Etymology
- Derived from the Latin word collapsus, meaning “fall together,” and the Greek word atelectasis, meaning “incomplete expansion.” The term refers to the complete collapse of an entire lung.
AKA
- Complete lung atelectasis
- Total lung atelectasis
Definition
What is it?
- Total lung collapse refers to the complete atelectasis of an entire lung, resulting in the absence of aeration in the affected lung and significant volume loss. It is often a life-threatening condition requiring immediate intervention.
Caused by
- Obstruction of the mainstem bronchus:
- Mucus plugging
- Foreign body aspiration
- Endobronchial tumor
- Post-intubation stenosis
- External compression of the lung:
- Massive pleural effusion
- Tension pneumothorax
- Large intrathoracic mass
- Severe loss of surfactant in neonates (e.g., neonatal respiratory distress syndrome)
Resulting in
- Complete alveolar collapse in the affected lung
- Severe hypoxemia and respiratory distress
- Mediastinal shift and hemodynamic compromise in severe cases
Structural Changes
- Complete alveolar collapse with no residual air in the affected lung
- Severe displacement of mediastinal structures toward the collapsed side
- Compression of the contralateral lung in cases of significant volume loss
Pathophysiology
- Total lung collapse occurs when the entire lung becomes atelectatic due to obstruction of the mainstem bronchus or external compression. Air distal to the obstruction is absorbed, leading to alveolar collapse. In cases of pleural effusion or pneumothorax, external pressure forces the lung to collapse entirely. The complete loss of ventilation in the affected lung causes profound ventilation-perfusion mismatch, hypoxemia, and potentially life-threatening hemodynamic instability.
Pathology
- Collapsed alveoli with no air spaces
- Distorted bronchi and vessels pulled toward the collapsed lung
- Possible inflammation or fibrosis in chronic cases
Radiology in Detail
CXR
Findings
- Uniform opacification of the hemithorax corresponding to the collapsed lung
- Mediastinal shift toward the collapsed side
- Elevation of the hemidiaphragm on the affected side
- Crowding of ribs on the affected side
Associated Findings
- Contralateral hyperinflation due to compensatory mechanisms
- Potential pleural effusion or pneumothorax contributing to collapse
CT
Parts
- Entire lung parenchyma on the affected side
Size
- Significant volume loss involving the whole lung
Shape
- Homogeneous, dense opacity replacing the aerated lung
Position
- Complete collapse of the lung, typically with mediastinal structures pulled toward the affected side
Character
- Uniform opacity with sharp demarcation at the fissure or pleural boundary
- Displacement of bronchi and vascular structures
Time
- Acute onset in cases of obstruction or pneumothorax
- Chronic in cases of untreated obstruction or progressive fibrosis
Associated Findings
- Pleural effusion, pneumothorax, or evidence of a mass or obstruction
Other Imaging Modalities
MRI/PET CT/NM/US/Angio
- MRI: Rarely used but may assess associated soft tissue masses or lesions
- PET-CT: Useful for identifying malignant causes of bronchial obstruction or associated masses
- Ultrasound: Detects pleural effusion contributing to collapse
Key Points and Pearls
- Total lung collapse is a life-threatening condition requiring urgent evaluation and management.
- Common causes include mainstem bronchus obstruction, massive pleural effusion, or tension pneumothorax.
- Radiologically, it presents as complete opacification of the hemithorax with mediastinal shift toward the collapsed side.
- CT imaging is crucial for identifying the underlying cause, such as bronchial obstruction or pleural disease.
- Management involves addressing the underlying cause, such as bronchoscopy for obstruction, thoracentesis for effusion, or chest tube placement for pneumothorax.
White Out and Differential Diagnosis
- “White out” refers to complete opacification of a hemithorax on imaging, commonly seen in total lung atelectasis.
- Differential diagnosis for “white out” includes:
- Total lung collapse (atelectasis)
- Massive pleural effusion
- Pneumonectomy
- Extensive consolidation (e.g., pneumonia)
- Large pulmonary mass or malignancy
- Tension pneumothorax with contralateral mediastinal shift
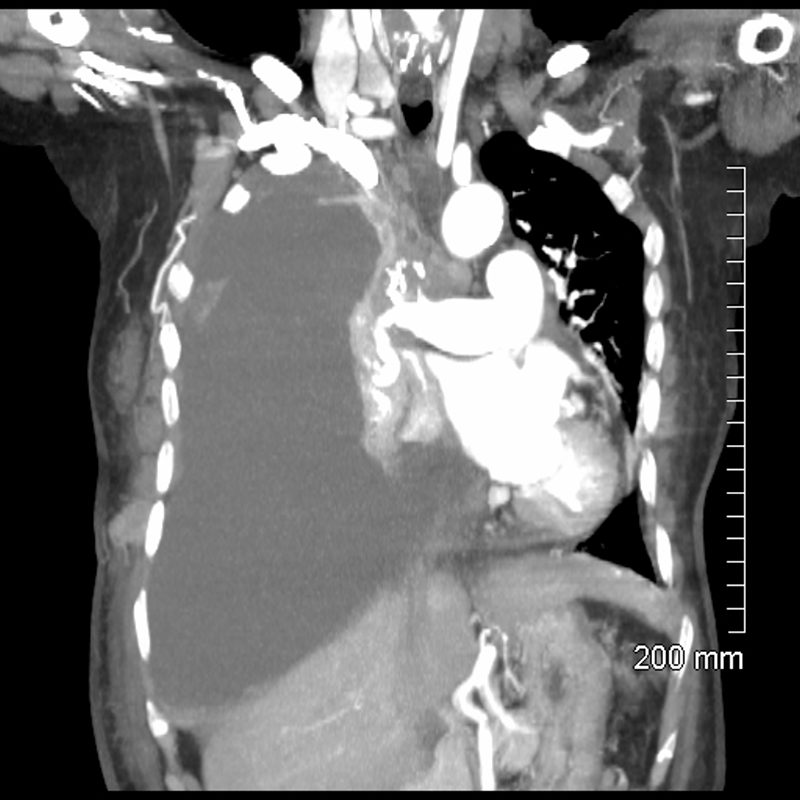
85-year-old female with a history of lung cancer, presents with a dyspnea and hypotension. CT scan shows a large right pleural effusion under pressure, with mediastinal shift to the left. In addition, there is compression of the heart with back up of venous return due the pressure effect on the heart and vascular structures. The effusion in the right pleural cavity with atelectatic lung herniates into the left hemithorax.
