Introduction
The breasts are modified apocrine sweat glands that develop under the influence of the sex hormones to become the organs of lactation providing nourishment and immunity for the newborn. This organ is common to all mammals. The word ?mamma? in Latin means breast, with the word ?mammal? of course having similar origins.
The breast is anatomically characterized by its symmetric presence on the anterior chest wall and its overt difference in structure in the two sexes, so that for the female it is one of the major secondary sex characteristics.
Although the ducts and glands are all present at birth, full development only occurs later in life as the female becomes physically prepared and enabled for reproduction. Thelarche is the period when the breast buds start to grow. This occurs when the female is about 10 or 11 years. Maturation is complete at about 13-15 years, though structural changes occur under the influence of the hormones throughout life. During the reproductive phase of a woman?s life these changes are cyclical under the command of the menstrual hormones. During pregnancy and lactation more dramatic changes occur enabling the breasts to perform their major function of lactation with the volume of the breasts almost doubling in size. The lack of the hormones following menopause results in structural regression.
There is a wide variation in breast size, breast symmetry, and breast shape, but in general the external morphology of the breast during the reproductive age of the female is characterized by a hemispherical shape inferiorly more rounded and superiorly slightly concave.
The breast and nipple are oriented toward the axilla to facilitate and optimize breast feeding since the infant is best positioned in the curvature of the mother?s arms lateral to the breasts.
As a secondary sex organ with a prominent profile, the breasts command great power. The beauty of the female form arouses instinctual intimacy; while in society at large they provide inspiration for photographers, artists, and clothing designers. In the Western cultures the breasts are the primary symbol of femininity.

Overview
This section is intended to give you an overview or summary of the module. The detail will follow.As noted the breasts are modified apocrine sweat glands that develop to the same extent in both males and females during embryonic life and are similar structures in both sexes until thelarche when they develop in the female under the influence of the sex hormones to become the organs of lactation providing milk and nourishment for the newborn.
In the female, the breasts continue to change in structure and function throughout life. In the male they have no known function but are still subject to change under the conditions of obesity, and the abnormal influence of estrogen or progesterone. We will focus on the breast of the female for this module.
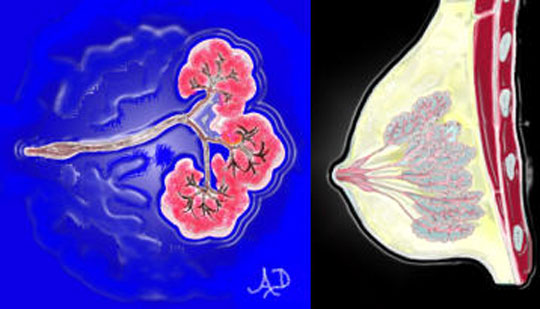
The breast is made up of radially positioned glands and ducts that converge on the nipple. There is a wide variation in breast size, breast symmetry, and breast shape. The size of the breasts is usually related to the amount of adipose tissue, but in the younger patient the stromal and glandular tissues may be more dominant. In general adipose tissue makes up 85-90% of the substance of the gland. Together with the connective tissue the adipose tissue surrounds, packs, and supports the glands or lobes.
The shape of the breasts changes during each physiologic phase of the female. In childhood they are flat, while in adolescence they become conical. As the breasts become fully developed the inferior part rounds out, while superiorly they become concave. The discrepancy in shape between the superior and inferior aspects of the breast is probably due to varying lengths and tensions of Cooper?s ligaments ? hair sized ligaments that provide support from the skin surface to the chest wall. With the aging process, the ligaments stretch or even break, the breasts lose support and they sag. In 1913 Mary Phelps Jacob a New York socialite, created the brassiere, in an attempt to prevent the dreaded droop. This Western industry capitalized on the social and cultural negative sentiment of the sagging breast. Prior to that, artificial support was in the form of a body corset with whalebones whose creation was attributed in the sixteenth century to Catherine de Medici.
The breasts are the seat of many diseases including fibrocystic change, fibroadenoma, mastitis, and carcinoma. Breast cancer unfortunately is the most common malignancy in women and is second to lung carcinoma as the leading cause of cancer death. In 1960 one in twenty women had the misfortune of developing breast cancer and that figure has increased to one in 8 currently.
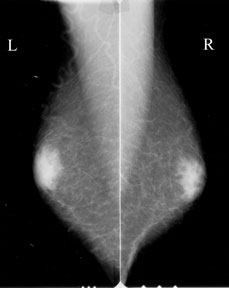
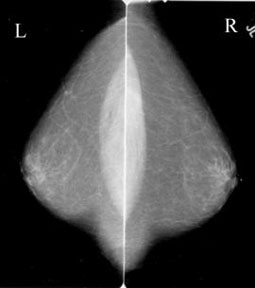
Diseases are commonly diagnosed by clinical examination, mammography, ultrasound and biopsy. Clinical concerns are raised mostly when an abnormal mass is felt, or a bloody discharge from the nipple is noted. The continued morphological changes create symptoms that may mimic disease, so that most patients have normal lumpiness in their breasts and many patients have a discharge as normal physiological events. Most small cancers are clinically silent and can only be detected by mammography. Screening mammography starting at age 40 is an essential strategy in the management of breast carcinoma.
Principles
In this section we attempt to put the structure and function of the breast in the context of the principles that govern structure and function in other parts of the body. When we look at the body as a whole we note for example that there are glands, supportive tissues, conducting and transport systems, protective systems, and controlling systems. Each organ usually has elements of all of these but is specialized to perform one of these functions that characterize it as a functional component of the body.The breast is a glandular organ, and is in fact a modified sweat gland. A gland is a collection of epithelial cells that produce a substance that is necessary for body function. In the case of the breast the functional substance produced is milk. The breast is a modified apocrine sweat gland. An apocrine gland is characterized by its mode of secretion where the secretion is pinched off from the apex of the cell and secreted into a duct that is about ten times larger than the duct of an eccrine sweat gland. Hair follicles are connected to an apocrine gland system. The larger diameter in the transport system of the apocrine gland is a necessary prerequisite to transport and store thick secretions. In the case of the breast, the thick secretion is milk. Storage of milk in the ducts places an unusual demand on the ductal system. One may think of this function as a mechanism to ensure that sufficient milk for the infant is available. The viscous secretion on the other hand may become impacted in the ducts and secondary obstruction and mastitis can result.
The other type of sweat gland that does not store secretion in the ducts is called an eccrine gland. Once secretion takes place, the sweat is immediately transported to the surface of the skin.
Milk is a life-sustaining nutrient for all mammalian newborns since it contains all the nutritional needs of the infant together with antibodies that are necessary to protect the baby who requires about six months to develop an adequate and independent immune system.
The glandular portion of the breast is an example of a compound tubuloalveolar gland. As a ?compound? gland it implies that the ductal portion is branched. As a ?tubuloalveolar? gland it is implied that the secretory element of the gland has both tubular and alveolar (grape-like) elements.
The transport system is a tube, and flow will depend on pressure differences across the tube, resistance, diameter length and viscosity of the medium being transported.
As an anatomical structure, descriptive features including size, shape, position, and character will define the breast. There will be a normal range for these elements, and abnormality will be recognized when these structural norms are disturbed by disease. These concepts govern and are applied in the evaluation of structures in pathology, radiology and clinical medicine. While size, shape, and position are self explanatory, character refers to how the structure looks, feels, and behaves when evaluated by the tools of the clinician, radiologist, or pathologist.
As a biological structure it will require lifeline connections including blood supply, venous drainage, and lymphatics. Vascular connections include arteries from the internal mammary and lateral thoracic arteries, while venous drainage is from similarly named veins.
All biological entities have a protective cover which in the case of the breasts is an outer layer of skin. Internally it is supported and protected by a thin, relatively flimsy capsule, together with fascial layers, Cooper?s ligaments, and surrounding fat. The breast rests on the pectoralis muscle.
For its functionality it depends on the organization of its glands and ducts, which as noted consist of 15-20 radially positioned lobes that terminate at the nipple.
The broad principles of space and time also apply to the breast. The breast occupies space and shares the space only with the structures of the anterior chest wall.
The breast changes with time and shows dramatic structural change during puberty, pregnancy, lactation, and aging.
Historical and Cultural Aspects
The breasts, unlike most other organs, have been a visible structure ever since the birth and evolution of the mammal. Although they have run the gamut of religious, psychological, and erotic environments in history, the study of its internal structure seems to have arrived relatively late.The breast was viewed as sacred (especially pre-1400), erotic (Renaissance and thereafter), political (French Revolution), psychological (as in Freud’s obsession), and medical (including breast cancer and cosmetic surgery).
Witcombe, a professor of art history at Sweet Briar College in Virginia explored the art and culture of the female figure in ancient civilizations. An electronic version of the work is available (Witcombe). Venus of Willendorf is probably the oldest figurine originating from the Stone Age (25000BC). The sculpture was found by Josef Szombathy in 1908 in Austria. She is believed to represent a goddess and is characterized by large breasts, abdomen, buttock and pubic area. (Witcombe image) A figure with similar proportions, “The Venus of Lespugue”, c. 30,000 BCE is also considered a deity and may even predate Venus of Willendorf. (Mazzola)
The Goddess of snakes from the Minoan culture in Crete (1600 BCE) is also felt to be a deity with implications of fertility and is characterized by the presence of a snake in both hands and two large protruding breasts. (Witcombe image)
Vesalius?s drawings of anatomy in ?De Corporis Humani Fabrica? of 1543 reveal one of the earliest interests in the internal structure. Da Vinci on the other hand, who demonstrated such in depth probing of the anatomy, has no established drawings of the dissected breast.
Classification Based on Function
The breast is an exocrine gland meaning that its secretion is transported into a ductal system. An endocrine gland on the other hand (for example the adrenal gland) secretes its products into the blood stream. The pancreas for example has both endocrine components (insulin secreted into the blood) and exocrine components (digestive enzymes secreted into the ducts).Functionally the breast is part of the reproductive system. Its primary role is to provide nutrition for the newborn infant, but it also provides essential cognitive and emotional aspects for the infant.
The breast acts as a secondary sex organ meaning that it is an organ that is not directly related to reproduction but enables physical distinction between the sexes. Voice depth and facial hair are other secondary sexual characteristics.
Classification Based on Histology
The breast is part of the skin and its glands. The skin contains two major layers – the epidermis, and dermis. The epidermis contains the hair follicles, sweat glands, sebaceous glands, nails and the mammary glands, while the dermis below consists of dense connective tissue.
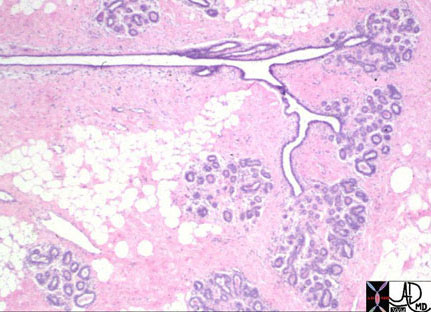
The functioning component of a gland is the epithelium, which in the case of an exocrine gland is organized around a ductal system. The epithelium in the breast is cuboidal meaning that the cells are almost square in shape. The shape, however, will vary from being flat to columnar depending on the stage of functional stimulation. Under the cuboidal epithelium in the lobules is a second layer of myoepithelial cells.
As a gland that has a lobular configuration, it is considered to be a compound tubuloalveolar gland. As a ?compound? gland it implies that the ductal portion is branched. As a ?tubuloalveolar? gland it is implied that the secretory element of the gland has both tubular and alveolar (grape-like) elements.
General
The female breast is a dynamic structure from month to month, with visible and palpable structural changes. These changes become more dramatic during pregnancy and lactation.
The structural changes that are visible and palpable to the patient are often combined with the ever-present fear of malignant disease.
Many patients, therefore, have multiple visits to their clinicians and radiologists, to allay or confirm their fears. An improved knowledge of the anatomy and the associated structural changes that occur with the physiology would serve all well.
Parts
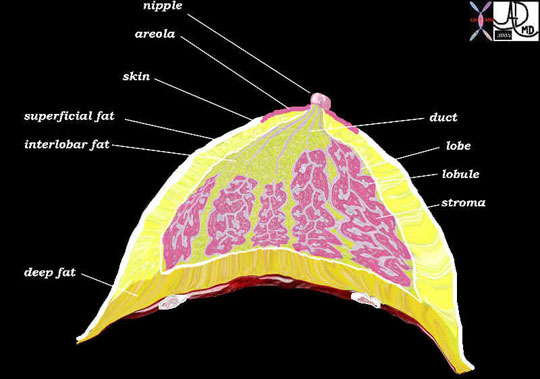
From a structural point of view the breast is a relatively simple organ. It consists of:
1) Skin with nipple and areola
2) Hypodermis consisting of adipose tissue, connective tissue and mammary apparatus.
The lobes of the breast are divided into lobules, which are the functional components of the breast.
Parts: Skin
The skin of the breast consists of two layers, the epidermis and dermis and is characterized by the addition of the nipple and areola.
The epidermis is the superficial keratinized squamous epithelium, which consists of five cell layers. These layers grow and progressively mature from the basal layer that generates new cells, to a superficial layer of keratinized cells that eventually slough and shed. The dermis consists of dense collagen, elastic tissue, blood vessels and nerves together with sweat glands and hair follicles.
Parts: Nipple
It consists of abundant nerve endings, dense collagenous tissue, smooth muscle, thick-pigmented keratinized skin, and the terminal components of the 15-20 lactiferous ducts. During lactation, stimulation of the abundant nerve terminals in the dermis of the nipple causes the release of oxytocin, which in turn causes contraction of the myoepithelial cells of the ducts and the nipples, resulting in the delivery of the milk. The smooth muscle that surrounds the ducts serves to straighten the nipple and the ducts in order to facilitate flow. The elastic tissue allows the nipple to stretch when the nipple is erect, and the fibrous tissue acts to support the nipple.
In the adult the size of the nipple ranges from ½ inch – ¾ inch and it may reach up to an inch during lactation. With age it usually retracts.
The nipple is positioned more laterally than centrally and directed up and out, a location, which is optimal for breast-feeding. In the infant it is usually opposite the 4th rib, during puberty it descends to the 5th rib and after lactation it descends to the 7th rib.
The shape of the nipple varies from person to person and also during different periods of life. In the child it is minimally raised and relatively smooth. In the adult it may be inverted (10%), flat, round or conical. At about 15 it develops a cleft near its center, which is the location, which houses the lactiferous ducts. Wrinkling progresses over the ensuing years.
In the young adult it is usually shaped like an inverted cone with the base having a relatively small diameter and the anterior aspect being flat. During lactation the base broadens and the anterior aspect narrows, resulting in a reversal of the cone shape.
In the lactating women the surface is relatively flat while the center continues to develop clefts. In the non-erect state the nipple thus appears puckered or wrinkled.
Within the nipple there are abundant melanocytes giving the nipple a darker hue compared to the skin. During infancy it is pinkish red, during puberty a florid red, and in young women a brownish red. At about the second month of pregnancy it darkens to an almost brown. It may lighten after lactation and pregnancy, but does not usually return to its original hue.
Although the skin of the nipple is hairless, the surrounding skin may have hair follicles.
The nipple and areola have a significantly thickened keratinized layer in order to protect them from drying and cracking that would otherwise result from continued sucking effects of breast-feeding. The sebaceous glands of the areola also assist this protective function by their oily secretion.

