Introduction
As medicine makes rapid advances in both acute and preventive health care, one finds that the aging population is growing at a commensurate pace. It may not be surprising that the fastest cohort of the population, the geriatric population (65 and older), utilizes the greatest portion of health care services.a In contrast, however, a striking minority (approximately 5%) of older people live in chronic health facilities; rather, most live in their own home or apartment and continue to function as a vital part of society.b Thus it is critical among the health care community and others, to be acutely aware of the unique considerations in caring for the geriatric patient, given the impact that this special cohort is exerting on the health care system, both in inpatient and ambulatory settings.
General Principles
Like all patients, the geriatric patient, in particular, requires a holistic approach. This includes not only careful attention to the anatomic and physiologic uniqueness of the aging body, but also the pathophysiology of geriatric disease in the context of a social milieu. In addition, patient?s activities of daily living (ADL?s) both serve as a backdrop to daily care, as well as strong predictors of prognosis. 1,2 .
Thus, the successful approach to the individual older patient hinges on an integrative understanding that ranges from cellular processes to family and community dynamics. In that vein, comprehensive geriatric assessment and care employs not only medical health professionals, but also members of the patient?s family and community as well. Additionally, quality geriatric care traces the patient?s steps, literally and figuratively, from their home setting to the point of the evaluation in order to truly understand the context of that patient?s health and disease. In fact, it has been demonstrated that home geriatric assessments are associated with overall improved outcomes. 3
Structural Changes
From head to toe, the geriatric patient presents unique challenges and the normal changes that organs and organ systems undergo with aging can periodically be related to subsequent disease. The anatomical approach will later shed light on the normal changes of the aging body and dispel some myths as well. The order of presentation may deviate from the standard presented order in a physical exam, only to emphasize the most apparent changes first.
Structural Changes: Skin
Wrinkled skin, the most obvious hallmark of aging, is a result of sun exposure, loss of subcutaneous fat, decreased oil and sweat production, and thinning of the dermis and epidermis.d Irregular pigmentation, brown macules (lentigines) and telangiectasias, among others, are also a product of the skin?s photoaging, the byproduct of ultraviolet radiation from the sun.
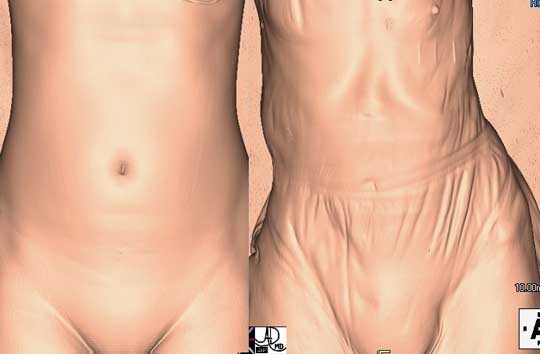
The two images are from reconstructed CT scans that show the difference in the appearance of the skin in a 25-year-old female and an 80-year-old female. The loss of subcutaneous fat, skin turgor and skin elasticity is readily apparent.
Courtesy of: Ashley Davidoff, M.D
Structural Changes: Bone
While there is a tendency toward osteopenia and low turnover osteoporosis in normal aging, skeletal deformities are not considered normal. Any lordosis, kyphosis and/or fractures of the skeletal system all fall under the category of pathology.

Here is a comparison showing the knee of a young adult (left) and a 97-year-old (right). The loss of bone density and joint space narrowing, signifiying osteoarthritis,muscle bulk, and the presence of calcific atherosclerosis of the tibial artery are all part of the aging process.
Courtesy of: Ashley Davidoff, M.D.
Structural Changes: Head Region
Head/Brain: While mild brain atrophy is a normal part of aging as seen both on head CT and gross pathology, delirium and dementia are not. One should never assume that a decline in mental health is due to age alone. Slowed central processing and reaction time, however, is considered a normal part of aging.
Eyes: Grossly, the color of the sclerae may not be as white as they were at a younger age; this is a result of varied, repetitive, normal environmental exposures. In addition, a ring of calcium and cholesterol salts may appear (arcus senilis) on the eye’s surface, which does not affect vision. Finally, the eye may appear sunken and bearing less proximity to the eyelids with normal age related changes of surrounding fat, muscle and tendons. d
Ears: The majority of elderly patients, contrary to popular belief, do not have hearing difficulty. Any hearing loss should warrant concern and careful attention.
Mouth/teeth: Neither is it normal for an elderly patient to be edentulous (lacking teeth), nor to wear dentures. Pathology, especially dental caries, should be addressed, even prior to tooth loss.
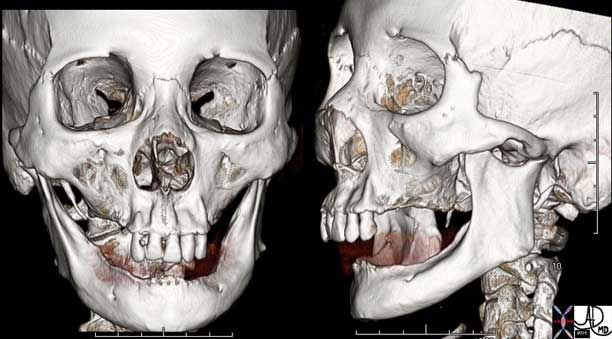
CT scan from an 82-year-old male showing an edentulous skeleton.
Courtesy of : Ashley Davidoff, M.D

Edentulous Elderly Patient
The lateral X-ray of the cervical spine is utilized in this elderly patient to demonstrate the eduntulous state. Note there are no teeth in the upper or lower jaw. Additionally, degenerative changes in the spine are characterized by joint space narrowing and osteophytic change.
