and Barry Giglio, M.D.
Barry Giglio, M.D. is currently employed as a Family Physician at a hospital owned practice in Concord, NH. He graduated from George Washington University.
Learning Objectives
-
-
- Describe the cause of the neck pain.
- Discuss the anatomy, physiology and pathophysiology of the cervical spine.
- Discuss the characteristic clinical presentations of neck pain.
- Recognize the usual diagnostic algorithm and procedures that are performed.
- Explain the general approach to the management.
-
Introduction
Neck pain is a common complaint seen in various medical settings including primary care and the emergency department.
It has many causes including dysfunction of the muscles and supporting structures such as bones and their joints (musculoskeletal dysfunction), infection, neurological disorders, pain from somewhere else in the body (referred pain, as in headaches or heart attack), and disorders of the various other structures in the neck including the esophagus and thyroid.
Cause: Most neck pain is related to musculoskeletal dysfunction. In the U.S., almost 85% of all neck pain is thought to result from neck injuries (either acute or recurring) or from chronic stresses such as prolonged computer use. In the general population, the 1-year prevalence rate for neck and shoulder pain is 16-18% (Dreyer, 1998) and about two thirds of people will experience neck pain at some time in their lives.
Note: Some of the images in this activity are displayed backwards. We acknowledge the display does not follow standard protocols. The images are backwards to accommodate the author?s notations and markings.

Many Structures can Contribute to Pain – Most are Musculoskeletal in Origin
Courtesy of: Ashley Davidoff, M.D.
Principles
In this section we summarize the principles involved in structural derangements. Many disorders result from structural changes which include a change in size, shape, position or character of the structures or parts of the structures. In the case of neck disease, the pain often results from impingement on nerve roots by displaced disc or from degenerative joint disease associated with proliferative osteophytes. Sometimes the primary derangement and pain may result from functional disorders. Muscle spasm is a frequent cause of neck pain. Aside from degenerative change, other less common causes of neck pain include inflammation, infection and neoplastic disorders.
Applied Anatomy
The neck is comprised of 7 vertebral bones, connected to each other by facet joints. Between the vertebral bodies are gelatinous cushions (nucleus pulposus) known as vertebral discs, which are surrounded by fibrous rings known as the annulus fibrosis. The joints between the vertebrae normally allow for a considerable amount of movement including rotation, lateral bending, flexion and extension while providing critical protection for the cervical spine and nerves.
Normal Anatomy
Courtesy of: Ashley Davidoff, M.D.
Normal Anatomy
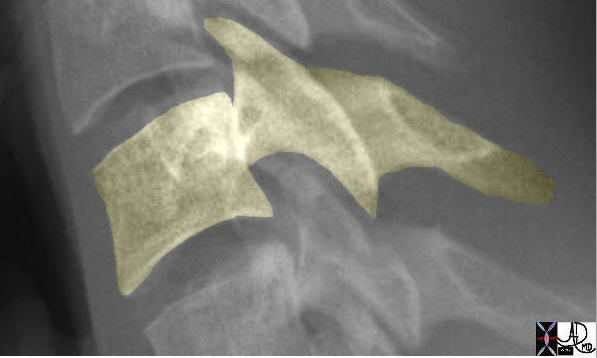
The vertebral bodies are connected to each other through intervertebral discs and facet joints, and are also held together by ligaments and muscles.
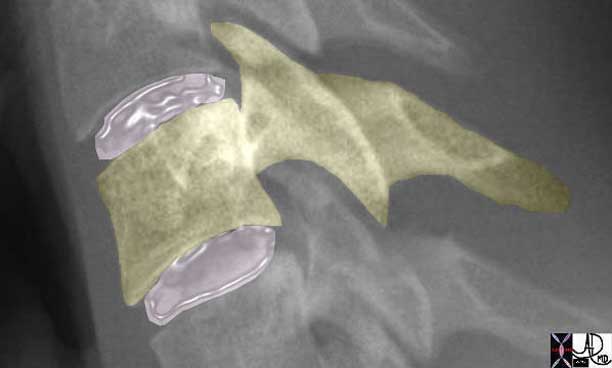
The pink intervertebral discs act like gelatinous shock absorbers or cushions between two vertebra and consist of a central nucleus pulposus surrounded by the annulus fibrosis.
Courtesy of: Ashley Davidoff, M.D.
Each vertebra has a pair of facet joints situated posterior to the vertebral body and on either side of the vertebra. Each side has both a superior and inferior component. Thus at the back of the vertebra there are 4 facet joints that contain both cartilage and a synovial lining. The joints are almost vertically oriented providing both strength and rotational ability.
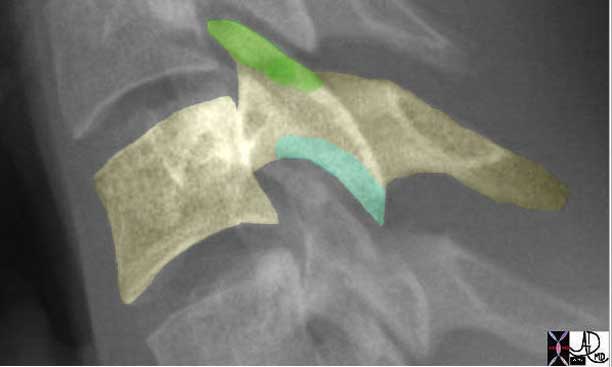
There is an almost vertical joint space between the vertebral body above and the one below. Each vertebra has a pair of superior facets (green) and a pair of inferior facets (teal) each of which form a cartilage lined synovial joint with the vertebra above and below. The design of the joint provides structure that allows for stability and rotational capability.
Courtesy of: Ashley Davidoff, M.D.
Ligaments
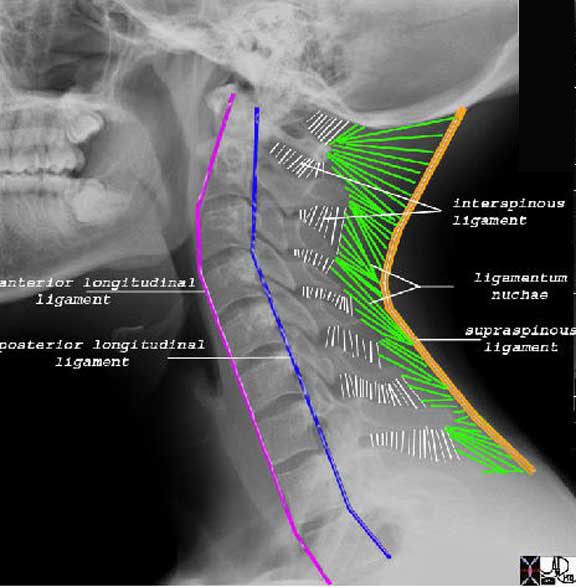
There are 5 major groups of ligament. The anterior longitudinal ligament (pink) runs along the anterior aspect of the spine, while the posterior longitudinal ligament runs along the posterior border of the vertebral bodies. (blue) The interspinous ligaments run between the spinous processes (white) while the ligamentum nuchae or nuchal ligaments (green) connect the bones and interspinous ligament and bony spinous processes to the supraspinous ligament (orange) which runs along the spinous processes in a vertical fashion.
