Introduction
The gallbladder (vesica fellea) is a pear-shaped, bulbous pouch or sac which lies on the visceral surface of the liver. It is part of the biliary and gastrointestinal systems.
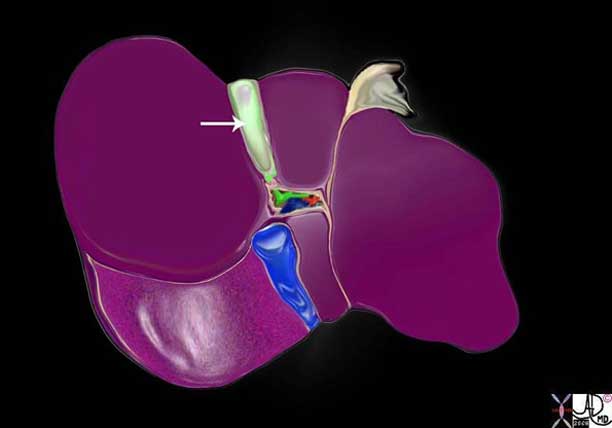
Structurally it is characterized by its pyriform shape and location between the right and left lobes of the liver. It is connected to the biliary tree which drains bile from the liver and transports it to the duodenum.
The function of the gallbladder is to store and concentrate bile until it is needed for fat digestion. Flow of bile into the duodenum is controlled by the sphincter of Oddi, which when relaxed will allow bile to pass into the duodenum and when closed will passively direct bile to flow into the gallbladder.
Common diseases include cholelithiasis, acute cholecystitis, acalculous cholecystitis, and the hyperplastic cholecystoses.
Right upper quadrant pain is the most common clinical presentation of gallbladder disease, while ultrasound, HIDA (hepatic dimethyl iminodiacetic acid, a nuclear medicine radiotracer) scan and CT (computed tomography) scan are the most commonly used diagnostic studies.
Treatment is usually surgical and percutaneous cholecystostomy is needed in certain circumstances.
Gall: is the Middle English word for bile. Bile was an important element in ancient Greek philosophy and medicine and subsequently used extensively in literature – usually with a negative connotation.
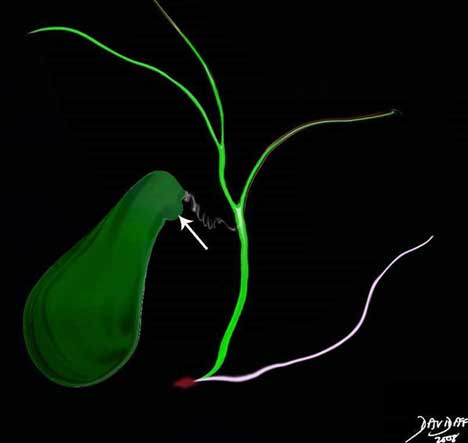
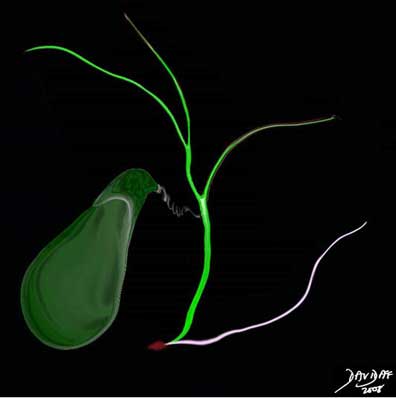
The cystic duct is the duct that connects the gallbladder to the common bile duct. The common bile duct (CBD) is housed in the ampulla (light brown) with the pancreatic duct (pink) and their flow is controlled by the sphincter of Oddi which is also housed in the ampulla.
Courtesy of: Ashley Davidoff, M.D
Basic Principles
The gallbladder is a distinct biological unit that through its links and connections, contributes to the well-being of the body at large. It demonstrates both independence from and dependence on other systems, it changes with time, occupies space and is subject to mechanical and chemical forces. It is commonly without disorder, though in Western cultures, high fat diets contribute to gallstone formation and associated diseases.
Structure
The structure of the gallbladder appears fairly simple at first but complexity unfolds as we start to examine the structure in detail. The size, shape, and position of the gallbladder in combination with its connections create a unique structure that defines it in form and function.

