Learning Objectives
Describe the basic anatomy including the fundus, body, cervix and Fallopian tubes
Discuss the physiology of the uterus
Describe the endometrium, the myometrium, and the serosa
Locate and identify the structures
Definition
The uterus, also known as the womb, is a hollow muscular organ that is part of the genitourinary system.
It is characterized by its important role in the female reproductive system.
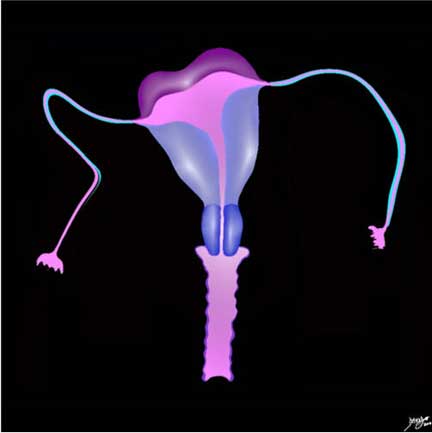
Structurally, it is characterized by its pear shape and its unique muscular structure that undergoes profound changes during different reproductive events. Though it is a pelvic structure, it enlarges many times over to become an intra-abdominal organ during pregnancy and returns to its pre-pregnancy state after child birth. Superiorly, the gracile fallopian tubes open on each side into uterine cavity, and inferiorly it communicates with the vagina through the cervix. The urinary bladder lies anterior to it and the rectum is posterior to it.
Functionally, it provides a nutritional and protective environment for a fertilized embryo to embed, and accommodates a growing embryo until child birth.

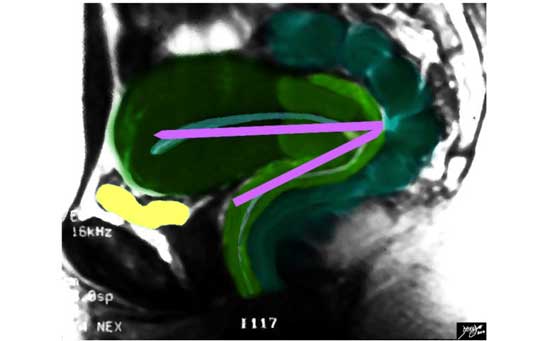
The sagittal diagram of the uterus and vagina shows an anteverted uterus. In this view the uterus, vagina, and the internal cavity starting in the endometrial cavity, coursing through the cervix and then into the collapsed vaginal cavity is exemplified.
Ashley Davidoff MD
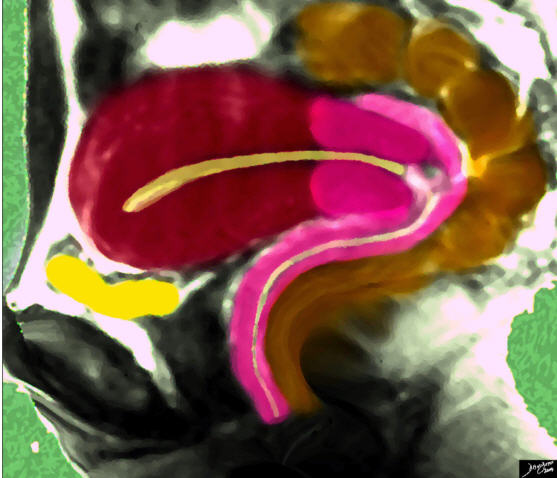
The sagittal diagram of the uterus shows the uterus surrounded by its neighbors, including the empty bladder (yellow) that lies anteriorly and inferiorly and the rectosigmoid colon (brown) that lies superiorly and posteriorly.
Ashley Davidoff MD
The Fallopian tubes are gracile structures that are only appreciated by hysterosalpingography, though when enlarged are also seen by other imaging modalities.

This hysterosalpingogram is from a 26-year old female with a normal endometrial cavity and cervical canal. Note the irregular shape to the cervical canal while the endometrial lining is smooth. Note also the free spillage of contrast from the tubes into the peritoneal cavity (white contrast in a), indicating patent tubes.
Endometrial cavity (rust), cervical canal (pink) and fallopian tubes (orange/yellow)
Images courtesy of: Ashley Davidoff, M.D.
Overview
Structurally, in the non gravid state, the mature uterus is about the size of a woman’s fist, and measures about 8cm X 6cm X 4cm with a volume of about 75-200 ccs, and it weighs 100-200gms. It is a pear or pyriform-shaped muscular organ and is situated between the bladder anteriorly and the rectum posteriorly. It is a muscular organ with a hollow; endometrial cavity. Superiorly the fallopian tubes open on each side into the uterine cavity; inferiorly it communicates with the vagina via the cervix. It consists of a fundus, body (corpus), and neck (cervix).
Histologically, the inner endometrial lining consists of a single layer of columnar cells supported by a thin layer of connective tissue. The middle layer is the thickest and is called the myometrium. It consists of smooth muscle and has different layers with various orientations of the fibers. The myometrium proliferates during pregnancy. There is a loose connective tissue layer next which is called the perimetrium and then the outer lining which is a cover and is called the peritoneum and is part of a serosal layer. The cyclical changes of the menstrual cycle present a continual change of events controlled by a series of integrated hormonal events. During the follicular phase (proliferative phase) which occurs in the first half of the cycle and after the shedding of the endometrial lining, there is a rise in estrogen which causes the endometrial lining to start to thicken. In mid cycle after ovulation, luteinizing hormone is released which heralds in the luteal phase (also know as (aka) the secretory phase). Progesterone now rises and further proliferation of the endometrium occurs. In the absence of pregnancy progesterone and estrogen levels fall and the endometrium sheds.
In Part 2 of Applied Anatomy of the Uterus, we will cover disease processes and diagnosis. Common diseases include alterations in the structure which can be congenital or acquired, benign or malignant tumors.Systemic disease, especially infections, can also affect the uterus and uterine cavity. Diseases include fibroid disease, polyps, adenomyosis, cervical stenosis, and carcinoma. The more common disorders are the functional disorders that relate to cyclical events including menstrual cramps, endometriosis, dysmenorrhea, amenorrhea, and menorrhagia. Pain relating to the placement of an intrauterine device is also relatively common.
The developmental uterine anomalies may hinder conception and normal child birth. The changes in position could give rise to chronic pelvic pain. During childbirth there is a risk of injury to the urinary bladder as well as the anal sphincter as the uterus is anatomically closely related to these structures. The uterus may lose its support with age, repeated pregnancies and post menopause and may give rise to uterovaginal prolapse. Uterine fibroids are most common benign tumors arising from the uterine myometrium. Uterine endometrium can stray and become ectopically placed in the myometrium giving rise to adenomyosis and when positioned in the ovaries or pelvis causing a condition called endometriosis.
The diagnosis of uterine diseases is dependent initially on clinical evaluation, while the most useful imaging modality is ultrasound. Clinically, symptoms include infertility, recurrent abortions, menorrhagia, acute or chronic abdominal pain and urinary complaints. The imaging modalities commonly used include ultrasound, MRI, hysterosalpingography, hysteroscopy and diagnostic laparoscopy.
Treatment options are guided by the disease process and may include hormonal treatment, minimally invasive surgery or open surgery.
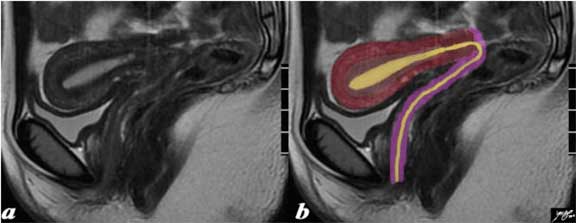
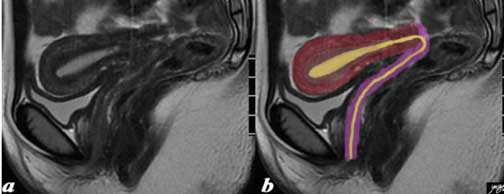
The normal sagittal view of the uterus is a T2-weighted MRI from a 16-year-old female with pelvic pain. It demonstrates that the uterus and more specifically the myometrium is more complex and consists of an outer part (dark red) and an inner, more homogeneous part called the junctional zone. Since a T2-weighted image is sensitive to water, we understand from this image that the outer part, since it has a greater white signal, contains more water and likely more vascularity. The endometrial canal, cervical canal and vaginal cavity are outlined in yellow and the vaginal wall is pink. Courtesy of: Ashley Davidoff, M.D.
Principles of the Uterus
The uterus is a muscular, pyriform structure specifically designed structurally and physiologically to allow implantation of the embryo and to accommodate a growing fetus until childbirth. The stroma and muscle develop from surrounding mesoderm. The uterus undergoes many changes during a woman’s lifetime, especially during pregnancy and childbirth. After menopause it becomes atrophic and may lose its support resulting in prolapse.
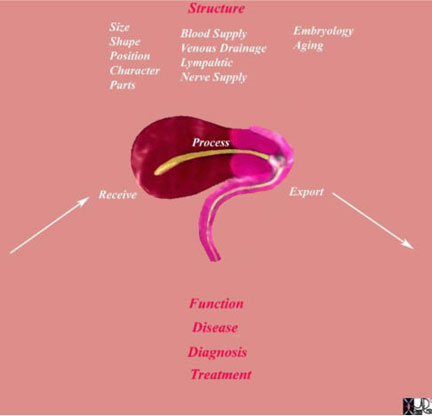
This diagram frames the underlying principles and approach to the uterus in this module. Since the uterus is a biological structure, its morphological characteristics are defined by its size, shape, position and character. As a biological unit it needs to be connected with other structures and it does this via blood vessels, lymphatics and nerves. It functions with the basic notion that it receives processes and exports its product. All structures, whether they are the smallest cell to the largest organ, work in the same way. They receive, process and export their product. Biological structures are subject to disease which may affect structure and or function. We use diagnostic methods to identify aberrant structure and or function and we apply therapeutic regimens to correct aberrant structure and function.
Ashley Davidoff MD
Principles of the Uterus: Basic Universal Principles
There are some basic, universal principles that apply to all living structures (also known as biological units) whether they are a cell or a person and they apply equally to the organ under consideration ? the uterus. These include the need to be functionally and structurally independent, but they need to also be linked to other structures in order to survive. All biological structures undergo change with time, need to occupy space, require an ability to convert one form of energy to another and apply or invoke certain forces to perform their functions.
As a Biological unit
The uterus is an important reproductive organ and has unique features like its lining of endometrium that changes with each menstrual cycle to allow implantation of the fertilized embryo and the criss-cross myometrium to stretch to accommodate a growing fetus. The criss-cross myometrium also acts as living ligatures to minimize blood loss during and after child birth. The fallopian tubes act as a conduit for the unfertilized ovum to be transported to the endometrial cavity to enable fertilization.
Dependence and Independence
The uterus, along with the ovaries form the female reproductive system which is an independent unit. However, the function of the uterus is under a complicated system of hormones which are secreted by the ovaries which in turn are controlled by the pituitary hormones. Some pituitary hormones also have a direct effect on the uterus. This constitutes a pituitary-ovarian-uterine axis.
Links and Connections
The uterus is connected to the fallopian tubes superiorly and to the vagina inferiorly. It is a pelvic organ and lies between the urinary bladder anteriorly and the rectum posteriorly. It has an independent blood and lymphatic supply. It has unique ligaments and a muscular sling that helps in maintaining its position and preventing uterine prolapse. It is intimately connected to the endocrine system via circulating hormones, particularly estrogen and progesterone.