Courtesy of: Ashley Davidoff, M.D.
Applied Anatomy: Vertebra
The first cervical vertebra, also called the atlas, is a ring shaped bone, which articulates with the occiput of the skull. This allows for about 1/3 of the flexion/extension and ½ of the lateral bending of the neck. The second vertebra, also called the axis, contains a bony prominence known as the dens or odontoid process. The dens prevent horizontal displacement of the atlas. The articulations between the first and second cervical vertebrae account for about ½ of the rotation of the neck.
The other cervical vertebra are considered independent building blocks that are connected to other vertebra above and below. Caudally, the seventh cervical vertebra is connected to the thoracic spine. In the larger sense, the cervical spine connects with the thoracic and lumbar spine to form a flexible supportive rod called the axial skeleton. The function of the cervical spine is to protect the spinal cord as it exits from the brain and enable mobility of the head. Controlled and rapid movement of the head is essential for survival. The ability to quickly turn the head in the face of danger that is seen or heard for example, requires rapidity of muscle contraction, as well as mobility and strength. These survival mechanisms are enabled by the simple, yet elegant, design of the unique first and second cervical vertebra.
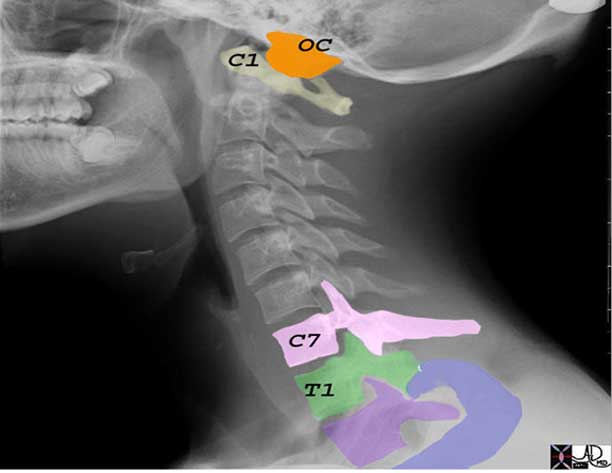
The cervical spine is connected to the skull through the atlanto occipital joint. The occipital condyle (OC orange) articulates with the lateral masses of C1 (also know as the atlas). At its caudal end the cervical spine articulates with the thoracic spine through the C7-T1 articulation which is similar in makeup as the other inter-cervical articulations.
Courtesy of: Ashley Davidoff, M.D.
Applied Anatomy: Muscles
There are many muscles in the neck that are essential for the support and movement of the head and neck. There are muscles connecting the skull and mandible to the neck, and in turn there are muscles that connect the neck and skull to the thorax and shoulders. Muscle spasm is an important cause of neck pain. In addition to the many muscles, there are other structures and organs that include ligaments, joints, bone, nerves, thyroid, trachea and esophagus that can be the source of neck pain.
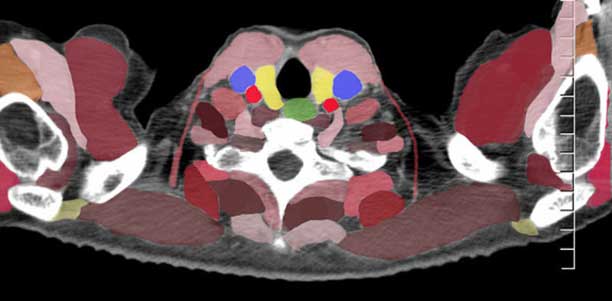
The axial image is overlaid revealing all the many structures that can contribute to neck pain. Most are musculoskeletal. There are numerable muscles connecting the neck to the skull and mandible, and muscles connecting the neck to the back, the chest and to the shoulders. The reds and maroons all represent muscles, except for the bright red carotid arteries that lie posterior to the internal jugular veins (blue). The central black structure is the trachea, and it is surrounded by the thyroid lobes (yellow). Behind the trachea is the esophagus (green). There are other parts and organs that include ligaments, joints, bone, nerves, thyroid, trachea and esophagus that can also be the source of neck pain.
Courtesy of: Ashley Davidoff, M.D.
Applied Anatomy: Neural Canal
When the relatively small space of the neural foramen is considered in conjunction with its intimate relationship with the posterior aspects of the intervertebral disc and space, and relationship to the facet joints, it is no wonder that a small space occupying event (disc protrusion, herniation or osteophyte presence) could result in a significant clinical event. The clinical event may be acute or chronic.

The oblique projection of the plain film of the cervical spine exposes the neural foramen with its pair of nerves (yellow). The second image which is also normal shows the intimate relationship to the intervertebral disc space and the facet joints.
Courtesy of: Ashley Davidoff, M.D.
Applied Anatomy: Nerve Root Deficits
Arising from each level of the cervical spine are the cervical nerve roots, which travel through the neural foramen at the level above the respective vertebrae. There are eight cervical nerve roots to the seven vertebrae, so that the eighth cervical root passes through the intervertebral foramen between C7 and T1 vertebrae.
Nerve root deficits can be localized to the level of the lesion:
C3: typically causes pain in the back of the neck to the pinnae and angle of the jaw. On exam, typically there are no reflex changes.
C4: typically causes pain into the back of the neck to the levator scapulae to the anterior chest. On exam, there are no reflex changes. Motor function is related to spontaneous breathing, and sensory function involves the back of the neck.
C5: Pain into the side of the neck to the superior lateral shoulder, numbness over the deltoid muscle. On exam, there typically is deltoid muscle atrophy and weakness of shoulder abduction and of shoulder shrugging.
C6: Pain to the lateral aspects of the arm and forearm and into the thumb and index finger, with numbness of thumb and dorsum of hand. On exam, weak biceps (elbow flexion) and brachioradial (wrist extension) muscles and decreased biceps and brachio-radial tendon reflexes are found.
C7: Pain into the mid forearm to middle and ring fingers. On exam, triceps muscle weakness (elbow extension) and wrist flexion with a decreased triceps muscle reflex is found.
C8: Pain to the medial aspect of the forearm into the ring and small fingers, with numbness of the ulnar border and small finger. Typically on exam, triceps weakness with weakness of intrinsic muscles of the hand is found.
Injuries involving the nerve roots above C5 can cause respiratory paralysis, which of course is life threatening. (?C3, 4, 5 keep the diaphragm alive?.)

Space Occupation – The degenerative process results in two structural deformities that can cause neck pain by impinging on the nerves. The first image shows a posterior slippage of the disc from its normal position with pressure effect on the nerve. The second image shows proliferative osteophytes (white nodules) extending from the intervertebral disc space and impinging on the nerve, while the third image shows osteophytes from the facet joints impinging on the nerve.
Courtesy of: Ashley Davidoff, M.D.
