Applied Anatomy of the Liver
Definition
The liver is the largest gland in the body and it is central to many metabolic functions. It is known as the “metabolic warehouse”.

The liver is integral to the digestive system, producing both internal and external secretions. The external secretion, bile, aids in the digestive process, while internal secretions are responsible for the metabolism of both nitrogenous and carbohydrate materials absorbed from the intestine.
As the largest gland in the human body, the liver serves several important functions. It secretes bile in order to chemically alter toxic substance (e.g. converts ammonia to urea), converts glucose to glycogen, and can produce glucose from breaking down certain proteins. The liver also synthesizes triglycerides and cholesterol, breaks down fatty acids and produces plasma proteins necessary for the clotting of blood such as clotting factors I, III, V, VII, IX and XI. Nearly 30% of the blood pumped by the heart passes through the liver in one minute.
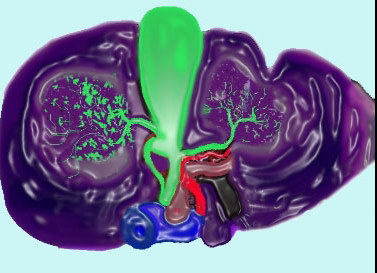
One of the unique structural features of the liver is its dual blood supply. It is supplied both by an artery (hepatic artery) and a vein (yes a vein!) – the portal vein. The portal vein (shown in the diagram below) drains the gastrointestinal tract of digested metabolic products and transports the nutrients to the liver for processing.
The Liver Long Ago
4000 – 5000 years ago, the sheep’s liver held godly powers over the Babylonian culture. The Babylonians, and many cultures thereafter, believed that since the liver was the largest organ, it certainly must be the organ of most importance.
Anatomy and Physiology of the Liver: Overview I

The middle hepatic vein divides the liver into two lobes – right and left lobes. The middle hepatic vein runs parallel and superior to the long axis of the gallbladder.
Anatomy and Physiology of the Liver: Overview II
A good way of defining the left from the right lobes of the liver is to use the gallbladder as a line of demarcation. The gallbladder runs in the same axis as the middle hepatic vein and performs the same structural function in dividing the liver into right and left lobes.

Anatomy and Physiology of the Liver: Position – Normal Frontal View
The liver resides in the upper and right quadrants of the abdominal cavity, nearly occupying the entire right hypochondrium, the greater part of the epigastrium, and not uncommonly extending into the left hypochondrium as far as the mammillary line.


Anatomy and Physiology of the Liver: Position – Normal Transverse View
The left lobe is usually mostly on the right side of the body. Sometimes the lateral segments of the left lobe will cross the midline to lie leftward of the midline. The medial segment, segment IV, usually remains on the right side.

Anatomy and Physiology of the Liver: Position – Abnormal
Although unusual, some day you may come across a patient with situs inversus, which can make you look twice. In these patients, the position of the organs are reversed, with the liver on the left!

Anatomy and Physiology of the Liver: Character – Normal
The liver has the consistency of a soft, solid, malleable, organ with a “jello” – like consistency. It is highly vascular giving it a reddish brown color. Due to its size and vascular nature the liver seemed to be at the center of life itself, and it thus attained godly powers over this culture. By virtue of its malleable and vascular character it is easily lacerated with a tendency to hemorrhagic complications.
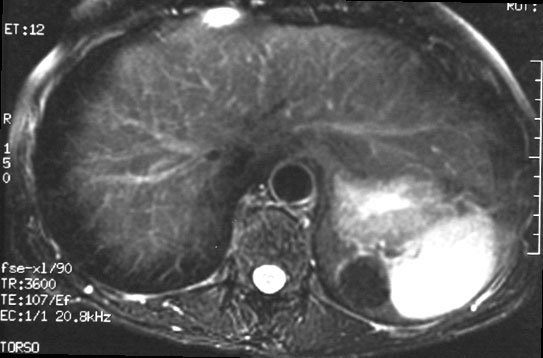
It has a soft tissue density by CT, (25-40HU – non contrast), is more echogenic than the parenchyma of the kidney by ultrasound, and is marginally brighter than the spleen on T1 weighted images, and darker than the spleen on T2 weighted images.