Courtesy of: Ashley Davidoff, M.D.
Structural Changes: Body Region
Heart/Blood vessels: Mild hypertrophy of the cardiac muscle is a normal part of normotensive aging, along with increase in left atrial size. Additionally, humans like most mammalian species, age without developing atherosclerosis spontaneously; thus, it is not considered a normal part of aging. 5 Even so, systolic blood pressure shows a general upward trend.
Chest/Lungs: The combination of decreased chest wall compliance and the stiffening of lung tissue (and subsequent loss of elastic recoil) leads to decreased airflow and air trapping. While these changes may not be clinically evident at baseline, a reduced reserve may be the difference between a speedy and prolonged recovery when respiratory infections do occur.
GI tract: Normal aging leads to decreased overall muscle mass, which can weaken, in turn, both chewing and the oropharyngeal phase of swallowing. Gross esophageal function and lower esophageal sphincter should be similar to those in younger patients. Anatomically, there is also a decreased size in the liver and pancreas6.
Kidneys: Gross renal mass is progressively lost with aging, mostly cortical, on average 70 grams by the time one is 80-years-old.
Genitourinary tract: Incontinence is not a normal part of aging, and should always warrant a workup for GU pathology.

The ultrasound scans shown above are from a normal 28-year-old adult (a) and a 97-year-old patient (b). The renal sinus fat is the echogenic tissue in the middle of the kidney and occupies about 25% in the young adult while in the elderly patient the fat occupies almost 80% of the kidney volume. On the other hand, in the normal patient about 75 percent of the tissue is hypoechoic representing the functioning renal parenchyma, while only 20% of the kidney in the elderly patient represents functioning tissue. The border of the kidney of the young patient is smooth, while the border of the elderly patient is minimally irregular. The aging process in the kidney is called nephrosclerosis and it affects both kidneys to the same degree with loss of parenchyma and an increase in fibrous tissue.
Courtesy of: Ashley Davidoff, M.D.
Functional Considerations
Changes in structure lead to changes in function. The structural changes described earlier caused by wear and tear, loss of subcutaneous fat, elasticity of tissue, and decrease in muscle and bone mass result in functional changes. The decrease in muscle mass and strength have far reaching effects in mobility and strength. The aging muscle and nerves of smooth muscle have functional effects in swallowing. The loss of elasticity and the changes that occur in cardiac muscle have functional effects in cardiac physiology. The wear and tear on joints leads to stiffness and pain, limiting function and mobility in any of the many joints.
Functional Considerations: Skin
As normal elasticity of skin collagen diminishes with age and the number of melanocytes diminishes, skin becomes more easily damaged by contact and by the sun’s ultraviolet rays. Dry skin (xerosis) is also very common. Actinic keratoses, which are characteristic red dysplasias on the skin, mark a higher risk for skin cancer in those areas. 4 In addition, simple, common issues like corns and excessive toenail length can limit the geriatric patient?s ability to walk properly and may increase fall risks in an otherwise healthy patient.
Functional Considerations: Muscle/Fat
Due to the decrease in muscle mass (sarcopenia) and particularly muscle to fat ratio, the ability of the geriatric patient to maintain past strength in walking and transferring can be limited. A combination of sarcopenia, decreased muscle innervation and increased fatigability contributes to an overall loss of strength as well. In addition, sarcopenia parallels a decrease in the basal metabolic rate of the elderly patient6 and patients may subjectively feel more tired and/or cold.
Functional Considerations: Bone
It is normal at every age for bone loss to occur. In a younger patient, bone formation (osteoblastic activity) balances out bone resorption and loss (osteoclastic activity). In an elderly patient, there can be more bone loss than formation, up to 30mg/day.5 The lack of bone forming activity behind bone resorption leads to low turnover osteoporosis (see next section). That being said, fractures of any bone are not the norm, and pathology should always be pursued, if and when they occur.
What is the term for a decrease in muscle mass?
(Note: You will be given 2 tries to answer this question, then the answer will be provided.)
Xerosis
Sarcopenia
Edentulous
Presbycusis
Functional Considerations: Head Region
Head/Brain
Normal age related brain atrophy leads to increased stretch of bridging veins, making them more prone to subdural injury, even from minimal or no trauma. And while there may be increased numbers of neurofibrillary tangles and senile plaques and impaired brain autoregulation of perfusion6, this does not necessarily translate into brain pathology. Even when there are minimal declines in memory, most are not pathological, and are often referred to as Age-Consistent Memory Decline or Age Related Cognitive Decline (DSM-IV).
Eyes
Normal aging can lead to dry eyes, due to decrease of mucus cells in the conjunctivae and decreased tear production. This issue can be especially exaggerated in post-menopausal women. Also, mild age related visual changes, including contrast sensitivity and dark adaptation, may result from normal degeneration of the lining of the inner surface of the cornea, as well as slower pupillary reaction and the decrease in pupil size with age. Finally, stiffening and yellowing of the lens, which is normal with aging, leads to difficulty focusing on close objects (presbyopia). In addition, color differentiation becomes less acute. Jaundice is never normal in an elderly patient and should prompt a hepatic or hematologic etiology.
Ears
While hearing loss is not a normal byproduct of aging, it still remains quite common among the geriatric cohort, and its incidence rises with age. It falls under the category of disease.
Nose
On average, smell detection dimishes in the elderly by approximately 50%. 6
Mouth/Teeth
While there is a decrease in muscle mass, especially type I (slow) fibers, the overwhelming majority of the geriatric cohort will not develop clinically significant oropharyngeal weakness, leading to swallowing abnormalities. Though a minority of normal elderly have been demonstrated to have mild pharyngeal muscle weakness and abnormal cricopharyngeal relaxation, this has not shown to be a cause of clinical disease.
Functional Considerations: Body Region
Heart/Blood vessels
Due to changes in collagen and elastin, arterial walls become harder and the aorta dilates and elongates. The above changes can lead to reduction of both cardiac filling rate (diastolic), as well as increased afterload.4 Importantly, there is a marked dropout of pacemaker cells in the SA node, which may or may not lead to subsequent electrophysiologic abnormalities.6
Chest/Lung
Ventilatory response to hypoxia and exercise capacity can be blunted due to mild ventilation-perfusion mismatches, decreased lung compliance and chest wall stiffening of normal aging. This is reflected in a decreased FEV1 and FVC, and a decreased CO diffusion (DLCO).6
GI tract
A mild decrease in innervation of the esophagus, and a decrease in slow-acting (type I) muscle fibers in the distal esophagus, can lead to decreased amplitude of esophageal contractions in patients over 80, but this does not necessarily lead to a functional abnormality in swallowing; in fact, for the most part, esophageal function is preserved in the elderly. Metabolically, however, after the age of 60, decreased calcium absorption is considered the norm, secondary to decreased levels and sensitivity to metabolites of vitamin D. 5
Genitourinary Tract
Kidney
Increased post-void residual and incomplete emptying of the bladder could potentially set up the geriatric patient for urinary bacterial overgrowth and create a higher risk for urinary tract infection. In addition, incontinence is not normal for an elderly patient and its presence should always be a red flag. A sudden mental status change in the elderly can often be the sign of a simple urinary tract infection.
Blood/Hematopoesis
Bone marrow is not always able to respond to disease stress as quickly as it once did, given decreased marrow reserves of all cell lines.6
Endocrine
Multiple changes are seen in normal aging of the endocrine system, including impaired glucose tolerance (leading to increased serum insulin), decreased testosterone (men and women), ovarian failure (women), decreased T3, decreased vitamin D production, increased PTH, and increased homocysteine levels. These changes may contribute to increased tendencies toward diabetes, osteoporosis and heart disease in older patients.
Immune system
Multiple factors of the immune system are decreased in normal aging, including, but not limited to, cell-mediated immunity, IL-2 release, B-cell production, and macrophage function.
Sexual Function
For men there is a prolonged refractory period for erections and for both women and men there is a reduced intensity of sexual orgasm. Loss of sexual ability should, however, always prompt a secondary workup (i.e. prostate, medications).
Diseases Prevalent in Group
The changes described in structure and function that occur with aging, not only impair activities of normal daily life, but also result, or are associated with diseases and disorders. Wear and tear and mutation accumulation are some of the theories that are proposed.
As patients age, the risk of developing cancer is increased, with close to 80% of cancers being diagnosed in people 55 years and older. The risk of breast cancer in a 30-year-old woman is 1 in 2000 and at the age of 60, it becomes 1 in 30. The probability of prostate cancer before 40 is about 1 in 13,000 while by 80-years-old it is 1 in 7. For colon cancer, the risk before the age of 40 is about 1 in 1600, while in the 80-year-old, it is about 1 in 30. By the age of 65, 50% of patients will have had skin cancer. Lung cancer is usually seen in patients over the age of 40 years. As a result of these risks, screening programs that are age-related have been put in place. Colon cancer screening starts at age 50 and breast screening starting at 40 years are two examples.
While cancer accounts for about 20% of deaths in patients over 65, cardiovascular disease with atherosclerotic changes and hypertension are the most common causes of death in patients over 65, accounting for about 30% of all deaths.
Degenerative arthritis is a disease that is directly related to the aging process due to wear and tear on the joints, being particularly prominent in the weight-bearing areas. The tendency to gain weight with the aging process aggravates the process.
By the age of 65, _____ of patients will have had skin cancer.
25
50
75
90
Diseases Prevalent in Group: Skin
Elderly suffer from similar skin disease that younger patients do, including dermatitis of any cause, psoriasis and bullous disorders. Yet, more importantly, with age, risk for skin neoplasms also rises. Thus, any change in shape, border, color, or character of any skin lesion should always warrant concern for a skin cancer workup.

The images are taken from a reconstructed CT scan. Three dermatomes are shown that correspond to three of the areas of innervation supplied by three thoracic nerves. Herpes zoster infects the nerves and pain is distributed along the affected dermatomal distribution of the nerve. Symptoms are usually unilateral but may be bilateral, but are always along the distribution of the nerves affected.
Courtesy of: Ashley Davidoff, M.D.
Cellulitis and Skin Ulcers
Due to increased skin fragility and potential microtrauma, cellulitis is a common entity in geriatric medicine. While the pathogens are often the same as in younger patients (Staphylococcus aureus, group A streptococcus), frail patients referred from chronic health facilities or who have been recently hospitalized would be more at risk for gram negative and other more resistant organisms leading to, perhaps, prolonged and more intensive intravenous treatments, and slower recovery. While any skin infection can ulcerate, debilitated and/or bedbound patients have a predominance for decubitus skin ulcers, seen often on the sacrum and heels, among others. This complication of prolonged bedrest can often be prevented by frequently turning the patient (at least every 2 hours) and providing proper cushioning in beds and chairs, most notably at bony prominences. Pressure sores are graded from I-IV, from superficial erythema all the way to muscle and bone involvement; yet at times, a stage I ulcer may be hiding a deep stage IV just under the skin. Thus, all pressure sores must be treated seriously and aggressively from the start. Proper nutrition and specialized dressings are also important adjunct therapies in pressure ulcers.
