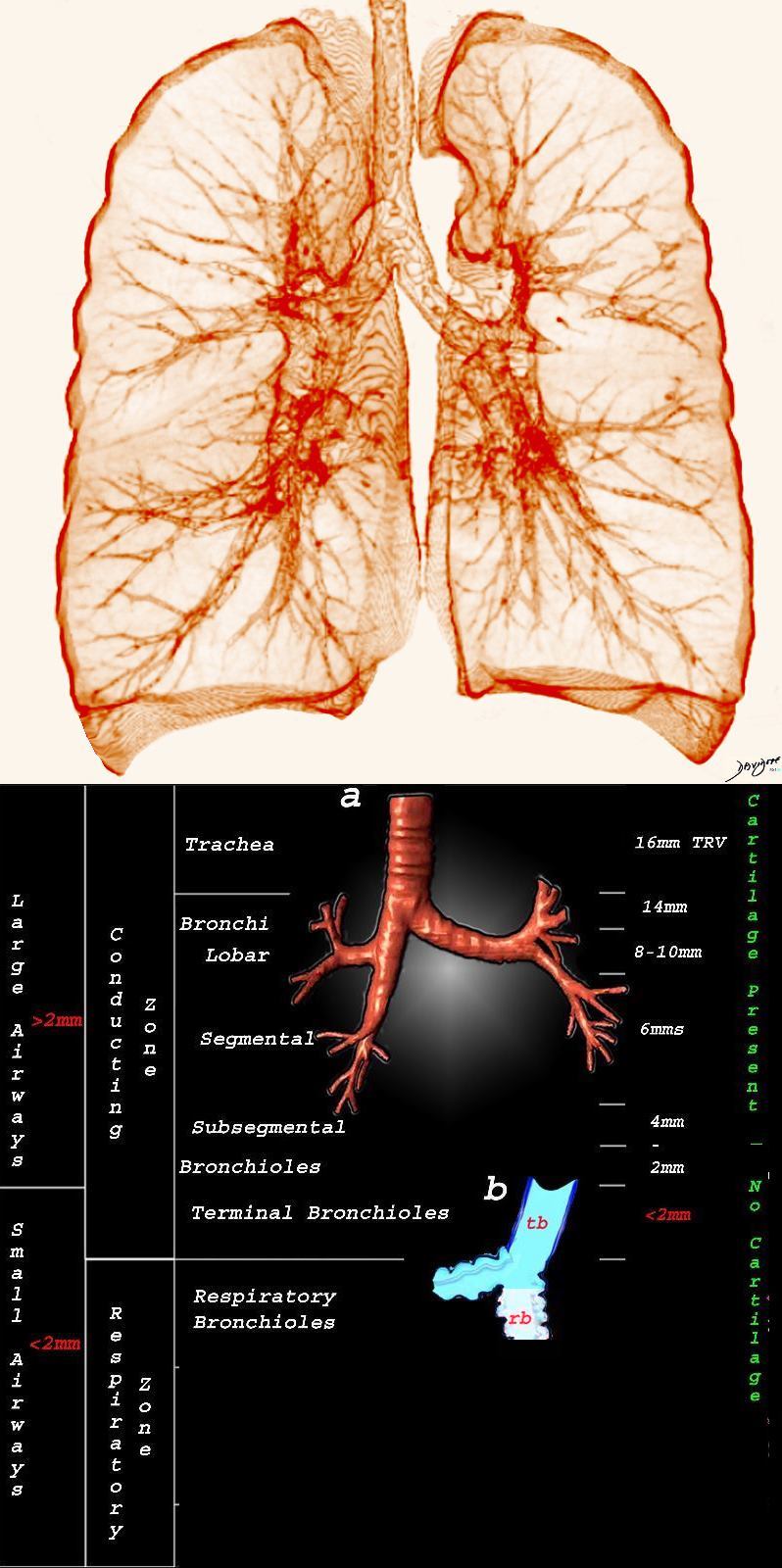
- The tracheobronchial tree is the branching system of airways that extends from the trachea to the terminal bronchioles, facilitating the transport of air into the alveoli for gas exchange.
- It is a hierarchical structure comprising progressively smaller airways.
Classified as
- Conducting zone (trachea to terminal bronchioles).
- Respiratory zone (respiratory bronchioles to alveoli).