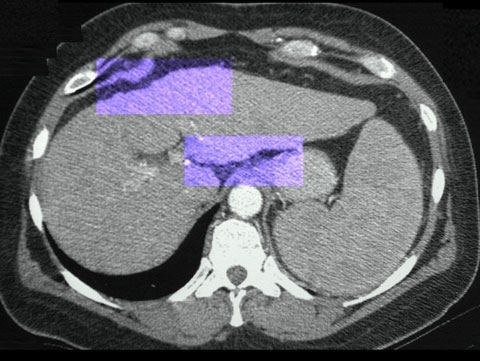
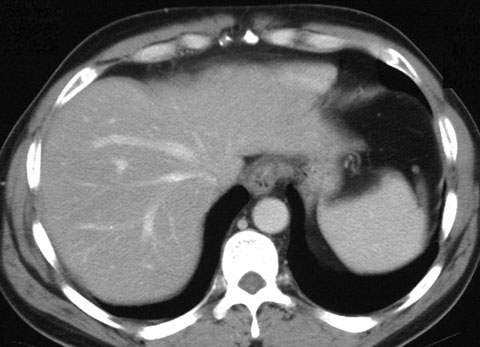
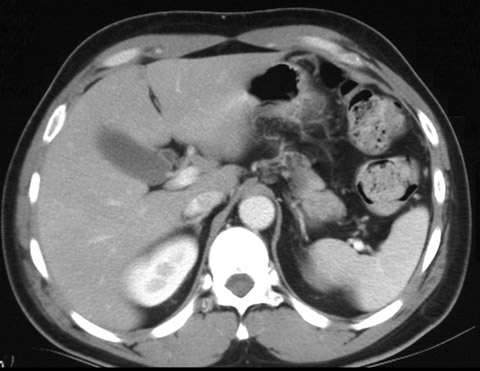
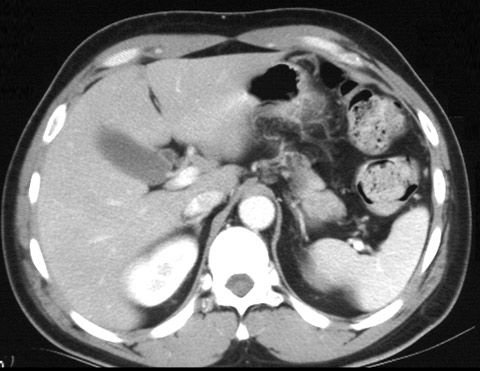
Anatomy and Physiology of the Liver: Character – Normal CT
The following is a cross sectional, portal venous phase CT. In this study, the spleen is more dense than the liver. On a non-contrast CT the liver is slightly denser than the spleen due to the glycogen content of the liver, and the water nature of the spleen.
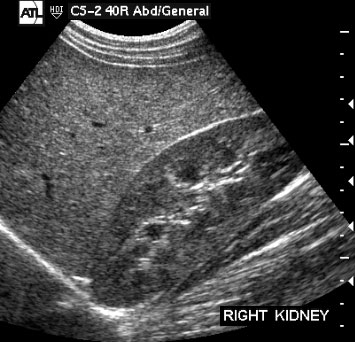
Anatomy and Physiology of the Liver: Character – Normal Ultrasound
Anatomy and Physiology of the Liver: Character – Normal MRI

Anatomy and Physiology of the Liver: Character – Abnormal – Trauma
The liver is commonly injured with blunt trauma producing a classic “bear claw” abnormality.

To try and visualize this abnormality, sometimes it is easy to visualize a large bear claw.

Anatomy and Physiology of the Liver: Character – Abnormal – Masses
In the following image, a mass can be identified in the posterior aspect of the right lobe of the liver. Notice the difference in character between the mass and the rest of the liver.

Image courtesy of Ashley Davidoff, M.D.
Additional abnormalities are seen in patients with masses in the liver. In this non-contrast cross sectional CT image the normal homogeneous soft tissue density of the liver is disturbed by a heterogeneous mass with a lower density periphery and central coarse calcification. This mass represents a metastatic carcinoma.
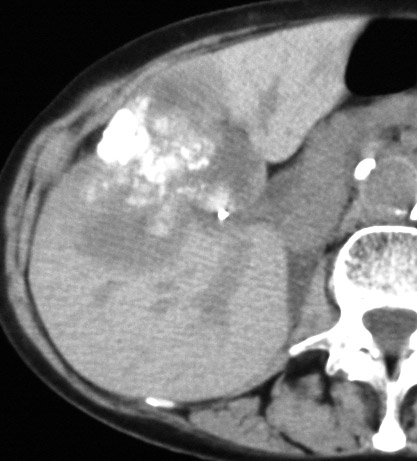
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Size – Normal
In the male, the liver weighs between 1.4 to 1.6 kg, and in the female, between 1.2 to 1.4 kg. Its greatest horizontal measurement is from 20 to 22.5 cm. Vertically, near the right surface, it measures about 15 to 17.5 cm., while its greatest antero-posterior diameter is on a level with the upper end of the right kidney, and measures 10 to 12.5 cm.
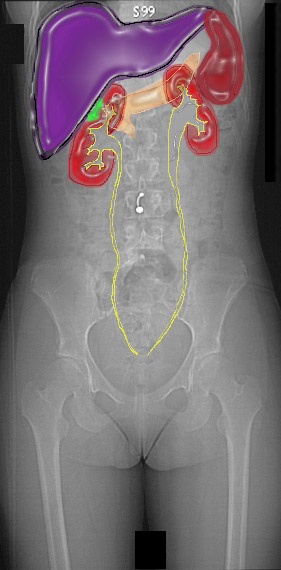
Image courtesy of Ashley Davidoff, M.D.
The linear measurements of the liver are not easy to apply in the clinical context. Sometimes the right lobe will reach all the way down to the iliac crest as a normal variant called a Riedel’s lobe. The size and shape of the left lobe is a better indicator of the size of the liver. Using planimetry and density conforming techniques, the volume and hence the size of the liver is more accurately assessed. This method is not yet automated and therefore only performed under special circumstances such as in the screening of candidates for liver transplantation. The normal volume of the liver is between 1200 and 1500 cc’s.
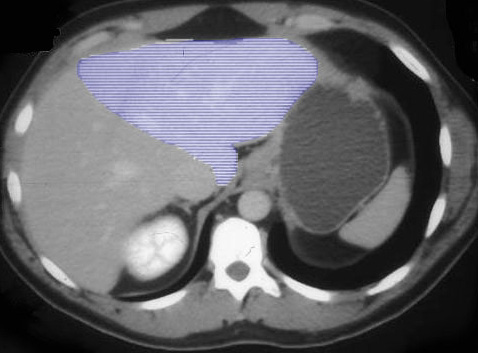
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Size – Abnormal – Acquired
A case of a larger than normal liver.

