- Etymology
Derived from the Latin word “cavus,” meaning “hollow.” - AKA
Cavitation, Pulmonary Cavity - Definition
- What is it?
A lung cavity is a gas-filled space within the pulmonary parenchyma, typically formed by necrosis and subsequent evacuation of lung tissue. - Caused by
- Infection
- Tuberculosis (active or post-primary/reactivation TB is the most common infectious cause of cavities).
- Bacterial infections such as Klebsiella pneumoniae or Staphylococcus aureus (necrotizing pneumonia).
- Fungal infections, such as aspergillosis or histoplasmosis, leading to cavitation.
- Malignancy
- Most commonly squamous cell carcinoma of the lung, which can cause necrosis and cavitation in centrally located tumors.
- Adenocarcinoma can also occasionally cavitate, although less commonly than squamous cell carcinoma.
- Inflammatory diseases
- Rheumatoid arthritis-associated necrobiotic nodules.
- Granulomatosis with polyangiitis (Wegener?s granulomatosis).
- Trauma
- Pulmonary lacerations resulting from blunt or penetrating injury.
- Other causes
- Septic emboli, particularly in intravenous drug users or patients with endocarditis.
- Post-radiation necrosis.
- Infection
- Resulting in
Localized hollowing within the lung parenchyma, which may impair gas exchange and predispose to secondary infections. - Structural changes
Disruption of alveolar architecture, thinning or irregularity of cavity walls, and potential communication with the airways or pleural space. - Pathophysiology
The formation of a cavity begins with localized tissue necrosis, often secondary to infection, malignancy, or ischemia. Liquefaction and subsequent evacuation of necrotic material create a gas-filled space. In infections such as tuberculosis, cavitation reflects extensive tissue destruction and can facilitate the spread of disease. - Pathology
The cavity may have thick or thin walls, depending on the underlying etiology. It can contain air, fluid, or debris and may demonstrate inflammatory or neoplastic cells in histopathologic evaluation. - Diagnosis
- Clinical
Symptoms may include cough, hemoptysis, fever, weight loss, and dyspnea, depending on the underlying cause. - Radiology
Cavities are typically identified on imaging as air-filled spaces within the lung with or without air-fluid levels. - Labs
Laboratory tests, such as sputum cultures, acid-fast bacilli (AFB) testing, fungal serologies, and autoimmune panels, can help identify specific causes.
- Clinical
- Treatment
Treatment depends on the underlying cause, such as antibiotics for bacterial infections, antifungals for fungal diseases, chemotherapy for malignancies, or surgery for structural complications.
- What is it?
- Radiology
- CXR
- Findings
A cavity appears as a lucent area within the lung parenchyma with a surrounding wall of variable thickness. - Associated Findings
Air-fluid levels may indicate superimposed infection or abscess formation.
- Findings
- CT
- Parts
Includes cavity wall, contents (air, fluid, debris), and surrounding lung parenchyma. - Size
Variable, depending on the cause; small in early stages or large in advanced cases. - Shape
Typically round or oval; irregular in cases of malignancy or complex infections. - Position
May occur anywhere in the lungs; often upper lobes in tuberculosis and apical or peripheral regions in fungal infections. - Character
Thin-walled in benign conditions; thick-walled in malignancies or active infections. - Time
Can evolve with treatment or progression of disease. Chronic cavities may calcify. - Associated Findings
Adjacent consolidation, nodules, or pleural abnormalities.
- Parts
- Other relevant Imaging Modalities
- MRI/PET-CT/NM/US/Angio
- PET-CT can assess metabolic activity, helping differentiate benign from malignant cavities.
- Ultrasound may aid in characterizing pleural-based lesions.
- MRI/PET-CT/NM/US/Angio
- Pulmonary function tests (PFTs)
Not directly diagnostic but may show restrictive or obstructive patterns depending on the underlying disease.