Ashley Davidoff MD TheCommonVein.net 106Lu 118467
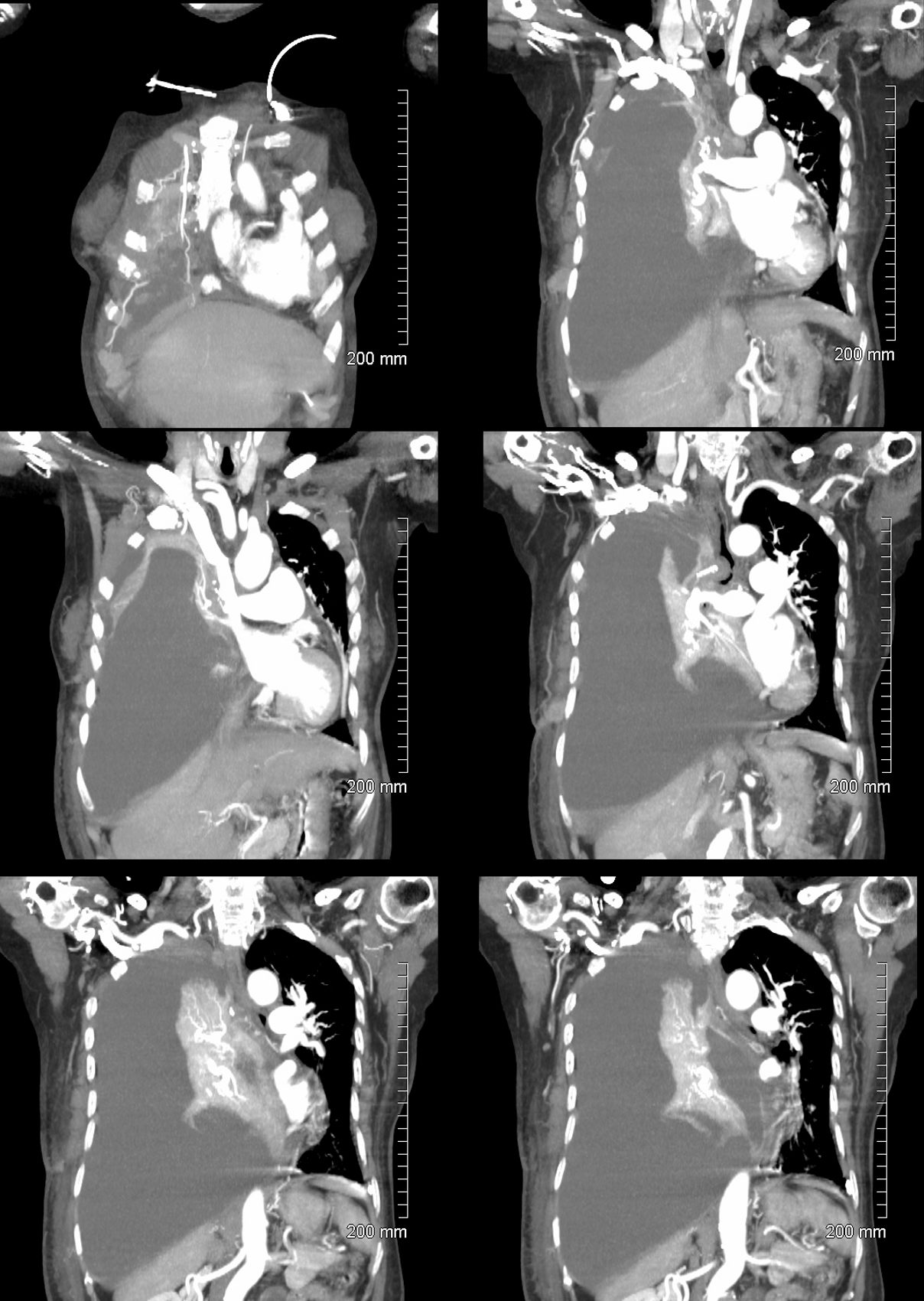
85-year-old female with a history of lung cancer, presents with a dyspnea and hypotension. CT scan shows a large right pleural effusion under pressure, with mediastinal shift to the right. In addition, there is compression of the heart with back up of venous return due the pressure effect on the heart and vascular structures. Among the structures showing venous distension are the SVC (blue arrowhead, a) right sided upper limb veins (blue arrowhead b) and the left upper pulmonary veins (red arrowhead, b. The effusion in the right pleural cavity with atelectatic lung herniates into the left hemithorax, (white arrowhead, c). There is a dense sediment in the pleural fluid (red arrowhead, d) suggesting blood in the pleural cavity. The left atrium is compressed (maroon arrowhead, d)
Ashley Davidoff MD TheCommonVein.net106Lu 118467c
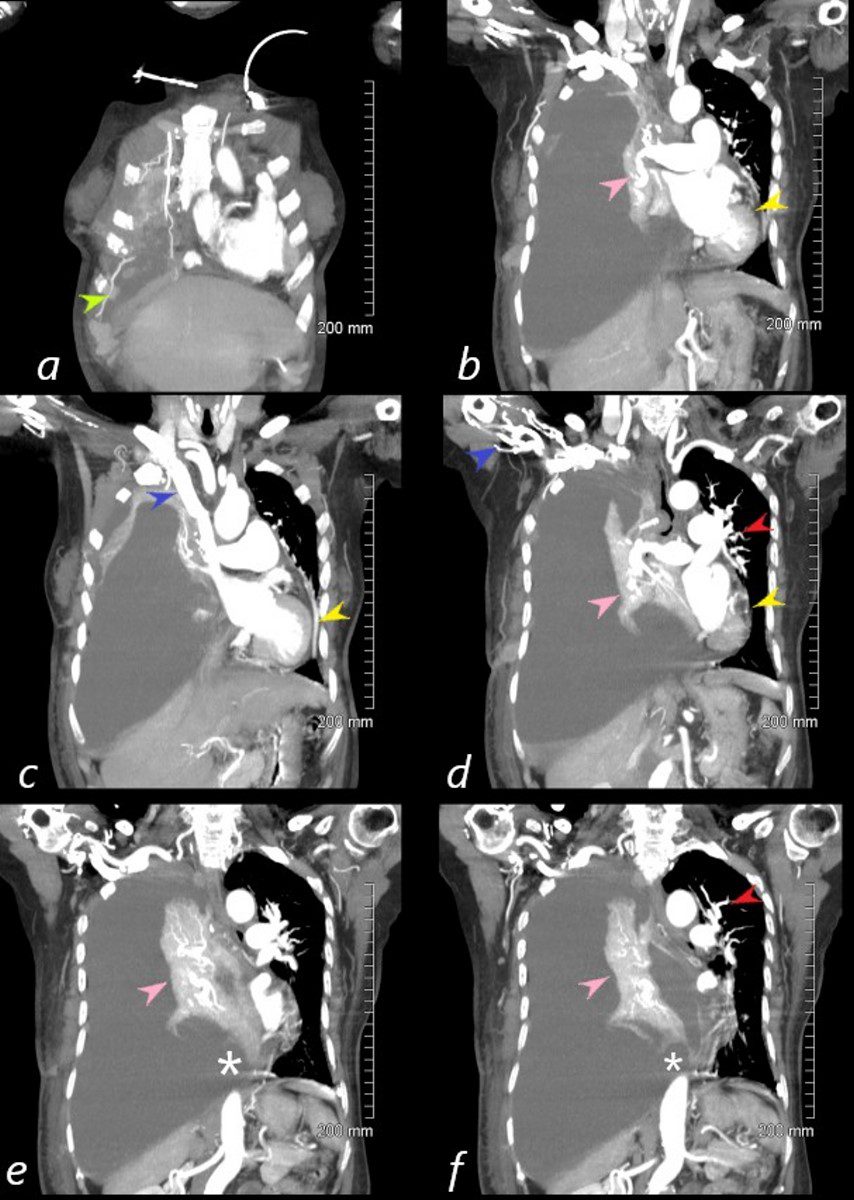
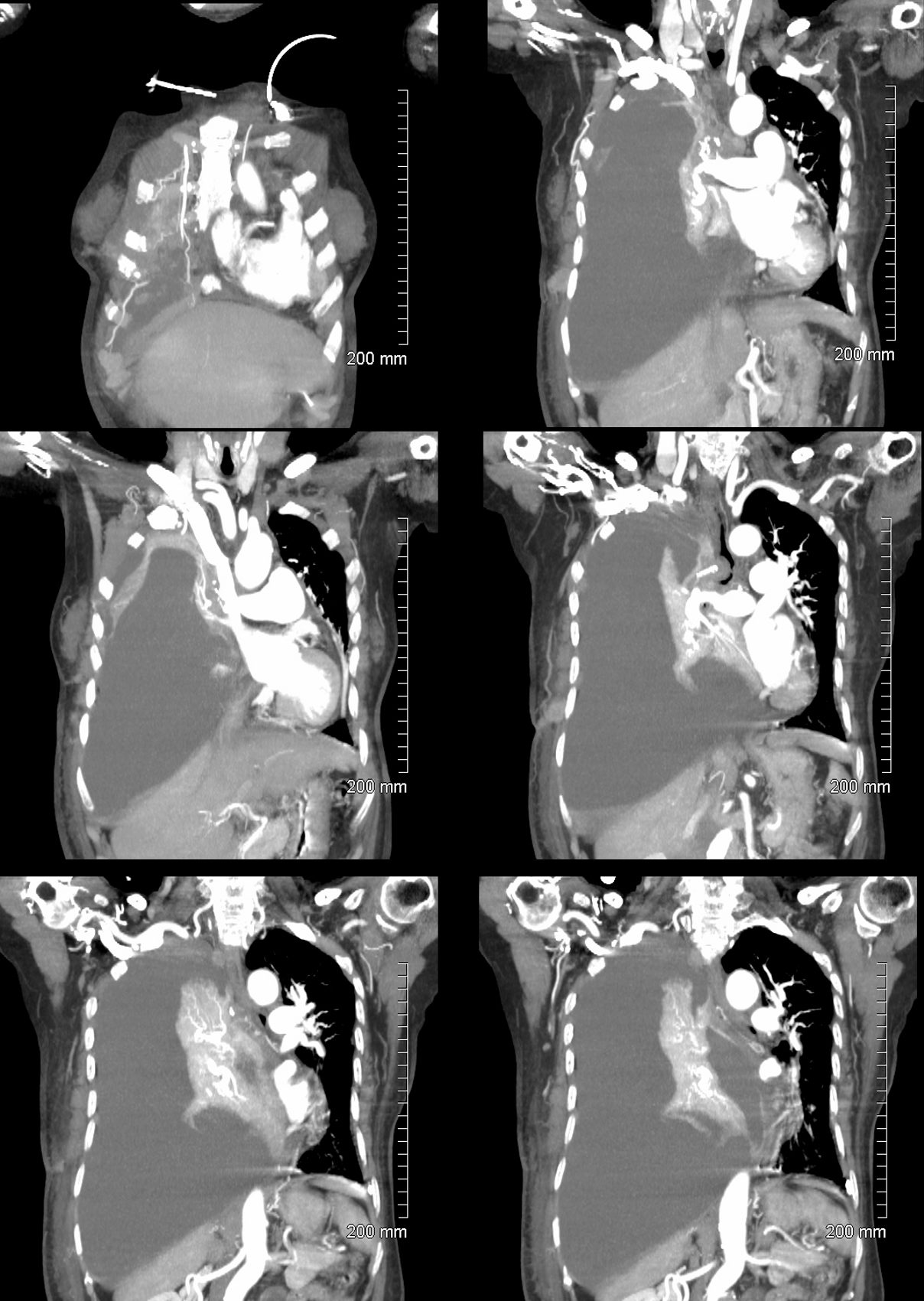
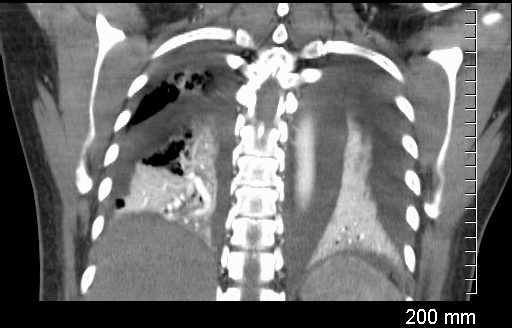
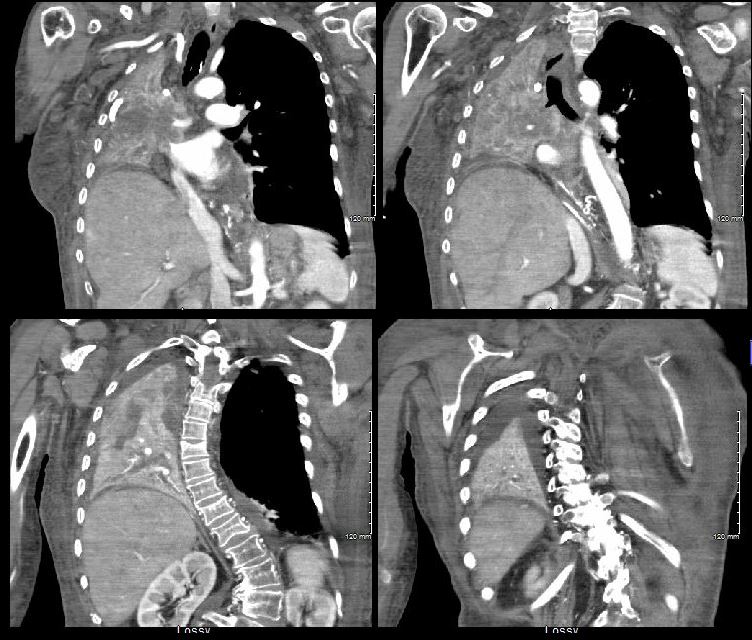
85-year-old female with a history of lung cancer, presents with a dyspnea and hypotension. Reconstruction of the CT scan in the coronal plane, shows a large right pleural effusion under pressure with herniation into the left chest (white asterisk e,and f) , with mediastinal shift to the left (yellow arrowhead b, c, d). In addition, there is compression of the heart with back up of venous return due the pressure effect on the heart and vascular structures. Among the structures showing venous distension are the SVC (blue arrowhead, c) right sided upper limb veins (blue arrowhead d) and the left upper pulmonary veins (red arrowhead, d and f). The density of the systemic venous and arterial systems is similar, but vascular structures as noted by the green arrowhead in a could represent venous collaterals.