A case of a smaller than normal liver.

This liver has suffered the consequences of cirrhosis, in which liver tissue is replaced by scar tissue resulting in an overall shrinkage of the liver. Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Size – Abnormal – Congenital
This image shows a small lateral segment (II and III) of the left lobe. This condition is called congenital hypoplasia of the left lobe, implying that the person was born with this anatomic variant. It has no functional significance.
module28_25025.jpg
In this patient, part of the anterior segment (V)of the liver is missing and the colon pokes its head through the missing right lobe segment. This condition is also congenital and has no clinical significance.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Shape – Normal – Variations
We reviewed the following image when we discussed the malleability of the liver, indicating that the tendons of the diaphragm were able to indent the soft liver.
Anatomy and Physiology of the Liver: Shape – Normal – Frontal View
The liver is pyramidal in shape with its base at the left and its apex toward the right. The external surface of the liver is smooth with the apex rounded over, similar to a large mushroom cap. (see diagram below)

Image courtesy of LifeArt Lippincott, Williams & Wilkins All rights reserved
Anatomy and Physiology of the Liver: Shape – Normal – Transverse view
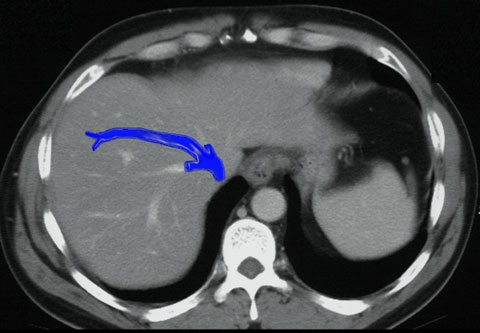
In cross sectional imaging, the surface of the liver is interrupted by normal notches and grooves. The most obvious are the grooves and fissures within the porta hepatis and the region of the entry point of the falciform ligament.
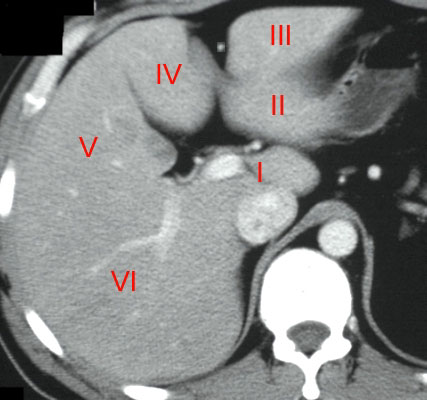
Image courtesy of Ashley Davidoff, M.D.
In the following image, the thick blue line runs to the interlobar fissure and corresponds to the border between the right and left lobes as well as the expected location of the middle hepatic vein and gallbladder axis. The thin blue line runs between the border of the anterior and posterior segments of the right lobe and corresponds to the expected location of the right hepatic vein.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Shape – Normal – Variations
We reviewed the following image when we discussed the malleability of the liver, indicating that the tendons of the diaphragm were able to indent the soft liver.

Anatomy and Physiology of the Liver: Shape – Abnormal
Compare the previous normal variant with the abnormal lobular contour of this liver. There is a distinct lack of uniformity with coarse micronodular and macronodular change. This is an example of severe cirrhosis.

Micronodular disease

Image courtesy of Ashley Davidoff, M.D.
The highlighted area in the image below reveals micronodular cirrhosis, a characteristic of alcoholic cirrhosis.
Anatomy and Physiology of the Liver: Segments of the Liver – Frontal View
There have been numerous methods of dividing and naming the parts of the liver. The earliest methods divided the liver into the left lobe, the quadrate lobe, the right lobe and the caudate lobe. Subsequently, the liver divisions were based on the venous anatomy. The right lobe was separated from the left by the middle hepatic vein. The falciform ligament divided the left lobe into the medial segment (closest to the middle hepatic vein) and the lateral segment. The right lobe was divided by the right hepatic vein into an anterior segment and a posterior segment. The next several diagrams outline the current segmental nomenclature which is still based on the distribution of the hepatic veins:
- Segment I = caudate lobe
- Segments II, III & IV = left lobe
- Segments V, VI, VII & VIII = right lobe

