Multifocal Lung Finding
- What is it:
- “Multifocal lung finding” refers to the presence of multiple abnormal areas within the lungs, involving more than one focus or region.
- These findings can represent discrete lesions, consolidations, nodules, or other abnormalities and may affect one or both lungs.
- Etymology:
- Derived from the Latin roots multi- (many) and focus (center or point), indicating numerous focal abnormalities.
- AKA:
- Multiple pulmonary lesions, disseminated lung findings (depending on context).
- TCV adjectives it applies to:
- Parts: Highlights multiple foci within the lung.
- Position: Refers to distributed involvement across various lung zones or lobes.
- Character: Can describe the morphology of the findings (e.g., nodular, cavitary, ground-glass).
- Time: May indicate whether the findings are acute, subacute, or chronic.
- Modality:
- Most commonly identified on chest X-ray or chest CT.
- MRI or PET-CT may be used for further evaluation in specific cases (e.g., metastases or inflammatory lesions).
- What does it imply:
- Normal or abnormal: Multifocal lung findings are always considered abnormal.
- Potential meanings (abnormal):
- Infectious: Pneumonia (e.g., bacterial, fungal, or viral), septic emboli, tuberculosis.
- Inflammatory: Sarcoidosis, vasculitis (e.g., granulomatosis with polyangiitis), hypersensitivity pneumonitis.
- Neoplastic: Metastatic disease, multifocal primary lung cancers.
- Trauma: Fat embolism (rare).
- Vascular: Pulmonary infarcts due to embolism.
- Idiopathic: Cryptogenic organizing pneumonia (COP).
- Next step:
- Further imaging:
- Contrast-enhanced CT for characterization of findings.
- PET-CT for metabolic activity to assess malignancy.
- Biopsy:
- CT-guided or bronchoscopic biopsy for histopathological diagnosis.
- Clinical correlation:
- Assess for systemic symptoms such as fever, weight loss, or hemoptysis to guide the differential.
- Laboratory tests:
- Blood work (e.g., inflammatory markers, infectious testing, tumor markers) as clinically indicated.
- Further imaging:

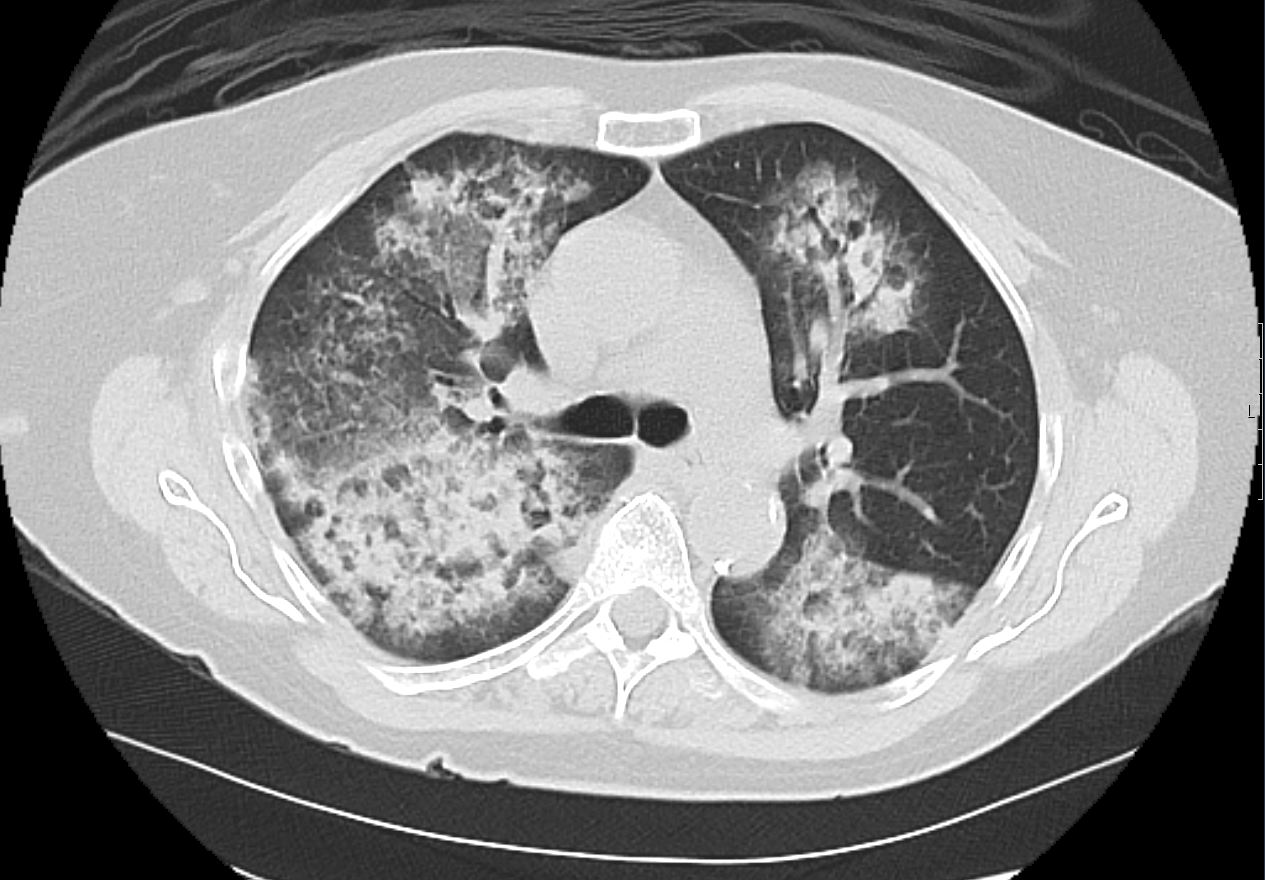
CXR and CT scan shows multifocal pneumonia involving right upper lobe, right lower lobe and to lesser extent the left upper lobe characterised by segmental and subsegmental consolidations and air bronchograms
Ashley Davidoff MD TheCommonVein.net b11521
Key Characteristics
Number:
More than one lesion or abnormality.
Distribution:
Can involve one lung or both lungs.
May be confined to specific regions (e.g., upper lobes, peripheral, or central) or diffusely spread.
Appearance:
Nodules, masses, infiltrates, ground-glass opacities, consolidation, cavitations, or mixed patterns.
Common Causes of Multifocal Lung Findings
Infectious Diseases:
Bacterial Pneumonia: Multifocal consolidations, especially in bronchopneumonia or aspiration.
Fungal Infections: Nodules or cavitations (e.g., aspergillosis, histoplasmosis).
Viral Pneumonia: Multifocal ground-glass opacities (e.g., COVID-19, influenza).
Tuberculosis: Multifocal nodules or cavitating lesions.
Malignancies:
Metastatic Disease: Hematogenous spread from cancers (e.g., breast, renal, thyroid, colorectal).
Primary Lung Cancer: Multifocal tumors in the setting of synchronous primary cancers.
Inflammatory/Autoimmune Conditions:
Sarcoidosis: Perilymphatic nodules, usually bilateral.
Rheumatoid Arthritis-Associated ILD: Multifocal reticulonodular patterns or ground-glass opacities.
Granulomatosis with Polyangiitis (GPA): Multifocal cavitating nodules.
Vascular Causes:
Septic Emboli: Multifocal nodules or cavitations.
Pulmonary Infarcts: Wedge-shaped peripheral opacities.
Pulmonary Hemorrhage Syndromes: Diffuse or multifocal ground-glass opacities.
Vasculitis
35 year old male in acute renal failure and respiratory distress with hemoptysis. CT shows multicentric segmental and subsegmental regions of consolidations and ground glass opacity in the upper and lower lobes with subpleural sparing consistent with pulmonary hemorrhage
Ashley Davidoff MD TheCommonVein.net 137273
Trauma or Iatrogenic:
Fat Embolism Syndrome: Multifocal ground-glass opacities or nodules.
Post-radiation Pneumonitis: Multifocal opacities in radiation fields.
Radiological Features
Imaging Modalities:
Chest X-ray: May show multiple opacities but limited in spatial resolution.
High-Resolution CT (HRCT): The gold standard for characterizing multifocal lung findings, including size, shape, distribution, and associated findings (e.g., cavitation, lymphadenopathy).
Key Patterns to Note:
Nodular: Suggestive of infections (e.g., tuberculosis), metastases, or sarcoidosis.
Ground-glass opacities: Associated with viral pneumonia, autoimmune diseases, or hemorrhage.
Consolidation: Seen in bacterial pneumonia, aspiration, or infarcts.
Cavitation: Possible in infections, GPA, or metastatic disease.
Clinical Correlation
Multifocal findings require integration with clinical data such as:
Symptoms: Fever (infection), hemoptysis (vasculitis, cancer), weight loss (malignancy).
Risk factors: Smoking, occupational exposure, immunosuppression.
Laboratory tests: Cultures, autoimmune panels, or tumor markers.
Differential Diagnosis
The differential depends on the patient’s history, imaging characteristics, and associated systemic findings:
Acute Symptoms:
Infections, pulmonary embolism, trauma.
Chronic Symptoms:
Malignancy, autoimmune diseases, chronic infections (e.g., tuberculosis).
Management
Further Testing:
Biopsy (bronchoscopic or surgical) for unclear causes.
Microbiological tests for infectious causes.
Treatment:
Targeted therapy based on the underlying etiology (e.g., antibiotics for infection, steroids for autoimmune conditions, chemotherapy for cancer).
Multifocal lung findings represent a wide spectrum of conditions, and their management hinges on accurate diagnosis and understanding of the underlying pathology.