The image shows some of the structures in the body that are functionally and structurally linked to the uterus in order for it to function as an integrated organ. The brain (purple) reigns supreme and is responsible for the neural axis, the pituitary (orange) and ovary (black and gray) for the hormonal axis. The vascular axis is exemplified by the arteries and veins (red and blue) while the lymphatic connections are outlined in yellow.
Ashley Davidoff MD
Time Growth and Aging
During organogenesis a pair of Mullerian ducts arise from coelomic epithelium and subsequently fuse to form the uterus. The proximal portions form the fallopian tubes and distal portions form the body and cervix of the uterus and upper 4/5ths of the vagina.
Spaces
The non gravid uterus is a pelvic organ. However, a gravid uterus becomes an abdominal organ occupying a large area in the abdomen almost up to the tip of the xiphisternum at term. It is also only partially covered by peritoneum on its superior aspect.
Forces
Uterine contractions can occur in the non pregnant state. During the menses, contractions occur to help eject the shedded endometrium. During pregnancy the uterus undergoes painless contraction called Braxton Hicks, which increase as the pregnancy advances. During parturition, uterine contractions have two separate effects in the upper uterine segments. There is one set of contractions which gradually create a downward force and shortening of the muscle fibers which tend to get smaller by a process called retraction, causing descent of the fetus and rotation of the fetal head. The second effect is on the cervix and lower uterine segment which dilates as the upper uterine segment contracts.
Interactions
The uterus, ovaries and pituitary form a sophisticated unit playing an important part in ovulation, conception and child birth. The uterus, along with the fallopian tubes and cervix are the structural pillars of this unit.
State of Health and Disease
Uterine problems are very common, manifesting as fibroid disease, dysfunctional uterine bleeding, structural anomalies and uterovaginal prolapse.