Image courtesy of Ashley Davidoff, M.D.
The right lobe is divided at the level of the porta hepatis into superior and inferior parts. Segments VII and VIII are superior segments and V and VI are inferior. The left lobe is divided by the falciform ligament into leftward segments II and III and rightward segment IV. Segment IVa lies above the porta hepatis and segment IVb below.
Anatomy and Physiology of the Liver: Segments of the Liver – Transverse View – Superior Segments
Starting from a cross section of the liver just below the diaphragm, we can identify the superior segments of the liver.
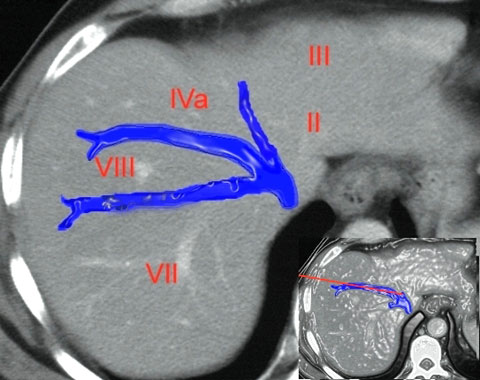
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Segments of the Liver – Transverse View – Inferior Segments
The following image reveals the cross sectional segmental pattern at the level of the porta hepatis.
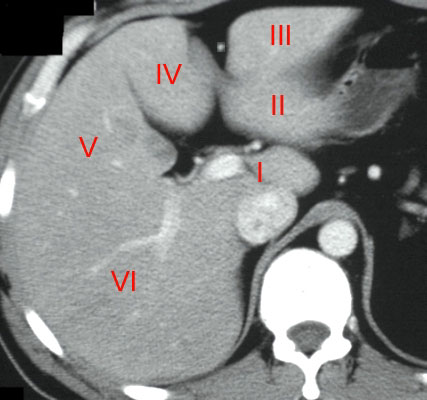
Image courtesy of Ashley Davidoff, M.D.
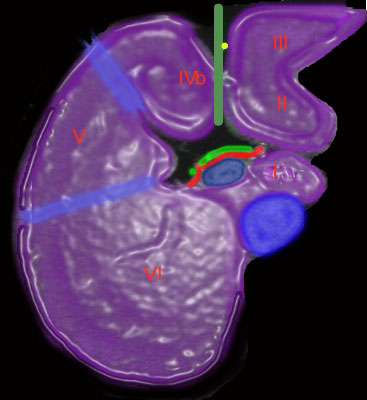
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: The Caudate Lobe – Segment I
The caudate lobe (also known as segment I) is positioned medial to the right lobe and posterior to the left lobe. It is bounded inferiorly by the porta hepatis, posteriorly by the inferior vena cava, anteriorly by the portal vein and more superiorly and anteriorly by the ductus venosus. The caudate lobe is a rather curious structure, situated almost as an appendage to the liver. A unique characteristic is that its venous drainage flows directly and independently to the inferior vena cava below the diaphragm. As previously stated, it belongs neither to the left nor the right lobe, and it is considered as an “independent” segment.
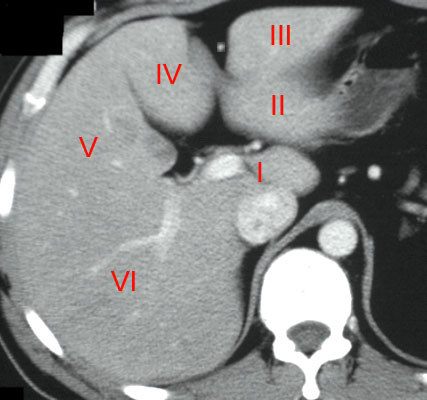
Image courtesy of Ashley Davidoff, M.D.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: The Caudate Lobe – Have you seen the woodpecker?
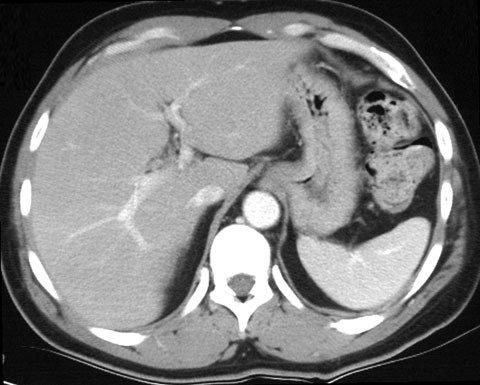
Image courtesy of Ashley Davidoff, M.D.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: The Liver Lobule

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: The Liver Lobule to Central Vein Connection

Image courtesy of Ashley Davidoff, M.D.
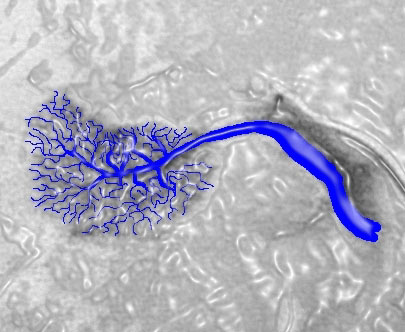
Image courtesy of Ashley Davidoff, M.D.
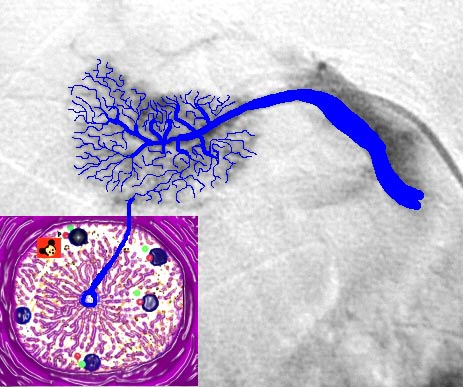
Image courtesy of Ashley Davidoff, M.D.
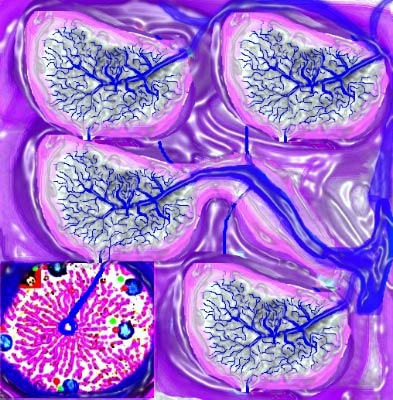
Anatomy and Physiology of the Liver: The Liver Lobule Conglomerate – Power in Numbers

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: The Porta Hepatis – Gateway to the Liver
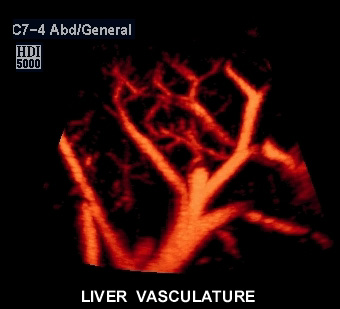
A unique feature of the liver is that it is nourished by a dual blood supply: 75% via the portal vein, and the remainder from the hepatic artery. Blood is drained from the liver by the hepatic veins.

Image courtesy of Ashley Davidoff, M.D.
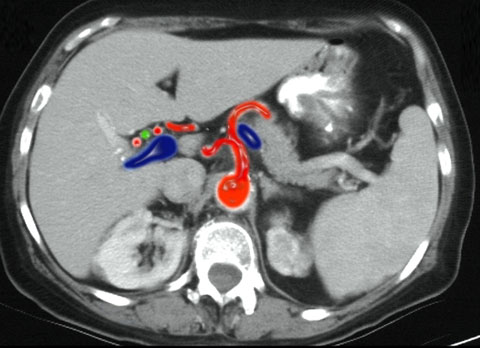
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: The Porta Hepatis – Where is Mickey Mouse?
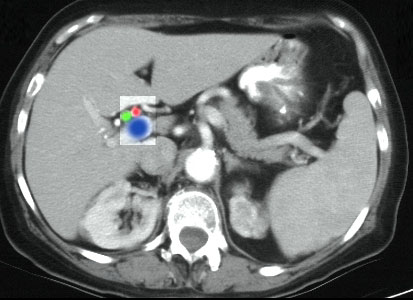
Image courtesy of Ashley Davidoff, M.D.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Hepatic Artery
The hepatic artery originates from the celiac axis, which is a short thick trunk extending from the the aorta just below the diaphragm. (the other two branches of the celiac are the left gastric and the splenic) The hepatic artery enters the liver at the porta, along with the portal vein and hepatic duct, and divides into two main branches that supply the right and left lobes respectively. The liver depends on the hepatic artery for only 25-30% of its blood flow.
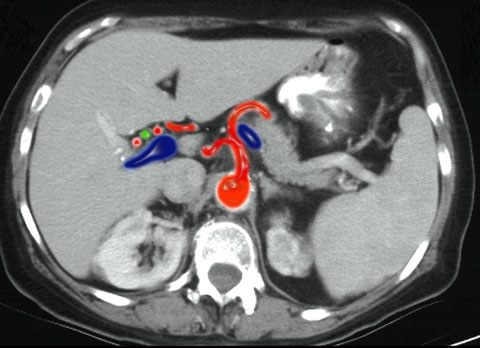
Image courtesy of Ashley Davidoff, M.D.

Image courtesy of Ashley Davidoff, M.D.
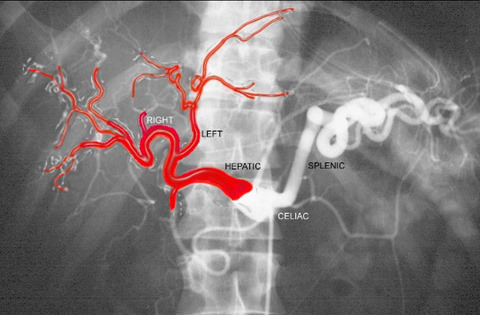
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Portal Vein
The portal system includes all the veins, which drain the blood from the abdominal part of the digestive tube, including the pancreas, spleen, and gall-bladder. The blood and other products of the digestive process are conveyed to the liver by the portal vein. The blood enters the sinusoids, which are the unique capillary system of the liver. The end point of the sinusoid is the central venule. Blood is transferred into the hepatic veins, and eventually to the inferior vena cava (IVC). The portal vein is responsible for 75-80% of the blood flow to the liver. The hepatic artery transports oxygenated blood, while the portal vein transports metabolic products to the liver.
Image courtesy of Ashley Davidoff, M.D.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Sinusoids of the Liver
Once in the liver, the portal vein branches into the main left and right branches and after several divisions, end in capillary-like vessels termed sinusoids.

Image courtesy of Ashley Davidoff, M.D.
At the sinusoids, metabolic exchange occurs with the liver cells -the hepatocytes. The products of digestion in the portal vein are exported into the liver cells and processed nutrients are transferred into hepatic venules. The end point of the sinusoids is the central hepatic venule. The venules from each lobule join to form segmental hepatic veins and eventually blood is transferred from the hepatic veins to the inferior vena cava.
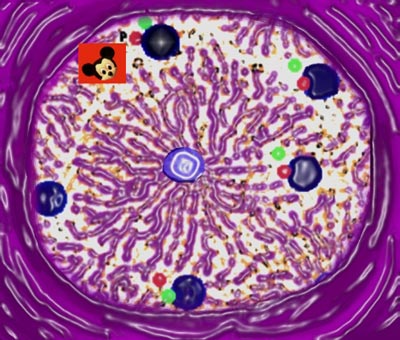
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Sinusoids to Central Veins – The End of the Blood Line
The hepatic veins originate from the sinusoids and convey blood from the liver to the vena cava. Hepatic veins tend to be open and solitary, allowing them to be distinguished from the branches of the portal vein, which are more or less collapsed and always accompanied by an artery and duct.

Image courtesy of Ashley Davidoff, M.D.
module28_13009%20W17.jpg
There are a multiplicity of lobules, each with a central vein and each delivering the “goods” to venules, which collectively join to form the hepatic veins and then into the IVC. Destination? The heart, from where it will be distributed to the body wide system.
Image courtesy of Ashley Davidoff, M.D.
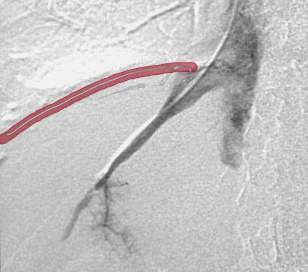
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Hepatic Veins to the IVC – Have you seen the rabbit?
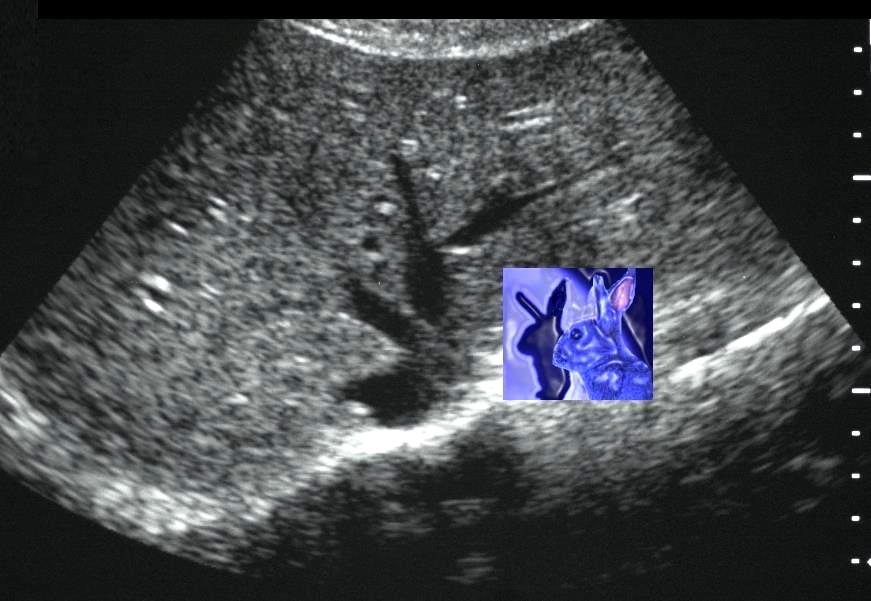
Image courtesy of Ashley Davidoff, M.D.
This coronal view of the abdominal cavity shows the confluence of the 3 major hepatic veins as they form the IVC at the diaphragm.
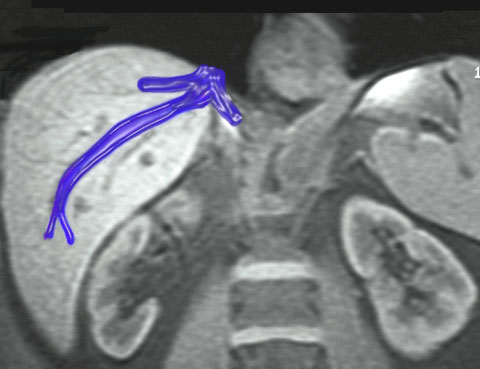
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Bile Ducts
Bile ducts accompany the hepatic artery and the portal vein throughout the liver. Bile, which is created in the hepatocytes, is secreted and collected after passing through the bile capillaries by the bile ducts, which join to form two large ducts that unite to form the hepatic duct. The bile is either carried to the gallbladder by the cystic duct or transported directly into the duodenum by the common bile duct.