Parts: Areola
The areola is a modified part of the skin that is also slightly more pigmented than the surrounding skin. It contains an excess of sebaceous glands. It is circular in shape and surrounds the nipple. The color varies from pink to dark brown depending on parity and race. Muscle fibers are present in the areola, which will cause the areola to pucker when the nipple is stimulated, presumably to assist the straightening of the nipple during milk delivery.
At about the second month of pregnancy the color of the areola darkens and the sebaceous glands hypertrophy. With the onset of lactation these sebaceous glands (also called areolar glands) become quite prominent and remain as small tubercles called Montgomery tubercles after pregnancy and lactation. These Montgomery tubercles also appear to have ductal tissue associated with them. Their function is to secrete an oily substance to enable lactation by lubricating the nipple and also to protect the skin from the continued sucking action. The areola lightens once nursing is over, but it does not usually return to its former color.
Parts: Hypodermis
The hypodermis, also called the superficial fascia, is a layer of adipose tissue that lies deep to the dermis and superficial to muscle. The functional breast tissue lies within this layer. Three layers can be identified.
- A superficial layer of fat lies just below the dermis
- A middle layer of functional mammary apparatus of the breast, which consists of lobes, lobules, stroma, and interlobar adipose tissue.
- A deep layer of adipose tissue lies on the chest wall musculature.
Parts: Adipose Tissue

.
Parts: Connective Tissue Elements
The fibrous connective tissue component of the mammary apparatus varies from individual to individual and may be prominent in the young or the old and hence a postmenopausal patient may have dense breasts on mammography because the fibrous connective component (not the glandular component) is thickened. The connective tissue has no functional significance other than support of the breast tissues, but it is subject to the effects of hormonal influences and changes synchronously with other hormonally induced changes in the glandular elements. During lactation for example the glandular elements proliferate at the expense of the stromal elements.
Like the adipose tissue in the mammary apparatus, the connective tissue is present both between the lobes as well as within the lobules. The intralobular connective tissue contains more capillaries and is less densely collagenized than the interlobar connective tissue.
Parts: Mammary Apparatus
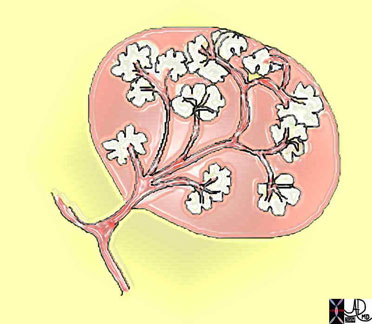
The mammary apparatus and connective tissues of the breast lie in the middle layer between the superficial and deep layers of adipose tissue, and are surrounded by a weak capsule within the hypodermis. The apex of mammary apparatus projects through the superficial layer of adipose tissue as it connects to the nipple. The middle layer consists of the lobes, lobules and interlobar tissues. The secretory parts of the breast are located in the lobes and lobules. A lobe, also called a gland consists of a single major lactiferous duct, which serves and drains a series of lobules, and which terminates at the nipple as a single opening. Within the lobules there are the acini, ducts, ductules, fibrous connective tissue and adipose tissue. The glandular elements are a pale reddish color to the eye and are usually prominent in the young and involute in the elderly when it is replaced by fat.