Ashley Davidoff MD TheCommonVein.ne 106Lu 118467cL
Radiologic Findings of Total Lung Collapse
- Increased Opacity:
- The collapsed lung becomes densely opaque on imaging, as the air is absorbed from the lung tissue and the remaining lung is composed primarily of soft tissue.
- The entire hemithorax (one side of the chest) may appear more opaque than the unaffected side.
- Mediastinal Shift:
- Structures such as the heart, trachea, and mediastinum shift toward the collapsed lung due to the loss of volume on that side.
- This shift can be prominent, especially in cases of complete lung atelectasis without compensatory hyperinflation on the contralateral side.
- Elevation of the Hemidiaphragm:
- The diaphragm on the side of the collapsed lung is pulled upward due to the decreased intrathoracic pressure on that side.
- The hemidiaphragm may be noticeably higher than the one on the unaffected side.
- Rib Space Narrowing:
- There is narrowing of the intercostal spaces on the side of the collapse, as the chest wall is pulled inward by the loss of lung volume.
- Silhouetting of Adjacent Structures:
- The normal borders of structures like the heart, aorta, and hemidiaphragm may be obscured by the collapsed lung, which now occupies a smaller, dense space adjacent to these structures.
- This finding can help in determining the location of the collapse and distinguishing it from other causes of increased opacity.
- Compensatory Hyperinflation of the Opposite Lung:
- The unaffected lung may appear hyperinflated, as it expands to fill some of the space left by the collapsed lung.
- The expansion of the unaffected lung may include herniation across the midline into the space of the collapsed lung.