Life depends on the uterus. The uterus is the ultimate organ that enables the survival of the human race. It houses, protects and nourishes the fetus for approximately 9 months and bears its fruit by delivering its product through the use of strong muscular forces. Images courtesy of: Ashley Davidoff, M.D.
Structure of the Uterus
The uterus is a hollow, muscular structure consisting macroscopically of a fundus, body, cervix and Fallopian tubes, continuing above with the peritoneal cavity and below with the vagina. As a hollow, muscular organ it conforms to a basic histological pattern of all the hollow organs. In pursuit of understanding the structure of the uterus, we will initially explore its histological makeup and then progress to the anatomy and physiology. Finally we will explore disease entities as they apply to the anatomy, histology and physiology. Entities such as the menstrual cycle and pregnancy have implications at the histological, anatomical, physiological and at the level of diseases. These aspects are repeated from the different perspectives of histology, anatomy, physiology, imaging and disease.
Structure of the Uterus: Histology
The uterus has three basic histological layers:
endometrium – (also known as the mucosa) which is the inner layer abutting the lumen
myometrium – which is the middle and thickest layer
serosa – the superficial layer
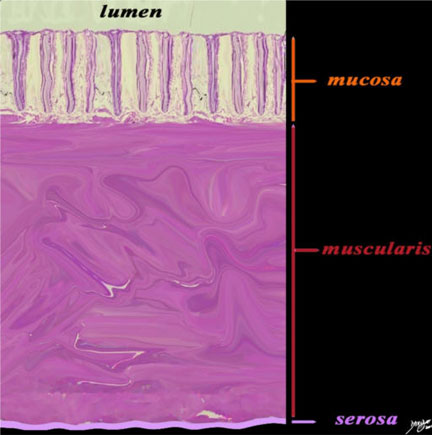
The wall of the uterus contains three basic layers: the mucosa, the muscularis and the serosa as demonstrated in this artistic rendition of the wall of the uterus in the premenstrual phase. Courtesy of: Ashley Davidoff, M.D.
Structure of the Uterus: Endometrium (Mucosa)
The endometrium is a dynamic structure and in the reproductive female is turned over every thirty days. It is subject to the influences of the hormonal changes of the menstrual cycle.
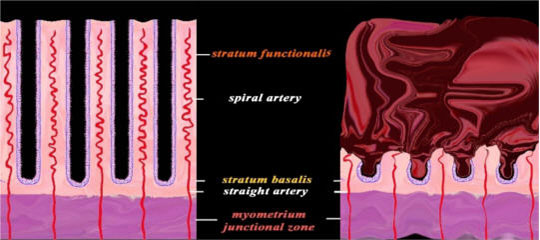
The endometrium is divided into two zones: a thinner basal layer called the stratum basalis and a thick superficial functional layer called the stratum functionalis.
The stratum functionalis is considered a temporary tissue and since it comes and goes in 28 days it has an “unfinished” appearance. The stroma resembles embryonic tissue and does not have a characteristic appearance of a lamina propria.
The stratum basalis has a more permanent appearance characterized by mature appearing stromal tissue, together with the deep tips of the glands.
The epithelium (or cellular lining) is made of simple tubular glands that dip down like test tubes into the stroma. The epithelium contains ciliated columnar cells and secretory cells embedded in a highly cellular, connective tissue with numerous lymphatics, vessels and uterine glands. The mucosa folds inward to form simple, tubular, uterine glands that extend deep into the stroma.
The stroma consists of vessels, lymphatics and connective tissue.
During the cycle, both the epithelium and the stroma undergo significant change. At the time of menstruation the superficial functional layer, which is sensitive to hormonal influences, sloughs and the basal layer remains intact to enable regeneration during the next cycle.
The mucosa continues into the Fallopian tubes and opens into the peritoneum. It also continues downstream into the vagina through the external os.
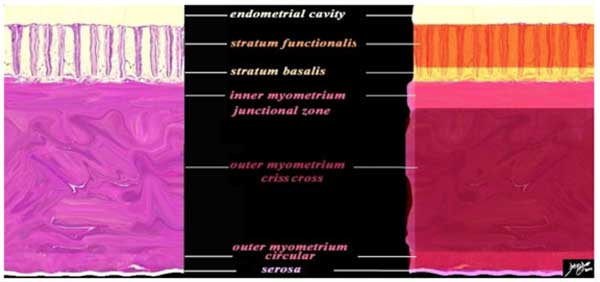
The diagram typifies the histological appearance of the wall of the body of the uterus with other parts that are subdivisions of the three basic parts. The mucosa has two layers: the superficial functional layer called the stratum functionalis and a deeper basal layer called the stratum basalis. The mucosa contains deep, simple, tubular glands embedded in a matrix (cream). The muscularis ? (pink) consists of three layers: the subendometrial, junctional zone organized in a circular fashion and an outer myometrium which has two layers. The middle zone with criss-cross pattern is the thickest and the thin, circular, outer zone. On the surface the thin serosa (mauve) acts as a capsule for the uterus and a lining for the endometrial cavity. Courtesy of: Ashley Davidoff, M.D.
Structure of the Uterus: Simple Tubular Glands
A single layer of ciliated, columnar cells line the glands of the endometrium. They are cemented to the stroma by a basement membrane.
The stratum functionalis is the layer that sheds at menstruation and the stratum basalis remains to assist in the regrowth of the stratum functionalis. The spiral arteries run within the stratum functionalis and are the potential nourishment for the implanted fertilized egg if pregnancy occurs. They are branches of the arcuate arteries.
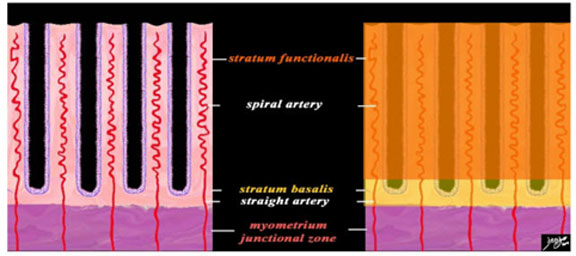
A closer view of the endometrium as seen in the premenstrual phase, exemplified by the characteristic spiral (helical) arteries running in the stroma (pink) between the simple, tubular, test tube shaped glands (purple). The spiral arteries supply the functional layer (stratum functionalis – deep orange) and the straight arteries supply the basal layer (stratum basalis- light orange). Beneath the basal layer is the myometrium and the subendometrial smooth muscle or junctional zone (dark pink).
The other structures that run in the stroma between the tubular glands are the veins and lymphatics.
Ashley Davidoff MD
Structure of the Uterus: Cyclical Changes of the Endometrium
The three major phases of the cycle that manifest in the endometrium are the proliferative (follicular), secretory (luteal), and menstrual phases. The follicular phase occurs just after the shedding of the endometrium ending with ovulation and is followed by the secretory phase. The secretory phase is the period that follows ovulation preparing the uterus for implantation, and ends with the menstruation or the menstrual phase if implantation does not occur.
The diagram reflects the premenstrual endometrium (left) and the post menstrual endometrium right, revealing the necrosis of the functional layer with sloughing and hemorrhage. The basal layer with the straight arteries and a small portion of the spiral artery remains intact. The hemorrhage is controlled by spasm of the arteries and contraction of the myometrium. Courtesy of: Ashley Davidoff, M.D.
In the cervix the mucous membrane is sharply differentiated from that of the uterine cavity. The cervical mucosa is thrown into numerous oblique ridges. The mucous membrane secretes a clear, viscid alkaline mucus. The upper two thirds of the cervix is composed of a ciliated, cylindrical epithelium which gradually transforms into stratified, squamous epithelium. On the vaginal surface of the cervix the epithelium is similar to the vaginal epithelium.
Structure of the Uterus: The Muscular Layer
The muscular layer forms the bulk of uterus. It is thick in the fundus and the middle part of the body and thin at the entry point of the Fallopian tubes. There are three component muscular layers: internal, middle, and external.
The internal or deep layer is like muscularis mucosa; the fibers are arranged in circular fashion like two hollow cones with apices at uterine tube orifices and bases intermingling in the middle of the body. The fibers at the internal os are arranged in circular fashion like a sphincter.
The middle layer has no regular arrangement of the fibers; they are disposed longitudinally, obliquely and transversely in criss-cross fashion. This layer has the largest number of blood vessels. After parturition, these layers act as living ligatures and limit blood loss.
The external layer consists of fibers which pass transversely across the fundus and converge at each lateral angle of the uterus. They continue on to the Fallopian tube, the round ligament, and the ligament of the ovary. Some of the fibers pass on each side into the broad ligament, and some continue backward from the cervix into the sacrouterine ligaments.
During pregnancy the muscles undergo both hyperplasia (more smooth muscle cells) and hypertrophy (larger muscle cells).
Structure of the Uterus: The Serosa
The serosa does not cover the uterus completely. It is derived from the peritoneum; it invests the fundus and the whole of the posterior intestinal surface of the uterus, but covers the urinary bladder surface only as far as the junction of the body and cervix. In the lower fourth of the posterior surface, the serosa is loosely attached to the uterus separated by connective tissues. The reflection of intestinal peritoneum from the uterus to the intestine forms the pouch of Douglas. This is the area where a pelvic collection, such as an abscess, can accumulate and can be drained vaginally.
The Anatomy – Parts
The uterus is divided into two parts by a constriction called isthmus, midway between apex and base. The portion above the isthmus is called corpus or body of the uterus and the portion below the isthmus is called the cervix. The isthmus corresponds to the internal orifice of the uterus. The portion of the body above the opening of the fallopian tubes is called the fundus.
Conceptual Framework
The conceptual framework provides a simple framework from which to start understanding the structure of the uterus. Simple lines and vectors are used much like the initial foundation or a framework of a building on which the detail will be built.
Coronal Plane
In the coronal plane the uterus has features reminiscent of the letter “T”.
The ?T? can be further subdivided into 3 main parts including the fundus superiorly, the body, and the cervix inferiorly. The fundus is connected to the fallopian tubes and the cervix to the vagina.
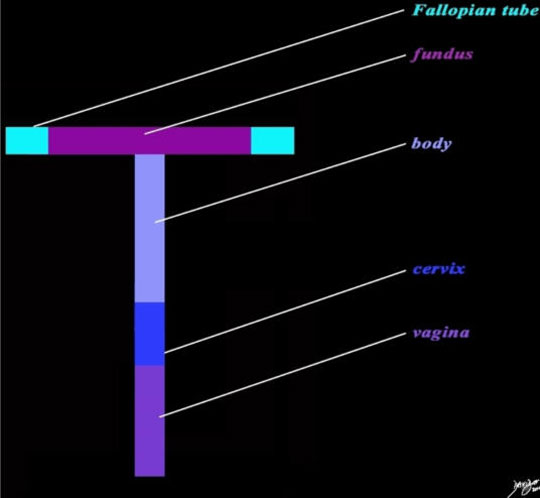
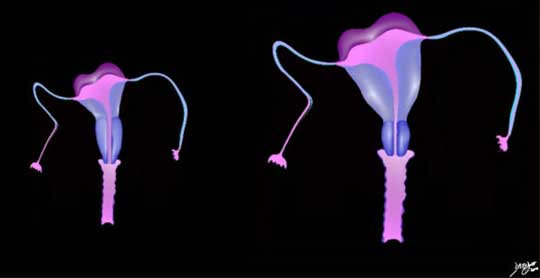
The diagram reflects the “T” shaped structure of the uterus as well as the component parts including the fundus (dark pink) the body (light purple), and cervix (royal blue). The Fallopian tubes (teal) at the upstream end, and the vagina at the downstream end (purple) complete the tract of the genital tract. Courtesy of: Ashley Davidoff, M.D.
The form of the uterus and genital tract is more complex than a simple foundation ?T? shape, being broad and muscular and triangular in form in the body region, cylindrical and fibrous in the cervical region and having thin and delicate Fallopian tubes.
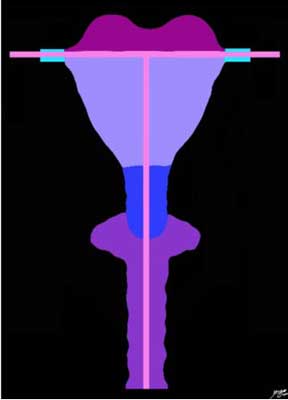
The diagram reflects the “T” shaped structure of the uterus, the component parts, and the tract (light pink) starting from the vagina (purple and extending through the uterus and Fallopian tubes (teal). The form of the structures surrounding the tract have been expanded to their relative dimensions and shapes. The upper part consisting of the fundus (maroon) and body (mauve) are muscular and triangular, while the lower cervix is cylindrical and fibrous (royal blue). Where the apex of the body meets the cervix is called the isthmus. The genital tract (pink) starts with the vagina at the downstream end (purple), is relatively capacious, but is generally collapsed, continues into the narrow lumen of the cervix (royal blue), then into the more capacious endometrial cavity within the body (mauve) and fundus and exits out into each of the Fallopian tubes (teal) at the upstream end. Courtesy of: Ashley Davidoff, M.D.
The diagram reflects the “T” shaped structure of the uterus and the genital tract. The form of the structures and the tract have been expanded to their relative dimensions and shapes. The uterus and fallopian tubes are quite mobile and flop forward and backward. The uterus and cervix usually flop forward, and this position is called anteverted.
The genital tract (pink) starts with the vagina at the downstream end (purple), is relatively capacious, but is generally collapsed, continues into the narrow lumen of the cervix (royal blue), then into the more capacious endometrial cavity within the body (mauve) and fundus and exits out into each of the Fallopian tubes (teal) at the upstream end.
Ashley Davidoff, M.D.
In the Sagittal Plane
In the sagittal plane the uterus has a structure reminiscent of an “L”.
The Anatomy – Parts : Applied Anatomy
This section combines the anatomy of the uterus with images as viewed with imaging including ultrasound, CT and MRI. The sagittal view consistently provides an excellent overview of the uterine size, shape and position.
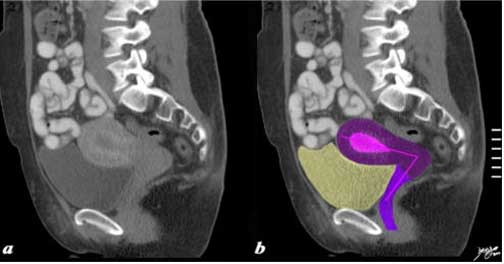
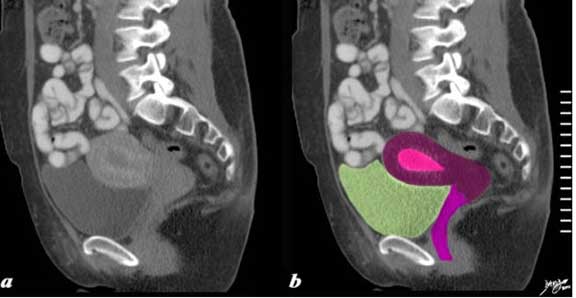
This sagittal reconstructed CT shows an anteverted uterus buoyed and cushioned by a partly filled bladder (yellow). In this sagittal view of the uterus an ?L? shaped structure, the vagina and the internal cavity is diagrammed in by the pink vectors of the tract. Courtesy of: Ashley Davidoff, M.D.
The fundus and body of the uterus (also known as corpus uteri) form the largest portion of the uterus which gradually narrows to meet the cervix inferiorly.
The anterior surface is flattened and covered by peritoneum which reflects onto the bladder to form the vesicouterine space. The intestinal or posterior surface is convex transversely and is covered by peritoneum down to the cervix and vagina. Between the posterior surface of the uterus and the rectosigmoid colon is the pouch of Douglas, also called the cul de sac. It is the most posterior and inferior space in the abdomen and the place where fluid first collects when the patient is in the supine or upright position. The lateral margins of the uterus are usually convex. At the upper end of each lateral margin, the fallopian tubes, the uterine wall, below and in front of it, is the attachment of round ligament, while posterior to it is the attachment of the ligament of ovary. The peritoneum is reflected off the uterine wall and invests the fallopian tubes. These folds are called the broad ligaments.
The Anatomy – Parts : Endometrium
The endometrium is a dynamic structure subject to the fluxes of the hormones. Its size and character varies with age, being thin in the young prepubertal female and in the elderly postmenopausal female. In the female of reproductive age, it ranges in size between about 2-3 mm in the post menstrual phase up to 16 mm in the premenstrual phase about 28 days later.
The endometrium is best evaluated using ultrasound for its macroscopic in vivo evaluation. In the young and old it is echogenic and with proliferation and accumulation of secretions in the glands, it initially becomes trilaminar. Following ovulation it becomes homogeneously echogenic.
In the postmenopausal female it should not measure more than 4 mm on ultrasound. There are profound changes in the endometrium during the menstrual cycle and pregnancy and these in part have been discussed in the histology section and will be revisited in the menstrual cycle section.
The Anatomy – Parts : Myometrium
The myometrium, the middle and thickest layer as stated consists of three layers:
the internal or deep layer is like muscularis mucosa. The fibers are arranged in circular fashion.
the middle layer is the thickest layer and the fibers are arranged in criss cross fashion.
the external layer consists of fibers which pass transversely across the fundus and converge at each lateral angle of the uterus.
From an imaging perspective two major layers are identified: the sub-endometrial layer (also known as the junctional zone) and the thicker outer layer.
The junctional zone is sub-endometrial smooth muscle that is more compacted and contains less water in comparison to the outer myometrium. (McCarthy)
The junctional zone is also functionally different from the outer myometrium. For example, myometrial contractions in a non-pregnant woman originate exclusively from the junctional zone. The amplitude, frequency, and direction depend on the phase of the menstrual cycle.

The sagittal STIR sequence from an MRI study shows the normal appearance of the uterus in a 34-year-old female. The pear-shaped form is exemplified together with the three parts of the uterus: the inner endometrium of intermediate signal, the junctional zone of low signal consisting of compacted smooth muscle with low water content and the surrounding myometrium of smooth muscle with a higher water content.
Ashley Davidoff MD
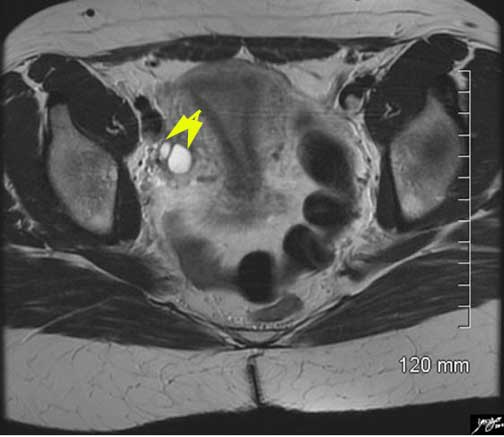
The axial STIR sequence from an MRI study shows the normal appearance of the uterus in a 34-year-old female. Because the uterus is anteverted it lies flat, so that in this instance, the coronal plane of the uterus is demonstrated. The pear shaped form is exemplified together with the three parts of the uterus. Two high signal cysts (yellow arrows) are seen in the right ovary.
Ashley Davidoff MD