Parts
- Trachea:
- Approximately 10?12 cm long and 2?2.5 cm in diameter.
- Supported by C-shaped cartilaginous rings.
- Main bronchi:
- Right main bronchus is wider, shorter, and more vertical.
- Left main bronchus is longer and more horizontal.
- Lobar bronchi:
- Three on the right, two on the left.
- Segmental bronchi:
- Each supplies a bronchopulmonary segment.
- Smaller bronchi and bronchioles:
- Bronchioles lack cartilage and submucosal glands.
- Terminal bronchioles mark the end of the conducting zone.
- Respiratory bronchioles:
- Transition to alveolar ducts and sacs.
Size and Shape
- Size:
- Trachea: ~2?2.5 cm in diameter.
- Bronchi decrease progressively in size, with bronchioles <2 mm in diameter.
- Normal bronchus-to-artery ratio is approximately 1:1 in the central airways and 0.8:1 in the peripheral airways.
- Abnormal thickening of the wall – For objective measurement, wall thickness greater than 3 mm in large airways or exceeding 20% of the airway?s total diameter in smaller airways may be considered abnormal. Associated findings, such as peribronchial cuffing, can provide additional evidence of pathology.
- Shape:
- Tubular with smooth muscle and elastic fibers.
Position
- Extends from the cricoid cartilage in the neck to the alveoli within the lungs.
- Right main bronchus is more vertical and prone to foreign body aspiration.
Character
- The bronchial walls demonstrate an elastic and muscular character, which contributes to their ability to change diameter with inspiration and expiration. Larger bronchi maintain a fixed structure due to cartilage, while smaller bronchioles are collapsible during expiration, particularly in diseased states.
- Cartilage, smooth muscle, and elastic fibers provide structural support and flexibility.
Blood Supply
- Arterial:
- Bronchial arteries (from thoracic aorta).
- Pulmonary arteries supply distal regions.
- Venous Drainage:
- Bronchial veins drain into the azygos and hemiazygos systems.
- Pulmonary veins return oxygenated blood to the heart.
Lymphatic Drainage
- Drains to hilar, mediastinal, and paratracheal lymph nodes.
- Rich network of lymphatics ensures immune surveillance.
Nerve Supply
- Parasympathetic: Vagus nerve (bronchoconstriction, mucus secretion).
- Sympathetic: From thoracic sympathetic trunk (bronchodilation, reduced mucus secretion).
- Sensory: Afferent fibers from the vagus nerve.
Embryology
- Derived from the foregut endoderm.
- Begins as the respiratory diverticulum (~4th week of gestation).
- Branching morphogenesis creates the complex airway tree.
Histology
- The airways are lined with pseudostratified ciliated columnar epithelium, transitioning to cuboidal epithelium in smaller bronchioles.
- Epithelium: Pseudostratified ciliated columnar with goblet cells.
- Submucosa: Contains glands and connective tissue.
- Muscularis: Smooth muscle encircling the airways.
- Cartilage: Provides structural integrity in larger airways.
Physiology and Pathophysiology
- Physiology:
- Conducting airways transport air without gas exchange.
- Mucociliary clearance protects against infection.
- Pathophysiology:
- Obstruction (e.g., asthma, COPD).
- Infection (e.g., bronchitis, pneumonia, bronchopneumonia). These infections can lead to increased mucus production, which may obstruct the airways and impair gas exchange. Bronchopneumonia specifically involves patchy inflammation and consolidation centered around the bronchioles, which can lead to small airway obstruction. Excessive mucus is a hallmark of many inflammatory airway conditions, often resulting in cough and sputum production.
- Structural damage (e.g., bronchiectasis).
- Spastic Nature The spastic nature of the airways in asthma leads to bronchoconstriction, often resulting in wheezing?a hallmark symptom of asthma.
Applied Anatomy to Radiology
CXR
- Visible trachea and main bronchi.
- Displacement can indicate mediastinal shift, atelectasis, or mass effect.
- Airway narrowing suggests stenosis, obstruction, or extrinsic compression.
- Hyperinflation and increased bronchovascular markings may suggest chronic airway disease.
- The presence of air bronchograms can be seen in both atelectasis and consolidation. In consolidation, air bronchograms are visible when air-filled bronchi are surrounded by alveoli filled with fluid. In atelectasis, air bronchograms may also be present, but the bronchi become crowded together, and their angles become more acute due to the collapse of adjacent lung tissue.