The mammary apparatus is roughly triangular or pyramidal in shape when looked at in cross section. The axillary portion in the upper outer quadrant of the breast is usually more prominent than the other parts of the breast. This component is called the Axillary Tail of Spence. The tail of tissue usually traverses a defect in the axillary fascia. This defect is called the Foramen of Langer.
In the young adult, the glandular component of the mammary apparatus is prominent, while in the postmenopausal woman it involutes and is replaced by intralobular fat. Replacement hormones would affect this process by continuing to stimulate the glandular elements of the breast.

Parts: Lobes

Each lobe is an individual gland. The lobe is encapsulated consisting of a main duct, 6-10 segmental ducts, and a progeny of ductules and acini in the form of lobules. The lobules are surrounded by stromal tissue and since this tissue is within the confines of the capsule encasing the lobe, it is called intralobar stromal tissue. (pink in the diagram below) The stromal tissue consists of connective tissue and microscopic adipose tissue. Outside the confines of the encapsulated lobes but still within the middle layer of mammary apparatus there is a variable amount of adipose and connective tissue as well. The adipose tissue and connective tissue that lies between the lobes is called interlobar stroma. (yellow in the diagram below) The word stroma is sometimes used to refer to a combination of fat and connective tissue, and sometimes used to refer to the connective tissue only. The terminology can be confusing.
Between the lobes and within the lobes there are blood vessels, lymphatics and nerves as well. The vascular bundle and nerves are more prominent within the lobes since this is where the activity of the breast takes place and hence the location where the lifelines would naturally reside.

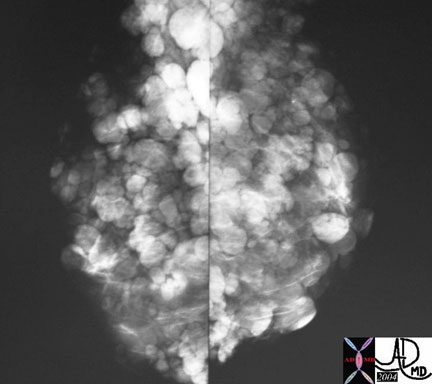
Parts: Lobules
The number of breast lobules has been estimated to be about one million. The lobules contain ducts, ductules, and the acini or alveoli.
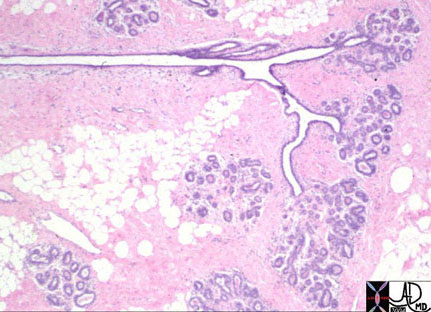
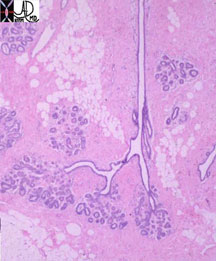
A terminal ductal lobular unit or TDLU consists of an intralobular terminal duct, ductules, and secretory units, which are called alveoli or acini.
The terminal duct lobular unit is the primary anatomical and functional unit of the human breast.

The terminal portions of the lobules differ in shape depending on hormonal influence. In the unstimulated state, while dormant, the terminal portions of the lobules are blind ending and tubular in shape. Under the influence of estrogen the terminal portions elongate still with tubular form. Under the influence of progesterone during the latter half of the cycle they bud and become grape like and rounded. Under the influence of prolactin during lactation, proliferate and become even more rounded with grape-like alveoli.
There are two types of epithelia in the breast. The epithelium of the ducts and the epithelium of the terminal duct lobular units, which are found in both the terminal ducts and in the acini. Within the lobule there are two types of cells; the luminal cells and the myoepithelial cells. During the early stages of pregnancy the lobules increase in size and number. During lactation the luminal cells proliferate. The true distinction between the ducts outside the lobule and those of the lobule is difficult to make, and strictly can only be made during lactation where the larger ducts show no change whereas the ductule of the lobule does show change.
Most diseases, both benign and malignant, arise from this highly active terminal lobular unit in which there is constant change of structure. This will be discussed in the applied anatomy of this section.
The intralobular stroma unlike most stromal tissue is quite active tissue with activity changes that parallel activity in the glandular tissue. Both the glandular tissues and the stromal tissues are under the influence of hormonal activity. Similarly when there is disease of the one component there are changes in the other. For example, when there is abnormal proliferation of stromal tissues there is consequent abnormal proliferation of the epithelium. Additionally, there is proliferation of the glandular elements during lactation with relative volume loss of the parenchyma.
As a ?tubuloalveolar? gland, it is implied that the secretory element of the gland has both tubular and alveolar (grape-like) elements. In the resting gland, the tubular elements dominate and at the peak of lactation there is florid dominance of the grape-like acini.
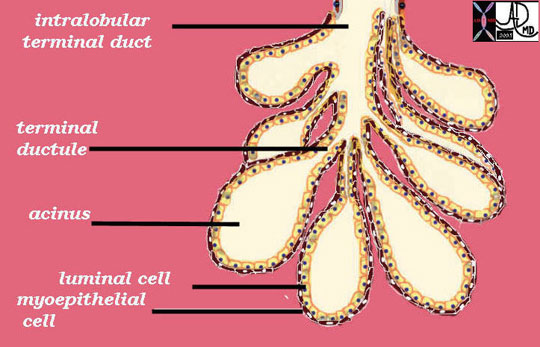
Parts: Ducts and Ductules
The duct of one gland or lobe is called the lactiferous duct. This duct has a small region of focal dilatation (measuring 2-4mms) called the ampulla (aka lactiferous sinus) present just before it enters the nipple. The ampulla serves as a reservoir for the milk. Each of the 15-20 ducts perforates the nipple with a separate relatively narrowed orifice. The lactiferous duct branches into segmental ducts that in turn give rise to the subsegmental ducts. The terminal portion of the subsegmental duct is called the extralobular terminal duct and it gives rise to the intralobular terminal duct as it enters the lobule. Each intralobular terminal duct enters an acinus of which there are many in a lobule.
At a histological level, the lactiferous duct is composed of two layers of cells ? a basal cuboidal epithelium and a luminal columnar epithelium. In addition there is are both longitudinal and transverse elastic fibers. Branches of the lactiferous duct are lined with a simple cuboidal epithelium.
The acinar structures achieve full physiologic development only with pregnancy. During lactation, the alveolar cells secrete milk, which is carried to the nipple via the ducts, and is expressed with the aid of the smooth muscle components, which are stimulated by the sucking reflex.
The acinar structures achieve full physiologic development only with pregnancy. During lactation, the alveolar cells secrete milk, which is carried to the nipple via the ducts, and is expressed with the aid of the smooth muscle components, which are stimulated by the sucking reflex.

Courtesy of: Priscilla Slanetz, M.D., MPH
Size
The size of the breasts varies significantly between individuals and is different in each individual depending on their age and functional state. The normal mature female breast ranges from less than 30 grams to more than 500 grams.
Because the breast is a major repository for fat, the size and density of the breast is greatly influenced by diet and muscle development. Difference in size between individuals and differences during different phases of life can be dramatic, and is related to a combination of weight, hormonal influence and genetic factors.
In the young the differences are usually related to hormonal differences and genetics while in the post menopausal women the relationship of breast size to weight and fat distribution becomes more relevant. The hormones mostly responsible for breast changes are estrogen and progesterone.
Estrogens cause fat deposition, duct elongation and branching, development of the stromal tissues, including the connective tissue and blood vessels. They have some effect on the lobules and alveoli but it is progesterone and prolactin that transform the breasts into lactating organs. Progesterone causes the alveoli and lobules to proliferate and enlarge and enable the organ to become secretory, but it is left up to prolactin to provide the final capability of milk production.

Size and Breast Maturation
Puberty is the first phase of breast maturation. Before puberty the breasts are small, and start to enlarge with the onset of thelarche at about 11 years, becoming fully developed at the age of 15 or 16 years. Early development of breasts has no bearing on the final breast size.
During puberty the anterior pituitary gland produces follicular stimulating hormone (FSH), which causes the follicles of the ovary to produce estrogen. Estrogen causes ductal development and proliferation of periductal fibrous tissues. Both these changes result in the enlargement of the breasts and the increasing firmness.
The second phase of breast maturation occurs with the onset of ovulation when progesterone becomes a factor in breast size. It is produced by the corpus luteum in the second half of the menstrual cycle, and is responsible for the proliferation of the glandular component of the breast development. Under the influence of progesterone stromal fluid accumulation occurs in the last few days of the cycle.
The intrinsic MRI signal differences between parenchyma (glandular tissue and stroma) water and fat makes evaluation of breast changes relatively easy to study using MRI. During a single cycle the parenchyma increases by more than 30%, while water content increases by about 25%.

Size and Pregnancy
During pregnancy the breasts increase significantly in size, increasing by about 400 grams per breast, under the influence of estrogen, progesterone, growth hormone, insulin, and cortisol. Prolactin also plays a role of breast enlargement during pregnancy resulting in an overall average increase in size of about 145mls. The higher levels of estrogen result in progressive proliferation, elongation, and dilatation of the ductal system while progesterone is mostly responsible for glandular development. Most of the fat of the breast is replaced in late pregnancy by enlarging glandular tissue necessary to produce milk. The nipple and areola become deeply pigmented and increase in size as well.