- CXR
- Complications
- Fungal superinfection
Aspergillus species can colonize pre-existing cavities, leading to aspergillomas or invasive aspergillosis. - Other mycetomas
Colonization by other fungi, such as Candida or Histoplasma. - Active tuberculosis
Can lead to transbronchial spread of infection, contributing to new areas of disease within the same or opposite lung. - Hemoptysis
Can occur due to erosion of blood vessels by the expanding cavity or superimposed infections.
- Fungal superinfection
- Recommendations
Further evaluation may include bronchoscopy, biopsy, or microbiological studies for definitive diagnosis. Regular follow-up imaging is critical to assess resolution or complications. - Key Points and Pearls
- Cavities are a hallmark of active tuberculosis and may facilitate transbronchial spread of infection.
- Thick-walled cavities raise suspicion for malignancy, particularly squamous cell carcinoma.
- Secondary fungal infections, such as aspergillosis, are common complications in pre-existing cavities.
- Air-fluid levels within a cavity suggest superimposed infection or rupture into the airway.
- Prompt diagnosis and treatment are essential to prevent complications, especially in infectious causes.
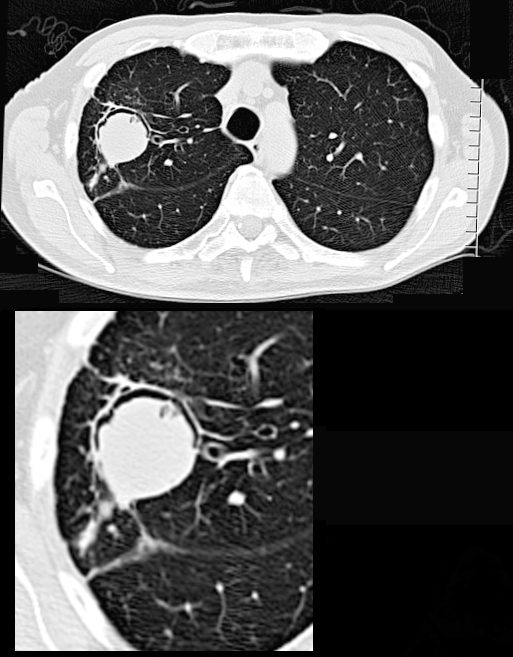
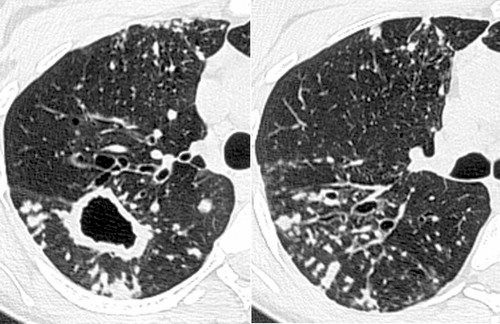
66- year-old malnourished, immunodeficient male presents with a chronic cough.
CT in the axial plane shows a 3.2cms right upper lobe mass with a rim of a crescentic accumulation of air in the dependant portionof the mass (magnified in the lower image) while the aspergilloma “sinks” to the most dependent portion of the cavity . This finding reflects an air -crescent sign and is consistent with a diagnosis of an aspergilloma
Ashley Davidoff TheCommonVein.net 293Lu 113528c
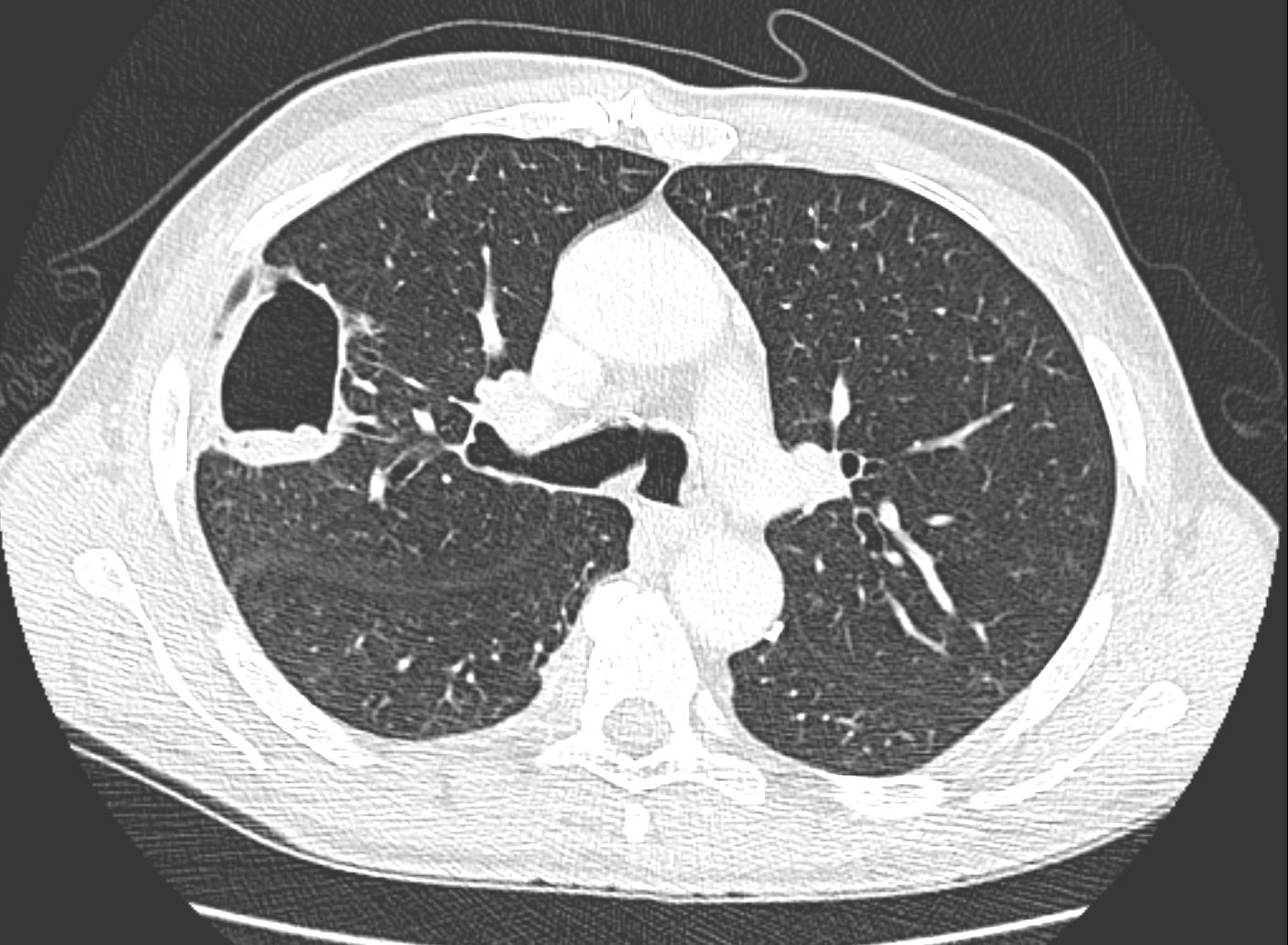
CT in the axial plane, 1 month later shows shows decreased consolidation and cavity size has become more prominent.