Junctional Zone Prominent In Early Proliferative Phase
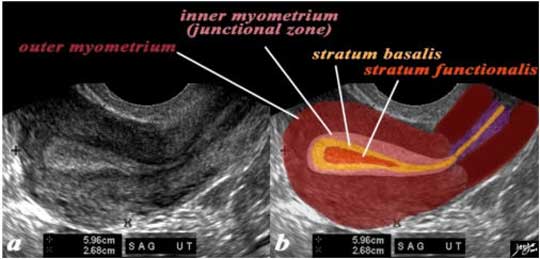
The normal sagittal view of the uterus is a transvaginal ultrasound in the first week after menstruation and just prior to the next proliferative phase. It demonstrates that the endometrium becomes a single, echogenic line consisting of opposing walls (orange) and is surrounded by a subendometrial halo of the junctional zone (reddish). This layer is more compacted and relatively hypovascular and is under the influence of progesterone which has just passed its peak. This image is typical of the early proliferative phase. It is during this time that estrogen starts to rise and progesterone has just fallen. The endometrium in this case measures about 3 mms.
Ashley Davidoff MD
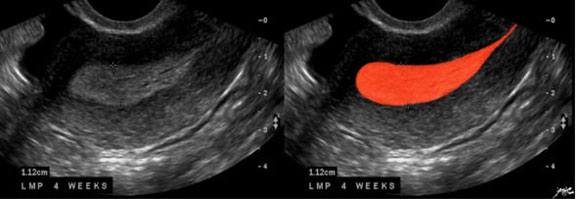
Last Monthy Period 4 Weeks Prior
In this 26-year-old premenstrual female a transvaginal ultrasound in the sagittal plane reveals a normal view of the uterus with characteristic premenstrual appearance (a). The stripe is almost homogeneously echogenic and thick but also shows a hypoechoic halo of the junctional zone or inner myometrium (salmon). The homogeneous stripe is made up from two histological layers (barely distinguished by this ultrasound) ? the inner stratum functionalis (deep orange) that will shed once the spiral arteries vasoconstrict and the outer stratum basalis (deep yellow) that will not shed and will be the basis for regenerating the endometrium in the next cycle. The next layer as stated above is the compact myometrium – the junctional zone (also known as the inner myometrium) and is followed by the thicker outer myometrium (maroon) (b).
Images courtesy of: Ashley Davidoff, M.D.
The Anatomy – Parts : Fallopian Tubes
The Fallopian tubes (also known as the salpinges, oviducts) are a pair of tubular structures that are part of the female reproductive system and also part of the genitourinary system. They are characterized by their delicate and gracile nature and functional importance in fertilization.
Structurally, they are usually about 10 cm long (range 7-14 cm) and are funnel-shaped. The widest portion of the funnel is situated laterally, is called the infundibulum and is open to the peritoneal cavity. The fimbriae are delicate finger-like processes that surround the opening. Medial to the infundibulum is the middle and longest portion called the ampulla. It continues to taper as it progresses medially and it takes up half the length of the tube with a maximum outer diameter of 1-2 cm. More medial to the ampulla is the isthmus which is also slightly tapered, constitutes about 1/3 of the length and has an outer diameter of 0.5 to 1 cm. There is a 1 cm long medial intramural portion of the tube called the interstitial portion or cornual portion that connects the tube to the uterus and has an internal diameter of 1 mm.
Histologically, the tubes are structured like many other tubular organs of the body. There are three layers: an inner mucosa, intermediate muscular layer and an outer serosa which is continuous with the peritoneum.
Functionally, the tubes act as the site which allows fertilization to take place and also acts as the transport system that carries the fertilized egg (gamete) to the uterus.
Common diseases include pelvic inflammatory disease and ectopic pregnancy. Primary tumors of the tubes are rare.
Treatments are based on the cause of disease. Surgical procedures include tubal ligation, salpingolysis, resection and anastomosis and neosalpingectomy.

The normal hysterosalpingogram shows the gracile Fallopian tubes demonstrating patency with minimal spillage bilaterally. Note the serrated appearance of the cervix and smooth shape of the endometrial cavity.
Ashley Davidoff, M.D.
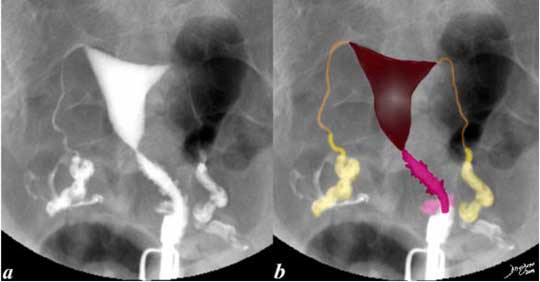
This hysterosalpingogram is from a 26-year-old female with normal appearing delicate and patent Fallopian tubes (orange in b), fimbriae (yellow) with free spillage (white).
The endometrial cavity (maroon) and cervical canal (pink) are also normal.. Note the irregular shape to the cervical canal while the endometrial lining is smooth.
Images courtesy of: Ashley Davidoff, M.D.
The Anatomy – Parts : Cervix
The cervix is the lower constricted segment of the uterus. It is somewhat conical in shape with its truncated apex directed downwards and backwards. The cervix projects through the anterior wall of the vagina which divides it into the supravaginal and vaginal portions.
The supravaginal portion is related to the bladder anteriorly and separated by fibrous tissue called parametrium. This extends laterally and the uterine arteries enter the cervix through it. The ureters run downward and forward in it about 2 cms from the margin of the cervix.
The vaginal portion (portio vaginalis) projects free into the vagina through the anterior wall, dividing it into anterior and posterior fornices. The external orifice is a circular aperture bounded by an anterior and posterior lip.
The cavity of the uterus is triangular in shape, slit-like in size and flattened anteroposteriorly. The base of the triangle is formed by the internal surface of the fundus and the apex by the internal orifice.
The cavity of the cervix is a fusiform, broader in the middle part of the canal. It communicates with the uterine cavity through the internal orifice and with the vagina through the external orifice. It has a posterior and anterior ridge from which the mucosa is thrown into palmate folds giving it a tree-like appearance in cross section. This appearance is reminiscent of a tree and is thus called the arbor vitae uterina.
Size
The nature and structure of the uterus allows it to change its size dramatically based on age and physiological state. The mature, adult uterus has been described as about the size of a small pear or an avocado. It is slightly smaller than the heart. In the non gravid state it is confined to the deep pelvis but is able to reach the epigastrium and subxiphoid region when at peak pregnancy.