The gallbladder has to store and concentrate bile and this occurs in the same chamber. The more capacious fundus lies inferiorly so that the oldest and most concentrated bile should be positioned within the fundus with the patient in the standing position
Courtesy of: Ashley Davidoff, M.D
The histology of the gallbladder is also unique. It does not conform to the typical histology of the rest of the gastrointestinal tract; the mucosa is thrown into irregular folds and pits, there is no submucosa, and the muscularis externa is relatively incomplete containing both prominent connective tissue and elastic elements. The peritoneal covering on the free wall side results in a smooth serosa and the lack of peritoneal covering on the liver side results in a coarse adventitia. This latter surface acts as the “hilum” to the gallbladder since it houses blood vessels and lymphatics to and from the liver to the gallbladder.
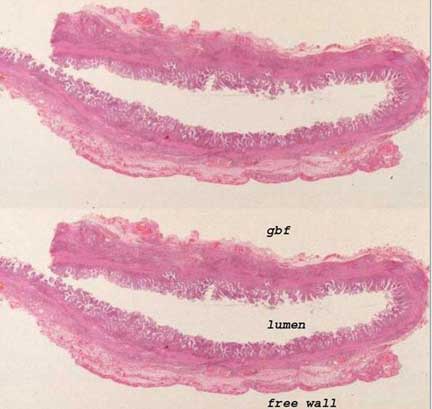
The upper and lower images represent whole mounts of a normal gallbladder. The upper unlabelled image shows three relatively indistinct layers. The irregular luminal surface shows the folds of the mucosa under which the invisible lamina propria runs. The layer below is the muscularis which is a poorly defined layer that consists of smooth muscle and connective tissue. The outer layer on the free wall is covered by peritoneum and hence it is called a serosa. The inner layer lacks a serosal covering and hence it is called an adventitia.
Image courtesy of: Ashley Davidoff, M.D.
gbf = gallbladder fossa
Structural Principles
Structural principles are grounded in the notion that biological units have characteristic and defining size, shape position and character, and are connected via neurovascular bundles, ducts and lymphatics to the system at large.
The size of the gallbladder allows it to store only 50-70cc of bile while the liver produces and delivers 500-1000cc of bile per day. If we approach the gallbladder with simple minded mathematics we are puzzled, since if it empties its contents at three meals a day, it would empty a total of 210cc per day when the juice gates of Oddi are open. One would have expected the gallbladder volume using the “three meals three empties” per day concept to have been in the order of 200cc, for example, three times its volume of about 65cc. Where does the remaining volume of approximately 700cc of bile go? We will attempt to unravel this puzzle as the module progresses.
The pear-shaped form and position of the gallbladder has rational design. The fundus with the largest diameter and the body with the most volume are relatively inferior so that they act as a storage dump when the patient is in the upright position. Additionally, they act as a pump that has to process the bile for three major deliveries per day. Unlike the heart, it has the additional function to concentrate its product and therefore it has to separate bile that has already been processed and new bile that is freshly delivered from the liver. “Old” concentrated bile is stored in the fundus and “new? bile is located in the infundibulum. As we progress with this module we will try to expand this concept.
The character of the gallbladder is based in its wall and its contents. As a musculomembranous sac it has been designed with a three-layered wall that has muscular elastic and absorptive properties. The lumen houses bile which is a homogeneous, relatively clear, and limpid fluid. Bile fresh from the liver has a specific gravity (SG) that ranges between 1.010 – 1.030 being slightly greater than water and after it has been concentrated by the gallbladder the SG is usually in the 1.040 range.
The connections of the gallbladder to the rest of the gastrointestinal tract are via the cystic duct which plugs into the hepatic duct to form the common bile duct. Its blood supply is via the cystic artery, venous drainage via the cystic veins, and lymphatics via the hepatic system. Parasympathetic and sympathetic systems connect it to the autonomic system, while the hormonal control is via intestinal polypeptides and cholecystokinin (CCK).
The parts of the gallbladder include the fundus, body, neck, and cystic duct. It has a serous capsule on its free wall.
Histology

This image shows four layers of tissue characteristic of the histology of many gastrointestinal (GI) structures. A simple columnar epithelium is the the inner cellular layer of the mucosa and it is supported by a muscularis mucosa (pink). The submucosa (yellow) consists of loose connective tissue with blood vessels, lymphatics, and macrophages. The muscularis (red) is next and is followed by the outer covering (white), which may be a serosa or adventitia. The histology of the gallbladder does not conform exactly. It does have a simple columnar epithelium, lacks a muscularis mucosa, but has a lamina propria as part of the mucosa that houses blood vessels and lymphatics. This layer is followed by an ill-defined muscular layer that is intermingled with collagen and elastic tissue and is covered on its free surface by a serosa and liver surface by an adventitia.
Histology: Histological Makeup of the Gallbladder Wall
The gallbladder lacks a distinct submucosa but also lacks a muscular layer in the mucosa (muscularis mucosa). The lamina propria functions as a submucosa to house blood vessels and lymphatics but it is tucked into the folds of the gallbladder and is rapidly within a short distance from the folds followed by the muscularis layer.
There is also a difference in the wall of the gallbladder that abuts the liver and the wall that abuts the peritoneal cavity.
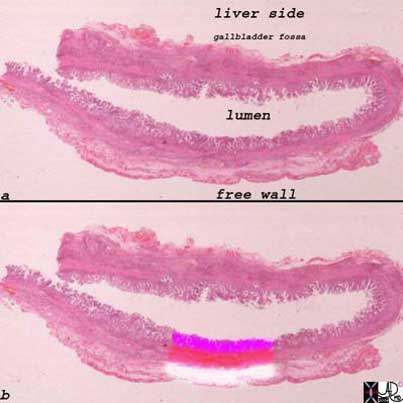
The upper and lower images represent whole mounts of a normal gallbladder. The upper image shows the liver surface of the gallbladder and the region of the gallbladder fossa, the lumen, and the free wall that is covered by the peritoneum.
The lower image shows the three basic histological layers. The pink mucosa, the red muscularis, and the white outer serosa.
Images courtesy of: Ashley Davidoff, M.D.
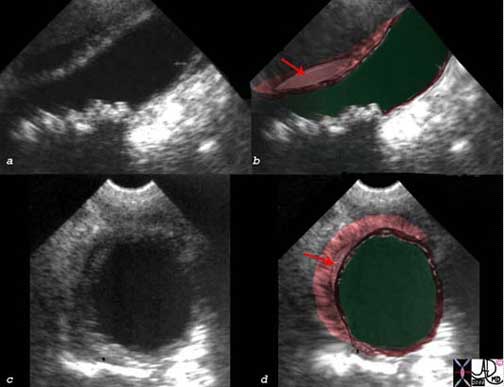
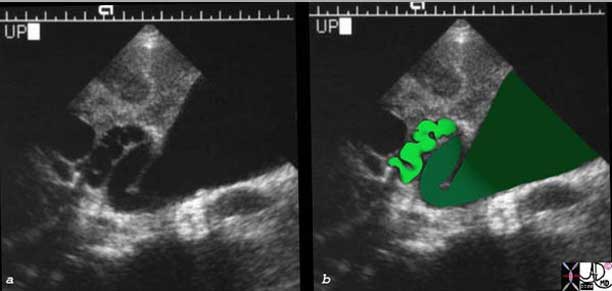
Ultrasound examination of the gallbladder is performed in the fasting state and it is therefore distended. When the gallbladder is distended, the three layers cannot be distinguished. When the gallbladder is contracted, three distinct layers representing echogenic mucosa, hypoechoic muscularis and echogenic serosa adventitia become obvious.
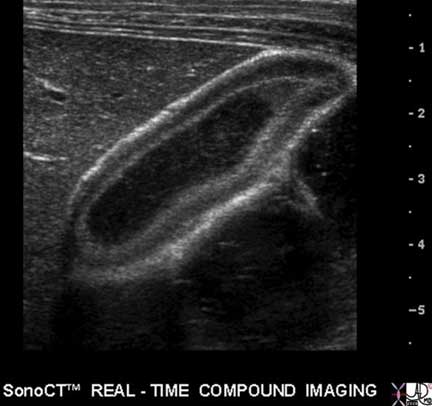
In this ultrasound image of the contracted gallbladder, three distinct layers are obvious. The inner echogenic mucosa abuts the lumen, the hypoechoic muscular middle layer is the thickest, while the outer layer is most echogenic since it contains relatively large amounts of collagen.
Images courtesy of: Ashley Davidoff, M.D.
Histology: Mucosa
The folds of the mucosa that project toward the lumen are frond-like in form and are quite irregular and non-uniform when viewed in comparison to the folds of the small bowel, for example. The mucosa consists of a tall, columnar epithelium with basal nuclei and pale cytoplasm (due to sulfomucins) and lack goblet cells. In the neck, however, mucus secreting goblet cells are found. The mucosal layer secretes mucous to protect the gallbladder from the relatively alkaline bile it stores (pH 7.6 to 8.6).

This is a low power photomicrograph of the wall of a normal gallbladder. Note the delicate finger-like projections (fronds) of the mucosa. The lamina propria (submucosa functional equivalent) is tucked into the folds. Just under the folds is the muscularis mucosa, seen here as loosely connected bundles of smooth muscle. Deep to that is some connective tissue of the gallbladder bed. On its peritoneal aspect the gallbladder is covered only by a single layer of mesothelium. Thus, the gallbladder has a much simpler wall structure than the GI tract. The thickness is only about 2 mm. The implications for penetration of stones, spread of inflammation, and perforation are obvious.
Courtesy of: Barbara Banner, MD
Deep to the epithelium, the lamina propria contains abundant capillaries and larger blood vessels. The epithelial layer and the lamina propria comprise the mucosa.

Courtesy of: Barbara Banner, MD
Next, there is a smooth muscle layer called the muscularis externa appearing as irregular layers of smooth muscle, connective tissue and elastic tissue. The inner components align longitudinally and the outer align diagonally so that they spiral around the gallbladder.
The peritoneum covers the gallbladder on its free surface and so in that location a serosa is formed. There is no peritoneum in the gallbladder fossa and so in this region it is called an adventitia.
In 10% of people, aberrant vestigial ducts of Luschka project from the liver into the wall of the gallbladder without connecting to the gallbladder lumen. There are also larger accessory ducts that communicate with the cystic or hepatic ducts.
Histology: Rokitansky-Aschoff Sinuses
The Rokitansky-Aschoff sinuses are diverticula or pockets in the wall of the gallbladder that may be microscopic or macroscopic. They are thought to be an acquired abnormality caused by increased intraluminal pressure resulting in mechanical stresses on a mucosa and outward bulging of the mucosa.
Structurally, they are characterized as outpouchings of the gallbladder mucosa extending into and sometimes beyond the gallbladder muscle layer. They are not of themselves considered abnormal, but they seem be associated with elevated pressures in the gallbladder possibly as a result of normal and hypercontractile states and are also associated with chronic cholecystitis and cholelithiasis which may have similar pathogenetic mechanisms.
The diverticula do not cause functional impairment.
No clinical impairment is therefore implicated but they are associated with the hyperplastic cholecystoses (adenomyomatosis and cholesterolosis) as well as gallstone disease. Sometimes, calcific concretions accumulate within the diverticulum.
When the diverticula are large, the diagnosis is usually accomplished by ultrasound and less commonly by CT or Magnetic Resonance Imaging (MRI).
Treatment is only considered when a patient presents with right upper quadrant pain and no other cause can be found. In some patients symptomatic relief has been accomplished with cholecystectomy.
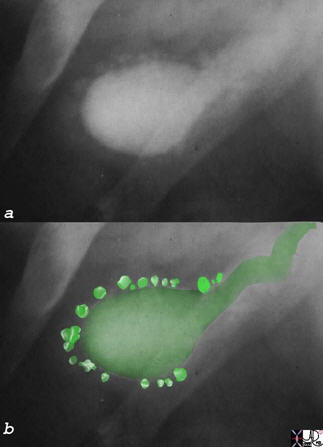
The old fashioned oral cholecystogram best typifies the deep Rokitansky Aschoff sinuses, as characterized by deep diverticuli, which in this case are scattered around the gallbladder like a pearl necklace.
Courtesy of: Ashley Davidoff, M.D

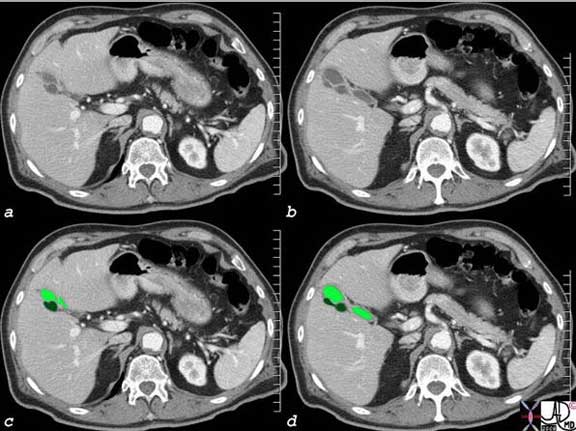
The thickening of the wall noted in the above CT is non specific. It is stated to occur in the “subserosal” layer, presumably implicating the loose muscular layer but probably also implicating the loose tissue of the serosal/adventitial layers and the lamina propria. The enhancing inner mucosa is seen in (c) as a white pencil thin line. Below the mucosa and colored in red (image (b & d) the blood vessels in the lamina propria are noted. The edema (gray wall (c) and (d) is noted between the vessels and liver on the right and the vessels and the stomach on the left. Thus, the edema probably lies in both the muscularis layer and in the outer serosal/adventitial layer.
Images courtesy of: Ashley Davidoff, M.D.