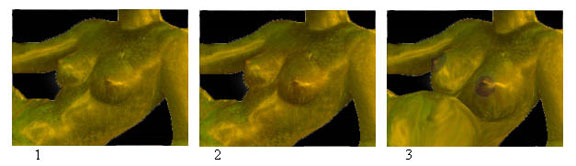
Courtesy of: Ashley Davidoff, M.D.
Courtesy of: Ashley Davidoff, M.D.
Size Following Birth and Delivery
Following birth and delivery of the placenta there is a sudden drop of estrogen and progesterone levels. Prolactin plays an increasing role in breast function and morphology as milk production is initiated and continued throughout the nursing period.
As the infant starts to suck on the nipple a reflex production of prolactin from the anterior pituitary gland occurs. The prolactin in turn stimulates a cascade of hormonal events with a subsequent cascade of flowing milk. As stated, the ducts of the apocrine glands act as storage sites for the milk produced by the acini. The breasts are larger by about 10-20% as they become distended with milk. In the first two days post partum there is only about 50ccs per day of milk produced, which increases dramatically to 500ccs per day by day four. At three months post partum this usually plateaus at 850-1000ccs per day. If the mother feeds every four hours then at peak production prior to feeding there should be about 120ccs of milk in the breasts equating to about 50-60ccs per breast. The rate of milk production has been estimated at between 10-60ccs per hour. The basic size of the breast has no bearing on the volume of milk. At the peak of lactation the breasts become almost double their baseline size.

.
Size and Advancing Age
With advancing age, glandular and stromal tissue atrophies but fatty tissue may become quite abundant. The breasts may become very large in postmenopausal life due to fat accumulation. Hormonal supplementation may cause added increase in size. In advanced age the breasts usually shrink as the fat regresses.
Psychologically the size of the breasts to some cultures and individuals has been linked to sexuality. Breast surgery both enlargement and reduction, is a well known and accepted method used for psychological benefits.
In summary, the size of the breasts relates to a combination of the quantity of fat, glandular tissue and stromal tissue. The glandular, ductal, and stromal tissues change by month, with growth and regression while under the influence of estrogen and progesterone. The amount of fatty tissue relates to a combination of hormonal, hereditary, racial factors, nutritional factors, body size, and age. Overweight patients for example tend to have larger breasts.

Applied Anatomy -Size
The breasts in up to 50% of women are unequal in size. Difference in size may occur during development and may become symmetrical with maturation. The left breast is generally a little larger than the right.

Courtesy of: Ashley Davidoff, M.D.
The glandular tissue is not uniformly distributed within the breast. The axillary parenchymal tissue is thickest followed by the inferior aspect, sternal aspect and then the clavicular aspect. This dominance of tissue in the upper outer quadrant has clinical relevance. Cyclical discomfort is most commonly felt in this region, and about 50% of carcinomas occur in this region as well.
The overlying skin of the breast should be less than 3mm thick. This has important implications in the evaluation of the breast in mammography since thickening of the skin implies a pathological process.

Courtesy of: Ashley Davidoff, M.D.
Congenital absence of the breast does occur but is rare. It is called amastia. When it is unilateral it often occurs with ipsilateral absence of the pectoralis muscle. When it is bilateral it is usually associated with other anomalies. Reference to amastia is thought to be present in the Songs of Solomon “We have a little sister, and she hath no breasts” (Song of Songs VIII:8).
Polymastia on the other hand occurs in between .2 – 2% of females, and less commonly among males. It is characterized by accessory breast tissue that occurs along the milk line starting in the axilla, proceeding with an anterior arc through the normal nipples, and ending in the groin. Hormonal changes and diseases that affect the normal breast can affect the accessory breast tissue as well. If there are accessory nipples without breast tissue the condition is called polythelia or supernumerary nipples.
The number of breasts differs among mammals. Humans and guinea pigs have two, cows have four, cats have eight, and dogs ten. The size of the breasts also differs significantly among mammals and bears no relation to the relative size of the animal. Cows have enormous udders while horses have relatively small breasts. Goats also have breasts that are relatively large compared to sheep that have relatively small breasts.
Applied Anatomy in Males
The testes normally secrete circulating estrogen produced in small amounts but it is rapidly and effectively metabolized by the liver so that in health there are no overt estrogen effects on the male body. However in liver disease, when the liver is unable to catabolize the estrogen, excess estrogen circulates which may cause breast growth. This condition is called gynecomastia. There are other stages in the normal male such as in puberty and old age where excess estrogen causes breast tissue proliferation. In the pubescent male this may be unilateral or bilateral but is usually self-limiting after a few months but may be present for up to three years. In obesity there is also an excess of estrogen, which may have the same effects on the male breast. Certain drugs such as anabolic steroids illegally used by athletes as well as other illegal drugs such as marijuana and heroin can also cause gynecomastia. Drugs used in the cardiovascular system including digoxin, spirinolactone and reserpine are well known causes of gynecomastia.


Shape
Like the size of the breast, the shape of the breast is very varied and depends upon genetic factors, racial factors, dietary factors, age, parity, and menopausal status.
However, in general the shape of the breast is almost hemispheric, with the superior surface arising more gradually from the chest wall. The superior border is relatively long and flat (sometimes minimally concave) and the inferior border is rounded and shorter.
The shape of the breasts changes during each physiologic phase of the female. In infancy there is a variable amount of breast tissue due to the transplacental effect of the maternal hormones and there may even be milk production known as ?witches milk? in either sex. In childhood the breasts are flat, while at the onset of thelarche they become conical. As the breasts become fully developed the inferior part rounds out, while superiorly they become concave. The discrepancy in shape between the superior and inferior aspects of the breast is probably due to varying length and tension of Cooper?s ligaments ? hair sized ligaments that provide support from the skin surface to the chest wall. With the aging process, the ligaments stretch or even break, causing the breasts loses support and as a result they sag.

Shape with Position
The shape can change significantly with position of the person, with the physiologic state, and based on the innate structural make-up of the breast. Thus, the firm breasts of the adolescent (prior to any pregnancy related change) may change very little with position, as opposed to the other extreme of the senile breast that would sag without support.
The shape of the breast also changes with position so that in the supine position they fall to the chest sides and flatten whereas in the decubitus position and prone position they elongate and in the upright position they move downward and flatten.
Although mammoplasty with implants can reproduce and enhance the size of the breasts, reproducing the shape of the breast is a real challenge that is mostly not achieved.


Position
The breast is found as a paired organ on the anterior chest wall, anterior to the pectoralis muscle and the serratus anterior muscle.

Courtesy of: Ashley Davidoff, M.D.
The breast overlies the second to sixth or seventh rib, lying within the hypodermis and superficial to the anterior fascia of the pectoralis major muscle.
Landmarks of its medial and lateral borders correspond to the lateral sternal border and laterally to the anterior axillary fold.
The breasts develop along the lateral line, primitive milk streak or “galactic band”. As previously noted this line runs from the axilla through the nipples arcing slightly anteriorly and then coursing back to the inguinal regions.
In the human, the breasts seem to have been positioned under the watchful eye of the nursing mother whereas in animals it seems like they have been positioned for protection from injury. In the cow, elephant, horse, goat and deer they are in the inguinal region and in the whale the breasts are on either side of the anus. The monkey and bat have breasts that are positioned anteriorly and laterally ? similar to positioning in the human.
The glandular tissue as stated above is radially oriented around the nipple with a preponderance of parenchyma in the upper outer quadrant in the tail of Spence.
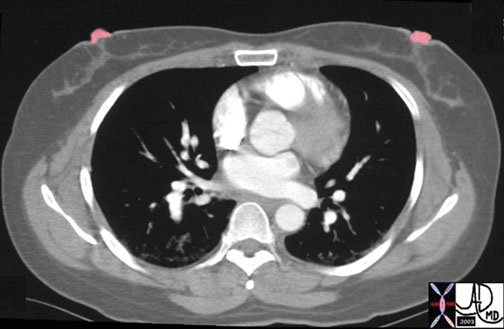
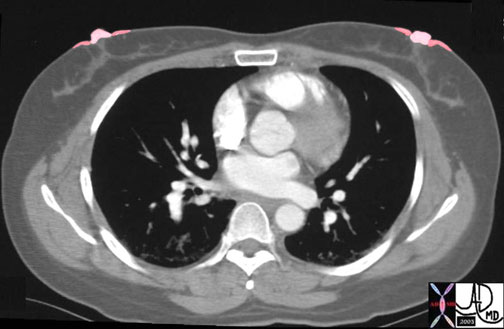
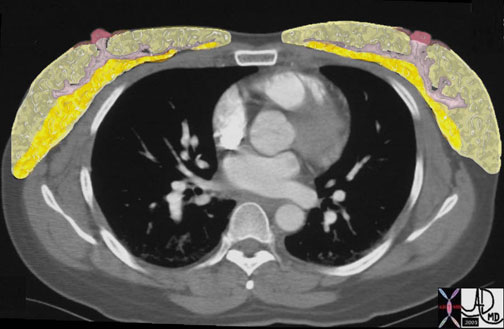
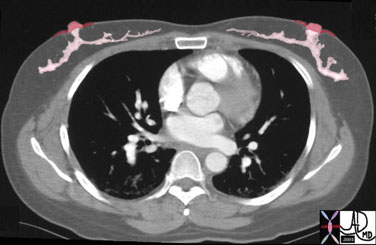
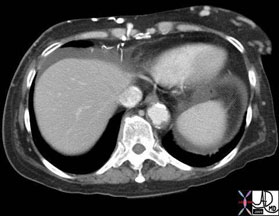
The glandular tissue is normally separated from the pectoralis muscles of the anterior chest wall by a fat plane and from the skin by adipose tissue as seen in the next image. This is called the retromammary layer of fat.