The avocado pear has some interesting implications in the structure and function of the uterus. The approximate size of the non gravid adult uterus is about that of an avocado pear. It also takes between 6 and 12 months to grow an avocado from blossom to ripened fruit. The human gestational period is about 9 months.
Ashley Davidoff, M.D.
The mature, non gravid uterus measures about 8 cm in length, 4 cm in A-P dimension by nearly 6 cm in transverse dimension; it weighs from about 35 gms in the virgin state up to 200 gms in the postpartum state. The volume of the uterus ranges between 75-200 cc. The myometrium measures between 1.5-2.5 cm in thickness and the endometrium measures from 1-10 mms but sometimes can be greater than 10 mm in the secretory phase.
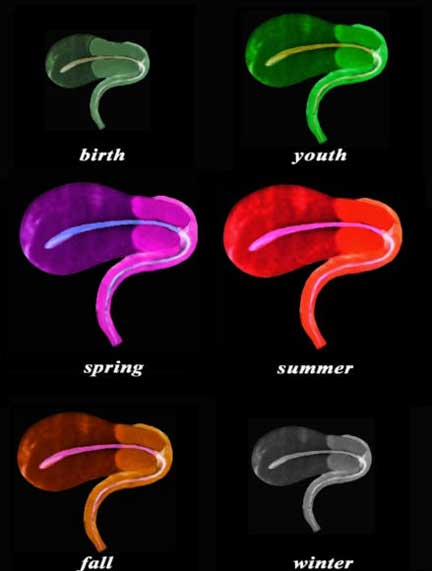
The sagittal diagram of the uterus and vagina through time shows an anteverted uterus at birth, through youth as it slowly matures and enlarges, entering spring as it reaches maturity, summer time when it bears fruit, and then through fall as it starts to involute in the postmenopausal period, and finally in its winter when it shrivels. In this view the uterus, vagina, and the internal cavity starting in the endometrial cavity, coursing through the cervix and then into the collapsed vaginal cavity is exemplified.
Images courtesy of: Ashley Davidoff, M.D.
Size: Size Continued
At Birth
At birth the dimensions of the body of the uterus are similar to the size of the cervix. Its overall length is between 2.3-4.6 cms (Nabaloff).
Ashley Davidoff, M.D.
Prepubertal State
In the virgin state the uterus is flattened antero-posteriorly and is pyriform in shape with the apex directed downward and backward.
The prepubertal uterus measures about 2-4.4 cms in the craniocaudad (C-C) span.
The Mature Uterus
The nulliparous uterus measures between 6-8.5 cms in the craniocaudad span, 2-4 cms in the anteroposterior (A-P) dimension and 3-5 cms in the transverse dimension.
The multiparous uterus usually measures about 8-10.5 cms in the C-C span, 3-5 cms in the A-P dimension and 4-6 cms in the transverse dimension.
This sagittal reconstructed CT shows an anteverted uterus buoyed and cushioned by a partly filled bladder (greenish-yellow). In this sagittal view the adult uterus measures about 10 cm in the craniocaudad span and 5 cm in the A-P dimension and the endometrial stripe measures about 1 cm. Images courtesy of Ashley Davidoff, M.D.
Size: The Gravid Uterus
In the gravid state the uterus rises out of the pelvis and enters the abdominal cavity gently displacing other abdominal structures.
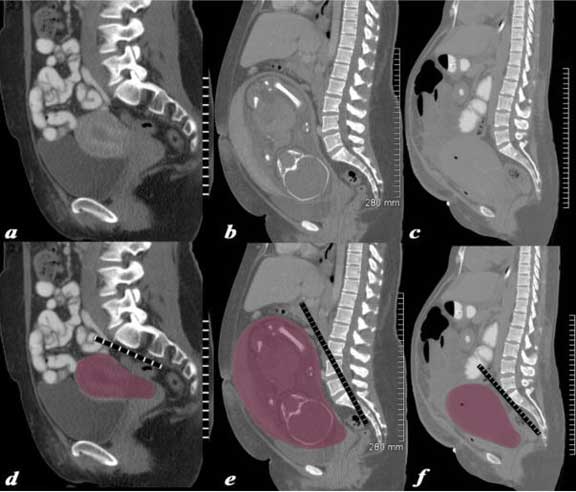
The series of CT scans from different patients are reconstructed in the sagittal plane to show the mature uterus in the non-gravid state (a,d), with a 32 week pregnancy (b,e), and in the postpartum, post cesarean section state (c,f). In the nongravid adult the uterus in the craniocaudad span (C-C) measures about 8.5 cms and in the anteroposterior (A-P) dimension it measures 4.5 cm. The uterus containing the 32 week pregnancy measures 24 cms (C-C) by 16 cms (A-P). In the post cesarean section patient the uterus measures 17cm (C-C) by 9 cms (A-P).
Ashley Davidoff MD
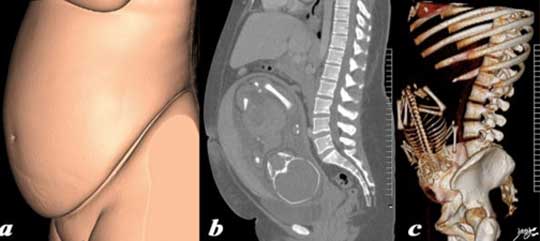
The three sagittally reconstructed images of the gravid uterus are from a normal 31-year-old woman carrying a 32 week gestation. They depict the outside appearance of the patient (a), 2 D sagittal view (b) and 3D sagittal view (c). The function of the uterus is to enable the housing, protection and nourishment of the developing pregnancy. This function is only required for a brief time in the long life of an adult female ? but the species depends on this brief sojourn.
Ashley Davidoff MD
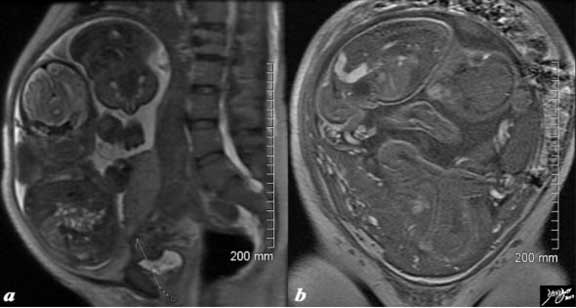
The T2-weighted MRI from a 44-year-old patient with 32 week twin gestation in the sagittal plane (a) and in the coronal plane (b) revealing a uterus that measures 30 cm in the craniocaudad span, by 18 cm A-P, by 26 cm in the transverse plane. Images courtesy of Ashley Davidoff, M.D.
Size: Post Partum Uterus
The mean size of the uterus 24 hours after delivery is 14 X 7cms. (Garagiola)
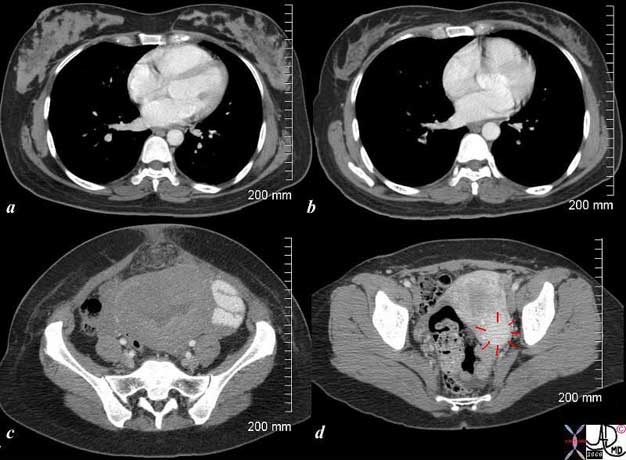
The CT scan is from a 26-year-old female showing breasts and uterus in a post partum post cesarean section state (a,c) and then 18 months later (c,d). The transverse dimension of the uterus in the post partum state is about 11 cm, while 18 months later is about 5 cm. Her breasts in the post partum state are enlarged with prominent glandular tissue (a) and 18 months later are reduced in size and glandular volume (b). Surgical footprints are noted in the subcutaneous tissue in (c) following her cesarean section. A cervical fibroid (red arrows) is suggested post partum image (d). Courtesy of Ashley Davidoff, M.D.
Size: The Uterus in Old Age
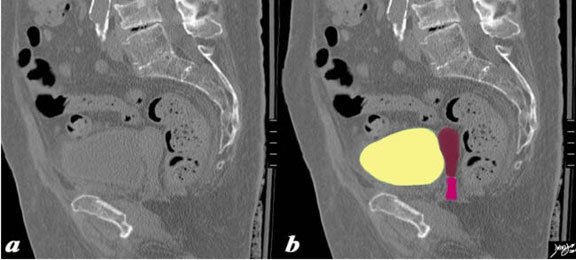
This sagittal reconstructed CT is shown of an 82-year-old female. The craniocaudad span (C-C) is about 5 cm and the A-P dimension is 1.5 cm. The endometrial stripe is not visible. The uterus is buoyed and cushioned by a partly filled bladder (yellow).
Courtesy of Ashley Davidoff, M.D.
Size: Endometrial Size
Size and the Menstrual Cycle
The cyclical changes of the menstrual cycle present a continual change of events controlled by a series of integrated hormonal events. These changes are most easily observed in the endometrium by ultrasound. When performing a pelvic ultrasound, it is of the utmost importance to record the patient?s menstrual history.
The measurement is taken from echogenic border to echogenic border in the midsagittal plane.
During the menstrual phase (days 1- 4) the endometrium is thin and typically is seen as a single echogenic line by ultrasound examination measuring between 1-4 mm thick and reflecting the early development of glands and stroma.(Nalaboff). The junctional zone is irregularly thick and the myometrium loses water and thins.
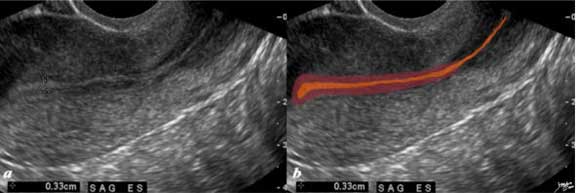
The normal sagittal view of the uterus in a transvaginal ultrasound in the first week after menstruation and just prior to the next menstruation after the endometrium has been shed. It demonstrates that the endometrium becomes a single echogenic line consisting of opposing walls (orange) and is surrounded by a subendometrial halo of the junctional zone (reddish). This layer is more compacted and relatively hypovascular. This image is typical of the early proliferative phase. It is during this time that estrogen starts to rise and progesterone has fallen. The endometrium in this case measures about 3 mm.
Ashley Davidoff, M.D.
In the proliferative phase (day 4-14) the endometrium thickens to 5-7 mm and becomes more echogenic than the myometrium. This reflects growth of the endometrial glands, blood vessels and stroma, stimulated by estrogen production by the ovarian follicles. This proliferative endometrium is structurally and functionally preparing for implantation of the fertilized egg. In the late proliferative phase (periovulatory phase) the endometrium becomes multilayered with an echogenic basal layer, hypoechoic inner functional layer and a thin echogenic line alongside the junctional zone of the myometrium and measures up to 11 mms. (Nalaboff).
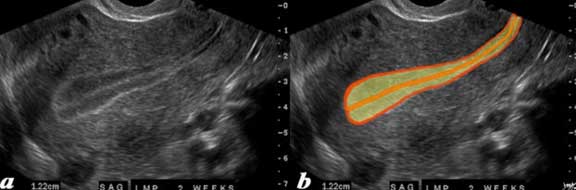
The normal sagittal view of the uterus in a transvaginal ultrasound, 2 weeks after menstruation and just prior to ovulation. It demonstrates that the uterus and more specifically the endometrium are more complex than just a simple columnar epithelium. This is an example of the trilaminar appearance of the endometrium and is characteristic of the appearance of the endometrium in the preovulatory phase. This phase is also called the follicular phase or proliferative phase. It is during this time that estrogen is the dominant hormonal influence. The appearance is also known as a “triple stripe” and conversely, its presence is seen before progesterone is produced. If present with a 9 mm+ diameter, it reflects an ideal potential lining for fertilization. In this case it measured 1.2 cm.
Ashley Davidoff, M.D.
Following ovulation, the endometrium is under the influence of progesterone secretion by the corpus luteum. The endometrial glands fill up with mucus. The resulting appearance of the endometrium is a thick echogenic structure (secretory phase). During the secretory phase (days 15-28), the endometrium is at its thickest in mid secretory phase and has a typical homogeneously, echogenic appearance. It usually measures between 7-16 mms. (Nalaboff).
Premenstrual Endometrium – End of Secretory Phase
The normal sagittal view of the uterus in a transvaginal ultrasound about 4 weeks after menstruation and just prior to the next menstruation when the endometrium is overripe. It demonstrates that the uterus and more specifically the endometrium are more complex than just a simple columnar epithelium. This is an example of the hyperechoic, homogeneous, thick endometrium characteristic of the secretory phase. It is during this time that progesterone is the dominant hormonal influence and estrogen influence is minimal. The endometrium in this case measures 1.2 cm.
Images courtesy of Ashley Davidoff, M.D.As luteinizing hormone levels fall in the latter phase of the cycle, the level of progesterone falls and there is shedding of the endometrium.
Size: The Post Menopausal Endometrium
The postmenopausal stripe in the absence of hormonal replacement therapy should measure <5 mms (Nalaboff). In a patient with post menopausal bleeding if the stripe measures <5 mms it is unlikely that the patient has endometrial cancer.
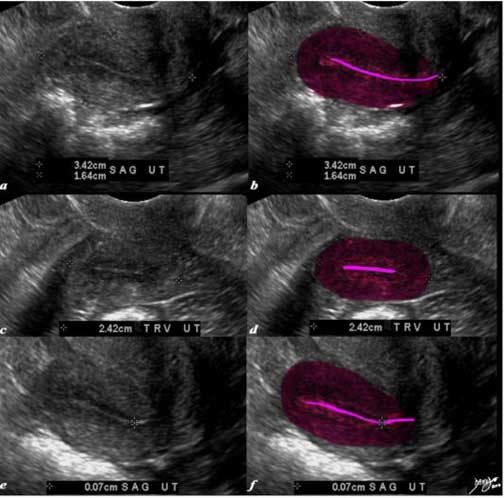
The transvaginal ultrasound is from a 62-year-old post menopausal patient who presents with pelvic discomfort. The ultrasound shows a small atrophied uterus. The myometrium (dark red), junctional zone (light red) and endometrial cavity (pink) are outlined. In the sagittal plane the uterus measures 3.4 cm in the cranoicaudal dimension by 2.4 cm in the anteroposterior dimension (a,b). In the axial dimension (c, d) the uterus measures 2.4 cm. The endometrial stripe is measured at 0.7 mm in the sagittal plane.
Courtesy of Ashley Davidoff, M.D.
Shape
Overall, the uterus is pear-shaped and usually bent anteriorly (anteflexed) between the cervix and body.
The cavity is roughly triangular or “T” shaped. The cervix is cylindrical prior to puberty.
Shape of the Body of the Uterus
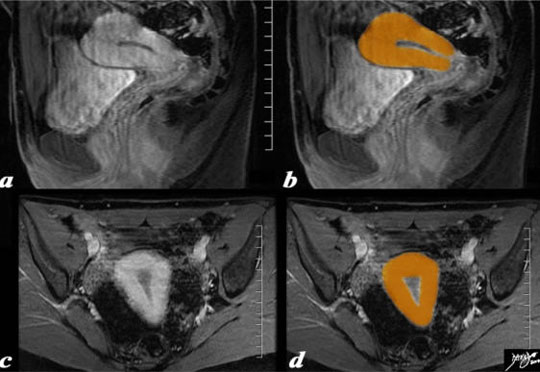
The uterus is pear-shaped as depicted in this overlay of a MRI study. The sagittal view (a, b) and coronal (c, d) T1-weighted enhanced MRI study reveal a normal uterus.
Ashley Davidoff, M.D.
Applied Anatomy
An abnormal shape of the body of the uterus is most commonly caused by the presence of a fibroid uterus.