Causes and Predisposing Factors
Risk factors associated with neck pain include heavy lifting, smoking, diving, and working with vibrating heavy equipment. Prevalence is generally highest in middle age. However, sports injuries are more common in younger people and malignancy is a more important consideration in those over the age of 50 and in those with a previous history of cancer. Trauma generally is more commonly seen in young males. Patients with osteoporosis, most commonly associated with older females, are at increased risk of fractures to the c-spine. Patients with Down?s syndrome and those with rheumatoid arthritis are at particular risk for atlantoaxial instability/subluxation.
Most uncomplicated neck pain is associated with poor posture, anxiety and depression, neck strain, occupational injuries, or sporting injuries. With chronic pain, mechanical and degenerative factors are more likely. Some neck pain results from soft tissue trauma, most typically seen in whiplash injuries. Rarely, inflammatory, infective, or malignant conditions can affect the cervical spine and present as neck pain with or without neurological features.
Neck pain can manifest with pain in the neck itself (axial pain) or in the extremities (radiculopathy or neurological deficit). Axial pain can be caused from disorders of the bones, joints, ligaments, or muscles of the neck. Neurological deficits involve either conditions which impinge on the spinal cord (myelopathy) or the nerve roots (radiculopathy). Myelopathy can result in upper motor neuron dysfunction associated with weakness, poor coordination, sexual dysfunction, gait disturbance or bowel/bladder dysfunction. Radiculopathy can lead to muscle weakness, sensory deficits, reflex deficiencies, and pain in the patterns noted above.
Most uncomplicated neck pain is associated with poor posture, anxiety and depression, neck strain, occupational injuries. The wear and tear on the spine as people age is universal and nobody is spared. We walk, we stand, we lie down, we move, we jog we play sport – and at each turn we depend on the strength and integrity of the tissues. All the elements described above pull and push on the cervical spine and over the years degeneration is inevitable. With chronic pain, mechanical and degenerative factors are more likely.
Causes and Predisposing Factors: Additional Risk Factors
Additional risk factors associated with accelerated progression of degenerative change and neck pain include other occupational stresses that include heavy lifting, or the repetitive motion of working with vibrating heavy equipment. This can also sometimes lead to spinal stenosis, a narrowing of the nerve openings around the spinal cord or individual nerve roots, leading to symptoms similar to those in a herniated disc. Prevalence is generally highest in middle age.
Causes and Predisposing Factors: Other Causes
Less commonly, inflammatory, infective, or malignant conditions can affect the cervical spine and present as neck pain with or without neurological features. Malignancy is a more important consideration in those over the age of 50 and in those with a previous history of cancer.
Fibromyalgia is a poorly understood condition causing chronic pain in many areas of the body including the neck, frequently associated with many tender spots or ?trigger points,? fatigue, and multiple other physical complaints.
Non-Spinal Causes of Neck Pain and referred pain – Shoulder and elbow injuries, heart attacks, and gall bladder disease are examples of problems that can refer pain to the neck area. Thyroiditis, an inflammation of the thyroid and other thyroid disorders may cause pain in the neck.
Pathogenesis and Pathophysiology
The source of pain can be as simple an explanation as induced muscle spasm, but there can be more complex issues related, for example, to nerve endings in the facet joints which are innervated with C fibers and A-delta fibers both of which have been implicated in the sensory aspect of pain perception. They can be stimulated by inflammatory agents such as substance P and phospholipase A. Other factors that create the sensation of pain have been thought to arise from the dorsal horn in the spinal cord which also are stimulated by substance P, gamma-aminobutyric acid (GABA) and N-methyl-D-aspartate (NMDA) in the spinal cord.
Muscle spasm is an important cause of the pain. It is a reflex response of the muscles to injury of the discs, ligaments, bones or muscle. The net effect functionally is that motion around the injured area is reduced and in effect protects the injured area. The pain that results is due to the accumulation of lactic acid that stimulates the pain fibers. The muscular spasm causes the occlusion of small arterioles that would otherwise deliver oxygen to the muscles and occludes the veins preventing removal of waste products. In effect, the pain is caused by ischemia and accumulation of lactic acid. Once the spasm is relieved, the vessels are opened, the lactic acid is removed and the pain is relieved.
Neck pain can manifest with pain in the neck itself (axial pain) or in the extremities (radiculopathy or neurological deficit). Axial pain can be caused from disorders of the bones, joints, ligaments, or muscles of the neck. Neurological deficits involve either conditions which impinge on the spinal cord (myelopathy) or the nerve roots (radiculopathy). Myelopathy can result in upper motor neuron dysfunction associated with weakness, poor coordination, sexual dysfunction, gait disturbance or bowel/bladder dysfunction. Radiculopathy can lead to muscle weakness, sensory deficits, reflex deficiencies, and pain in the patterns noted above in the applied anatomy section.
Clinical
Physical examination includes inspection and palpation of the neck and surrounding structures, range of motion evaluation of the neck (once it is certain there are no cervical spine fractures), and further neurological evaluation including testing of strength and sensation of the extremities.
Range of motion of the neck includes rotation (90 degrees), lateral bending (45 degrees) and flexion (60 degrees) /extension (75 degrees).
Neurological examination includes evaluating muscle strength, sensation, and reflexes. Strength of shoulder abduction, elbow flexion/extension, and wrist flexion/extension, along with flexion/extension of the lower extremities, should be assessed. Evaluation of sensation should include the neck, shoulders, arms, and hands/fingers. Reflexes tested should include the biceps, triceps, and brachioradialis tendons.
Along with this general examination, further evaluation may include provocative maneuvers such as:
-
- Spurling Test: This test uses cervical extension and lateral bending while the examiner applies a downward axial load, and may provoke radicular symptoms in a patient with cervical radiculopathy.
- Upper Extremity Tension Test (Elvey?s Upper Limb Tension Test): This test is a nerve root tension sign for the upper extremity. It involves turning the head to the contralateral side while abducting the arm and extending the elbow. This test is positive if the symptoms are reproduced. (Isaac and Anderson)
It is important to consider the underlying pathology when considering further evaluation such as lab studies and imaging. Some issues, such as trauma or infection, may require more immediate evaluation.
Serious trauma such as after a motor vehicle accident, diving accident, or other serious fall requires emergent evaluation after neck immobilization and transport to the emergency department. Evaluation in the emergency department involves careful neurological assessment and examination of the neck, followed by imaging. Assessment for palpable ?step offs? indicating possible cervical spine fractures and neurological deficits may provide information as to the level affected by the injury. There are multiple guidelines for C-spine assessment after trauma including the Canadian C-spine rule and Nexus Low Risk criteria. (Isaac and Anderson)
Labs
As the most common cause of neck pain is musculoskeletal, labs are frequently not indicated, but specific clinical scenarios may warrant further investigation:
Electromyography (EMG)/nerve conduction studies: are useful in isolating the location of a nerve lesion and therefore helpful in deciphering the etiology of a lesion. These studies are performed by measuring the electrical activity of various muscles through small solid needles. These needles can send small amounts of electrical stimuli into the nerves which can then help measure the function of these nerves. EMGs can be helpful in discerning whether a nerve lesion is related to a cervical spine issue versus a peripheral nerve issue such as nerve entrapment.
Thyroid studies: can help evaluate the functional status of the thyroid if a thyroid disorder is suspected clinically.
Lumbar puncture (LP)/spinal tap: if meningitis is suspected, a sample of cerebral spinal fluid (CSF) may be obtained by a spinal tap. CSF is a fluid that bathes the brain and the spinal cord. An LP involves inserting a needle into the space in the lower part of the spine (below the end of the spinal cord) and obtaining a sample of CSF. The CSF can then be evaluated for signs of infection including blood counts, chemistries, and cultures. It is frequently felt necessary to start antibiotics even prior to this procedure if there is a strong suspicion for bacterial meningitis.
Imaging: X-Ray
X-rays are urgently required following neck trauma before the cervical collar (used to stabilize the neck) is removed. At least three different x-ray views of the cervical spine are required to exclude a fracture. A lateral view must include all seven cervical vertebrae as well as the space between C7-T1 to assess for proper alignment. The most common reason for a missed cervical spine injury is a cervical spine radiographic series that is technically inadequate. (American Family Physician, 1999) Missing a fracture could potentially risk paralysis or death if not treated appropriately.
Imaging: Computed Tomography (CT)
Computerized Tomography (CT) is a medical imaging technique involving multiple 2-dimensional (2D) X-rays that are combined by a computer to form a three-dimensional (3D) image which appear as contiguous slices. CT scans are excellent for identifying fractures, but its ability to show ligamentous injuries is limited. Given their wide availability in the emergency room, CT is common used in trauma situations if there is any concern of a possible c-spine fracture.
Imaging: Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) is a medical imaging technique which uses high powered magnets that align the hydrogen atoms of the body, which are then disrupted by radio waves and are detected by the scanner, producing an image. This allows for better soft tissue contrast than is permitted by the X-rays used in CT scanning. MRI exams are especially helpful if there is concern for neurological compromise such as in disc disease. An MRI may also be helpful for evaluation of malignancy or infection.
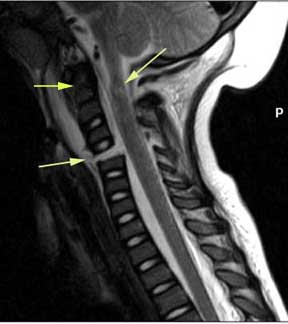
This MR image on a 2-year-old child shows an injury to the odontoid (left top arrow) with cord contusion (right arrow) and a complete C5 fracture (bottom left arrow).
Courtesy of: Philips Medical Systems
Management
Treatment of neck pain must address the underlying disorder. A brief review of the management of musculoskeletal neck pain is discussed here:
As a majority of neck pain is self limited, many symptoms can initially be managed conservatively with symptomatic management including NSAIDs and acetaminophen, muscle relaxants and possibly narcotic medications for more severe acute pain. NSAIDs include such medications as ibuprofen and naproxen sodium which act as analgesics and anti-inflammatories and can provide temporary relief of symptoms. Patients need to be monitored closely for GI bleeding and renal dysfunction. Muscle relaxants, such as cyclobenzaprine and metaxalone may be helpful if neck pain is associated with muscle spasm. Use of muscle relaxants may be limited by somnolence. Judicious use of narcotic analgesia can be considered, but their role in chronic pain is controversial due to such concerns as risk for abuse and dependence issues.
Sometimes, oral steroids (such as prednisone) are used for radiculopathy. These medications may raise blood sugars (especially concerning for a diabetic), decrease bone density, and affect mood and therefore should be used sparingly.
Cervical collars may prolong recovery in musculoskeletal neck injuries and are generally not recommended.
There are many available treatment options for neck pain including physical therapy (mobilization), chiropractic (high velocity) manipulation, and surgery. There are limited evidence based studies providing guidelines about effective treatments.
There is some evidence to support the use of both manipulation and mobilization at least to relieve neck pain short term. Such physical therapy modalities as ultrasound and transcutaneous electrical nerve stimulation (TENS) do not have evidence supporting their effectiveness. No clinical review has shown acupuncture to be effective for neck pain and is not recommended. (Douglass)
For persistent or progressive neurological symptoms, fluoroscopically guided epidural steroid injections may be helpful.
Surgical intervention for cervical radiculopathy is reserved for patients with cervical disc herniation confirmed by imaging and radicular signs and symptoms that persist despite at least 6 to 12 weeks of conservative (non-surgical) therapy or progressive motor weakness. The optimal treatment of cervical radiculopathy remains unclear.
There are generally two surgical approaches but it is unclear whether there is a beneficial difference between the two. Which approach is taken may depend on the nature and location of the lesion being treated:
Anterior cervical discectomy and fusion is a procedure which removes disc herniations and osteophytes through the front of the neck. This approach appears to be emerging as the preference of many surgeons. This procedure?s advantages are that it involves less manipulation of the spinal cord and nerve roots; however, there is a small risk of damaging other neck structures including the carotid arteries, trachea, or esophagus. The other concern is that fusion might cause more wear and tear of the adjacent vertebral structures, as it has been shown that by limiting movement at one level leads to more movement at adjacent levels. Work is being done on artificial discs in order to minimize this effect. (Feiz-Erfan, et al.)
With posterior laminoforaminotomy, there is no alteration of the cervical spine structures (i.e. fusion) and less risk for the anterior neck structures but post operative recovery may be more difficult. The posterior approach does allow for treatment of centrally located lesions.
Treatment of the various other disorders which may cause neck pain (including heart attacks, cancer, and thyroid disorders) are beyond the scope of this article.
Potential Complications
Due to all of the important structures in the neck, many serious potential complications exist depending on the underlying pathology. With trauma such as a C-spine fracture, paralysis is a risk. With radiculopathy, permanent neurological compromise is possible. If meningitis or other infection of the neck is not treated in a timely fashion, death is possible.
Acute Neck Pain
Acute neck pain is a devastating and debilitating event. It may result from an aggravation of a longstanding process where the precipitating event was a minor trauma sufficient to cause a shift of tissues with significant clinical effects. (“The last straw that broke the camel’s back” effect) Patients with otherwise asymptomatic degenerative disease may fit into this category. Patients with osteoporosis, most commonly associated with older females, are at increased risk of fractures to the cervical spine. Patients with Down?s syndrome and those with rheumatoid arthritis are at particular risk for atlantoaxial instability/subluxation.
The precipitating event on the other hand could be a major traumatic event on an otherwise normal spine. The whiplash injury and sports injuries are examples. The neck pain results from soft tissue trauma, most typically seen in whiplash injuries. Soft tissue trauma implies injury to ligaments, tendons and muscles.
Sports injuries are a common cause of neck pain. They range from minor sprains and strains to severe irrecoverable changes and sometimes to death. Sports injuries are more common in younger people and more common in males.
Fractures
Fractures of the cervical vertebrae typically occur with trauma such as a motor vehicle accident, falls, or even sports injuries.
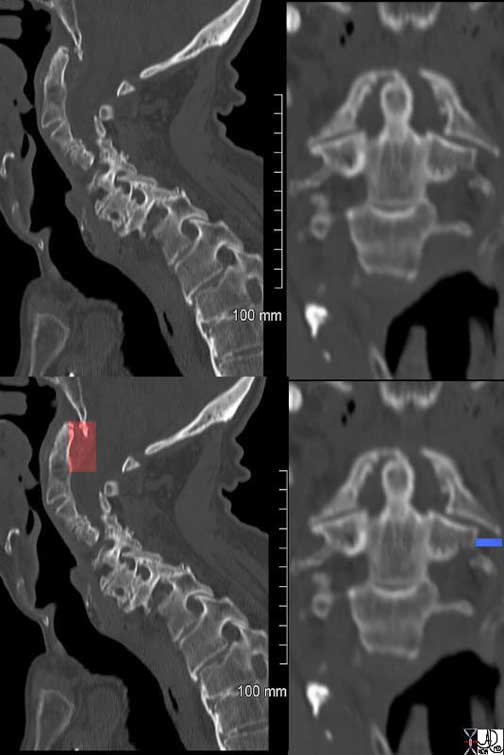
The case above is on an elderly man who presented to the ER with neck pain following trauma. The CT sagittal images on the left show anterior displacement of the odontoid peg in relation to the foramen magnum above associated with soft tissue swelling (red) posterior to the odontoid. In the coronal images (right) the left-sided lateral mass of C1 is displaced laterally off the vertebral body C2 (blue line).
Courtesy of: Ashley Davidoff, M.D.
Trauma : C1 Fractures
C1 Fractures (Jefferson Fractures): typically occur with axial loads, and present with neck pain and no neurological symptoms. There are two types: Posterior arch fractures and burst fractures. Burst fractures are more serious and involve disruption to the anterior and posterior arches and can lead to neurological and vascular compromise if not diagnosed and treated promptly. Often treatment involves bracing rather than surgery.
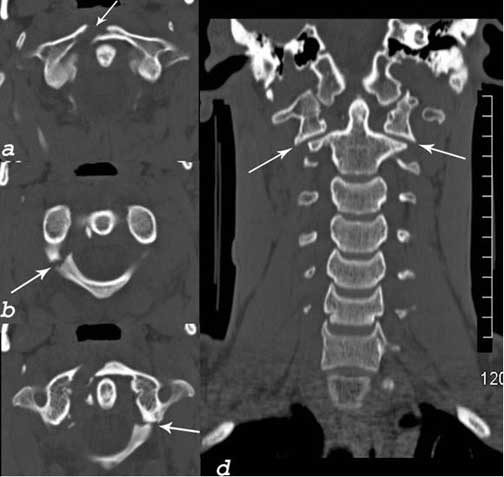
The CT scan is from of a young man who sustained a neck injury during a football game. The axial images show a fracture through the anterior arch of C1, (a), a fracture through the posterior arch on the right (b), and on the left (c). The coronal image (d) shows lateral displacement of C1 on the body of C2. This is a burst fracture of C1 and is also called a Jefferson fracture.
Courtesy of: Ashley Davidoff, M.D.
Trauma : C2 Fractures
C2 Fractures: Hangman fractures usually are caused by a hyperextension injury related to motor vehicle injuries or diving accidents. This involves bilateral pedicle fractures and can cause anterior displacement (subluxation) of C2 on C3, and resemble injuries previously sustained when people were executed by hanging. A second type of fracture involving C2 is an odontoid fracture, which is also usually treated without surgery.
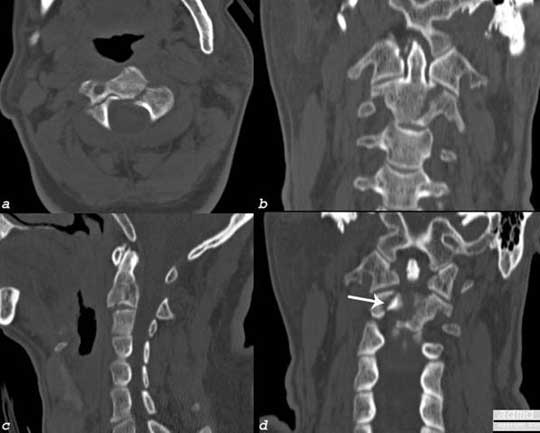
The CT shows a fracture through the body of C2 extending into the pedicles on the right and left side as well as extending into the C2-C3 interspace.
Image a: axial view showing extension of the fracture from the body into the lamina
Image b: coronal view showing fracture through the body on the left side
Image c: sagittal view showing fracture through the posterior body
Image d: posterior coronal view showing comminuted nature of the fracture
Courtesy of: Ashley Davidoff, M.D.
Trauma : Neck Sprain – Whiplash Injury
Whiplash is a traumatic injury to the neck caused usually by a decelerating motor vehicle accident, resulting in neck pain. It is also called a neck sprain and is most commonly related to soft tissue injury. This typically involves the acceleration/deceleration injury related to a side or rear impact motor vehicle accident. It is characterized by acute and sometimes chronic pain, sometimes associated with prolonged morbidity compared to other sources of neck pain. The precise etiology of whiplash is unclear and the subjective complaints often are more severe than objective findings. The diagnosis is suspected given the appropriate mechanism of injury and confirmed by less significant objective findings. Imaging may involve plain X-rays. Typically, CT scanning or MRI is not indicated unless there is concern about other neck pain etiologies i.e. those showing neurological involvement (which is not typical of whiplash injuries).
Neck Sprain – Whiplash Injury: Structural Principles
This poorly defined group of conditions seems to involve the complex interplay of the multiple components of the neck including articulations, ligaments, and muscles. Injury to bone, intervertebral disks facet joints, nerves (including root and spinal cord), and soft tissues of the cervical spine (ligaments, tendons, muscles) are the most likely sources of dysfunction and pain. Cervical strain is produced by an excessive force on the muscle-tendon unit, or the muscle periosteum unit. Muscle spasm is often the cause of acute pain.


Courtesy of: Ashley Davidoff, M.D.
Many muscles of the cervical spine are attached to the periosteum directly rather than via a tendon or ligament and the shearing stress on the periosteum may also contribute to the pain. The facet joints and ligaments have also been shown to contain free nerve endings that when injured may result in chronic pain.

Courtesy of: Ashley Davidoff, M.D.
Neck Sprain – Whiplash Injury: Structural Principles Continued
The presence of edema, hemorrhage, and inflammation have also been thought to contribute to the pain.

Prevertebral edema (pink) can be a source of chronic pain and may result from edema or hemorrhage.
Courtesy of Ashley Davidoff, M.D.
The pathophysiology of the pain and discomfort is poorly understood since no distinct structural changes can be identified.
Clinically, the severity of the symptoms often do not correlate with the severity of the injury. So, mild injury may be associated with severe symptoms. Whiplash can commonly cause chronic ill-defined neck pain, sometimes also pain in the shoulders and arms. Although the most common symptom is neck pain there may be a variety of multiple symptoms associated with whiplash, many of which are non-specific. Non-specific symptoms include fatigue, tinnitus, dizziness, and visual symptoms. These symptoms are sometimes associated with a complex psychosocial situation, and patients may suffer mentally as well as physically. Whiplash pain typically resolves within 6 months of the initial injury. Sometimes though, whiplash can lead to chronic pain, which potentially could progress to drug dependency, depression, relationship issues, and social isolation.
The diagnosis is recognized by the clinical setting of pain and discomfort in the presence of a decelerating injury.
Following trauma, more serious sources of traumatic neck pain need to be excluded including fracture, dislocation, and injury to the neurological components of the neck.
Plain X-rays may show previous degenerative changes and/or loss of the usual curvature of the cervical spine (lordosis). It is important in the acute setting to ensure that no bony injury is present and a CT of the c-spine may be helpful if pain persists in the presence of a negative plain film.
There are few studies which have looked at whiplash management in an evidence-based fashion. It does appear that early active physical intervention rather than passive treatment (such as cervical collars) is preferable
The prognosis is generally good for whiplash, but the rate of chronic pain is higher with whiplash than with other neck pain conditions. It is reported that up to 40% of whiplash sufferers are plagued with chronic pain for years after injury, for unclear reasons. (Binder, 2001)
Trauma : Burners/Stingers
This injury relates specifically to a more shearing the pain is more stinging in nature and is thought to be caused when the nerves in the neck are stretched, typically when force is applied to the shoulder when the head is forced in the opposite direction. This is a common football injury which is typically self limited.
Trauma : Herniated Cervical Disc
Acute cervical spine injury has also been associated with disc herniation and can be precipitated by sports injuries in team sports such as football, rugby, and ice hockey, or in individual sports such as gymnastics and diving. When the disc is degenerated due to wear and tear lesser forces could result in the same clinical scenario. The clinical presentation ranges from neck pain or radicular pain, to quadriparesis, or quadriplegia.
When the annulus ruptures the inner nucleus pulposus may herniate anteriorly, posteriorly or internally. If the disc ruptures posteriorly it may impinge on the spinal cord or the exiting nerves.
Clinical Presentation
There are two distinct scenarios. The young athlete who has sustained an excessive axial load to the spine and the patient who is usually older than 30 years whose disc has been subject to wear and tear and who may have sustained a relatively minor injury. In the elderly population the overall volume and turgor is significantly reduced so that herniation of a sufficient amount of material with sufficient force becomes less likely.
The clinical features of herniated disc include segmental neck pain, muscle spasm, loss of range-of-motion (ROM). Nerve root involvement leads to radicular upper extremity pain, weakness, and sensory changes. Pain symptoms may be aggravated by strains induced by motion, lifting, or by Valsalva maneuvers.
Herniated Cervical Disc: Diagnosis
The important clinical difference between the young athlete with a forceful injury and the older patient with a lesser precipitating force, is to exclude unstable associated bony injury. Plain film or CT scan should be performed in the former. When disc herniation is suspected then an MRI is the study of choice to visualize the disc. The nature and and the position of the disc can be best characterized by MRI. For the patients who cannot undergo MRI, a myelogram is utilized.

There is a subtle but definite deformity of the thecal sac seen in this T2 weighted left parasagittal view of the spine. This represents an acute disc herniation following acute trauma in a young man following trauma with left sided pain and paresthesia.
Courtesy of: Ashley Davidoff, M.D.
Return to play is an important but controversial issue following successful treatment of cervical Vertebral discs are fibrous shock absorbing cushions (donut like structures with a central gel) between the vertebral bones of the spine. Sometimes these discs can become disrupted, with the central gel leaking out into the surrounding structures. This can cause pain locally or apply pressure to the spinal cord or nerves (pinched nerve/radiculopathy), affecting the areas supplied by those nerves. The pain is described either as an aching or an electrical feeling down the arm, sometimes into the hands.

The oblique projection of the plain film of the cervical spine exposes the neural foramen with its pair of nerves (yellow). The image reveals impingement of the nerve by the posterior displacement of the disc.
Courtesy of: Ashley Davidoff, M.D.
Meningitis
Meningitis is a potentially life-threatening infection or inflammation of the meninges of the brain caused by viruses, bacteria, drugs and sometimes by metastases clinically resulting in headache, neck pain, nuchal rigidity, fever, and mental status changes.
The diagnosis is best made by evaluation of the CSF with attention to the presence of leukocytes, red cells, or bacteria, and or abnormal levels of sugar and protein.
Early administration of antibiotics is an essential part of the treatment when meningitis is suspected since it is a life threatening disease. Viral meningitis is treated with supportive care.
Chronic Neck Pain
Most uncomplicated neck pain is associated with poor posture, anxiety and depression, neck strain and occupational injuries. The wear and tear on the spine as people age is universal and nobody is spared. We walk, we stand, we lie down, we move, we jog we play sports – and at each turn we depend on the strength and integrity of the tissues. All the elements described above pull and push on the cervical spine and over the years, degeneration is inevitable. With chronic pain, mechanical and degenerative factors are more likely.
Degenerative Cervical Arthritis
Degenerative cervical arthritis is an age related arthritis caused by wear and tear on the cervical spine with secondary changes in the intervertebral disc, surrounding vertebral bodies and or the facets. Protruding or herniating disc material, or proliferative bony changes are the usual result of degeneration all or any of which may impinge on the exiting nerves resulting in pain, paresthesias, sensory and or motor loss. The space occupation of the spinal canal may be aggravated by hypertrophy of ligament and spinal stenosis is a complication of the disease.
Age, injury and poor posture play a role in the development of the disease. Nearly everyone over the age of 50 will experience some wear and tear in the spine, but not everyone develops cervical arthritis. People usually develop symptoms of cervical arthritis when they are between 40 and 50 years of age. Men are more likely than women to develop this type of arthritis. However, postmenopausal women have a higher incidence of this disease.

Disc Degeneration and Osteophytes – The first image is normal showing normal bony character, normal height of the intervertebral disc spaces and no evidence of space occupying osteophytes.
In the second image of the older patient the image is remarkably different. Osteophytes have developed as a response to distresses on the bony components as a result of degeneration of the tissues. The osteophytes buttress the bones so that support can be maintained in the face of the degeneration. They can be seen as beak shaped excrescences anterior to the vertebral bodies as well as posteriorly. They also can occur along the edges of the facet joints.
Courtesy of: Ashley Davidoff, M.D.
Rheumatoid Arthritis
Rheumatoid Arthritis (RA) is an autoimmune inflammatory disease involving the destruction of synovial joints. In the neck, it is characterized by cervical joint destruction which may lead to misalignment of the vertebrae. The cause of rheumatoid arthritis is unknown, but an infectious process leading to activation of the immune system has been theorized. There is a genetic predisposition to the disease.
The major end result of rheumatoid arthritis in the cervical spine is C1-C2 instability.
The diagnosis is suspected clinically when a patient with known RA complains of neck pain, or neurological deficit. Imaging includes plain radiographs which may show alteration of the relationships of skull base, C1and C2. CT scanning and MRI may reveal more precisely the effect of soft tissue and bony changes on the cord.
Treatment typically involves those medications involved in the treatment of RA known as DMARDs (disease modifying antirheumatic drugs) but also may involve surgery to stabilize the C1-C2 relationship.
Rheumatoid arthritis involving the cervical spine affects about 50% of patients with rheumatoid arthritis. It is characterized by vertebral joint destruction which can lead to neck instability leading to neck pain, C2 radicular pain, and myelopathy. Neurological manifestations/deficits including those of cord compression and even death can occur. (Harris)
Cause and Predisposing Factors:
The exact cause of RA is elusive, but infectious and predisposing genetic factors are theorized. There have been some genetic subtypes identified, and an identical twin has a higher risk of developing RA if their twin has it.

The classical features with severe arthritis, involving the proximal interphalangeal joints and the carpal joints with resulting ulnar deviation and severe osteopenia are characteristic features of rheumatoid arthritis. Neck pain in a patient with this entity requires an alertness of associated involvement of the cervical spine and the most serious involvement is related to the C1-C2 joint.
Courtesy of: Ashley Davidoff, M.D.
Osteoarthritis: Diagnosis
The diagnosis requires a careful and meticulous clinical evaluation with particular attention to sensory and motor loss. A plain film of the cervical spine may show severe degenerative disease but may not necessarily reflect severe disease. On the other hand, a normal plain film may suggest normal bony abnormality but severe disease as a result of soft tissue changes may be present. It is usual that bony detail of the degenerating spine is best evaluated by CT scan, while soft tissue changes including disc disease is best evaluated by MRI. For those patients who cannot undergo a conventional MRI, CT myelography study is indicated.
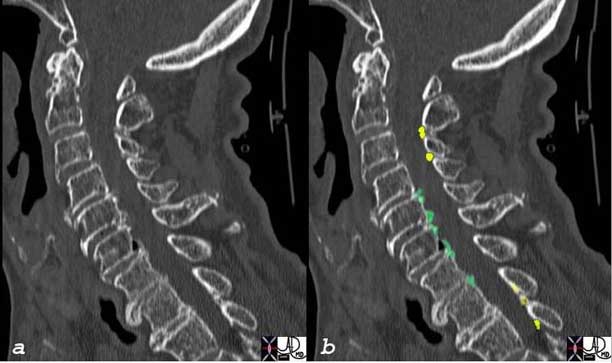
The sagittally reformatted CT scan shows posterior osteophytes (green) impinging on the thecal sac, and small facet joint osteophytes protruding anteriorly. (yellow) If these impinge on the nerves they will cause of symptoms. The anterior osteophytes off the vertebral bodies impinge on the air filled esophagus and can occasionally be the cause of dysphagia.
Courtesy of: Ashley Davidoff, M.D.
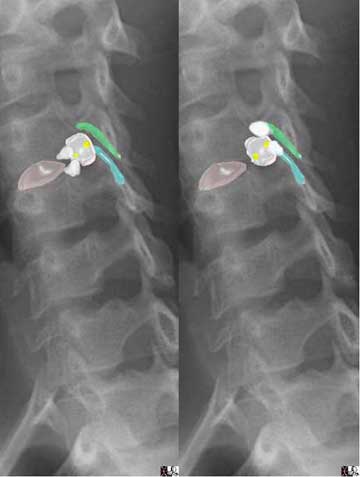
The plain oblique films are overlaid with theoretical osteophytes (white) and their relative position to exiting nerves. In the case on the left the osteophytes (white) are positioned off the posterior edge of the vertebral bodies and in the case on the right the osteophytes (white) are positioned off the anterior edge of the facet joints.
Courtesy of: Ashley Davidoff, M.D.
In the cases where acute or chronic disease or chronic pain are the issues then conservative treatments including rest, exercise, and improvement of posture are first steps. Sometimes the type of pillow the patient uses creates stresses on the neck leading to neck pain and finding the right pillow may be a small but important contribution in the management. Gentle neck exercises as directed by a professional may also help. Other helpful conservative measures include massage therapy, cold compressors, ultrasound and hydrotherapy.
Non-steroidal anti-inflammatory medications (NSAIDs) such as aspirin, acetaminophen or ibuprofen will be helpful in reducing swelling and reduce pain. Muscle relaxants may be helpful when spasm is considered to be a major cause of the pain. Directed steroid injections using fluoroscopy or CT guidance into the epidural at the site of the pain is sometimes used in patients with severe acute pain.
Failure of conservative measures or the presence of neurological deficit are usual indications for surgery.
Rheumatoid Arthritis: Structural Principles
Like other joints in the body, the joints of the cervical vertebrae may be affected by the destruction caused by the inflammation involved with RA. Most importantly, RA may involve the c-spine at critical sites such as the odontoid process and the articulations involving C1 to the skull and to C2. The destruction of these critical sites can lead to serious complications such as paralysis and death.
The structural derangement is as a result of loss of articular cartilage, ligamentous destruction, and bone erosion. Thus the transverse ligament that stabilizes the odontoid process with the anterior arch of C1 becomes lax and enables mobility of the odontoid that can potentially intrude onto the cord. Periodontoid pannus may also result in mass effect on the cord.
Physiological Principles:
The health of joints involves the interplay of many different components including the maintenance of bones and cartilage. These in turn rely on a supply of nutrients from the surrounding vasculature. When inflammatory destruction affects the joints they cannot retain opti mobility and stability.
Pathophysiology and Pathogenesis:
Rheumatoid arthritis involves joint destruction secondary to the overgrowth of synovial macrophages and fibroblasts. This leads to invasion of the joint by lymphocytes and the abnormal growth of blood vessels into the joint. These blood vessels then occlude and lead to the formation of a pannus, which is a collection of irregular growth of joint tissue. This overgrowth destroys bone and cartilage.
Result:
Destruction of the bone and cartilage leads to destruction of the joint involved and resultant joint dysfunction and pain.
Potential Complications:
Depending on the joint involved, multiple complications can develop. Most concerning regarding RA and the cervical spine is atlantoaxial instability. This can lead to neurological compromise when the supporting structures of the neck impinge upon the neurological components.
Diagnosis is usually suspected when a patient with known RA complains of neck pain and/or progressive neurological symptoms such as weakness.
Clinical:
In cervical subluxation, there can be numbness in the extremities or even a progressive spastic paralysis. Physical findings can include a loss of the natural cervical spine curvature and resistance to passive flexion of the neck. Weakness of the extremities can also be found.
Differential Diagnosis:
There are multiple forms of arthritis and rheumatologic disorders which need to be considered prior to the diagnosis of RA and they can all share some elements of similar presentation. These include but are not limited to: osteoarthritis, fibromyalgia, Lupus, mixed connective tissue disease, gout and infection.
Lab Tests:
There is no single definitive laboratory test to diagnose RA, but several tests are helpful in the evaluation. These include a complete blood count, metabolic panel, rheumatoid factor, and ESR (erythrocyte sedimentation rate) or CRP (C-reactive protein) measurement. The rheumatoid factor is known to be susceptible to false negatives as well as false positives.
Imaging:
Imaging of the c-spine by plain film, CT and or MRI show joint destruction and other characteristic joint changes and patterns. Sometimes, evaluation of the synovial fluid by joint aspiration can be helpful. The findings on plain film or CT scan may include:
-
-
- atlantoaxial subluxation, (space between the odontoid and anterior arch of C1 that is greater than 3mm is abnormal)
- cranial settling, and
- subaxial cervical subluxation.