CT
- Provides detailed visualization of airway lumen, wall, and surrounding structures.
- Trachea: Detects stenosis, tracheomalacia, or tracheal tumors.
- Main Bronchi: Assesses narrowing due to extrinsic compression, wall thickening, or masses.
- Segmental and Subsegmental Bronchi:
Abnormal thickening of the wall – For objective measurement, wall thickness greater than 3 mm in large airways or exceeding 20% of the airway?s total diameter in smaller airways may be considered abnormal. Associated findings, such as peribronchial cuffing, can provide additional evidence of pathology. - Identifies tree-in-bud opacities, mucus plugging, or airway collapse.
- The presence of air bronchograms can be seen in both atelectasis and consolidation. In consolidation, air bronchograms are visible when air-filled bronchi are surrounded by alveoli filled with fluid. In atelectasis, air bronchograms may also be present, but the bronchi become crowded together, and their angles become more acute due to the collapse of adjacent lung tissue. In CT what criteria do you use
- Expiratory CT is critical for evaluating air trapping in small airway diseases.
- Quantitative CT can assess airway remodeling and emphysema severity.
MRI
- Rarely used but helpful in cases of vascular airway compression, such as tracheal narrowing due to vascular rings or masses.
- Can provide soft tissue contrast for tumor assessment.
PET-CT
- Useful for detecting hypermetabolic activity in malignancies or inflammatory processes.
- Differentiates active disease from fibrotic or post-treatment changes.
- Highlights areas of increased glucose uptake, correlating with inflammatory or neoplastic processes.
Other
- Fluoroscopy: Dynamic studies can detect tracheomalacia or airway collapse during forced expiration.
- Ultrasound: Limited to evaluating pleural-based abnormalities or guiding biopsies.
Labs
- PFTs:
- Obstructive Patterns: Reduced FEV1/FVC ratio, indicative of diseases like asthma or COPD.
- Restrictive Patterns: Reduced total lung capacity (TLC) in cases involving fibrosis or structural abnormalities.
- Mixed Patterns: Features of both obstruction and restriction in advanced or complex cases.
- Air trapping and hyperinflation can be identified on plethysmography.
Pathological Implications
- Infections: Bronchitis, pneumonia.
- Obstructions: Tumors, foreign bodies.
- Inflammatory conditions: Asthma, COPD.
- Structural abnormalities: Tracheomalacia, bronchiectasis.
Key Points and Pearls
- The tracheobronchial tree is essential for air conduction and mucociliary clearance.
- Right main bronchus anatomy predisposes it to aspiration.
- Radiological evaluation is crucial for diagnosing structural and functional abnormalities.
-
Branching patterns in nature, including the tracheobronchial tree, are governed by principles of optimization and efficiency. The asymmetrical branching of the tracheobronchial tree arises from functional and anatomical considerations, such as accommodating the heart’s position on the left side and optimizing airflow to the three lobes of the right lung and two lobes of the left lung. These patterns are shaped by physical and biological constraints to maximize function while minimizing energy expenditure.
Key aspects include:
- Fractal Geometry:
- The tracheobronchial tree follows fractal principles, with self-similar branching structures that ensure efficient air distribution. This geometry allows for an exponential increase in surface area as the airways divide, supporting effective gas exchange.
- Murray?s Law:
- This law states that the radii of parent and daughter branches are optimized to minimize energy loss in fluid transport. In the airway tree, the sum of the cubed radii of daughter branches equals the cubed radius of the parent branch.
- Space-Filling Design:
- Branching patterns are designed to fill three-dimensional space effectively. The tracheobronchial tree ensures even ventilation across all lung regions.
- Minimizing Resistance:
- The branching structure minimizes resistance to airflow by ensuring smooth transitions between branches and progressively reducing airway diameter while maintaining proportionality.
- Dynamic Adaptability:
- Airway branching allows for flexibility during inspiration and expiration, ensuring efficient airflow under varying conditions of pressure and volume.
- Evolutionary Efficiency:
- The tracheobronchial tree has evolved to balance structural stability with flexibility, supporting airflow without significant collapse in smaller airways.
These physical principles underline the tracheobronchial tree’s ability to perform its critical respiratory functions while conserving energy and maintaining structural integrity.
- Fractal Geometry: