Lung Abscess: Radiology Perspective
Definition
- Localized collection of pus within lung parenchyma caused by tissue necrosis.
- Typically results from microbial infection.
Consolidation with Liquefaction

54-year-old female presents with a cough, fever and leukocytosis. CT in the axial plane shows a consolidation in the right upper lobe, with multiple abscesses with enhancing walls, consistent with lung abscesses.
Ashley Davidoff MD TheCommonVein.net 19598
-

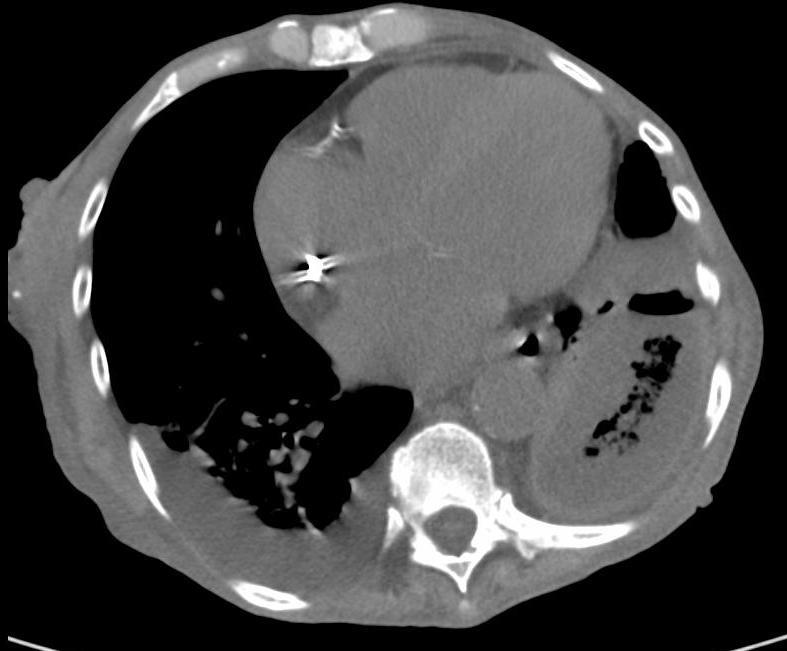
CT Right Upper Lobe Pneumonia with Abscess Formation
CT scan in the axial plane of a 63-year-old female with cough fever and leukocytosis, shows a right upper lobe consolidation with a 2.8cms fluid collection and a dependent bubble of air consistent with a diagnosis of a lung abscess secondary to pneumonia
Ashley Davidoff MD TheCommonVein.net 136170Consolidation with Cavitation

CXR Lung Abscess with Air Fluid Level
61-year-old – male presented with 3-week cough productive of phlegm and blood, right-sided chest pain, and 20-lb weight loss over the past 4 months.