Diseases Prevalent in Group: Musculoskeletal
Osteopenia/Osteoporosis
Bone loss, resulting in bone microfragility and clinical fractures, can be categorized as either high turnover, as seen in post-menopausal women or low turnover (a normal aging phenomenon). Osteoporosis is multifactorial, potentially stemming from lack of vitamin D intake, lack of light-induced vitamin D activation in the skin (decreased sun exposure), increased PTH (parathyroid hormone) production, decreased GI calcium absorption and overall decreased ratio of osteoblastic to osteoclastic activity. Diagnosis is made with bone densiometry.
Compression Fractures
Compression fractures of the spinal vertebrae are a common, often painful casualty of patients with osteoporosis, especially in older women. Compression fractures of the spine can occur with only minimal exertion, even simple walking and transfers.
Kyphosis
Kyphosis (curvature of the upper spine) and lordosis (inward curvature of a portion of vertebral column) are commonly experienced pathologic anatomical deformities of the spine, often a result of the combination of degenerative joint disease, thoracolumbar compression fractures and osteoporosis. Lying on a non-contoured gurney in the emergency department and/or waiting for radiological tests can make for a painful experience in kyphotic patients.
Hip Fracture
Hip fractures are a common medical condition in the elderly, yet whose morbidity and mortality can be astonishingly high, up to 14-36%, within one year from occurrence. Surprisingly, hip (proximal femur) fractures can occur frequently, prior to a fall, and can be, in fact the cause of a fall. All costs need to be taken to avoid this occurrence, including treatment of osteoporosis, among others; yet in the hospital setting, as much as is possible, trivial trauma should be avoided and aid in transfers should be always fully offered by trained staff for elderly patients.
Diseases Prevalent in Group: Head Region
Delirium is the most commonly seen disorder of cognition and is characterized by an acute alteration and cognition that often waxes and wanes. Delirium is frequently multifactorial, whether secondary consequence of concomitant disease(s) elsewhere in the body, postoperatively or a medication effect (the most common). In addition, delirium may be noted in geriatric patients by virtue of change of environment (e.g. home to hospital). Dementia has been shown to be a risk factor for delirium though does not necessarily have to be present to occur. Others are severe underlying illness, impairment of vision and pre-renal (dehydrated) status. The most important consideration in delirium is identifying the underlying cause, when possible, and correcting it.
Dementia is defined as progressive, global cognitive decline. A demented patient presents frequently with learning and memory deficits (recent more than remote), speech deficits (aphasia), difficulty performing purposeful movements (apraxia), and/or difficulty recognizing objects (agnosia). The most common form of dementia is Alzheimer?s disease, which can present with features of mood disturbance early on and psychosis later in the course. The cause of Alzheimer?s disease is thought to be multifactorial, including genetic, environmental and cardiovascular. The end result is neurofibrillary tangles in the brain, most notably in the frontal lobes. Another common cause of dementia is Lewy body disease, characterized by a marked fluctuation in cognitive impairment, prominent hallucinations, signs of parkinsonism and falls. Vascular dementia is a secondary consequence of atherosclerotic disease, often intimated by a history of stroke or ischemic brain injury on head imaging (e.g. CT/MRI). While Alzheimer?s, Lewy body and vascular dementia make up approximately 95% of commonly seen dementias, less common causes should be considered, including Pick?s (frontal lobe atrophy/loss of inhibitions), Parkinson?s, Huntington?s, Creutzfeld-Jakob, alcohol related, and AIDS, each with its own characteristic features. Unfortunately, most dementias are not highly amenable to treatment. 6
Eyes
Cataracts become very common in older age; in fact, cataract surgery is the most commonly performed surgery in the USA on the elderly. In patients with cataracts, direct and/or bright light can be bothersome, and should be avoided if at all possible, especially in the context of a patient examination or radiology holding room. 3
Glaucoma: Defined as an increase in intraocular pressure, glaucoma is not a geriatric disease, however it remains an important cause of blindness in the over 40 age group.
Age-Related Macular Degeneration (AMD): Over the age of 75 approximately 33% of the population will experience some degree of macular degeneration. This age-related phenomenon is fast approaching glaucoma and diabetic retinopathy as the leading cause of legal blindness. 90% of the cases encountered are untreatable, and are referred to as dry (atrophic); the remaining 10% (wet) may be amenable to halting disease with laser, but complete return to normal sight is not tenable. Peripheral vision in the latter form of age-related macular degeneration may suffice to function normally, however.
Ears
Deafness: Many elderly will experience some degree of idiopathic, bilateral, symmetric, sensorineural hearing loss (presbycusis). It is estimated that as many as 40-50% of patients over 75-years-old will have some sort of presbycusis. And though a common phenomenon, it is not part of normal aging to develop this disease, nor any hearing loss. And while in 1994, 33.2% of the geriatric cohort reported hearing loss, only 11.6% reported using a hearing aid in that year.
quizme.gif
__________characterized by an acute alteration and cognition that often waxes and wanes.
Mild atrophy
Delirium
Dementia
Alzheimer’s disease
Diseases Prevalent in Group: Mouth
Oropharyngeal dysfunction
As mentioned earlier, chewing can become weakened due to reduced masticatory muscle performance in the elderly. And while, not pathologic in and of itself, weakened chewing combined with dentures (or lack thereof), and diminished salivary gland function (often medication related) can lead to aspiration of food and subsequent pneumonias (see below).4
Oral thrush
While not particularly a geriatric disease, Candida albicans, a normal colonizer of the mouth, can become especially active in older patients with several disease states (e.g. cancer) or medications (e.g. steroids) that weaken immune system function or change local flora.
Edentulousness
Most recent data shows that only approximately 26% of the population over 65 are edentulous (toothless)c. The number of edentulous patients has decreased from 40% in 1986, likely in part to improved awareness and practice of dental hygiene. Those patients, however, who do have either partial or full dental prosthesis may suffer from improper fit and associated psychosocial stigmas. As edentulousness decreases, however, dental caries and preventive dental medicine, normally considered a realm of younger patients, is becoming a greater focus in geriatrics.6
Diseases Prevalent in Group: Cardiovascular and Lungs
Hypertension
More than 50% of Americans become hypertensive after the age of 65, often requiring anti-hypertensives. 4 In turn, as blood pressure rises, so too does the risk for hypertensive disease, including cardiovascular and renovascular disease and retinopathy.
Orthostatic hypotension
A drop in systolic blood pressure of >20 mm Hg when going from a sitting to standing position is relatively common in patients over 65 years old (approximately 20%). This can be exaggerated after eating (post-prandial) and/or taking certain medications (e.g. anti-hypertensives) and may lead to dizziness, near syncope, syncope and falls. Many times too, it is asymptomatic, though should always be concerning. Orthostatic hypotension may be one of the only signs of a gastrointestinal bleed.
Lungs
Aspiration pneumonia
Multiple factors play a role in the increased risk of elderly patients of developing aspiration pneumonia. These include, but are not limited to, chewing difficulties, impaired cough reflex, less effective ciliary action, decreased respiratory muscle strength, stiffened chest wall and a decreased ventilatory response to hypercapnia. 6 While more common in geriatric cohort of those with dementia and/or bedbound, aspiration can occur with any older patient, and should always be on the differential of dyspnea and/or hypoxia in the elderly.
Diseases Prevalent in Group: Gastrointestinal and Genitourinary
GI (gastrointestinal) Tract
Diverticulosis
The most common anatomical change of the aging GI tract is diverticulosis, caused by weakening of the colonic muscle. The incidence approaches half of all geriatric patients in Western countries, and rises with age. Though usually asymptomatic, it can lead to significant lower GI bleeds and infection (diverticulitis).
Constipation
Constipation is common in aging; though not necessarily a byproduct of aging, constipation is often multifactorial. Often times, however, a particular medication (e.g. opiates) or mineral (e.g. calcium) may be implicated. In addition, lack of water intake and lack of dietary fiber play important roles in constipation. Fecal impaction should always be entertained in a constipated elderly patient and efforts at manual disimpaction are often the mainstay of therapy in this disturbing condition, if conservative measures have failed.
GU (genitourinary) Tract
Urinary incontinence
While urinary incontinence is not necessarily normal in aging, it has become the hallmark of geriatric disease, given the significant social stigmas associated with them. Whether because of enlarged prostate (for men), lack of pelvic muscle support (women), medications or simply not being able to get up out of the bed for multiple reasons, urinary incontinence increases with aging. The differentiation should be made among urge (detrusor muscle irritability), stress (incompetent sphincter) and functional (impaired mobility) incontinence, since the management options vary. In any case, this issue should always be addressed in the initial evaluation of any geriatric patient, since the patient may not always mention it and a lack of attention, thereof, can often lead to an uncomfortable situation for both patient and caregiver.
Impotence and sexual dysfunction
Often a difficult subject to discuss with younger patients, a discussion of impotence or dyspereunia may appear even more ominous in a geriatric patient, yet should not be avoided. Sexual dysfunction may be a result of prostatic disease/surgery in men, lack of local vaginal estrogens in women and/or a side effect of common medications. Though common in aging, aging should not be labeled as the cause, and then be brushed aside. Whatever the case, the clinician may need to prompt the discussion as part of a comprehensive evaluation and should not shy away from addressing this phenomenon. In one study, approximately 87% of married men and 89% of married women in the 60-64 age range are sexually active. In addition, 29% of men and 25% of women over the age of 80 are still sexually active. g
Diagnostic Approach – Clinical Consideration
More time and patience is a clear need in geriatric evaluation and assessment and must be allotted as such. Integration of a potentially long and complex past medical history is an essential ingredient of the diagnostic approach of the elderly patient. And while time constraints are a part of any medical setting, from home visit to office to hospital, the caregiver must not only give more time to the elderly patient than the average patient, but also be perceived as giving more time. The elderly patient not only requires more time, due to the often complex nature of their past medical history and potentially varied complaints, he or she also requires more social interaction, support and validation of their overall condition. The key to a comprehensive evaluation of the geriatric patient lies in the details, many of which can often be obtained by varied personnel of the medical staff, and then be conglomerated and integrated by the direct primary caregivers.
Home visits of a multi-disciplinary nature, as hinted to earlier, are an important, if not crucial, part of evaluating the elderly patient and can often give insight into the pathology of disease (e.g. falling over a loose carpet). Home visits are now being covered by Medicare, as they have shown cost effectiveness by delaying onset of disability and future long term care placement. (Stuck AE. A trial of annual in-home comprehensive geriatric assessments for elderly people in the community. New England Journal of Medicine. 1995;333:1184-1189.)
The setting for evaluation of an elderly patient in the outpatient arena should always be kept at a comfortable temperature, with comfortable lighting, free of background noise and face-to-face in comfortable, safe chairs. Special, higher and/or mechanical chairs have been designed for the very frail and should be considered for the elderly who may suffer from thigh (proximal) weakness. A step stool, handrail and assistant should always be provided for the elderly patient in order to reduce possibility of falls. All other obstacles in the examining room should also be removed and/or adjusted to reduce fall risk, including exam curtains, lamps, chairs, and the like.6
The inpatient evaluation, often in the patient?s room, is similar to that of the outpatient, yet it should be emphasized that the patient?s private belongings may often be scattered and/or misplaced. This may leave a patient without his or her corrective lenses, hearing aids, and dental prostheses, creating patient anxiety as well as an incomplete exam. All efforts should be made to give the patient a feeling of home, sense of self, privacy, and completeness, even in this foreign, often confusing environment. Many times a simple picture from home can focus an elderly patient and turn confusion into familiarity.
Wheelchair access and automatically opening doors are a requirement for any facility that welcomes elderly patients. In addition, any evaluation of a geriatric patient, whether inpatient or ambulatory, should allow the patient the opportunity to be accompanied by a caregiver, family member or other companion. This can often be subtly communicated by the presence of extra comfortable chairs in the waiting room, evaluating room and registration areas. Waiting rooms need to be comfortable, with chairs well padded, and copious reading material, including large print options.
Bathroom facilities should have sidebars next to commodes to provide physical support for the patient using them and should, as above, provide room for entrance of wheelchairs and walkers, as a rule.
History
From the lucid ambulatory to the demented bed-bound patient, a face-to-face caregiver to patient history is strongly encouraged and important in both general rapport as well as diagnosis. Never should one rely only on word of mouth, nor medical records as sole tools for taking a history from a geriatric patient. Patience and genuine personal interaction is a defining characteristic of medicine in general, but it is even more an emphasis in geriatric history taking. And while patient autonomy is paramount, it may often be necessary to have a family member or caretaker present for the history. That is neither to say that the geriatric patient?s history is unreliable, nor to imply that the companion should give the history in place of the patient, rather an accompanying relative or caregiver can often fill in important blanks and make the patient feel more at ease in the healthcare setting. Bringing a companion should always be the patient?s initiative however, when able to make that decision, and all patients should be given the opportunity to be interviewed and examined alone, even when accompanied to the office.6
Any initial interaction at every level, from nursing aide to professor, one must address the patient?s potential need to use the restroom. Out of general courtesy and to avoid potential embarrassment, asking the patient if he or she would like to use the restroom sets the stage for a productive interaction and is a polite ice-breaker.
The initial baseline history, if not immediately obvious, should include information on baseline functional status (ambulatory, wheelchair bound, bed-bound) in order to assess severity of disease and further management. Assessment of the 7 basic ADLs (activities of daily living: feeding, hygiene, dressing, continence, transferring, bathing and mobility) and IADLs (independent activities of daily living: shopping, cooking, cleaning, managing money, telephoning, laundry, and travel) have been shown to be important tools in both diagnosis and prognosis of disease.
History of the geriatric patient is, of course, similar to any complete history of any patient. An initial geriatric history, understandably, will often take longer than the history of a younger patient, and requires allowance of greater time allotments. The review of systems in a geriatric patient can often point in several directions, rather than toward one diagnosis, and more often than not a unifying diagnosis is more elusive in the geriatric population. 6 In addition, there should be several foci within the geriatric history which include emphases on:
- Medications: Due to risk of dangerous drug-drug interactions, potential overuse of over-the-counter drugs, misuse of herbal supplements, and simple accumulation of medication that may no longer be indicated, a careful drug history should be obtained. A comprehensive medication history can give clues in diagnoses of common problems, such as changes in mental status, acute kidney injury, and liver function abnormalities, among others. Assessment of the organization of a patient?s medications, often best obtained by asking the patient to bring all bottles and/or pillboxes, will provide a window into the understanding and compliance that a patient demonstrates.
- Social History: should include detailed information on the patient?s living situation and, if possible, a home-visit should be conducted to further evaluate the physical environment of the patient, and identify possible safety concerns. It is also important to determine if a patient is a caregiver him/herself, which can place the patient at higher risk. In that context, social supports and potentials for social interactions should be identified, as they are a major factor in both prevention of and recovery from disease. In addition, it should never be assumed that an older patient does not drink alcohol or use recreational drugs. These topics should not be avoided due to health provider discomfort. Finally, smoking cessation is never too late to address, and can play a role in positive health strategies, even in the very old. 6
- Nutritional History: Though malnutrition is less common in ambulatory geriatric patients, the chronically ill or bed-bound pose a higher risk as such. Patients? dietary patterns are a prime concern in a patient with chronic disease of any type.
- Family History: Family history, though important, becomes less of a focus in the diagnosis of the geriatric patient, since all diseases cause morbidity and mortality more as most diseases go up as one ages. That being said, depression and dementia may be an important piece of family history to gather, as they can often run in family clusters.
Labs
A variety of laboratory anomalies can be seen in the elderly patient, most of which are noted upon hospitalization, when a value which might appear normal may not be and vice versa. A common example would be when an elderly patient would seem to have a normal or even low white blood cell count in response to a pneumonia. A sample summary of lab changes in aging appear in the following table.
| Lab Value | ? in Aging |
| Glucose toleranceê | decrease |
| Insulin | increase |
| DHEA |
decrease |
|
Testosterone |
decrease |
| T3 | decrease |
| Estrogen & Progesterone | decrease |
| Homocysteine levels | increase |
| Serum atrial natriuretic peptide | increase |
| PaO2 | decrease |
| GFR | decrease |
| Renin & Aldosterone | decrease |
| Autoantibodies | increase |
| IL-6 | increase |
| IL-2 | decrease |
| Cell mediated immunity | decrease |
Other Considerations
Albumin correlates with mortality and reflects the patient?s nutritional status over the prior 3 months. 7 Prealbumin reflects nutritional status over the past 20 days. A low prealbumin as well as a lymphocyte count may reflect a poor nutritional status.
Venous access issues
While it may be more common to have difficulty gaining venous access in the elderly patient, due to tissue fragility and blurring of venous markings, it is by no means impossible. As a rule, central venous catheters should be avoided at all costs in the elderly for venous access, unless a life-threatening medical condition arises (e.g. hypotension, severe sepsis), in order to avoid the complications of placing a central line, among them pneumothorax and bleeding. This is especially a concern for patients with COPD, ventilated patients, and those taking anticoagulants.
When IV access is difficult and long-term intravenous medications are required, an interventional radiologist may be consulted for a PICC (peripherally inserted central catheter) line to be placed under flouroscopy.
In addition, elderly patients requiring simple IV fluids for mild to moderate dehydration, multiple studies have shown that subcutaneous fluids (hypodermoclysis) is an equally safe alternative to and less agitating than IV.
Imaging
In 1990, geriatric patients accounted for almost half of all CT scans, arteriograms and angiocardiograms on hospital inpatients. (Darnay AJ, ed. Statistical Records of Older Americans. Detroit, Mich: Gale Research; 1994). A good review of geriatric radiography can be found in Dowd and Wilson?s Encycopedia of Radiographic positioning. And while the need to understand the special needs of the geriatric patient in the radiologic setting is great, it is not clear that those demands are being met. In one survey of 835 radiologic technologists (270 of which responded), it was found that attitudes of geriatric patients may be worth attention. Respondents felt that elderly patients are slower in completing exam, hear poorly in general, are less compliant with preparatory steps prior to radiologic tests, than younger patients. There were also open comments in the survey referring to older patients as complaining more, slower to move in general and often childlike. Interestingly, the surveys implied, however, that the more experienced the radiolographer, the more adept at handling elderly patients than new graduates (Rarey, Linda K. Radiologic Technology, July 1, 1998). Findings may suggest that there need be specific training approaches to address the need of attention and sensitivity to the growing needs to train radiographers in the needs of a rapidly expanding elderly population undergoing radiographic tests. In addition, the geriatric patient population may require greater amounts of education prior to, during and after, radiographic tests to avoid confusion and maximize the radiographer-patient interaction, and ultimately test result.
Imaging: Instruction before Coming to the Office or Hospital
Elderly patients should be instructed to wear loose comfortable clothing when coming for any exam or radiologic test. In addition, a patient should be aware that it is important to have all hearing aid devices readily in place, if appropriate.
Registration process
One should never assume that an elderly patient is hard of hearing and automatically speak loudly. If an elderly patient initially appears not to understand, it is often best that the interviewer readdress the patient at eye-to-eye level and speak clearly to avoid misunderstanding. The patient should be made aware that certain tests use IV dyes that may cause an allergic reaction and the patient should make any allergies clear and known from the outset prior to or during registration.
The special approach to the patient in the imaging department: Every effort should be made to keep the elderly patient comfortable and calm while waiting for tests to be done in the radiology department. Whether ambulatory in the waiting room or on the stretcher, more often than not, there is associated anxiety with undergoing radiologic tests for any patient. Elderly patients may be more prone to anxiety surrounding potential results and long waiting times. In addition, all attempts at fall prevention are crucial, whether that means an obstacle free waiting room, raised guardrails on the hospital gurney or assistance from the technologist to transfer to the examination table. Similarly, due to increased skin fragility of the elderly patient, hematomas and skin tears become more common with only minimal contact with doorways, bedsides, and the like. All efforts need to be made to avoid these casualties of normal movement.
Imaging: Special Equipment
Depending on the needs of the patient, appropriate equipment should be available for transport and transfer of patients in the radiology department. Wheelchairs should be readily accessible for patients who may have difficulty walking distances from the facility?s entrance to the imaging department, along with staff to transport the patient. Comfortable gurneys and/or hospital beds suffice for inpatients, yet staff trained in proper transfer techniques are crucial to prevent both patient and staff injury. In that regard, exam tables need to be made comfortable, with appropriate supervision and/or securing devices for maximal patient safety.
Bathroom facilities should provide safety bars alongside commodes, provide ample space for wheelchair entrance and storage when necessary and low sinks for wheelchair bound patients to facilitate hand washing.
Imaging: CT and MRI
Computed Tomography (CT) with contrast or other contrast studies
When a patient is required to receive IV contrast for a Computed Tomography (CT) or any study, staff at every level of care should inquire about allergies to IV dye as well as pursue relevant past medical history regarding risk of contrast induced kidney injury (nephropathy), including but not limited to, diabetes, hypertension, and chronic kidney disease.
Magnetic Resonance Imaging (MRI)
Inquiries need to be made regarding pacemakers in patients, although many MRI?s and pacemakers are becoming compatable with advancing technology. Recent stents or other procedures requiring metal staples and the like need to be addressed, as it is best to avoid MRI in a short time window after such procedures.
In any study requiring prolonged supine positioning, light sedation/anxiolytics may be considered, yet this should be administered, if at all, in the context of the patient?s overall medical condition. If a patient is ambulatory, any patient given the above medication classes should be asked to have an accompanying family member or friend to assist the patient in and out of a vehicle and home. Any sedation and/or anxiolytic use raises the fall risk of the elderly patient and should be avoided if at all possible. In the hospitalized patient, slightly more liberality in this regard may be appropriate, yet utmost attention to changes in mental status need to be made. Confusion of elderly patients secondary to medications (e.g. benzodiazepines) is an avoidable and undesirable phenomenon.
Management
The medical management of geriatric patients is similar to that of the management of other patients in many common conditions. Yet, while comprehensiveness is a tenet of the medical management of all patients, the geriatric patient often additionally requires several coordinated layers of care under the umbrella of a multidisciplinary approach. This team may include not only the internist for medical diagnosis and treatment and the nurse for daily care and basic therapies, but also the speech therapist for potential swallowing difficulties, physical therapist for potential mobility difficulties and occupational therapist for functional independence exercises. No less, a trained pharmacist is frequently a useful team member in evaluating potential drug-drug interactions, reduction of polypharmacy and dose adjustments for a diminished glomerular filtration rate. For patients with pneumonia, a respiratory therapist can often serve a crucial role in mobilizing secretions and preventing loculation and/or parapneumonic effusions in older patients who have difficulty clearing sputum. Additionally, a trained specialized wound care nurse, when available, has a pivotal role in the assessment and treatment of decubitus ulcers, skin tears and other issues surrounding increased dermal fragility in elderly patients.