Ashley Davidoff MD TheCommonVein.net 110Lu 136167
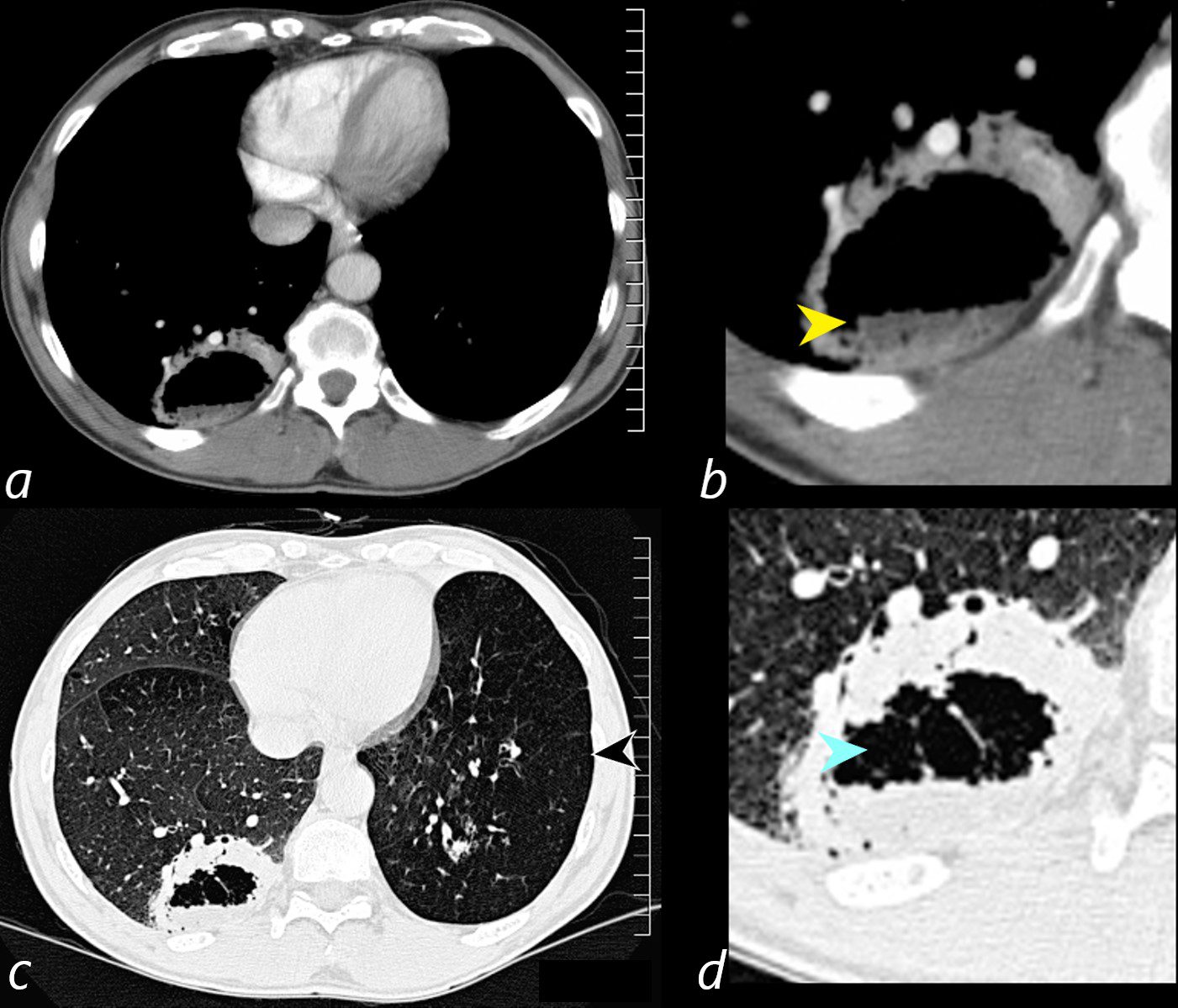
Axial CT scan at the level of the lung bases in a 56-year-old male with an obstructing carcinoid tumor of the lingula shows a cavitating abscess cavity(d, blue arrowhead) with an air fluid level in the right lower lobe (b yellow arrowhead).
The left lower lobe is relatively lucent, reflecting compensatory hyperinflation secondary to the lingula atelectasis (c, black arrowhead)
Ashley Davidoff MD TheCommonVein.net 261Lu 118383cL

CT of a 54 year old male shows a large left apical cavity with aspergilloma. These findings are consistent with chronic pulmonary aspergillosis In the apex of the right lung, there is pneumonic consolidation and abscess formation . Note the air fluid level in the right apex on axial soft tissue and lung windows.