CXR showed consolidative opacity in R upper lobe with two intrinsic air fluid levels concerning for abscess.
Ashley Davidoff MD TheCommonVein.net 110 LU 136164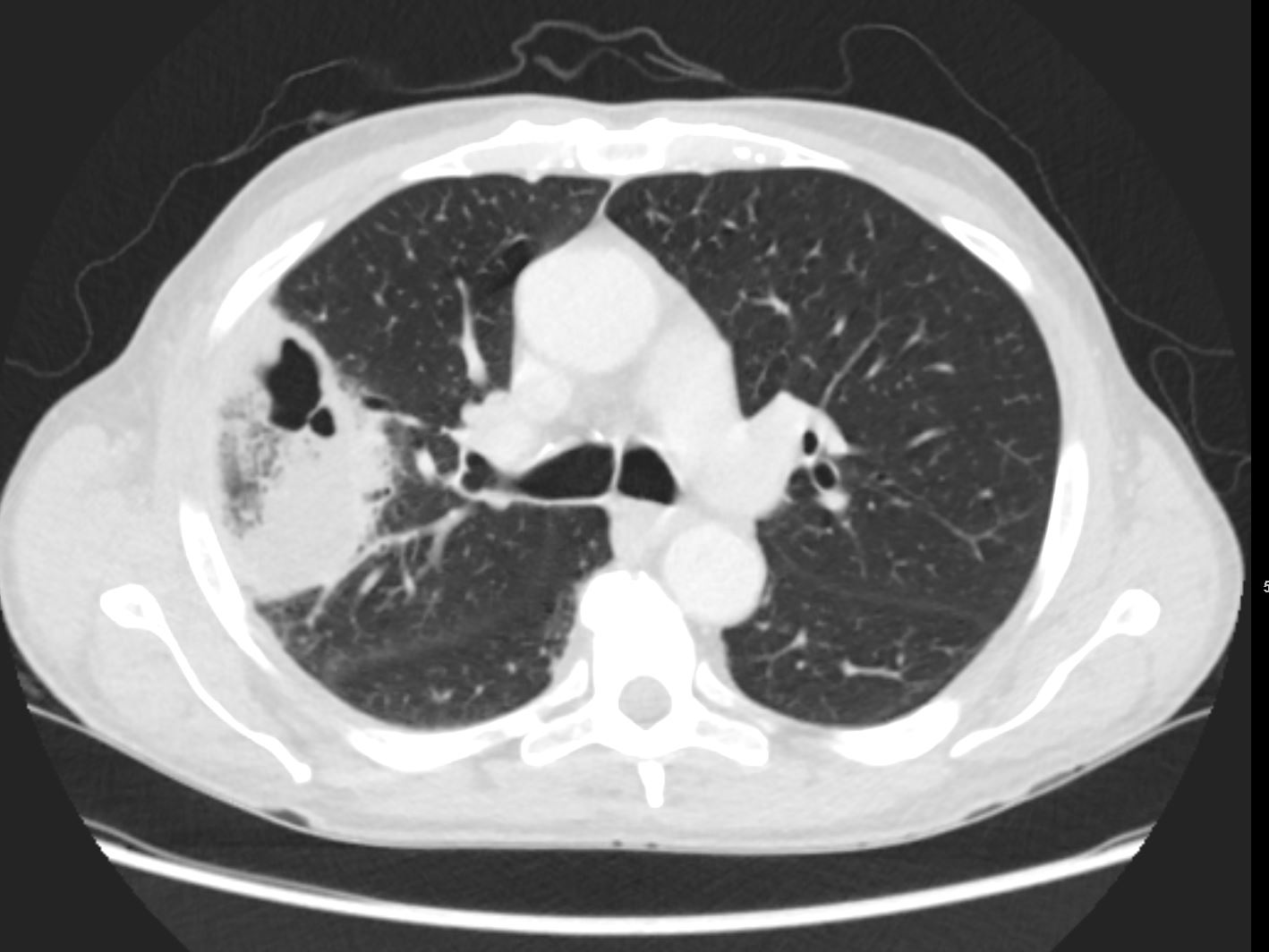
CT Lung Abscess
CT chest showed a cavitating right upper lobe abscess, with a region of consolidation and a smaller region of ground glass opacity
Ashley Davidoff MD TheCommonVein.net 110 LU 136165
Causes
- Aspiration: Most common cause, especially in patients with impaired consciousness or swallowing dysfunction.
Consolidation Cavitation Following Aspiration
76-year-old female presents 2 months after an episode of aspiration pneumonia with ongoing sepsis, now on dialysis. Axial CT shows left lower pneumonitis, cavitation l and associated parapneumonic effusion with thickened pleura. Culture of fluid confirmed an empyema
Ashley Davidoff MD TheCommonVein.net 261Lu 46130b01
- Infections: Bacterial (e.g., anaerobes, Staphylococcus aureus), fungal, or mycobacterial.
Pneumococcal Abscess

54-year-old female presents with a cough, fever and leukocytosis. CT in the axial plane shows a cavitating pneumonia (b, white arrowheads) with large abscess and air-fluid level (b, yellow arrowheads), and multiple small intraparenchymal abscesses (b, orange arrowheads)
Ashley Davidoff MD TheCommonVein.net 260Lu 31591cL
Septic Emboli and Cavitating Infected Infarction
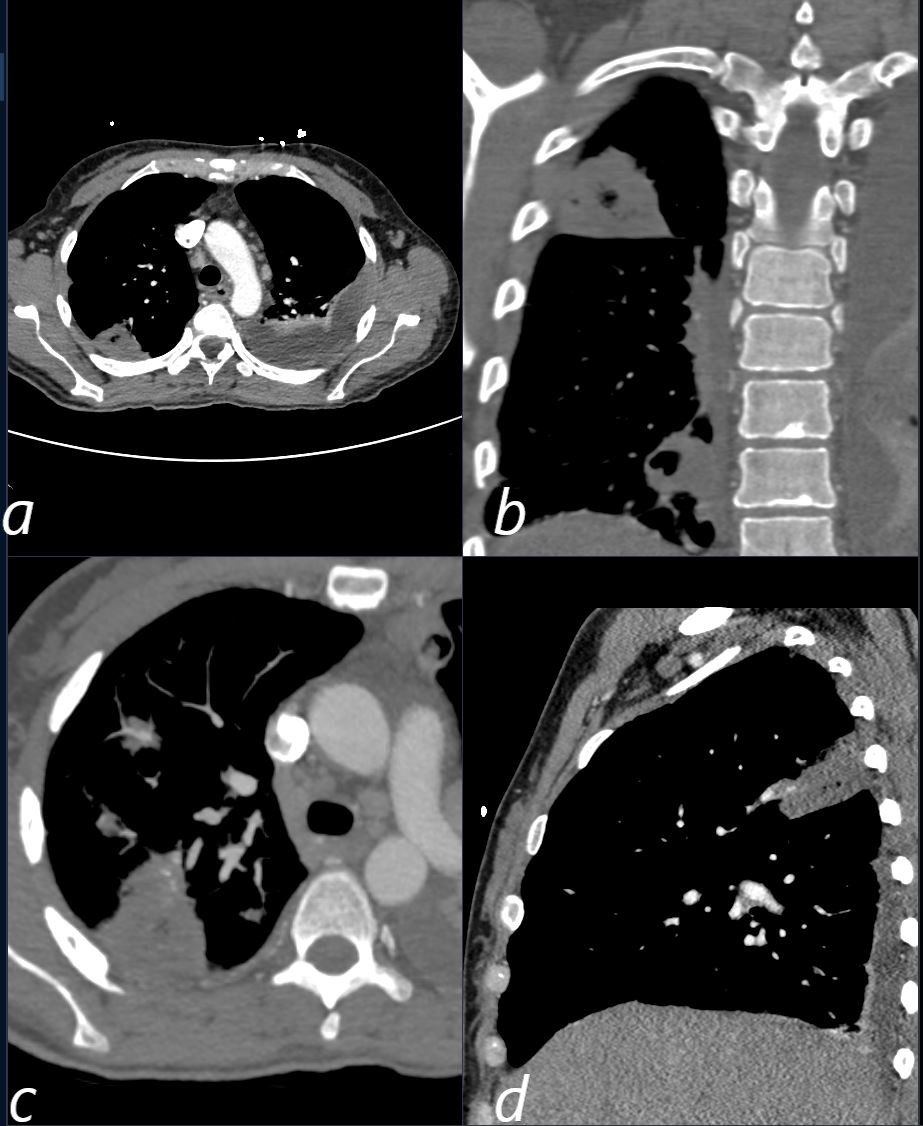
CT scan in a 39 year old female with endocarditis presents with a fever and right sided chest pain.
Multiple views in axial (a,c) coronal (b) and sagittal reveals the presence of a wedge shaped consolidation with cavitation confirming the presence of an infected and cavitating infarction in the posterior segment of the left upper lobe. A loculated effusion is noted at the left base.
Ashley Davidoff TheCommonVein.net
b11422c
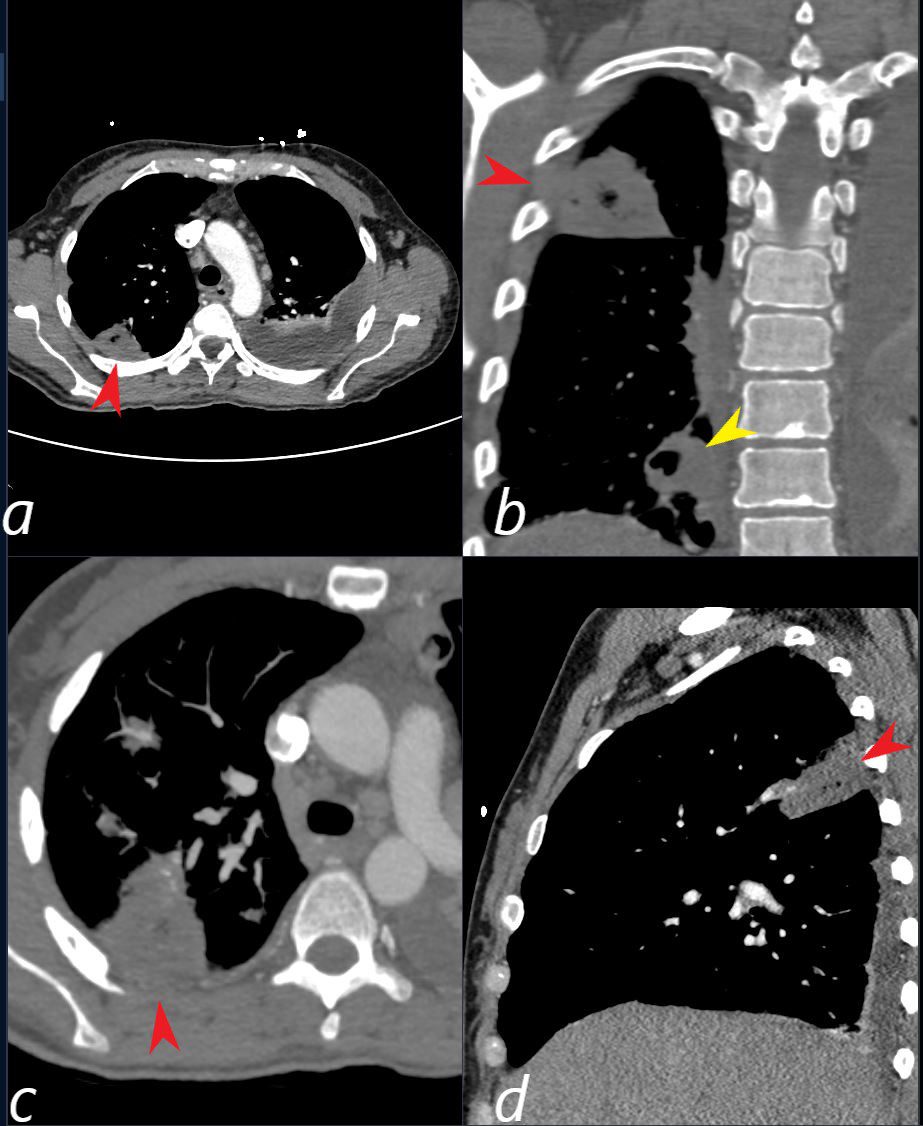
CT scan in a 39 year old female with endocarditis presents with a fever and right sided chest pain.
Multiple view in axial (a,c) coronal (b) and sagittal confirm the presence of a wedge shaped consolidation with cavitation (red arrowhead a,b,c, and d) confirming the presence of an infected and cavitating infarction in the posterior segment of the left upper lobe. A second similar subsegmental infarct and abscess (yellow arrowhead, is noted in the right lower lobe (b yellow arrowhead) . A loculated effusion is noted at the left base.