- Crowding of Pulmonary Vessels and Bronchial Structures:
- Bronchi and vessels within the collapsed lung appear crowded and may be displaced toward the hilum.
- Bronchial Cutoff Sign (If Visible):
- On CT or sometimes X-ray, the cause of the collapse, such as an obstructing tumor or mucus plug, may be visible as an abrupt cutoff in the bronchus.
Additional Findings on CT
CT imaging provides a clearer view and may show:
- Direct visualization of the obstruction if there is a mass, mucus plug, or foreign body.
- Collapsed lung tissue appearing as a dense, triangular or wedge-shaped opacity.
- Possible pleural effusion on the affected side, sometimes seen in cases of malignancy or infection.
Causes
Common causes of total lung collapse include:
- Endobronchial obstruction: Often due to a tumor, mucus plug, or foreign body in the main bronchus.
- Malignancy: Lung cancer can obstruct a major bronchus and is a common cause of total lung collapse in adults.
- Large pleural effusion or pneumothorax: Can indirectly cause lung collapse by compressing the lung from outside.
Summary
Total lung collapse results in a range of radiologic findings, primarily marked by increased opacity, mediastinal shift, elevation of the hemidiaphragm, narrowing of the rib spaces, and potential compensatory hyperinflation of the opposite lung. These findings are important to identify the presence and side of the collapse and suggest possible underlying causes that may require further evaluation.
Total Left Lung Collapse
Tension Pneumothorax

Ashley Davidoff MD TheCommonVein.net
77949
49 year old male with a cough presents for a Chest Xray which showed a tension pneumothorax. Chest tube was placed emergently in the radiology department.