Ashley Davidoff TheCommonvein.net 225Lu 134202
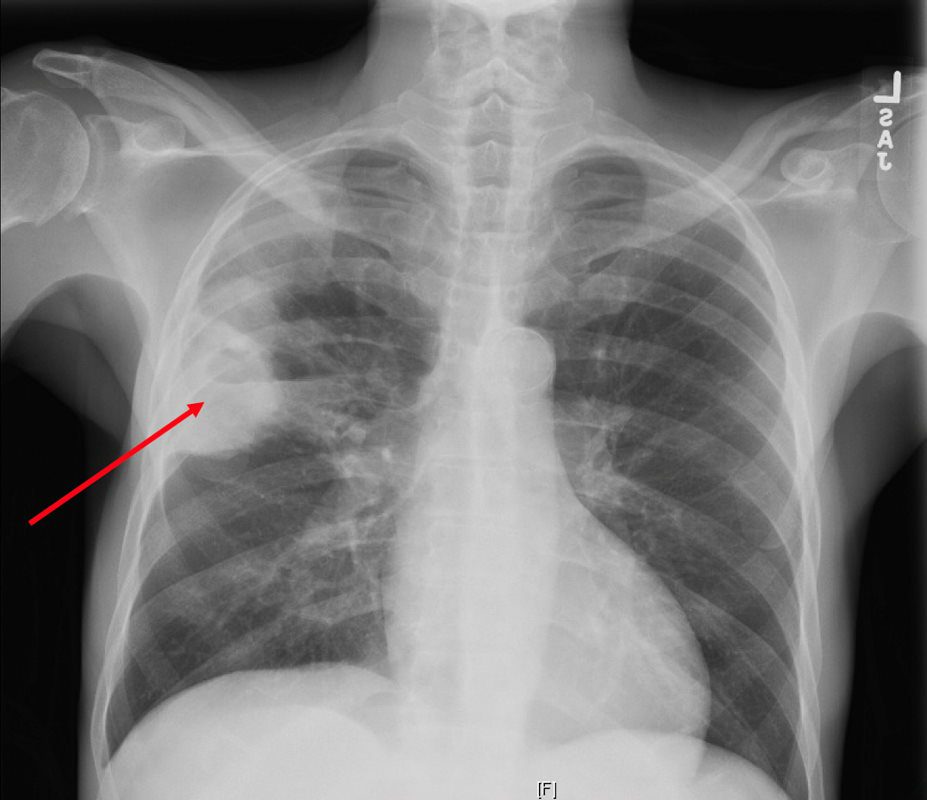
CXR reveals a dense consolidation in the right upper lobe (red arrow) with questionable air-fluid level. No pneumothorax. No pleural effusions. Differential includes right upper lobe pneumonia or tuberculosis. CT is recommended for further evaluation if there is concern for a cavity.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
TheCommonVein.net
Rossi, SE et al Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview RadioGraphicsVol. 25, No. 3 2005
132031.8.jpg
LUNG ABSCESS LIP HIV AIDS and LYMPHOMA27 year old male with a history of perinatal HIV with intermittent highly active antiretroviral therapy (HAART) compliance with a CD4 count of < 50 with biopsy confirmed B cell lymphoma of the liver, s/p CHOP therapy , chronic esophageal strictures s/p dilatations, esophageal candidiasis, LIP, bronchiectasis pancreatitis, and portal vein and splenic vein thrombosis.
Initial Chest X-ray shows a diffuse reticular pattern with cystic changes dominant at the bases.
CT at that time confirmed the presence of diffuse cystic changes with the largest cysts at the lung bases. Ascites and splenomegaly are also present
He presented one month later with fever and neutropenia.
CT showed an abscess cavity in the right upper lobe in the right upper lobe, thickened distal esophagus with edematous wall, atrophic gastritis and ascites. Bronchovascular thickening along a bronchiectatic segment in the right upper lobe was present in the last CT
Ashley Davidoff MD TheCommonVein.net 017Lu 132031

Ashley Davidoff MD TheCommonVein.net Wegeners-cavitation-018
