- Diffuse Lung Disease (DLD) refers to a
-
- broad group of pulmonary conditions
- characterized by
- widespread abnormalities affecting the lung parenchyma.
- The term encompasses diseases that
- primarily involve the
- interstitial,
- alveolar, or
- small airway compartments of the lung.
- primarily involve the
-
CXR showing
Extensive Lymphoid Interstitial Pneumonitis

Initial Chest X-ray shows a diffuse reticular pattern with architectural distortion and cystic changes dominant at the bases.
Ashley Davidoff MD TheCommonVein.net 139266 017Lu
CT Correlate
Extensive Diffuse Lung Disease Secondary to LIP
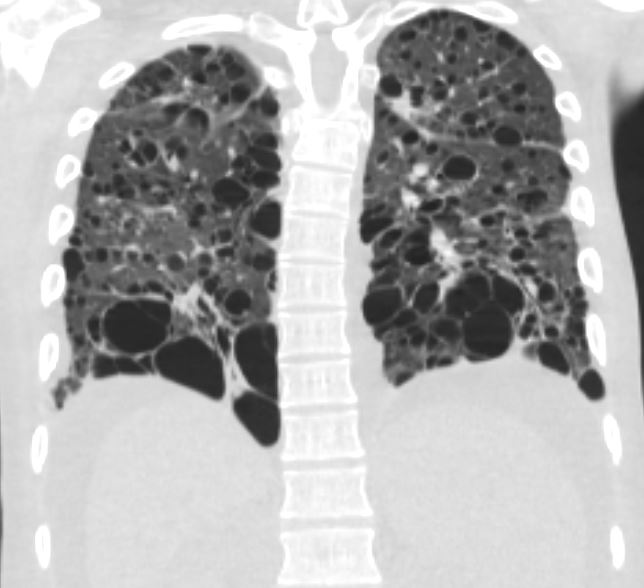
27 year old male with a history of perinatal HIV and lymphocytic interstitial pneumonitis
CT in the coronal plane confirms the presence of diffuse cystic changes with the largest cysts at the lung bases. Ascites and splenomegaly are also present
Ashley Davidoff MD TheCommonVein.net 139268 017Lu
Radiological Definition
Diffuse lung disease is defined radiologically by the presence of widespread, often bilateral, abnormalities on imaging studies (e.g., chest X-ray or CT), involving one or more of the following patterns:
- Reticular Pattern:
- Linear or curvilinear opacities forming a net-like appearance.
- Associated with interstitial thickening or fibrosis.
- Nodular Pattern:
- Multiple small, discrete round opacities.
- Can be distributed in a centrilobular, perilymphatic, or random pattern.
- Ground-Glass Opacities (GGO):
- Hazy increased opacity of the lung parenchyma with preserved bronchial and vascular markings.
- Suggests partial alveolar filling or interstitial thickening without complete consolidation.
- Consolidation:
- Homogeneous increase in lung parenchymal density obscuring bronchial and vascular structures.
- Indicates complete alveolar filling.
- Honeycombing:
- Clustered cystic airspaces of similar diameters, usually subpleural and basal in location.
- Hallmark of advanced fibrosis.
- Cystic Changes:
- Thin-walled air-filled spaces, often with a predilection for specific areas based on the disease.
Common Causes
- Interstitial Lung Diseases (ILDs):
- Idiopathic pulmonary fibrosis (IPF), hypersensitivity pneumonitis, sarcoidosis.
- Airway-centric Disorders:
- Bronchiolitis, chronic obstructive pulmonary disease (COPD).
- Alveolar Diseases:
- Pulmonary edema, alveolar hemorrhage, or organizing pneumonia.
- Infectious Diseases:
- Miliary tuberculosis, fungal infections.
- Systemic Diseases with Pulmonary Manifestations:
- Rheumatoid arthritis, systemic lupus erythematosus.
Imaging Modalities
- Chest X-Ray:
- Initial screening tool; may show reticular or nodular opacities, ground-glass changes, or reduced lung volumes.
- High-Resolution CT (HRCT):
- Gold standard for detailed characterization of diffuse lung diseases.
- Helps identify specific patterns and distribution to narrow the differential diagnosis.
Radiologists play a critical role in recognizing these patterns, correlating imaging findings with clinical history, and suggesting possible diagnoses.
Diffuse Alveolar Damage (DAD) is a pathological pattern of lung
injury characterized by widespread damage to the alveolar
structures, often seen as the hallmark of acute respiratory distress
syndrome (ARDS). It can result from various causes, including
infections, sepsis, trauma, or inhalation of toxic substances. The
pathogenesis involves an initial injury to the alveolar-capillary
barrier, leading to fluid leakage into the alveolar spaces,
inflammation, and subsequent formation of hyaline membranes
within the alveoli. Over time, this causes fibrosis and thickening of
the alveolar walls, severely impairing gas exchange. Clinically, DAD
presents with symptoms such as acute shortness of breath, low
oxygen levels, and respiratory failure. Diagnosis is based on clinical
findings and imaging, where chest X-rays or CT scans reveal
widespread ground-glass opacities and consolidations.
Pathological confirmation via lung biopsy shows the characteristic
hyaline membranes and alveolar collapse. (Etesami)