Ashley Davidoff MD TheCommonVein.net
117300c
Total Right Lung Collapse
Tension Hydrothorax
from large pleural effusion and probable hemothorax under tension with atelectasis of the right lung
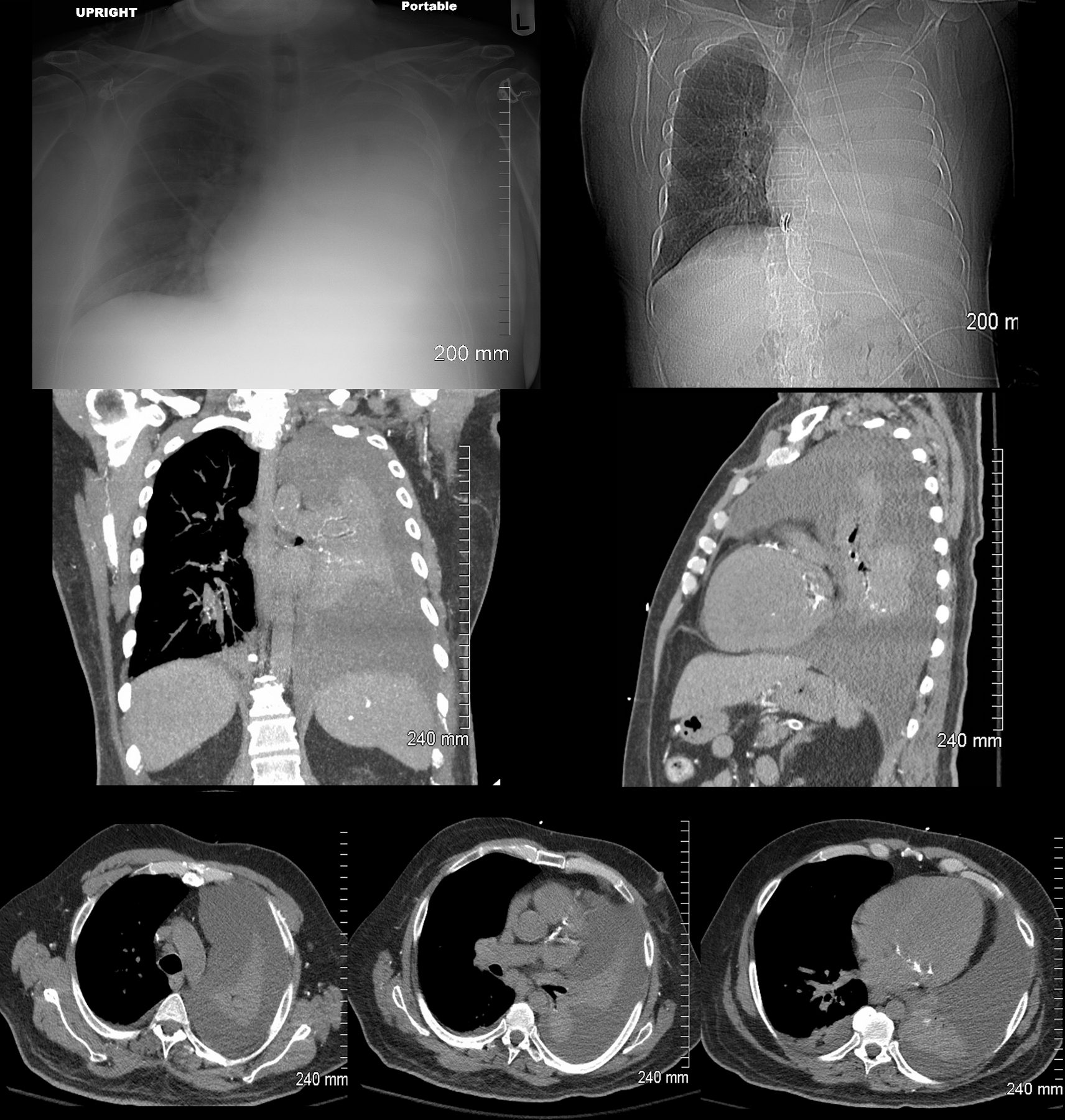
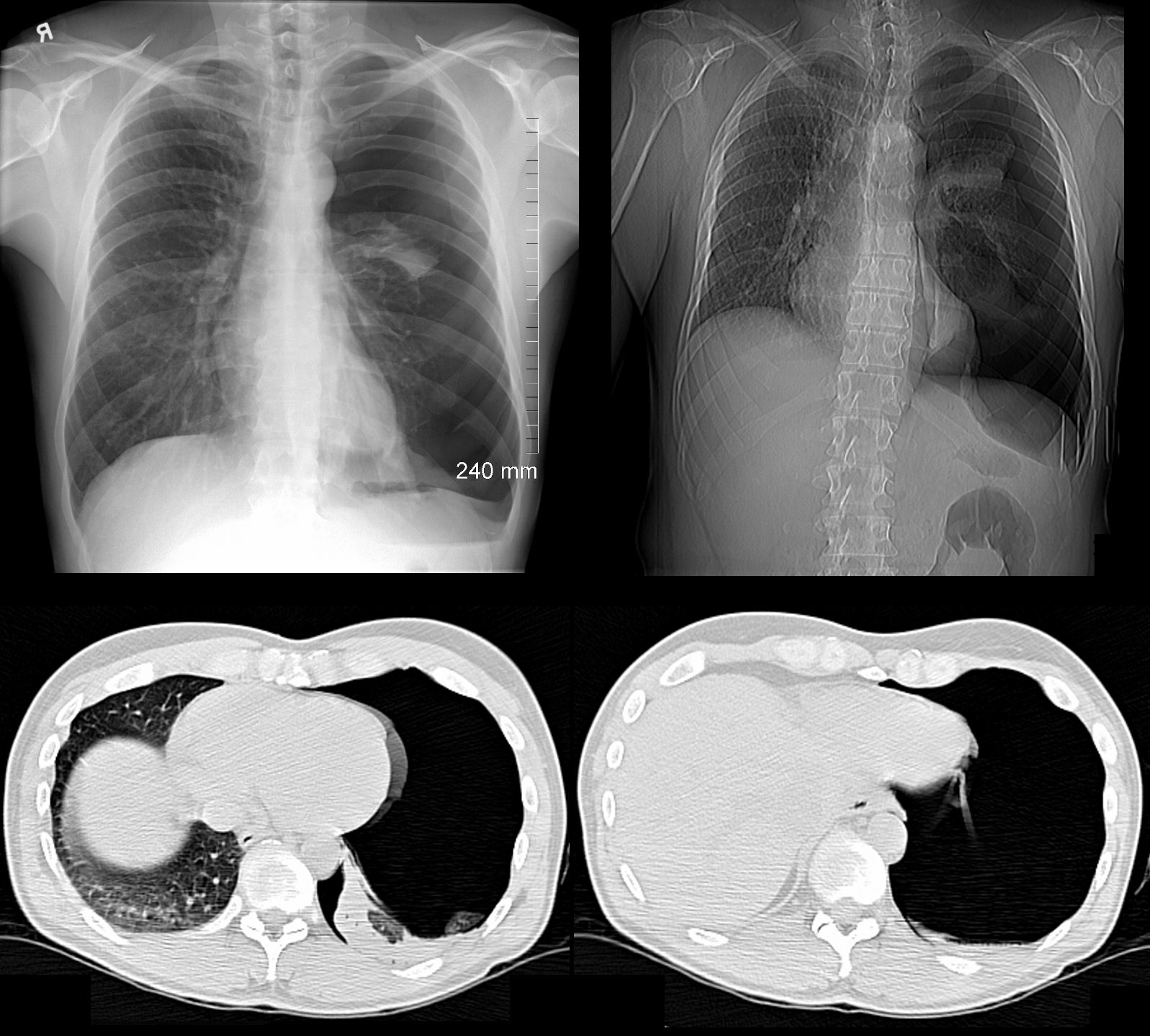
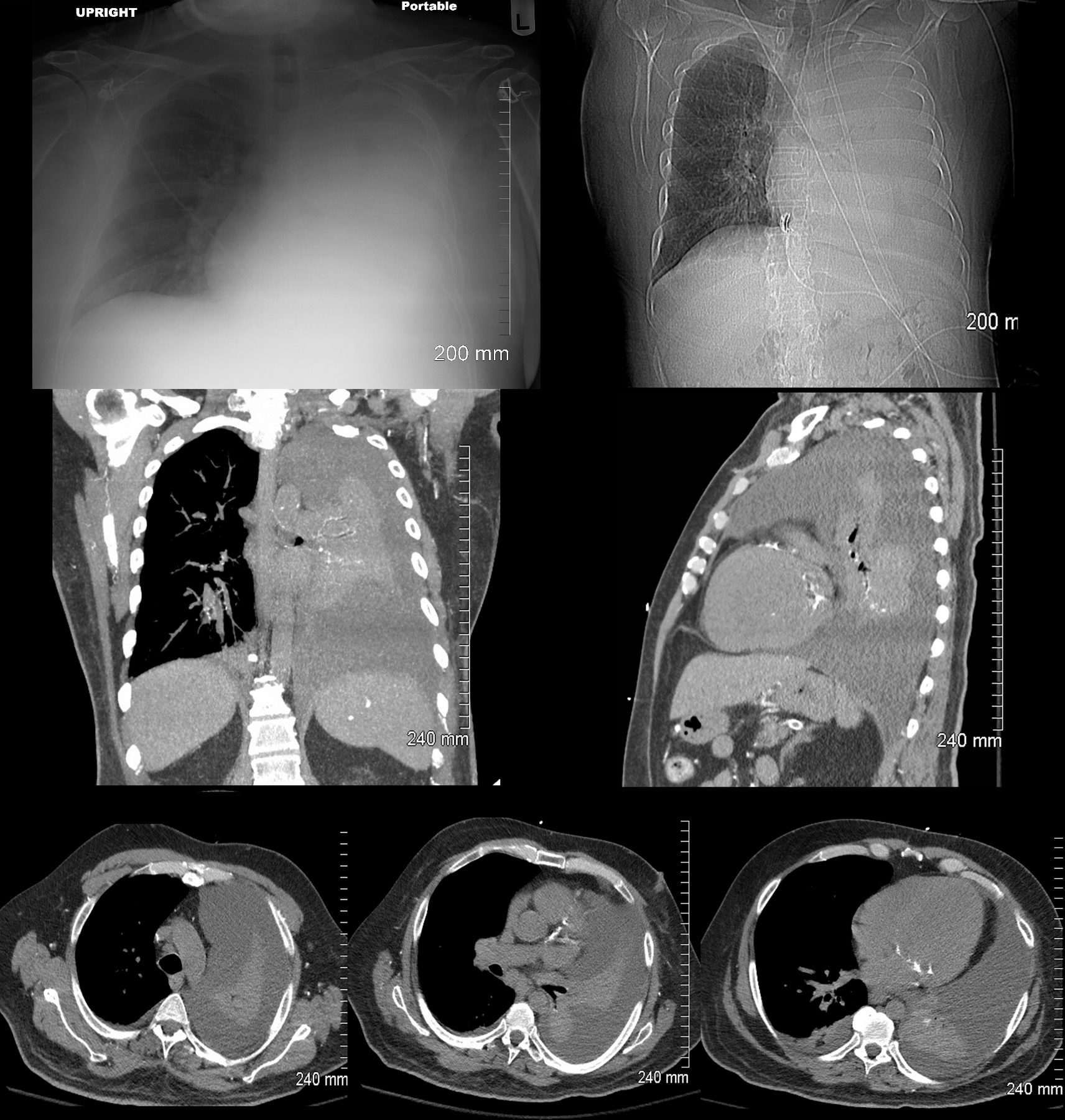
85-year-old female with a history of lung cancer, presents with dyspnea and hypotension. CXR shows white out of the right hemithorax with pressure effect characterised by narrowing of the distal trachea cardio-mediastinal shift to the left and atelectasis in the left lower lobe.