Position: Applied Anatomy
Malignant disease that originates in the lobules and ductal system is considered ?in situ? as long as the basement membrane does not get breached. The transgression of the basement membrane is an important microscopic and biological sign that the lesion has evolved into an aggressive entity and requires a plan for aggressive treatment. If not diagnosed at this point, a malignant lesion will progressively advance through the relatively weak caspular barriers of the lobe, mammary apparatus, and finally through the more resilient barrier of the skin, or posteriorly through the pectoralis fascia into the muscle. At this stage the cancer is classified as a stage III cancer. Stage I disease is the earliest stage with no spread of the disease, while stage IV is the most advanced disease, with widespread involvement of other organs beyond the breast.

Peau d?orange (peel of an orange in French) is a clinical sign in which the skin of the breast is likened to the dimpled skin of an orange. In this entity the lymphatics are obstructed and the skin becomes edematous. As a result there is a dimpling of the skin.

Character
The adipose tissue in general makes up 80-85 % of the breast gives it a soft feel and together with the stroma and glands the breast is characterized as having a rubbery feel. However, in general, the glandular portion of the breast has a firm, slightly nodular feel, while the fat is almost always soft.
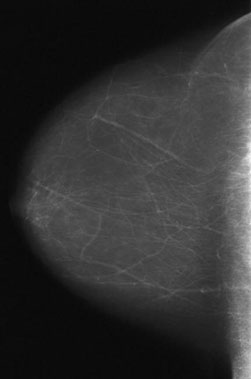
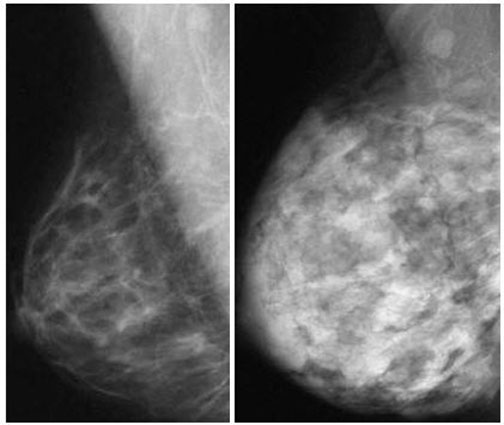
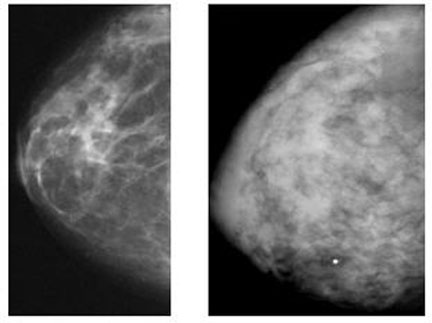
As we have noted above there are breasts where 80% of the breast is fibroglandular and others where the fat predominates. It is more common to see the dominance of fat in the breast of older patients, and fibroglandular dominance is usually seen in the young, though there is wide variation.
The breasts become firmer in pregnancy and lactation, but become softer and less rubbery with aging, mostly due to glandular regression and proliferation of fat.
Consistency of breast lobes varies from woman to woman, and will vary during the cycle, and may even vary in an individual from one side to the other.
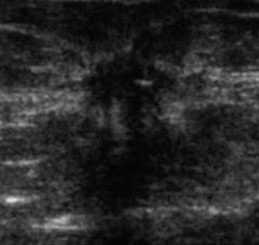
The ducts of the breast are usually not palpable unless they are engorged with milk, inflamed or contain a tumor.
The areola is of a delicate rose-colored hue in the nulliparous patient but enlarges and darkens with pregnancy, and may even become black. After pregnancy it may lighten but it never returns to its former rose-colored hue. The nipple also starts out as rose-colored structure, usually being slightly darker than the areola and darker than the skin. It also darkens with pregnancy.
Character: Applied Anatomy
The discrepancy in textures between the adipose tissue and the mammary apparatus, allows one to outline the lobes by carefully palpating the breast. When the breasts feel thick and lumpy the entity of fibrocystic change probably exists. This finding implies that the fibroglandular elements are enlarged. This enlargement is not necessarily abnormal.
The finding of a mass or a focally enlarged and hardened part of the breast is a significant finding and further characterization is important. It is essential to determine the mobility of the mass and get a feel as to whether it is tender (usually a finding in benign disease), whether it is fixed to the skin or deep muscles (a bad sign), and whether there are associated findings such as other masses, nipple discharge, or regional axillary adenopathy.
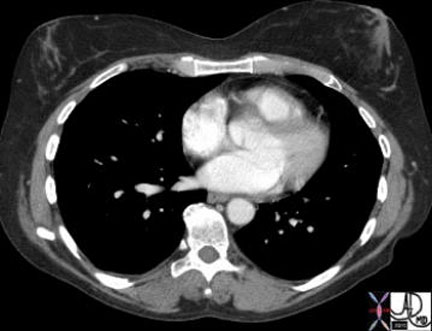
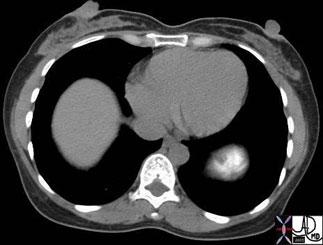
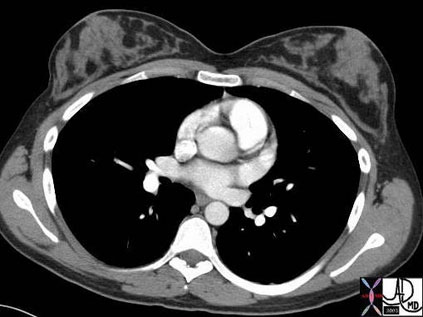
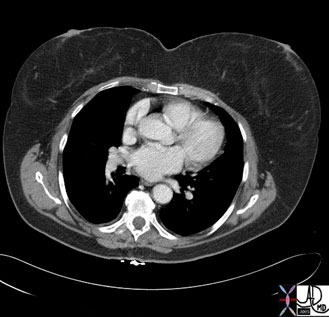
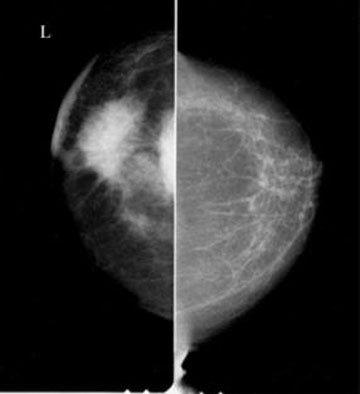
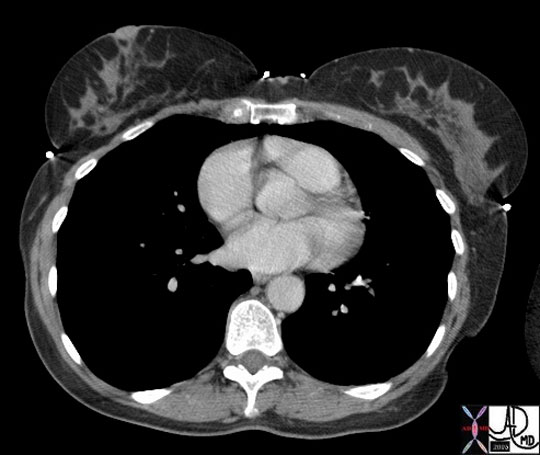
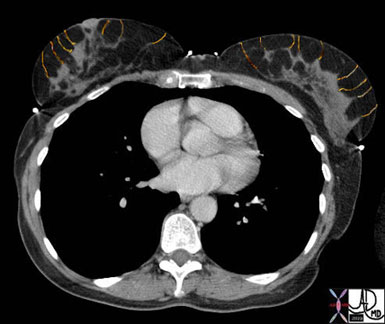
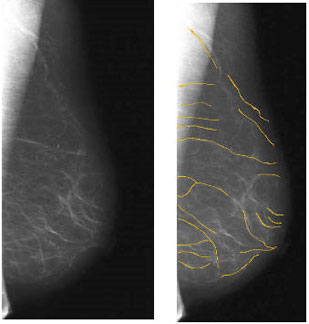
The radiographic difference in density between the parenchymal tissue and the fat allows structural evaluation and forms the basis for mammographic imaging, Ultrasound imaging, Computed Tomography (CT), and Magnetic Resonance Imaging (MRI).
Courtesy of: Ashley Davidoff, M.D.