Image courtesy of Ashley Davidoff, M.D.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Bile Ducts, Liver Lobule, and Duodenum – What are the connections?
The liver cells are accompanied by bile canaliculi (small bile channels) which are situated between neighboring liver cells. These become confluent at the periphery of the liver lobule and form the bile ductule member of the portal triad.
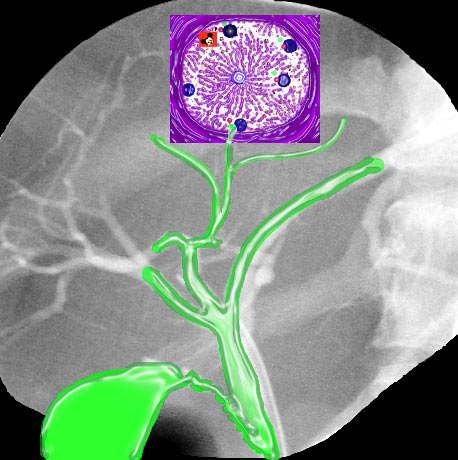
Image courtesy of Ashley Davidoff, M.D.
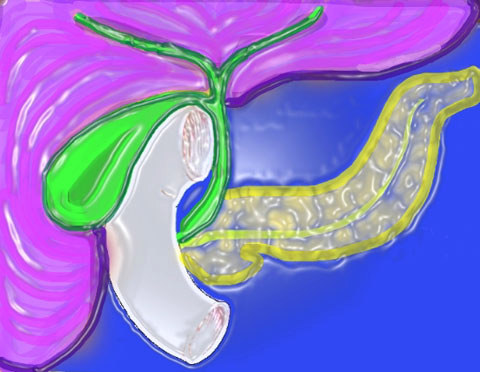
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Bile Ducts – Abnormal – Obstruction
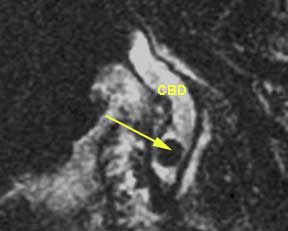
Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Lymphatic Drainage – Sinusoids to Porta
The liver represents the largest single source of lymph in the body, producing nearly 20% of overall total volume. Most hepatic lymphatics leave the liver at the porta hepatis and drain into hepatic nodes along the hepatic artery. Lymph is a clear fluid that is collected from the various organs and tissues of the body, flows through the lymphatic vessels, and eventually rejoins the venous circulation.
The lymphatic fluid is collected by small side channels called the spaces of Disse, which run along and in parallel with the sinusoids. These become confluent and form small lymphatic channels that surround the portal vessels – particularly the arterioles and portal vein.
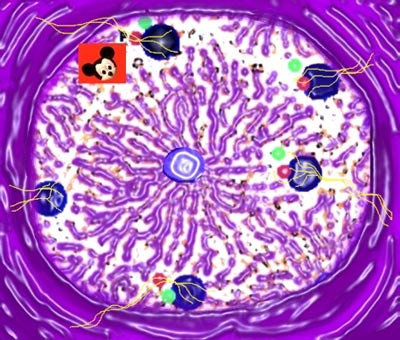
Image courtesy of Ashley Davidoff, M.D.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Lymphatic Drainage – Portal Lymph Nodes

Image courtesy of Ashley Davidoff, M.D.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: Lymphatic Drainage – Companion to the Hepatic Artery
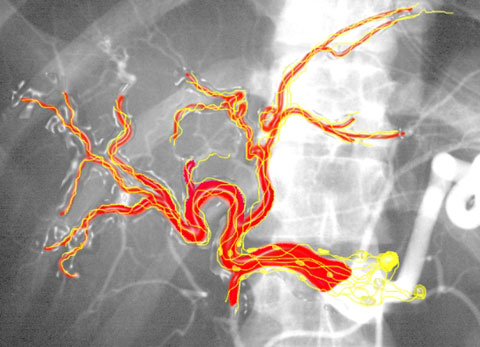
Image courtesy of Ashley Davidoff, M.D.