Ashley Davidoff MD TheCommonVein.netSee 106Lu 118468
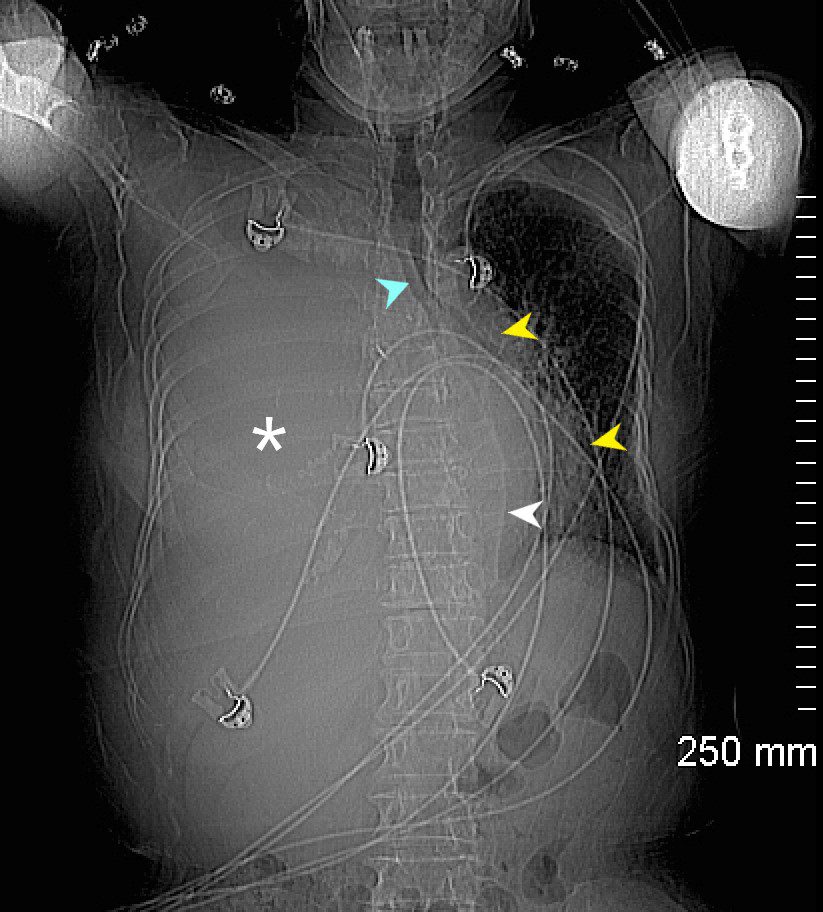
85-year-old female with a history of lung cancer, presents with a dyspnea and hypotension. Scout film prior to the CT scan shows ?white out? of the right hemithorax (white asterisk) with pressure effect characterised by narrowing of the trachea (blue arrow) mediastinal shift yellow arrows) and herniation into the left chest characterised by a leftward shift of the azygo-esophageal junction line (white arrow).
Ashley Davidoff MD TheCommonVein.ne 106Lu 118463L
85-year-old female with a history of lung cancer, presents with a dyspnea and hypotension. CT scan shows a large right pleural effusion under pressure, with mediastinal shift to the right. In addition, there is compression of the heart with back up of venous return due the pressure effect on the heart and vascular structures. Among the structures showing venous distension are the SVC (blue arrowhead, a) right sided upper limb veins (blue arrowhead b) and the left upper pulmonary veins (red arrowhead, b. The effusion in the right pleural cavity with atelectatic lung herniates into the left hemithorax, (white arrowhead, c). There is a dense sediment in the pleural fluid (red arrowhead, d) suggesting blood in the pleural cavity. The left atrium is compressed (maroon arrowhead, d)
Ashley Davidoff MD TheCommonVein.net106Lu 118467c

85-year-old female with a history of lung cancer, presents with a dyspnea and hypotension. Reconstruction of the CT scan in the coronal plane, shows a large right pleural effusion under pressure with herniation into the left chest (white asterisk e,and f) , with mediastinal shift to the left (yellow arrowhead b, c, d). In addition, there is compression of the heart with back up of venous return due the pressure effect on the heart and vascular structures. Among the structures showing venous distension are the SVC (blue arrowhead, c) right sided upper limb veins (blue arrowhead d) and the left upper pulmonary veins (red arrowhead, d and f). The density of the systemic venous abd arterial systems is similar, but vascular structures as noted by the green arrowhead in a could represent venous collaterals.
Ashley Davidoff MD TheCommonVein.ne 106Lu 118467cL
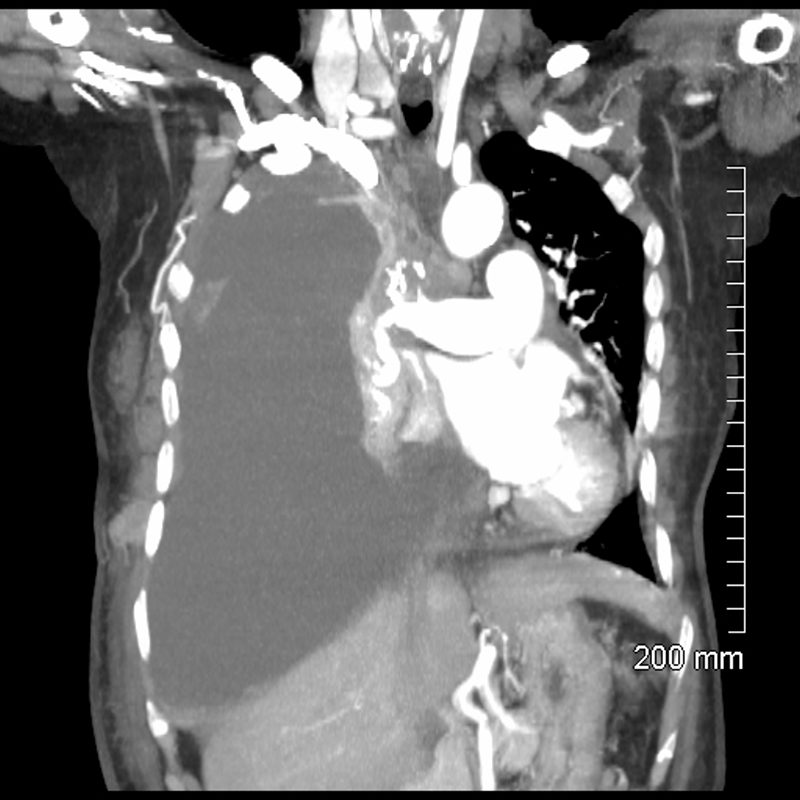
85-year-old female with a history of lung cancer, presents with a dyspnea and hypotension. CT scan shows a large right pleural effusion under pressure, with mediastinal shift to the left. In addition, there is compression of the heart with back up of venous return due the pressure effect on the heart and vascular structures. The effusion in the right pleural cavity with atelectatic lung herniates into the left hemithorax.