Support
Cooper?s ligaments run between lobes and lobules and span the breast from the corium of the skin to the fascia of the muscle. Cooper’s ligaments are composed of dense fibrous tissue.
They keep the breasts in their characteristic shape and position. In the elderly or in pregnancy these ligaments become loose, stretched, or may even fracture. As a result the breasts sag and they do not return to their former tension.
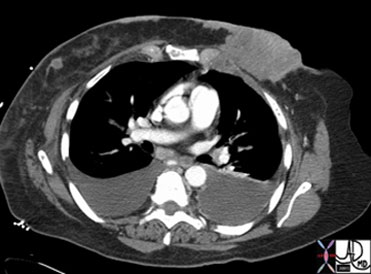
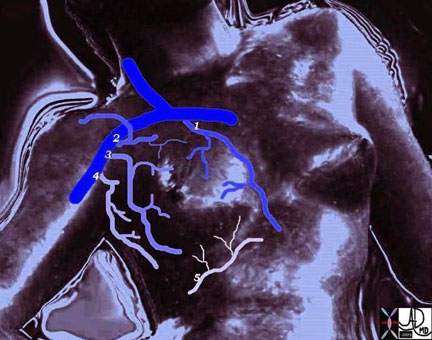
Blood Supply
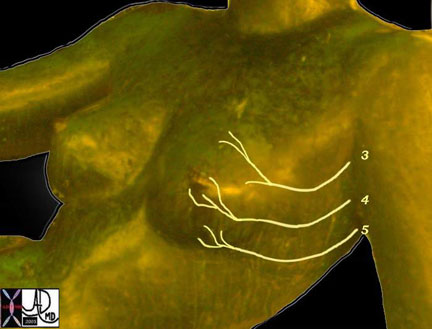
The breast is supplied with blood from five sources. The main vessels that supply the breast are the internal mammary artery (internal thoracic) that arises from the subclavian artery and lateral thoracic artery that arises from the axillary artery. The thoracoacromial artery and the thoracodorsal artery are two other arteries that supply the breast and they both arise from the axillary artery, which is a continuation of the subclavian artery. The intercostal arteries of ribs 3-5 are the last of the 5 vessels that supply the breast. They arise posteriorly from the aorta and anteriorly from the internal mammary artery, thus forming a circumferential ring around the chest.

The blood of the breast skin depends on the subdermal plexus, which is in communication with underlying deeper vessels supplying the breast parenchyma. There is a particularly rich periareolar plexus.
In the world of plastic surgery this rich blood supply allows for a variety of reduction techniques, ensuring the viability of the skin flaps after surgery.

Courtesy of: Priscilla Slanetz, M.D., MPH
Venous Drainage
Venous drainage is mainly to the axillary vein, but also to the internal thoracic, lateral thoracic, and intercostal veins.
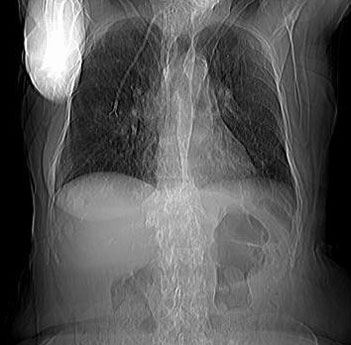
Blood Supply: Applied Anatomy
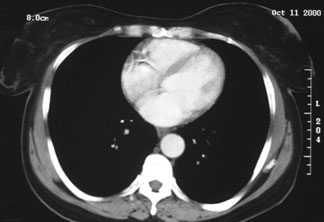
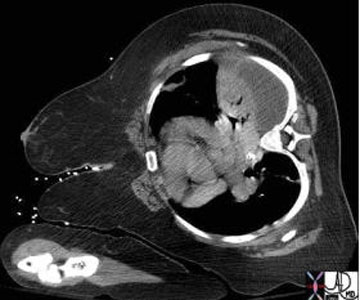
Normal engorgement of the veins occurs during lactation, but also occurs in congestive failure. The veins of the breast are sometimes utilized as collateral vessels when the superior vena cava is obstructed.

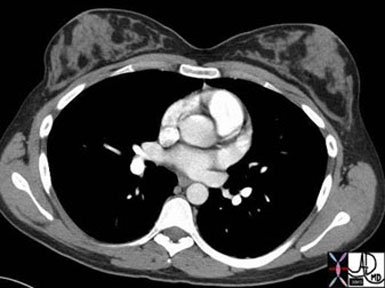
Lymphatic Drainage
The breast has a very rich supply of lymphatics with the dominant flow being toward the axilla. The lymphatics originate in the lobules and they accompany the veins and ductal systems coursing toward the nipple and areola. An extensive network develops in the subareolar region called the subareolar plexus.
There are about 35 nodes that drain the breast and they are basically divided into four regions. The axillary nodes are the largest group and they drain about 75% of the breast. The other major groups include the parasternal group, the infraclavicular group, and the supraclavicular group.

Courtesy of: Ashley Davidoff, M.D
Lymphatic Drainage: Subgroups of the axillary system of nodes
There are subgroups of the axillary nodes that mostly lie alongside the veins described above. The first of these is called the anterior pectoral group (aka low axillary nodes) consists of about four nodes and are distributed alongside the lateral thoracic vessels on the lateral border of the pectoralis muscles. The nodes that lie along the axillary vein are called the central axillary nodes. The nodes that lie alongside the subclavian vein are called the subclavian nodes.
There is a set that is not necessarily associated with any specific vein that lies deep to both pectoral muscles under the breast. This group is called the deep fascial system and they drain into set of nodes between the pectoral muscles called Rotter?s nodes. Subsequently some of these nodes will drain into the subclavian nodes and some will drain medially into the internal mammary system, which finally drains into the mediastinal nodes.
The other regions described including the infraclavicular, supraclavicular and internal mammary lymphatic drainage are less dominant sites. Even more uncommon is drainage to the infradiaphragmatic nodes.
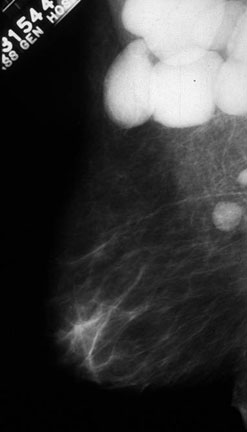
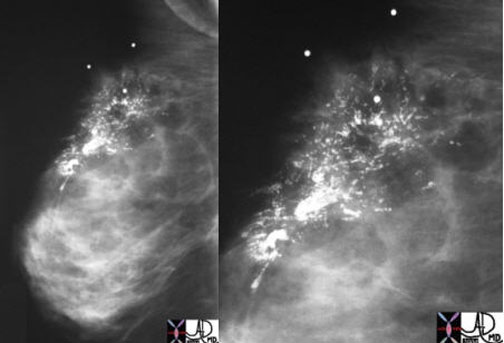
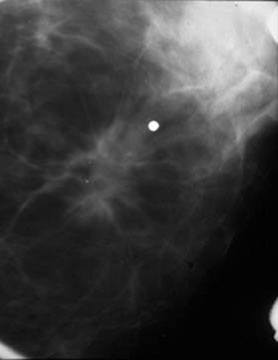
It should also be noted that there are intramammary lymph nodes that sometimes masquerade as a breast mass since they have features. On mammography they are typically reniform in shape, have a fatty or radiolucent notch, are less than 1 cm in size and are usually in upper outer quadrant.
Lymphatic Drainage: Applied Anatomy
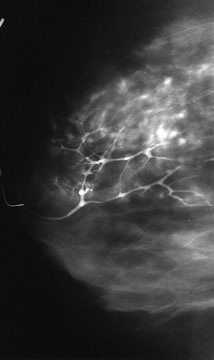
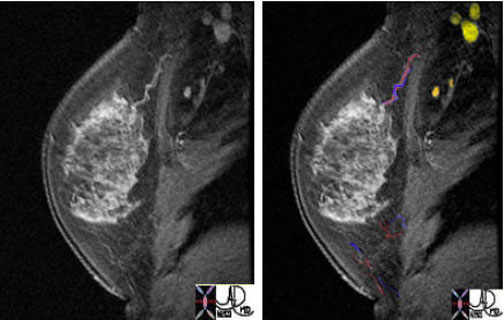
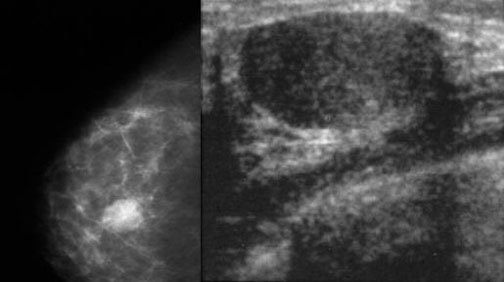
In the following mammogram and intramammary node is seen.