Image courtesy of Ashley Davidoff, M.D.
Anatomy and Physiology of the Liver: The Capsule – Wrapping it up
The liver is fully invested by a serous and a fibrous coat. The serous coat derives from the peritoneum, and covers the greater part of the surface of the organ. The fibrous coat lies beneath the serous coat, and covers the entire surface of the organ. It is difficult to see, except in cases where the serous coat is deficient.
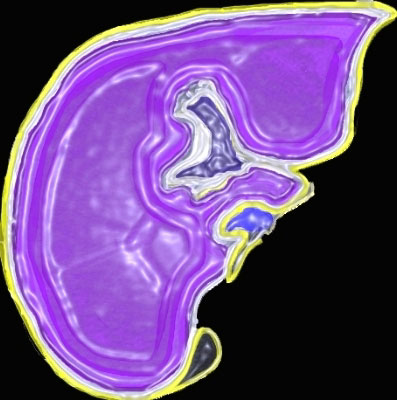
Image courtesy of Ashley Davidoff, M.D.
Embryology – Where did this all come from?
The transverse septum arises at an embryonic junctional site, where the ectoderm of the amnion meets the endoderm of the yolk sac. The junctional region internally is where the foregut meets the midgut. The mesenchymal structure of the transverse septum provides a support within which both blood vessels and the liver begin to form. The liver develops as the hepatic diverticulum from the endodermal lining of the most distal portion of the foregut during the 3rd and 4th weeks of gestation, and the liver grows rapidly from this point. The transverse septum then differentiates to form the hepatic diverticulum and the hepatic primordium. These two structures together will go on to form different components of the mature liver and gall bladder. The rapidly developing liver forms a visible surface bulge on the embryo directly under the heart bulge. Bile production begins in the 12th week, and excretion of bile into the duodenum by the 16th week. The liver is fully developed by the third trimester.
CT Imaging of the Liver: Overview
Dynamic bolus contrast-enhanced spiral CT can provide high quality images enabling the visualization of anatomic detail. CT provides good spatial and contrast resolution giving an excellent global view of the liver and abdominal cavity. With thinner sections, 3D reconstructions can be obtained providing in-depth information about the portal venous and arterial systems, as well as the liver parenchyma itself. Taking advantage of the liver’s dual blood supply, focal lesions, especially tumors, are well demonstrated with mutli-phase scanning techniques. Accurate segmental localization is key to surgical planning. Since the acquisition of images is operator independent and is not affected by patient habitus, CT can be more consistent and widely applied than other modalities. Normal liver density on CT (25-35 HU) is equal or slightly greater than spleen with or without contrast.
MR Imaging of the Liver: Overview
Although once limited by motion artifacts, the role of MRI in liver imaging has been increasing due to faster imaging techniques. MRI provides great detail about the character of liver tissue, specifically in identifying abnormalities in the soft tissue structure. MRI also allows for image acquisition in the axial as well as coronal and sagittal planes, which can provide better image quality without 3D reconstruction. MRI also provides good contrast in tissues with water and fat. However, MRI does not provide optimal visualization of calcification. Spatial resolution of MRI in the abdomen is generally inferior to CT due to motion and the nature of the abdominal tissues. This is not the case with the brain and the musculoskeletal system where MRI shows superior spatial resolution. On T1-weighted images, a normal liver is of slightly higher signal intensity than the spleen. On T2-weighted images, the liver is slightly less than the spleen.


US Imaging of the Liver: Overview
Ultrasound is a good screening technique for patients who have abdominal symptoms and suspected focal or diffuse liver disease. It also has the advantage of easy identification of dilated bile ducts, cysts, or tumors in the liver. Visualization of the gallbladder and porta hepatis with ultrasound is generally superior to other modalities. Accuracy, however, is decreased in obese patients and is operator dependent. In addition, ultrasound allows only certain portions of the liver to be visualized at any given moment and in any given plane due to a limited scanning field. On the other hand, a significant advantage is its real time capability. By using color-flow and spectral doppler techniques, hepatic vessels and tumor vascularity can be assessed dynamically. More recently, contrast agents have been used for improved contrast resolution and characterization of disease. US is also the study of choice for non-invasive imaging of the bile ducts. The normal liver is homogeneous and slightly hyperechoic to the kidney and hypoechoic to the spleen.

Image courtesy of Philips Healthcare
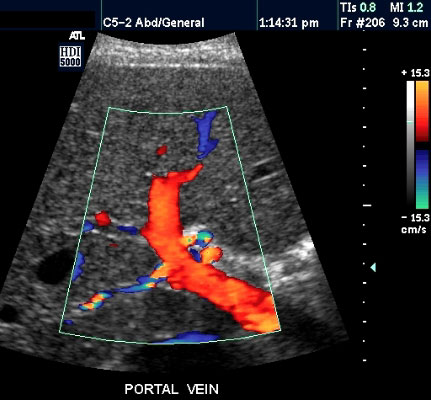
Image courtesy of Philips Healthcare
Images courtesy of Philips Healthcare
Conclusion: Overview
As the largest gland in the body, and second only to the skin as the largest organ in the body, the liver is a fairly easy target for all imaging modalities. It is remarkable, however, how the strength of each modality plays a role in defining anatomy and pathology in any given patient. It is also a continuing source of fascination to identify the differences between each liver, since no two organs are exactly the same. The variations in size, shape, position and character, as well as the multifaceted manifestations of disease keep us interested, focused, and stimulated. The technology continues to advance. By adding contrast and harmonic technology to US studies, multidetector scanning to CT, and advancing the speed and complexity of pulse sequences to MRI, the resolution of structures continue to unfold and improve. Additional imaging modalities, such as positron emission tomography (PET), may also lead to improved characterization, particularly in oncological imaging.