The CT scan is from a 31-year-old female who presents with a pelvic mass. The study reveals a large uterus with multicentric fibroids and mild hydronephrosis.
Images courtesy of Ashley Davidoff, M.D.
Shape of the Endometrium and Endometrial Cavity
The shape of the endometrium in the sagittal view is also pear-shaped or tear drop-shaped.
Depending on the phase of the menstrual cycle this shape will change but its pear shape is best appreciated in the secretory phase when the endometrium is thickest.
Shape of the Endometrium in the Coronal Plane
In the coronal plane the endometrial cavity is almost triangular in shape.
The shape of both the uterus and the endometrial cavity is reflected in this artistic rendition of a drop of water just as it starts to fall or on a sadder note a tear as it just starts to roll down the cheek.
Ashley Davidoff, M.D.

The T2-weighted MRI in axial projection of a 31-year-old female shows the endometrial cavity in coronal view with an arcuate shape. This is a normal variant and has no clinical significance. The follicles in the ovaries are also well demonstrated. Images courtesy of Ashley Davidoff, M.D.
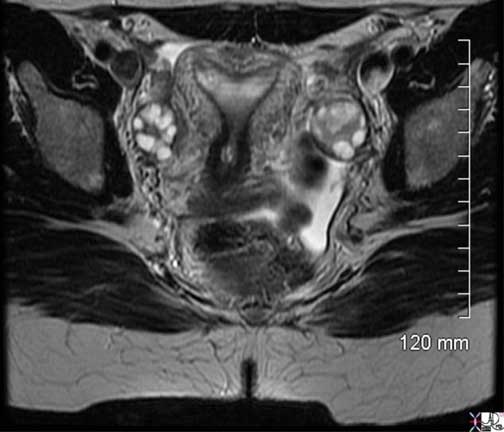
The axial T2-weighted sequence from an MRI study shows the normal appearance of the uterus in a 34-year-old female. Because the uterus is anteverted it lies flat, so that in this instance, the coronal plane of the uterus is demonstrated. The triangular shape of the cavity is exemplified. The endometrium is of intermediate signal, the junctional zone of low signal consisting of compacted smooth muscle with low water content and the surrounding myometrium of smooth muscle with a higher water content is higher in intensity. Two high signal cysts are seen in the right ovary .
Ashley Davidoff, M.D.
An arcuate uterus is a variant of normal where the base of the triangle is slightly convex.
Shape: Hysterosalpingogram: Defining the Shape of the Endometrial Cavity
Hysterosalpingogram involves the injection of contrast into the uterine cavity that enables the evaluation of the cavity as well as the patency of the fallopian tubes.
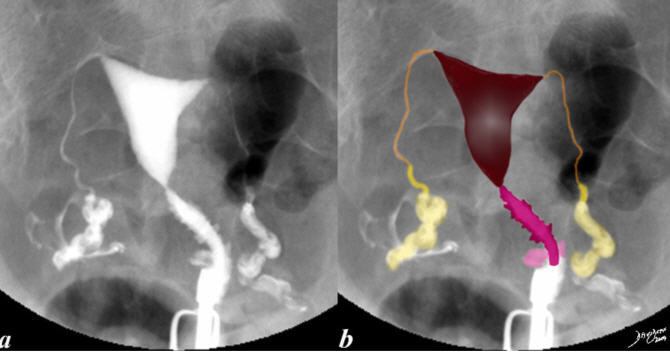
This hysterosalpingogram is from a 26-year-old female with a normal endometrial cavity and cervical canal. Note the triangular shape with smooth walls of the endometrial cavity as opposed to the cylindrical shape with serrated walls of the endocervical canal.
Ashley Davidoff, M.D.

40-year-old female with normal endometrial cavity and cervical canal and fallopian tubes using hysterosalpingography (HSG). The shape of the cavity is reminiscent of an arcuate uterus with a convex superior border of the fundal part of the cavity.
Images courtesy of Ashley Davidoff, M.D.
Shape: Applied Anatomy

34-year-old female who presented with infertility had a hysterosalpingogram which showed a unicornuate uterus (a). An MRI confirms the diagnosis using a T2-weighted sequence (b). The patient subsequently fell pregnant and was scanned with a normal 13 week pregnancy (c).
Ashley Davidoff, M.D.

The series of images from a young adult female with bicornuate uterus with agenesis of the left kidney.
Image (a) is a coronal T1-weighted contrast enhanced image that shows abnormal left kidney (arrowheads).
Image (b) is an ultrasound in transverse dimension that shows two endometrial cavities (arrows).
Image (c) is a T2-weighted image that shows 2 separate horns that fuse above a single cervix and overlaid in pink in image (d).
These findings are consistent with bicornuate uterus with agenesis of the left kidney. Combined congenital anomalies of the uterus and renal system are a well known association.
Ashley Davidoff, M.D.

74-year-old female with bicornuate uterus and dilated endometrial cavities. Diagnosis is carcinoma of the cervix with obstruction. The myometrium is overlaid in dark pink and the endometrial cavity is a heterogeneous orange consisting of both fluid and soft tissue elements.
Ashley Davidoff, M.D.

In this sagittal view of a T2-weighted MRI of the uterus of a 42-year-old female with multiple fibroids, two of which impinge on the endometrial cavity (the larger – light green) from posterior and the smaller (dark green) from anterior resulting in a sigmoid shaped cavity (yellow). In addition, incidentally noted Nabothian cysts (orange) are seen within the cervix.
Images courtesy of Ashley Davidoff, M.D.
Position
The uterus lies in the pelvis between the bladder and the rectum, and it projects supero-anteriorly over the urinary bladder.
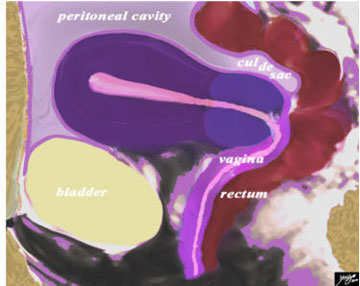
This diagram in the sagittal plane illustrates the peritoneal covering (light purple lining) of the uterus reflected posteriorly off the rectum, in the region of the fornix of the vagina, creating a pouch called the recto-uterine pouch (aka cul de sac. pouch of Douglas, recto-vaginal pouch Ehrhardt-Cole recess) This pouch is very important because it is the most posterior and inferior space of the peritoneal cavity and in the supine or upright position it will be the region where fluid will first accumulate. Anteriorly the peritoneal reflection is not as deep but a pouch is also formed called the utero-vesical (aka vesico-uterine) pouch.
Ashley Davidoff, M.D.
The position of the uterus is described in two ways: if the uterus is bent forward it is called anteverted and if it is bent backward it is called retroverted. When the body of the uterus is bent anteriorly on the cervix, resulting in different angles for the body and the cervix, it is called anteflexion. Similarly when the body is flexed on the cervix and they are angled posteriorly at different angles, it is called retroflexion.
In the case above the uterus is anteverted ? the uterus is bent forward. The long axis of the vagina forms a ninety degree angle with the axis of the cervix, which is directed posteriorly and inferiorly. The position of the uterus is significantly altered by the volume of urine in the bladder.
In the following case the bladder is moderately full and the angle formed by the uterus with the vagina is just under 90 degrees. However, the body appears to be bent on the cervix so there is both anteversion and anteflexion.
The diagram represents a sagittal view of the uterus reflecting a ?V? shaped structure of the uterus and vagina The uterus varies in position and in this case is anteverted; that converts the L shaped structure described to a “V” shaped structure. The cervix is directed posteriorly and along the same vector as the body and hence there is no anteflexion.
Ashley Davidoff, M.D.
When the uterus is flexed backward the position is called retroversion and the cervix is directed anteriorly and inferiorly. The whole uterus is bent back and the vector of the body is aligned with the vector of the cervix and therefore, retroflexion is not present. This is sometimes the normal position of the uterus.
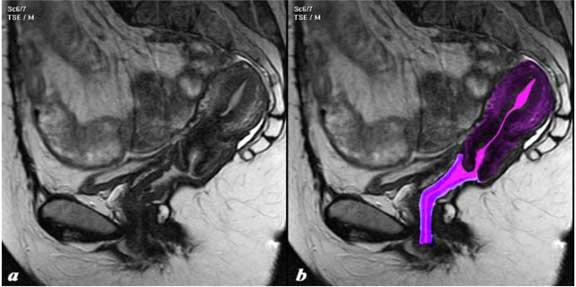
This T2-weighted MRI shows a retroverted uterus. The body of the uterus and cervix are in alignment and therefore retroflexion is not present. The uterus is fairly mobile and in this sagittal MRI it is retroverted and instead of being an “L” or a “V” configuration it is almost an “I” configuration.
Ashley Davidoff, M.D.

In this HSG of a 40-year-old female the arcuate uterus is tipped to the right. The uterus is mobile and often will tip to the right or the left.
The endometrial cavity, cervical canal and fallopian tubes are normal.
Images courtesy of Ashley Davidoff, M.D.
Character
Character implies the look and feel of the uterus on macroscopic evaluation. The uterus has a smooth, external surface. It is relatively hard to palpate since it is a fibromuscular organ. It has a hollow endometrial cavity. The fundus and body are muscular and the cervix is harder, more rigid and fibrous. The body of uterus is mobile, while the cervix is relatively fixed, though it can bend or flex.
Character – by Ultrasound
The outer myometrium by ultrasound is usually homogeneous, while the inner myometrium ? the junctional zone – is hypoechoic. The junctional zone is best appreciated in the late secretory phase and early menstrual phase when it is most prominent under the influence of progesterone.
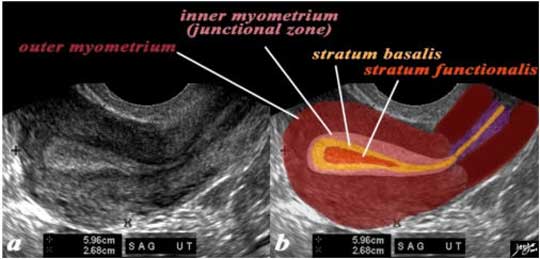
Last Monthy Period 4 Weeks Prior
In this 26-year-old premenstrual female a transvaginal ultrasound in the sagittal plane reveals a normal view of the uterus with characteristic premenstrual appearance (a). The stripe is almost homogeneously echogenic and thick but also shows a hypoechoic halo of the junctional zone or inner myometrium (salmon). The homogeneous stripe is made up from two histological layers (barely distinguished by this ultrasound) ? the inner stratum functionalis (deep orange) that will shed once the spiral arteries vasoconstrict and the outer stratum basalis (deep yellow) that will not shed and will be the basis for regenerating the endometrium in the next cycle. The next layer as stated above is the compact myometrium – the junctional zone (also known as the inner myometrium) and is followed by the thicker outer myometrium (maroon) (b).
Images courtesy of: Ashley Davidoff, M.D.