The staging and hence the management of breast carcinoma depends to a large extent on whether the lymph nodes of the breast are involved. Most of the search for disease is directed to the axillary group of nodes. Clinical examination is the first step, mammographic findings the second, sentinel node evaluation using radiopharmaceuticals the third, and surgery and microscopic evaluation the fourth. In cancers involving the medial breast tissue, when the axillary nodes are negative the internal mammary chain is involved in only about 15% of cases, and in lateral cancers the internal mammary nodes are only involved in about 5% of cases.
The sentinel node is defined as the first lymph node to drain a region of the breast and in the setting of breast carcinoma would be the first node to contain metastatic disease. Thus if a patient with biopsy proven carcinoma is on the surgical table to have the carcinoma removed, the question of staging and management comes up while the patient is on the table. Isosulfan Blue dye or radiolabeled technetium sulfur colloid would be administered into the subcutaneous tissue and the first node to pick up the tracer would be identified as the sentinel node. The surgeon would resect this node and submit it to pathology for frozen section, which means an immediate ?wet read?. If it is positive the tumor is upstaged and further dissection of the lymph nodes required. If negative, no further evaluation of the lymph nodes would be required since the implication is that the sentinel node reflects the status of the regional spread or lack of spread. In the past all axillary nodes would have been removed with consequent morbidity, including significant swelling of the arm from lymphedema and consequent cellulitis.
Surgical approach to lymph node dissection and resection requires dividing the nodes into three levels, going in general from lateral to the breast, to deep and under the breast and pectoral muscles, to deep and medial to the breast. More specifically, a level I dissection is bordered by the axillary vein superiorly, the lateral border of the pectoralis major and minor muscles medially, and the latissimus dorsi muscle laterally. A level II dissection includes nodes below the pectoralis minor muscle, and a level III includes nodes medial to the pectoralis minor muscle and below the costoclavicular ligament. In general if a patient requires lymph node dissection, resecting nodes from Level I and II is considered adequate.
Nerve Supply
The breast is supplied with cutaneous fibers from the anterior and lateral cutaneous branches of the third through fifth intercostal nerves. The autonomic components of these nerves supply the smooth muscles of the skin, nipple, acini and blood vessels. The parenchymal tissue is regulated by hormones.
Nerve supply provides sensory and sympathetic fibers supplying the skin, smooth muscle of the areola and nipple, blood vessels, and mammary gland.
Nerve Supply: Applied Anatomy
Nipple sensitivity to sucking is the important starting point of lactation. The nipple is supplied by the 4th dermatome. The stimulus created by the suckling infant is transmitted via the 4th intercostal nerve. Once the sensation of sucking is sensed at a neural level, there is a complex series of neural and hormonal events that cause the acini to contract, the nipple to become erect, sebaceous glands to secrete an oily protection, and lactiferous ducts to straighten enabling a smooth flow of milk from the acini and ducts to the infant. There is also a supratentorial feeling of pleasure created by this compound event that further enhances a most important biological event.
Skin and Capsules
Although we have covered the various protective covers in the sections above it is worthwhile reviewing the coverings of the breast with a relative perspective in relation to each other.
Each unit of the breast has a covering. The skin represents the first cover. The chest wall with the pectoralis muscle and its fascia represent the outer posterior cover of the breast. The capsule of mammary apparatus is the second cover, while the capsules of the individual lobes represent the third cover. Each lobule has a capsule and each acinus has a basement membrane, which acts as a barrier or ?capsule?. Each cell of course has a cell membrane.
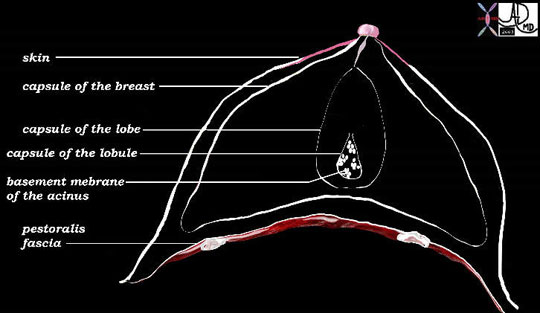
The skin provides the most resilient barrier. The mammary apparatus capsule, lobar capsule and lobular capsules are relatively weak while the basement membrane and cell membrane relatively strong. The capsule surrounding the normal mammary apparatus has a normal defect in the upper outer quadrant through which the axillary tail of Spence protrudes. This defect is called the foramen of Langer.

Relations
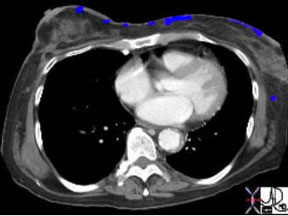
The mammary apparatus itself is completely surrounded by adipose tissue with a superficial layer lying deep to the dermis and the retromammary layer lying anterior to the pectoralis major muscle. Outside of the breast proper, the most important structural relation of the breast is the pectoralis major muscle and its fascia, which form the posterior border of the breast. The serratus anterior to lesser extent also forms a part of the posterior border. Its other borders include the clavicle superiorly, the sternum medially, 6th and 7th rib inferiorly.
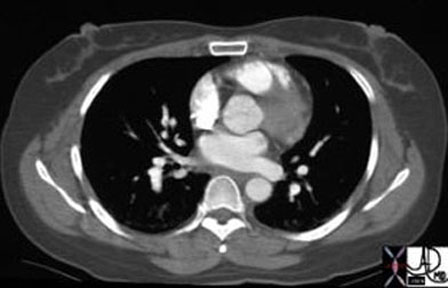
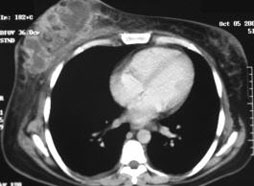
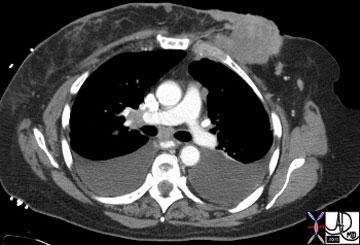
Relations: Applied Anatomy
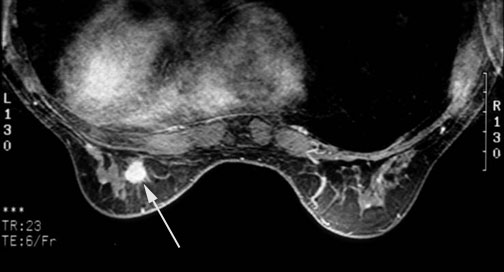
The involvement of the pectoralis fascia by a malignant mass is an important consideration in the staging of breast carcinoma, which was discussed previously. The pectoralis muscle can be identified by CT, MRI, and also by ultrasound.

Diseases and Conditions: Benign Diseases
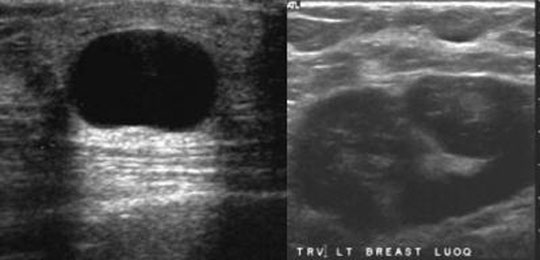
Benign breast masses are common and include predominantly fibroadenomas and fibrocystic disease. Cysts are part of the fibrocystic group of diseases.
Fibroadenomas are the most common breast lesion particularly in women under the age of 40. It is a benign neoplasm of the stromal and epithelial elements. The characteristic finding of a fibroadenoma is its smooth borders on mammography and US.

Diseases and Conditions: Fibrocystic Disease
Fibrocystic changes in the breast are the most common entity of the breast and accounts for the common lumpy bumpy feel of normal breast tissue. It is a benign entity that arises from the TDLU. The pathology is caused by proliferation of the connective tissue and or epithelial tissue, resulting in cystic change and or fibrous changes. It has a variety of clinical, imaging and pathological variations including a single dominant cyst, a diffuse irregularity caused by fibrocystic change and diffuse irregularity with a dominant lesion. The entity is subject to morphologic changes with hormonal changes of the menstrual cycle, and it may be associated with pain. The lesion is most common in the upper outer quadrant where the lobules are more voluminous in the tail of Spence.
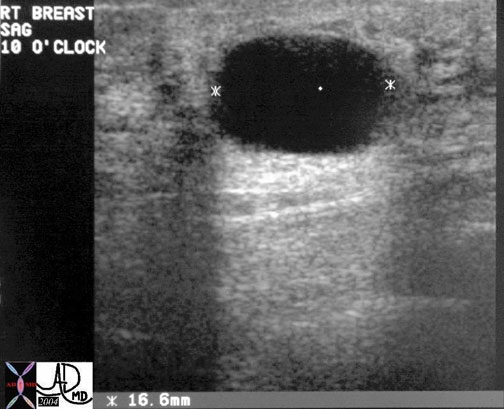
Diseases and Conditions: Fibroadenoma
Fibroadenoma is a common benign disorder of younger adult women that arises from the intralobar connective tissue elements and from epithelial elements. Unlike the cyst above the fibroadenoma presents on ultrasound as a well-circumscribed solid lesion.


Diseases and Conditions: Masses
An irregularly-shaped mass, particularly if spiculated, is concerning for malignancy. A spiculated lesion is concerning whether it is identified on mammography, ultrasound, MRI, or CT. The density of malignant lesions is also slightly greater than soft tissues. The high density of a carcinoma is characteristic of the scirrhous carcinoma.