Ashley Davidoff TheCommonVein.net b11422cL
- Post-obstructive:
Tumor or foreign body obstructing airways.
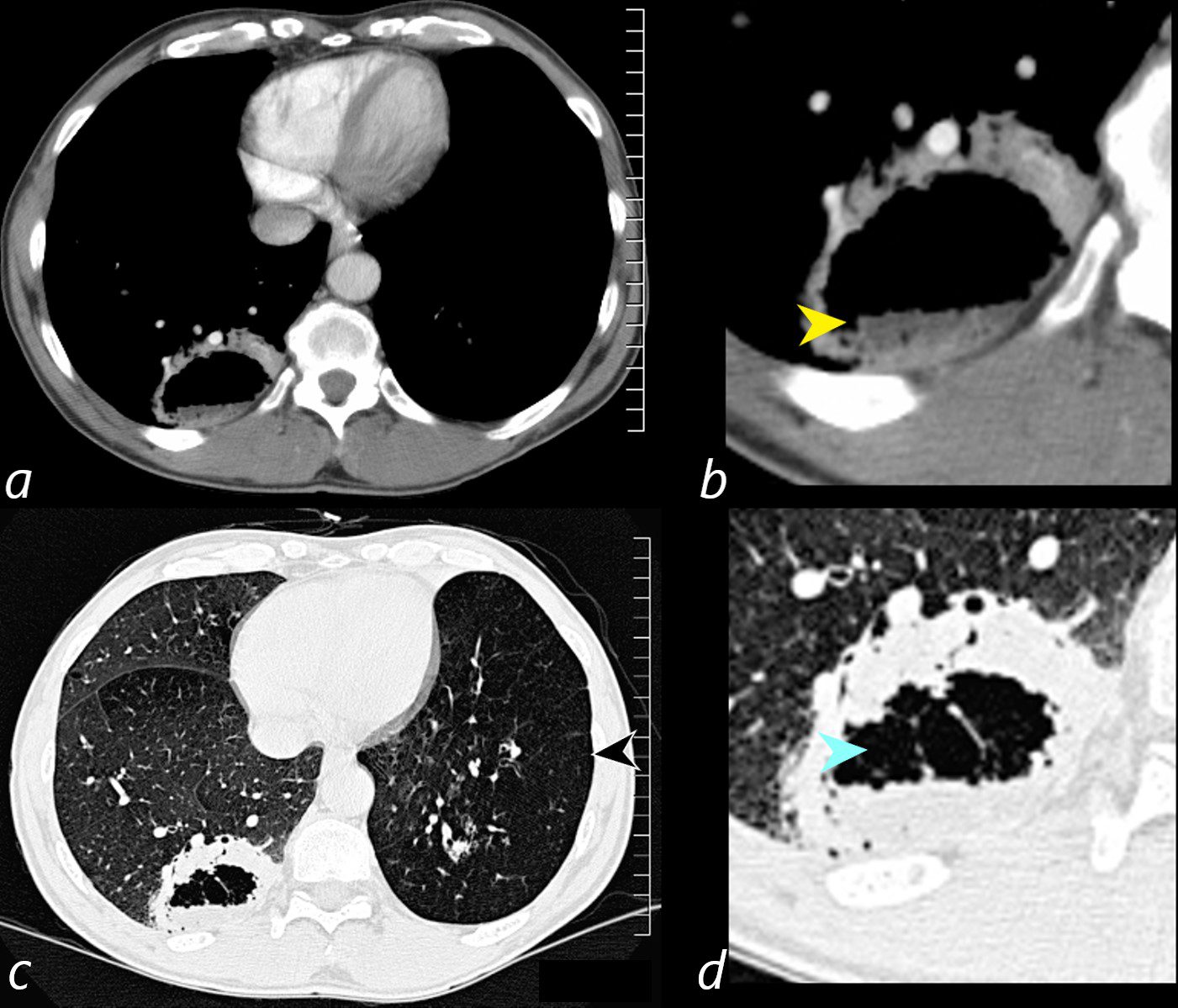
Axial CT scan at the level of the lung bases in a 56-year-old male with an obstructing carcinoid tumor of the lingula shows a cavitating abscess cavity(d, blue arrowhead) with an air fluid level in the right lower lobe (b yellow arrowhead).
The left lower lobe is relatively lucent, reflecting compensatory hyperinflation secondary to the lingula atelectasis (c, black arrowhead)
Ashley Davidoff MD TheCommonVein.net 261Lu 118383cL
- Hematogenous spread: From distant sites of infection.
- Trauma: Penetrating lung injuries.
Results
- Lung consolidation, often with surrounding inflammation.
- Progression to tissue necrosis and cavitation.
- Formation of a cavity filled with fluid or air-fluid levels.
- Potential complications: rupture into pleura (empyema), bronchopleural fistula, or sepsis.
Diagnosis
- Clinical Presentation:
- Fever, night sweats, weight loss.
- Cough with foul-smelling sputum or hemoptysis.
- Chest pain and dyspnea.
- Imaging:
- Chest X-ray (CXR):
- Initial: Consolidation with or without air-fluid levels.
- Later: Cavitation with visible air-fluid levels, typically in the dependent lung segments.
- Chest CT:
- Better delineation of consolidation and cavitation.
- Visualization of thickened cavity walls, necrotic tissue, and surrounding lung involvement.
- Detects complications (e.g., empyema, pleural extension).
- Chest X-ray (CXR):
- Laboratory Tests:
- Elevated WBC count.
- Sputum cultures and blood cultures for pathogen identification.
- Serologic testing for specific pathogens (e.g., fungal or mycobacterial).
Treatment
- Antibiotics:
- Broad-spectrum coverage initially, tailored based on cultures.
- Common regimens include clindamycin or beta-lactam with a beta-lactamase inhibitor.
- Drainage:
- Percutaneous drainage under imaging guidance for large or refractory abscesses.
- Surgical intervention:
- Reserved for cases with failure of medical management or complications like massive hemoptysis.
Pearls
- Suspect in at-risk populations (e.g., alcoholics, post-stroke, seizure disorders).
- Consolidation is often seen earlier in the disease course than cavitation.
- Differentiate from malignancy or other cavitary lesions via imaging and microbiologic workup.
- Early intervention improves outcomes and prevents complications.