In planning the course for both medical and surgical management of geriatric patients, the principal tenet, as in all medicine, is ?prima non nocere? (first, do no harm). Addressing treatments, their potential benefits and harms becomes an acute issue many times in the geriatric patient, who may or may not prefer invasive tests and/or therapies. Therapies that would certainly do more harm than benefit the patient are not obligatory to offer any patient, let alone an elderly patient. That being said, therapies whose risk/benefit ratio approaches 1:1 are important to offer the elderly patient and allow them to make an informed choice as to the direction he or she wants to take. It is feasible that a seriously ill older patient may want to engage in a potentially uncomfortable treatment or test if it offers the possibility of only a few more days or weeks to live, allowing for a distant family member to arrive at the bedside. It may be out of the realm of the health practitioner?s advice to withhold or withdraw therapies and/or tests due to practitioner perception of poor quality of life or suffering, if those wishes are not expressly stated by the patient. Finally, what is termed as ?code status? should always be addressed at not only regular intervals at an outpatient basis, but also at every significant change in health status, allowing for the patient to weigh the risks and benefits of cardiopulmonary resuscitation, temporary intubation for respiratory distress, dialysis, feeding tubes and similar topics in advance of their actual need and while the patient is able to make those decisions.
Potential Complications to Consider
Falls
Falls are a common event in the elderly, whose cause, more often than not, is multi-factorial. Falls may be the sign of other concomitant disease and/or may lead to other disease, including hip fractures and subdural hematomas, among others. And while falls may frequently be a compound result of the normal anatomic changes of aging described, pre-morbid pathology(ies) should always be considered. In an effort to preserve one?s natural self-autonomy, the elderly patient may tend to minimize the fall(s) by saying ?I just slipped,? a statement which must always be taken with a grain of salt. That is not to say a caretaker should not trust the words of a patient, rather pre-and post-fall morbidities must consistently be excluded, since in many cases, a fall is the tip of the iceberg. The discussion of falls must be weaved through our discussion of pathology and disease, as it is a common thread, and the harbinger of overall decline.
Red Flags
The following conditions should warrant concern and a comprehensive emergency room evaluation in the elderly patient, as they may be signs of a life-threatening condition:
- Fall with or without head trauma
- Pre-syncope or syncope
- Severe eye or headache
- Sudden blindness.
- Change in mental status, including but not limited to confusion and lethargy.
- Focal weakness.
- Dysphagia
- Productive cough
- Cyanosis or extreme pallor
- Tachypnea with or without pursed lip breathing.
- Tachycardia, even mild.
- New or sudden chest, back or abdominal pain.
- New abdominal distension.
- Bloody or black tarry stools with or without symptoms.
Patient / Family Information
Evaluation and care of the elderly patient can be markedly complex, yet their integration and simplification is the key to success. Recognition of subtle warning signs, like confusion, or not so subtle signs like falls, can be the difference between life and death in older patients at home. That being said, the emergency room is rarely the first stop in managing geriatric medical problems. Rather, often times, phone management, home visits and clinic appointments are a preferable alternative, when possible. Elderly patients should always have an emergency medical number available to call, in addition to neighbors, friends and family as part of their social support system; and when necessary it is best to recommend that one wear a call-button for an automatic medical emergency activation system.
In the clinic and hospital, altered and subtle presentation of disease results should be at the forefront of the diagnostician?s mind in the elderly patient presenting with vague and varied complaints. In addition, polypharmacy need always be addressed at every clinic and hospital visit in an effort to streamline medical regimens, not only to increase compliance of necessary medications, but also to remove unwanted side effects of those less necessary.
Care of the elderly patient requires a dedicated knowledge of the structural and functional changes that evolve with time and the approach to their clinical, diagnostic, and therapeutic care should be tailored to these changing needs.
References
- Katz S, Stoud MW. Functional assessment in geriatrics: a review of progress and directions. Journal of the American Geriatric Society 37:267, 1987
- Lichtenstein MJ, Federspiel CF, Schaffner W. Factors associated with early demise in nursing home residents: a case-control study. Journal of the American Geriatric Society 33:315, 1985.
- Barker LR, John R. Burton, Philip D. Zieve. Principles of Ambulatory Care. 7th ed. Williams and Wilkins, 2006.
- Hazzard, William R. et. al. Principles of Geriatric Medicine and Gerontology. McGraw-Hill. 5th edition 2003.
- Cassel, Christine, et. al. Geriatric Medicine: An Evidence Based Approach. 4th ed. Springer. 2003
- Koval KJ et al. Functional recovery after fracture of the hip. J Bone Joint Surg. 1994; 76:751-758.)
- Corti M-C, et al. Serum albumin level and physical disability as predictors of mortality in older persons. JAMA. 1994; 272:1036-1042.
Web References
- a) Older Americans Aging Stats.gov 2012
- b) Healthy Aging CDC.gov
- c) Geriatrics – The Merck Manual
- d) American Psychological Association ? Approach to the Aging Patient – multiple topics
- e) Vision, Hearing, Balance, and Sensory Impairment in Americans Aged 70 Years and Over: United States, 1999-2006 CDC.gov
- f) Sex, Romance, and Relationships Survey of Midlife and Older Adults AARP .