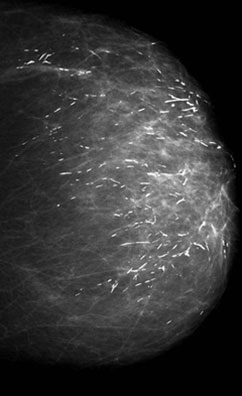
Diseases and Conditions: Calcifications
Diseases and Conditions: Breast Carcinoma
Most diseases both benign and malignant arise from this highly active terminal ductal lobular unit (TDLU) in which there is constant change of structure.
The carcinomas are the most significant lesions of the breast. There are two major types of breast carcinoma that arise from the lobule namely ductal carcinoma and lobular carcinoma. They both arise from the TDLU.
Carcinoma of the breast at this level is divided into the non-invasive or ?in situ? carcinomas on the one hand and the invasive carcinomas on the other. The ?in situ? carcinomas are restricted to the lobule and do not show invasion of the basement membrane, while in the invasive group, there is obvious transgression of the basement membrane.
The ?in situ? group has variable behavioral patterns and outcomes. These lesions may remain dormant for a lifetime, or may even involute. They do however place the woman at increased risk of developing cancer and should therefore be treated with heightened awareness.
The two types of ?in situ? carcinomas are called ductal carcinoma in situ (DCIS), and lobular carcinoma in situ (LCIS) and they are very different. DCIS is common and occurs in 70-95% of women at autopsy and is commonly associated with microcalcifications on mammography. It arises from ductal epithelium. LCIS is less common, clinically and radiologically more elusive, occurs in 1-5% of biopsies, and is rarely associated with microcalcifications on mammography. Once LCIS is identified the risk of developing cancer if untreated is about 30% within 20 years of diagnosis. It is not considered a precancerous disease, but a marker of increased risk.
Invasive Carcinoma
The invasive carcinomas of the breast are correspondingly called invasive ductal carcinoma and invasive lobular carcinoma and are defined by the transgression of the basement membrane by malignant cells.
The most common site of involvement is the upper outer quadrant since as we have learned it is the location of ?extra? tissue called the axillary tail of Spence. The presence of a larger amount of glandular tissue raises the relative incidence of disease in this quadrant. About 45% of carcinomas arise from this upper outer quadrant.
Invasive ductal carcinoma is the most common type of carcinoma and it has a tendency to incite a fibrous response, which has structural consequences. Firstly fibrous tissue is very dense so that this type of tumor has a relatively dense appearance on mammography. The scirrhous and desmoplastic nature of fibrosis also causes a tugging effect on other structures such as the Cooper?s ligament, the skin or the nipple so that retraction of these structures can occur. Peau d?orange is the dimpling of the skin in carcinoma that is reminiscent of the dimpling seen in the skin of an orange, and it is caused by the effect of the carcinoma on the ligaments of Cooper. New onset of nipple retraction is also an important warning sign of cancer.
Diseases of the Ducts
Disease of the larger ducts is relatively uncommon. Duct ectasia is a dilatation of the major ducts just behind the nipple that occurs in women nearing menopause and is really a normal finding. Accumulation of secretions may cause blockage of the duct, which can then become symptomatic.

Nipple Discharge
Nipple discharge is the third most common breast symptom after mass, and pain of the breast. Discharge is a normal event in women who are in the reproductive age. On self-examination, 50-60% of women can express some secretion. It is uncommon that a discharge is associated with breast cancer. Causes of nipple discharge include persistent secretion after pregnancy, benign hormonal affects, and mammary duct ectasia. Phenothiazines may also cause a nipple discharge. Benign features include bilaterality, and the involvement of multiple orifices. Bloody discharge that is spontaneous, from a single duct should raise concern for malignancy, but even so, only 10% of these patients have an underlying malignancy. Intraductal papilloma is the most common cause.

Paget?s disease of the nipple is a rare disease characterized by eczematous change of the nipple and almost always associated with an underlying breast carcinoma, specifically with high grade DCIS. The areola may also show eczematous change. It occurs in about 12% of patients with breast carcinoma. The findings in the nipple may be the only indication of disease, and so a new scaliness of the nipple warrants serious attention of clinician, mammography technologist, and radiologist. Only about 50% of patients with Paget?s have a radiographic abnormality on mammography.
Embryology
The breasts develop from a combination of ectoderm and mesoderm along the galactic line, which is a primitive symmetrical multicentric line from the axilla to the groin. In the human only two foci of the future breasts anterior to the pectoralis muscles develop. All the others regress during development. During the 5th week, part of the epidermis differentiates as a downgrowth into the mesenchyme below resulting in a ridge of tissue. There is a structural fusion of these primitive tissues. The ectoderm will develop into the glandular and ductal components while the mesoderm will develop into the connective tissue elements, and blood vessels. At the 10th week the bud begins to branch as a tubular structure. By the 12th week the secondary bud, starts to elongate and branch. By weeks 12-16 the infrastructure for the future ducts and acini are present. Maternal hormones including estrogen and progesterone that cross the placenta are responsible for early proliferation of the ductal and glandular tissues. From the mesenchyme smooth muscle differentiates and helps form the nipple and areola. Two months before birth the lobules mature and in both males and females colostrum may be secreted. It is not uncommon for both male and female infants to have prominent breast tissue at birth due to the high circulating levels of estrogen and progesterone. The prominence of breast tissue usually resolves in the first 3-4 weeks but in the breast fed infant it may be prolonged. Palpable glandular tissue should disappear by six months.
Growth
The breast buds, consisting mostly of blind ending ducts, lie dormant for about 11 years until thelarche. Thelarche is the period when the breast buds start to grow. The term thelarche comes from two Greek words “thele,” meaning nipple and ?arche,” meaning beginning. With the onset of puberty the ovaries start to produce estrogen and progesterone under the influence of follicle stimulating hormone produced by the hypothalamus. Estrogen is responsible mostly for proliferation of the ducts and progesterone in the presence of estrogen is responsible for proliferation of the acini and stroma. Under progesterone the blind ending ducts start to bud, producing the epithelial lined acini, which are capable of secretion. Other hormones including prolactin, growth hormone, ACTH, thyrotropic hormone and insulin assist in the development of the breast.
The external characteristics of the changes are divided into 4 stages. At stage 1, the breast is prepubertal and only the tip of the nipple is raised. Under the influence first of estrogen alone the breasts start to develop. In stage 2 the buds appear, the breast and nipple become raised, and the areola enlarges. During stage 3 the breasts enlarge further and the early influences of progesterone produce stromal and some glandular proliferation. In stage 3 the nipple and areola complex enlarges and rise above the breast forming a secondary mound of tissue. In stage 4 the breast rounds out bringing it level with the areola, while the nipple remains above (anterior to) the breast and areola. Full maturation is usually completed in 4 years at 15 or 16 years. However it can take as short as 18 months to as long as 9 years.
It should be noted that boys may experience some unilateral or bilateral breast growth at puberty but this usually resolves in a year.
The breast changes from the immature form of tubular type acini under the dominant influence of estrogen to bunches of grape shaped acini or alveoli in the mature and functional breast under the associated influence of progesterone. The changes in morphology of the glandular tissue of the breast is much like the changes of morphology of a tree – say a cherry tree – undergoes as it progresses through the seasons. The tubular form is like the tree in winter ? bare tubular branches devoid of leaves and flowers. The tree in full flower is in the spring of its life with florid proliferation of its blossoms. In between these two extremes are the cyclical changes of summer and fall. Full materialization of the mature breast occurs with lactation when there is florid proliferation of the acini totally filling the lobules.
Cycles
Cyclical changes with the menstrual cycle coincide with cyclical changes of estrogen and progesterone. There are two phases in the cycle. The first phase is called the proliferative phase and is controlled by estrogen, and the second phase is called the secretory phase and is governed by progesterone. In the proliferative phase of the cycle following the menses, estrogen progressively increases in concentration causing progressive ductal proliferation. Following ovulation the secretory phase is initiated, with progressive increase in the level of progesterone. Progesterone not only causes a relative proliferation of the lobular tissues, but also the accumulation of water in the stromal tissues. The histological changes have been studied and reported by Longacre in a very important autopsy series. This gearing up of the tissues for a potential pregnancy in the secretory phase, creates fullness and sometimes tenderness in the breasts. On examination of the breasts at this stage, the texture of the breast coarsens becoming more ?lumpy? corresponding to the proliferation occurring in the lobules. Tenderness discomfort and lumpiness of the breast disappear a week after menstruation.
In summary and simply stated, estrogen is responsible for ductal development, progesterone for ductules, acini and stroma, prolactin for secretory apparatus, and oxytocin for myoepithelial contraction. During pregnancy the presence of estrogen and progesterone inhibit lactation. In the postpartum period the levels of these two hormones drop, allowing prolactin to initiate milk production.
Pregnancy Lactation
During pregnancy the high levels of estrogen and progesterone cause proliferation of the ducts and lobules resulting in an average volume increase of about 145ccs. With lactation the volume increases a further so that the breasts almost double in volume
Milk production is present in the latter half of pregnancy, but real lactogenesis starts at about 40 hours after birth and is completed at five days. Milk is generally only secreted and available 1-3 days after birth under the stimulation of sucking.
Colostrum is first secretion of the breast after delivery containing more protein and less fat than subsequent milk and contains antibodies that impart some passive immunity. As the levels of estrogen and progesterone drop, following expulsion of the placenta, the inhibition to lactation is lost and milk production is initiated. Sustaining levels of production take about 1-3 days. The physical stimulation of suckling causes the release of oxytocin and stimulates prolactin secretion stimulating more milk production.
Aging
With aging the glandular elements involute and Cooper?s ligaments loosen so that the breasts lose their shape and their support. In postmenopausal women, since the breasts consist mostly of fat, small weight changes are reflected in the size of the breast. This change does not occur in women who are not taking estrogen supplementation. Weight becomes a significant factor in the size and appearance of the breasts. Being mostly composed of fat at this point, small changes in body weight can produce significant changes in breast size.
Conclusion
Although the breasts have a relatively simple structural makeup they are organs that are continually changing under the fluctuating levels of hormones, day-by-day, and month-by-month. They lie dormant for about 11 years after birth, mature in about 4 years, and then they are in continued cycles of preparation for lactation, a relatively brief but glorious period of their existence when they are in full bloom and function. The functional unit is called the terminal ductal lobular unit, TDLU, which is surrounded by stromal tissues. Understanding of these two entities allows understanding of the physiological and pathological processes that affect the breast.