Ashley Davidoff MD TheCommonVein.net 106Lu 118467
Coronal CT through the lungs show bilateral pleural effusions with compressive atelectasis
Ashley Davidoff MD TheCommonvein.net
238Lu

Sagittal CT through the left lung shows undulations of the posterior surface of the left lung, and the suggesting differing pressures on the lung parenchyma by the effusions and indicating complexity and loculation.
Ashley Davidoff MD TheCommonVein.net
238Lu
Whole Lung Atelectasis Due to Obstruction
59-F-total-atelectasis-001-1.jpg
59F shows total white out caused by collapse of right lung with an
occluded right main step bronchus associated with a
large right sided effusion. The occlusion is likely due to proximal cancer. A pigtail drain has been placed to drain the effusion
Ashley Davidoff MD TheCommonVein.net 104 Lu
59F shows total collapse of left lung with an
occluded right main step bronchus(top right image)associated with a
right sided effusion. The occlusion is likely due to proximal cancer
Ashley Davidoff MD TheCommonVein.net 104 Lu
Total Lung Compressive Atelectasis
Effusion
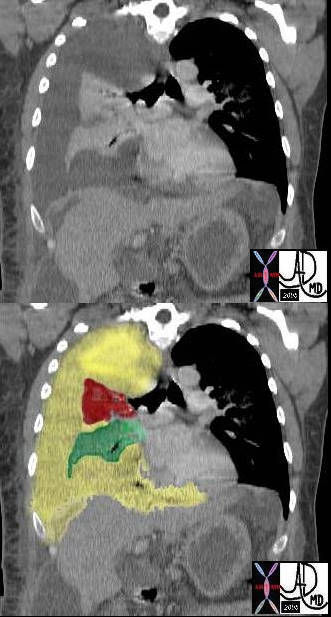
In this case there a large right sided pleural effusion (yellow) with secondary atelectasis of the right lung. (red and green) This coronal CT of the chest at the level of the left ventricle shows a large right pleural effusion which lies between the visceral and parietal pleura. Once the effusion is large enough to weaken the capillary forces that hold the parietal and visceral pleura together, it fail, and the lung collapses which is what is noted on this image ? ie total lung collapse because of loss of cohesive adhesive forces.
Courtesy of: Ashley Davidoff, M.D. TheCommonvein.net 42558c
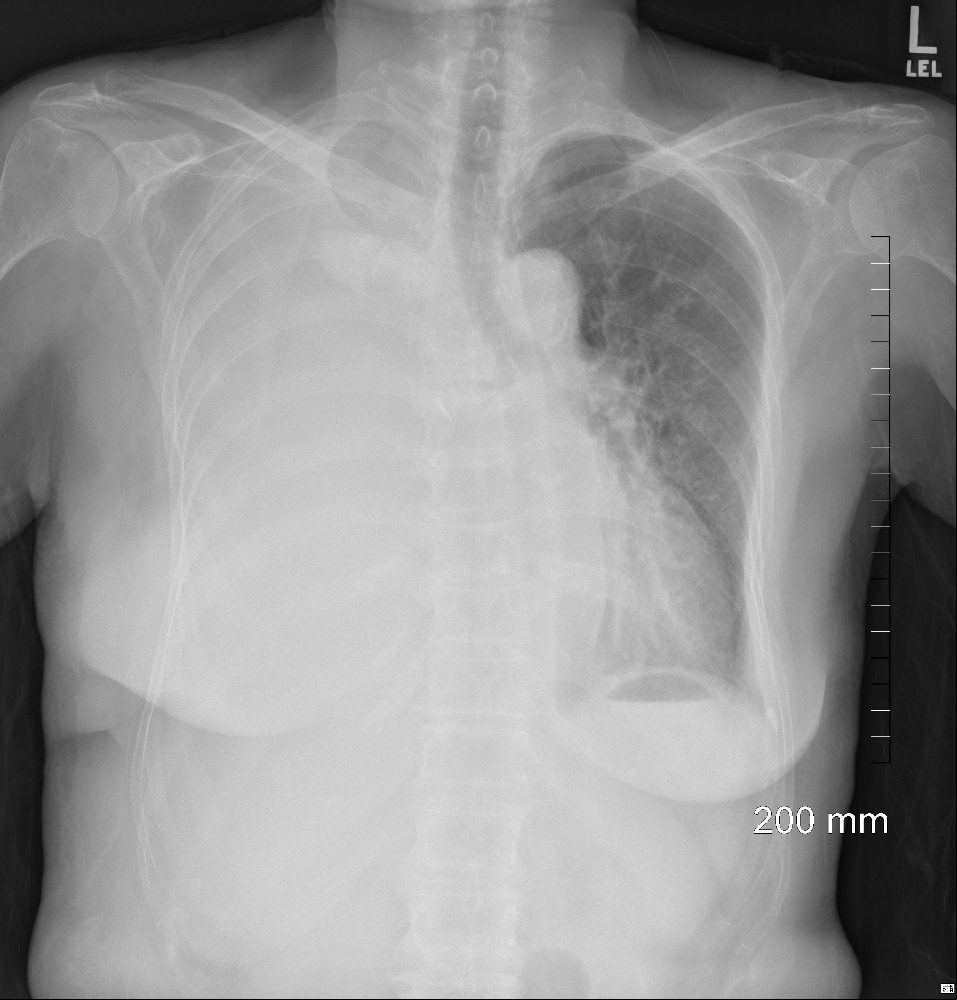
White Out of the CXR with Passive Compressive Atelectasis of the Left Lung
 White Out of the CXR with Passive Compressive Atelectasis of the Left Lung
White Out of the CXR with Passive Compressive Atelectasis of the Left Lung
48 year-old male presents with a dyspnea. CXR shows a total white out of the left chest with pulmonary congestion. CT scan shows a large left pleural effusion with total atelectasis of the left lung. Incidental note is made of premature calcific coronary artery disease.
Ashley Davidoff MD TheCommonVein.net
Links and References
Chat GPT Radiological findings of total lung collapse aka total lung atelectasis