-
Treatment and Management:
Joint destruction occurs early in the course of disease onset and ideally can be reduced by early treatment. This typically involves one or more DMARDs, which typically act on affecting immune function. These agents include methotrexate, sulfasalazine, Imuran, and multiple other agents. NSAIDs and glucocorticoids are also frequently used. Early treatment of RA may help avoid such complications as neck involvement. The goal of treatment is to minimize destruction of joints, manage pain, and maintain function as much as possible.
Prognosis:
Rheumatoid arthritis is typically a lifelong disease. It has varying severities, and those with early severe disease with multiple joint involvement tend to have a worse prognosis.
Rheumatoid Arthritis is a significant inflammatory arthropathy which can involve the neck leading to serious consequences such as atlantoaxial subluxation. In evaluating a patient with known RA for neck pain, this serious complication should be evaluated early. With early treatment, this complication can hopefully be avoided.
Ankylosing Spondylitis
Ankylosing spondylitis is a chronic inherited systemic inflammatory disease characterized by progressive ascending spondylitis, associated with systemic inflammatory manifestations.
The causative gene seems to be a genetic predisposition identified as HLA- B27 gene.
The resulting inflammatory changes starts with a sacroiliitis with progressive ascending pain and stiffness in the back starting in the lumbar region and progressively involving the thoracic and finally the cervical spine.
Associated diseases include arthritis of other joints, as well as other organs, such as the eyes, heart, lungs, and kidneys. It has similar features with other spondyloarthropathies, including psoriatic arthritis, as well as the arthritis associated with Crohn’s disease and ulcerative colitis.
Courtesy of: Ashley Davidoff, M.D

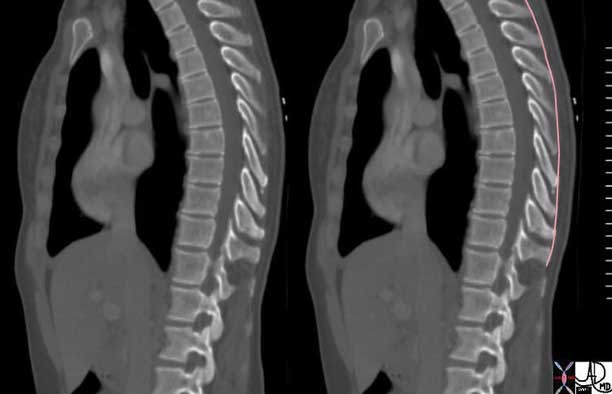
Shown are CT scans demonstrating a normal thoracic spine (top image) and an abnormal on a patient with a severe kyphosis and ankylosing spondylitis (bottom image).
Courtesy of: Ashley Davidoff, M.D.
Neoplasm/Cancer
In the appropriate clinical setting metastatic disease to the spine should always be considered in the patient with neck pain and a known cancer. This is particularly true when a patient with breast cancer, lung cancer or prostate cancer presents with neck pain. The site of metastasis is commonly the pedicle. While most metastases are of a lytic nature, breast and prostate cancer may be blastic.

In this elderly man who presents with neck pain, a blastic mass (green) represents a metastasis from prostate cancer.
Courtesy of: Ashley Davidoff, M.D.

The patient on the left is normal and the patient on the right is an elderly lady with blastic (dominant) and lytic metastases to both the thoracic and cervical spine from breast carcinoma. The kyphosis that is present in the patient on the right is age related due to osteopenia.
Courtesy of: Ashley Davidoff, M.D.
Fibromyalgia
Fibromyalgia is a poorly understood condition causing chronic pain in many areas of the body including the neck, frequently associated with many tender spots or ?trigger points,? fatigue, and multiple other physical complaints.
Non-Spinal Causes of Neck Pain and Referred Pain
Shoulder and elbow injuries, heart attacks, and gall bladder disease are examples of problems that can refer pain to the neck area. Thyroiditis, an inflammation of the thyroid and other thyroid disorders may cause pain in the neck.
Red Flags
There are several important factors not to miss when evaluating a patient with neck pain:
1. Fevers are suggestive of infection and warrant prompt investigation.
2. Age > 50 with new onset neck pain, or a history of cancer should raise concern for malignancy.
3. Night time pain, awaking patient from sleep may suggest more serious underlying pathology.
4. Trauma to the neck should be evaluated emergently.
5. Neurological symptoms, such as arm/hand weakness, which persist greater than 6 weeks.
Patient Information
Neck pain is an extremely common condition which affects the majority of adults at some time of their life. Most people who develop acute pain have a benign degenerative cause for the pain. The most common scenario is acute pain due to minor mechanical stress or chronic changes known as degenerative disease. The patient should be assured that the cause of the pain is most commonly of musculoskeletal origin and will usually be relieved with conservative therapy including activity, medications, and physical therapy. The concepts of the small space where the nerves exit and the structural changes that can cause clinical problems should be explained. In general, the approach in the absence of neurological symptoms is conservative and no imaging or lab studies are generally indicated. In this instance finding a “knot” in the muscle is a sign of muscle spasm that should respond to conservative therapy. Most patients will improve within 3-4 weeks.
It is frequently unnecessary to use imaging to evaluate neck pain. Degenerative changes are commonly seen on the plain film and MRI of the spine, but are not necessarily reflective of the acute symptoms. Also, the absence of change on the imaging study does not exclude significant disease, and hence the decision to image needs to be based on the clinical findings.
On the other hand, the presence of red flags such as associated neurological deficit, acute significant trauma, night time pain, fever or an elevated white cell count, must be emphasized as signs of more serious therapeutic implications.
References
Alan B. Douglass, M.D. and Edward T. Bope, M.D., “Evaluation and Treatment of Posterior Neck Pain in Family Practice”
Binder A. “Neck pain. Clinical Evidence” Concise 2004 (BMJ); 11:1534-50
Ferrari R, Russell AS, Carroll LJ: A re-examination of the whiplash associated disorders (WAD) as a systemic illness. Ann Rheum Dis 2005 Sep; 64(9): 1337-42 [Medline].
Feiz-Erfan, Iman M.D., Klopfenstein, Jeffrey D. M.D., Bambakidis, Nicholas C. M.D., and Sonntag, Volker K. H. M.D. : ?Surgical Management of Cervical Disc Disease: From No Fusion to Fusion and Back Again,? Congress of Neurological Surgeons, Clinical Neurosurgery, Volume 52, Chapter 43, pages 197-199. American Family Physician, Vol. 59/No. 2 (January 15, 1999)
Isaac and Anderson, ?Evaluation of the patient with neck and cervical spine disorders,? Up-To-Date Online, 15.3.
Iman Feiz-Erfan, M.D., Jeffrey D. Klopfenstein, M.D., Nicholas C. Bambakidis, M.D., and Volker K. H. Sonntag, M.D. : Congress of Neurological Surgeons, Clinical Neurosurgery, Volume 52, Chapter 43, ?Surgical Management of Cervical Disc Disease: From No Fusion to Fusion and Back Again,? pages 197-199.
The Journal of the American Board of Family Practice 17:S13-S22 (2004)
Web links