In this 26-year-old premenstrual female a transvaginal ultrasound reveals a normal transverse view of the uterus with characteristic premenstrual appearance. The stripe is homogeneously echogenic and thick but also shows a hypoechoic halo of the junctional zone or inner myometrium (salmon). The homogeneous stripe is made up of two histological layers (not distinguished by this ultrasound): the inner stratum functionalis (deep orange) that will shed once the spiral arteries vasoconstrict and the outer stratum basalis (deep yellow) that will not shed and will be the basis for regenerating the endometrium in the next cycle. The next layer as stated above is the compact myometrium – the junctional zone (aka inner myometrium), and is followed by the thicker outer myometrium (maroon).
Ashley Davidoff, M.D.
The character of the endometrium also changes significantly over the menstrual cycle. During the menstrual phase (days 1- 4) the endometrium is thin and typically is seen as a single echogenic line by ultrasound examination and measures between 1-4 mm in thickness, reflecting the early development of glands and stroma (Nalaboff). These changes were exemplified in the section on the size of the endometrium but are sufficiently important to repeat at this time to emphasize the changes in character during the 28 day cycle.
The preovulatory endometrium is highly characteristic with trilaminar appearance of a central thin line of echogenicity, followed by a thicker hypoechoic zone and then a thin echogenic line again.
When the glands are full and the endometrium is thickest in the late secretory phase the endometrium becomes homogeneously echogenic, occasionally with a few cystic areas of early breakdown.
Character: Character – CT and MRI
The character of the uterus is dependent on many aspects including the age, time of the month and the way the angle of the uterus is scanned.

In this 20-year-old patient the myometrium (maroon) is homogeneous and isodense with the soft tissues. The subendometrial layer is hyperemic (red) and likely is in the latter phase of the cycle and the endometrium and endometrial cavity are hypodense (yellow). She presented with colitis and ascites which enabled detail of the uterus to be appreciated. The ovaries are well visualized as well (purple). Courtesy of: Ashley Davidoff, M.D.
Characterization by MRI
T2-weighted imaging and contrast enhanced; T1-weighted image best evaluates the character of the uterus.
The normal sagittal view of the uterus is a T2-weighted MRI from a 16-year-old female with pelvic pain. It demonstrates that the uterus and more specifically the myometrium, is more complex and consists of an outer part (dark red) and an inner more homogeneous part called the junctional zone. Since a T2-weighted image is sensitive to water we understand from this image that the outer part contains more water, since it has foci of high intensity signal, likely related to greater vascularity. The junctional zone (light brown) and cervix are darker, related to greater fibrous tissue. The endometrial canal, cervical canal and vaginal cavity are outlined in yellow and have higher intensity related to higher water content. The vaginal wall is dark and overlaid in pink.
Images courtesy of Ashley Davidoff, M.D.
Blood Supply
The blood supply of the uterus is from the uterine artery, a branch of the internal iliac artery and ovarian artery, a branch of the aorta. The uterine artery passes inferiorly from its origin into the pelvic fascia and reaches the junction of the cervix and uterus by passing superiorly. It is superiorly related to the ureter which passes the pelvic brim to the urinary bladder and crosses the bifurcation of the common iliac artery. The uterine artery anastomoses with the ovarian artery superiorly and vaginal artery inferiorly.
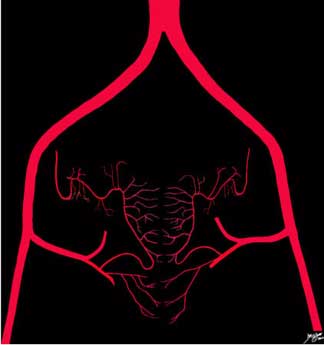
The blood supply to the uterus is from the uterine arteries, which take their origin from the iliac system. The uterine artery collateralizes with the ovarian artery and there are also rich anastomoses between the left and right sides, both anterior to and posterior to the uterus.
Ashley Davidoff, M.D.
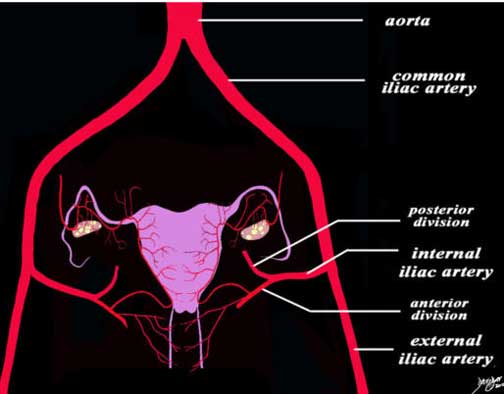
The diagram of the blood supply to the uterus in its most basic form and shows the large inflow arteries into the pelvis. The main artery is the aorta which branches into the common iliac arteries which in turn branch into the external and internal iliac arteries. The internal iliac branches into an anterior division and a posterior division. The uterine and vaginal arteries arise from the posterior division.
Ashley Davidoff, M.D.
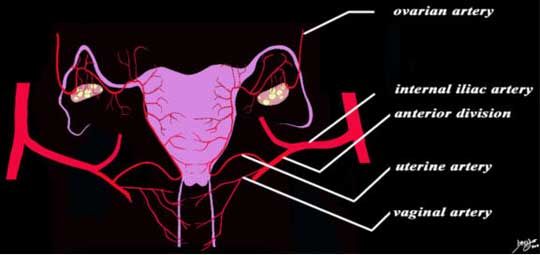
The diagram of the blood supply to the uterus in its most basic form shows that the uterine artery is a branch of the anterior branch of the internal iliac artery and the uterine artery collateralizes and in fact is continuous with the ovarian artery which takes its origin directly from the abdominal aorta. The main branches include the uterine branches, vaginal branches and the ovarian branches.
Ashley Davidoff, M.D.
The uterine artery runs along the lateral wall of the uterus and then penetrates the myometrium and divides in general into anterior and posterior branches. As they course toward the center they are called the arcuate arteries whose direction in general is circumferential to the uterus. They give rise to the radial arteries which course almost at right angles toward the endometrium.
Blood Supply: At the Mucosal Level
Branches from these arteries pass to the endometrium. As they enter the endometrium they run a straight course and supply the stratum basalis and as they enter the superficial layer of the stratum functionalis they become coiled and are called the spiral arteries. The straight arteries do not undergo cyclic changes and they supply stable unchanging blood supply to the stratum basalis which does not shed at the menses. The spiral arteries in the stratum functionalis, on the other hand, are subject to significant change with hormonal fluxes. Just before menstruation the spiral arteries coil and initially vasodilate and then there is an intense vasoconstriction causing ischemia and subsequent ischemia and destruction of the stratum functionalis which sheds as a result.
As they enter the endometrium they become the spiral arteries and their capillaries. The superficial layer of the endometrium (functionalis) is shed during menstruation. A basal layer, the basalis, is permanent and it regenerates after each menstruation. At the onset of menstruation the spiral arteries coil and initially vasodilate and then follow an intense vasoconstriction at the time of shedding.
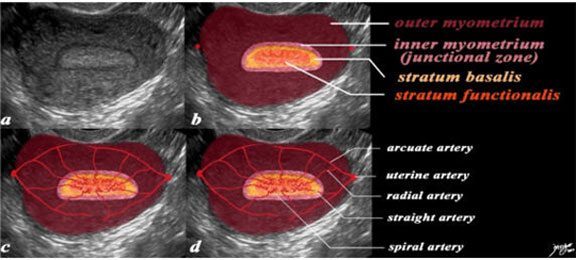
In this 26-year-old premenstrual female a transvaginal ultrasound reveals a normal transverse view of the uterus with characteristic premenstrual appearance (a). The stripe is homogeneously echogenic and thick but also shows a hypoechoic halo of the junctional zone or inner myometrium (salmon). The homogeneous stripe is made up of two histological layers (not distinguished by this ultrasound): the inner stratum functionalis (deep orange) that will shed once the spiral arteries vasoconstrict and the outer stratum basalis (deep yellow) that will not shed and will be the basis for regenerating the endometrium in the next cycle. The next layer as stated above is the compact myometrium – the junctional zone (aka inner myometrium) and is followed by the thicker outer myometrium (maroon) (b). In the second series of images (c, d) the blood supply of the uterus is exemplified to demonstrate the branches that lead to the spiral arteries which undergo vasoconstriction at the time of the menses, resulting in ischemia of the functionalis and subsequent shedding . The uterine arteries give rise to the arcuate arteries which in turn give rise to the radial arteries, straight arteries and finally the spiral arteries.
Ashley Davidoff MD
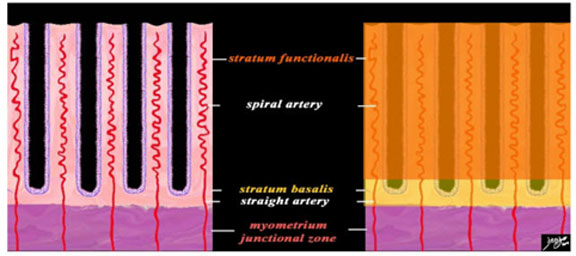
A closer view of the endometrium as seen in the premenstrual phase, exemplified by the characteristic spiral (helical) arteries running in the stroma (pink) between the simple, tubular, test tube shaped glands (purple). The spiral arteries supply the functional layer (stratum functionalis – deep orange) and the straight arteries supply the basal layer (stratum basalis- light orange). Beneath the basal layer is the myometrium and the subendometrial smooth muscle or junctional zone (dark pink).
The other structures that run in the stroma between the tubular glands are the veins and lymphatics.
Ashley Davidoff MD
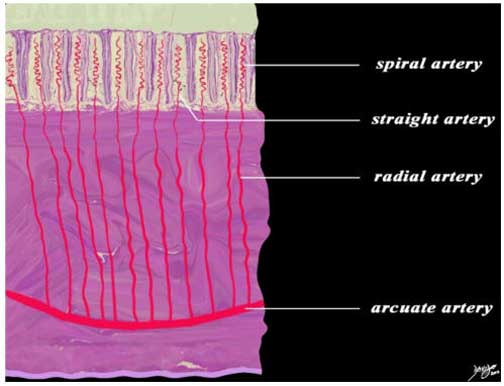
This diagram exemplifies the position of the arteries in the epithelial and muscular layers. The spiral arteries run in the stratum functionalis; the straight arteries run in the stratum basalis, while the radial arteries and the arcuate arteries run in the muscularis.
Ashley Davidoff MD
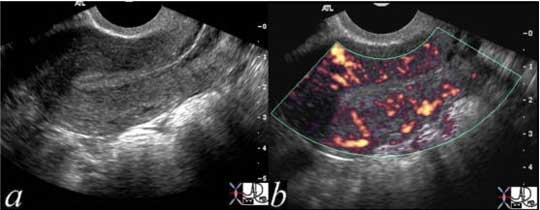
This power Doppler image reflects the normal perfusion of the uterus.
Image courtesy of Ashley Davidoff, M.D.
Venous Drainage
The venous drainage of the uterus is via the uterine veins, which in general parallel the course of the arterial supply and eventually drain into a branch of the internal iliac vein as well as into ovarian veins which drain into the IVC and left renal vein.
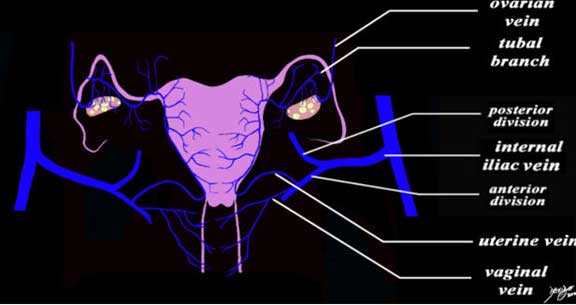
The uterine veins drain mostly into the anterior division of the internal iliac vein, which in turn drains into the common iliac vein, which subsequently drains into the inferior vena cava. The uterine veins, vaginal veins, tubal veins and ovarian tributaries are intimately integrated and interconnected.
Courtesy of Ashley Davidoff, M.D.
Lymphatic Drainage
The lymphatics of the uterus also, in general, follow the arteries. As is usual among the other lymphatics of the body there are extensive interconnections between all the lymphatics of the pelvis. The lymphatic system of the cervix drains to the sacral nodes and the body, fundus and fallopian tubes drain toward the external iliac nodes. There is some drainage toward the internal iliac nodes as well. Lymphatics may also reach the superficial inguinal nodes along the round ligament.
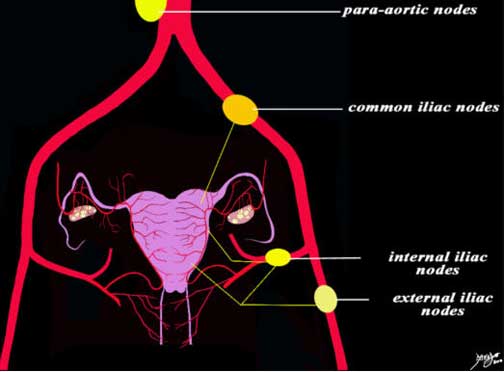
The uterus drains into the external iliac, internal iliac and common iliac chain and finally all drain into the para-aortic chain.
Ashley Davidoff, M.D.

61-year-old female with an enlarged endometrial cavity and cervical mass, consistent with cervical carcinoma, complicated by obstruction of the endometrial cavity. The cavity is filled with complex material probably from a combination of secretions, fluid, blood and tumor. Lymph nodes in the left para-aortic area (c, white arrow) were biopsied under CT guidance (d) and were positive for cervical cancer.
Images courtesy of Ashley Davidoff, M.D.
Nerve Supply
The innervation of the uterus is entirely autonomic, arising from the inferior, hypogastric plexus (sympathetic) and the pelvic, splanchnic nerves (parasympathetic from S2,3, 4). The afferent fibers travel with the sympathetic efferents to T10-12 and L1 spinal cord segments.
In the sympathetic chain there is an intermediary step between the viscera and spinal cord – a “halfway house” if you will, that runs alongside the spinal cord and it is called the sympathetic chain. There is therefore, a neuron that carries the signal from the spinal cord to the sympathetic chain called the preganglionic neuron and one that carries the signal between the ganglion of the chain to the organ called the post ganglionic neuron. In general T1 goes to the head, T2- T6 the thorax and T7 -T11 the abdomen. T12, L1 and L2 go to the legs. This is an approximation and there is a large cross over. The innervation depends on the embryological origin.
Most of the afferent fibers ascend through the inferior, hypogastric plexus and enter the spinal cord via T10-12 and L1 spinal nerves.
The nerve supply to the uterus is derived from the hypogastric and ovarian plexuses and from the third and fourth sacral nerves.
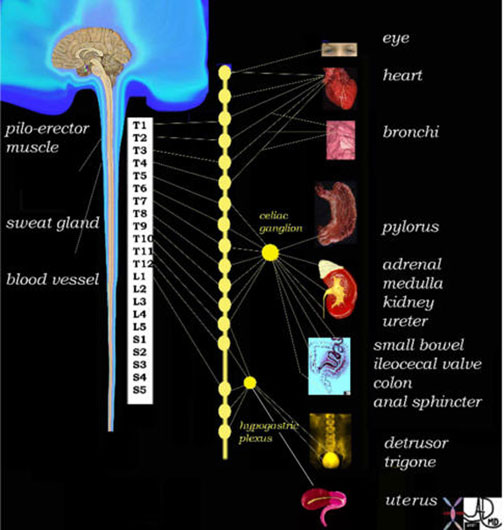
The diagram reveals the sympathetic nervous system of the body and in this instance attention is drawn to the contribution of the hypogastric plexus and specifically from a component called the inferior, hypogastric plexus which in turn gets contributions from the anterior and intermediate part known as the uterovaginal plexus. The plexus lies in the broad ligament on each side of the cervix.
Ashley Davidoff, M.D.
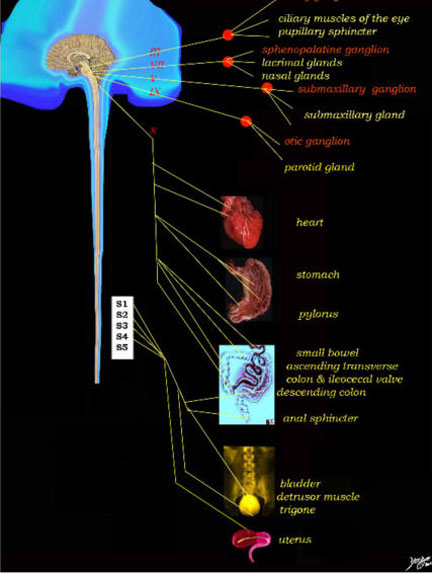
The diagram reveals the parasympathetic nervous system of the body and in this instance attention is drawn to the contribution of S2,3 and 4, called the pelvic splanchnic plexus.
Images courtesy of Ashley Davidoff, M.D.
Capsule of the Uterus
The uterus is covered by peritoneum anteriorly and posteriorly to the level of the isthmus. The peritoneal covering of the uterus is reflected posteriorly off the rectum in the region of the fornix of the vagina, creating a pouch called the recto-uterine pouch (also known as the cul de sac or pouch of Douglas or recto-vaginal pouch). This pouch is very important because it is the most posterior and inferior space of the peritoneal cavity and in the supine or upright position it will be the region where fluid will first accumulate. Anteriorly the peritoneal reflection is not as deep but a pouch is also formed called the utero-vesical (also known as the vesico-uterine) pouch.
Ligaments
The uterus remains in its pelvic position by virtue of its positions and various ligaments that keep it in position. These supports can lose strength with multiple vaginal childbirths, menopause and age and cause utero-vaginal position.
The anterior ligament consists of the vesicouterine fold of peritoneum, which is reflected onto the bladder from the front of the uterus, at the junction of the cervix and body.
The posterior ligament consists of the rectovaginal fold of peritoneum, which is reflected from the back of the posterior fornix of the vagina onto the front of the rectum. It forms the bottom of the recto-uterine pouch; laterally it is bound and the folds are called sacrogenital or rectouterine folds which have condensed fibrous tissue which attach to the sacrum and constitute the uterosacral ligaments.
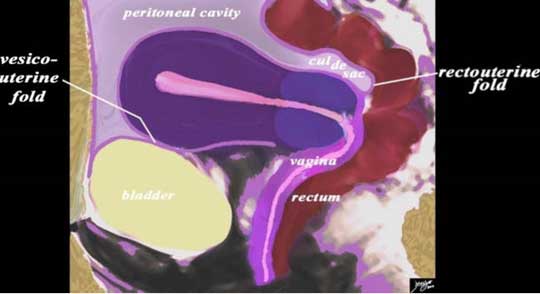
This diagram in the sagittal plane illustrates the peritoneal covering (light purple lining) of the uterus reflected. Anteriorly, the peritoneal reflection is shallow and a fold or ligament is created called the vesico-uterine fold. A pouch is also formed called the utero-vesical (a.k.a vesico-uterine) pouch. Posteriorly the peritoneum is reflected off the rectum in the region of the fornix of the vagina creating a ligament or fold called the recto-uterine fold. A pouch called the recto-uterine pouch (a.k.a. cul de sac. pouch of Douglas, recto-vaginal pouch Ehrhardt-Cole recess) is formed. This pouch is very important because it is the most posterior and inferior space of the peritoneal cavity and in the supine or upright position it will be the region where fluid will first accumulate.
Ashley Davidoff, M.D.
The two lateral or broad ligaments (ligamentum latum uteri) pass from the sides of the uterus to the lateral walls of the pelvis. The portion of the broad ligament which stretches from the uterine tube to the level of the ovary is known as the mesosalpinx. Between the fimbriated extremity of the tube and the lower attachment of the broad ligament is a concave rounded margin called the infundibulopelvic ligament.
The round ligaments (ligamentum teres uteri) are two flattened bands between 10 and 12 cm. in length, situated between the layers of the broad ligament, in front of and below the uterine tubes.
The cardinal, Mackenrodt or transverse ligaments are attached to the side of the cervix uteri and to the vault and lateral fornix of the vagina. They are continuous externally with the fibrous tissue, which surrounds the pelvic blood vessels.
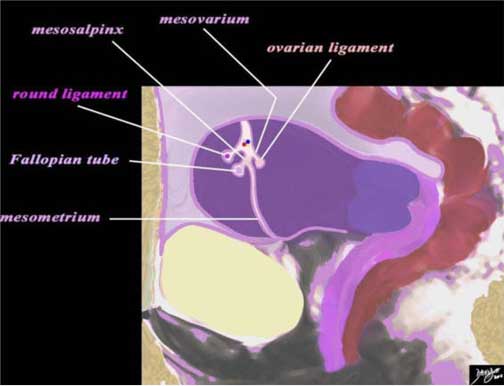
This diagram in the sagittal plane demonstrates the broad ligament within which resides the round ligament (shocking pink), the fallopian tube and the ovarian ligament. Within the broad ligament the uterine/ovarian artery runs (red), uterine/ovarian vein (blue), lymphatics (yellow) and nerves.
Ashley Davidoff, M.D.

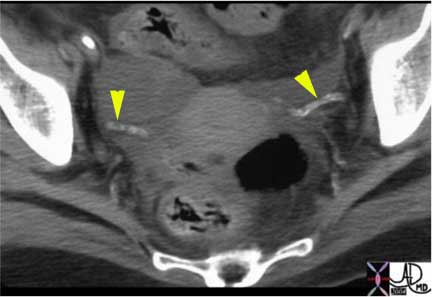
The broad ligaments with their vascular contents are seen like horns of a bull extending from the uterus to the side walls of the pelvis. They are well visualized because this patient has ascites which is apparent in the cul de sac between the uterus and the rectum (black air is seen in the rectum) as well as posterior to the uterus.
Ashley Davidoff, M.D.
In diabetes, old age, and sometimes in sarcoidosis the round ligament calcifies. In this patient with diabetes the two horns, extending from the lateral aspect of the uterus, represent calcifications of the round ligament.
Images courtesy of Ashley Davidoff, M.D.
Conclusion
In Part 2 of “Applied Anatomy of the Uterus’ we will discuss common diseases, which can be congenital or acquired, benign or malignant tumors. Systemic disease, especially infections, can also affect the uterus and uterine cavity.
From a clinical perspective, we will describe the more common ailments manifesting as infertility, menorrhagia, acute or chronic abdominal pain, urinary complaints, and recurrent abortions. The module will conclude with a overview of diagnosis and treatment options.