Size of the Gallbladder
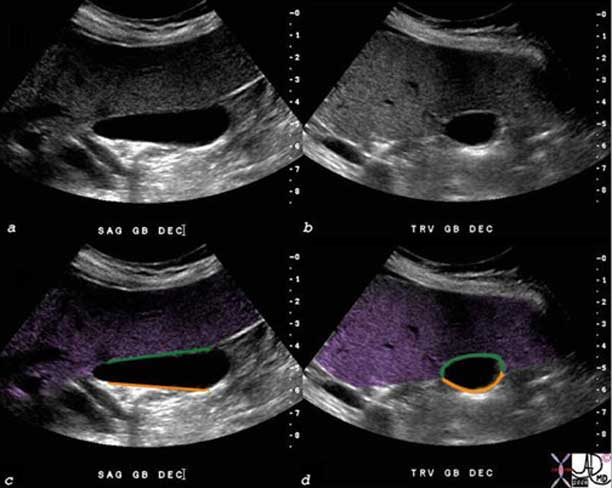
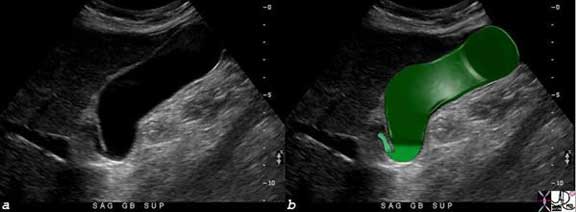
The normal gallbladder in the fasting state contains about 50-70ml of bile and measures 8-10cm in length, by 3-4cm in diameter using ultrasound. Because of its ellipsoid shape the approximation for gallbladder volume can be estimated by using the formula of length X width X depth X 0.5cm.
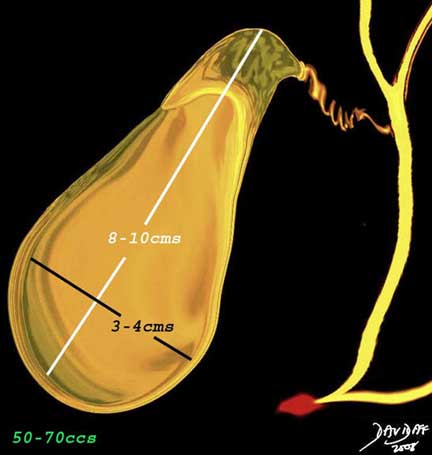
The normal gallbladder in the fasting state measures 8-10cm in longitudinal view, by 3-4cm in the transverse dimension and has a volume of 50-70cc.
Images courtesy of: Ashley Davidoff, M.D.

In this instance it measures 10 by 3.5cm.
The wall is normally 2-3mm thick in the fasting state. It is only about 1mm thick in the neonate.

The wall on this sagittal view of the gallbladder measures 1.00mm in this instance. From a technical view it is best measured at the liver surface as shown above.
Images courtesy of: Ashley Davidoff, M.D.
The gallbladder contracts following a fatty meal. Patients are therefore required to fast for 6 to 8 hours before the examination, for optimal evaluation. Examples of contracted gallbladders are shown below.

Shown are two Ultrasound images on a patient who has just had a fatty meal. The gallbladder, in this instance, measures 6.5cm by 1.3cm.
Courtesy Ashley Davidoff MD
The fundus has the largest diameter, the body the largest volume while the neck is the smallest part of the gallbladder proper.
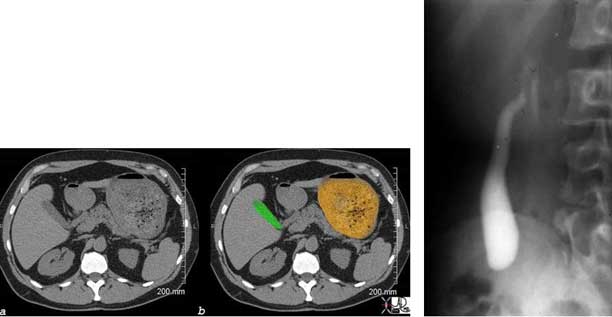
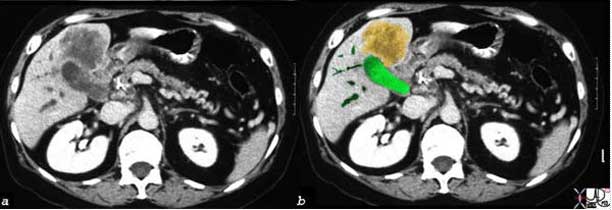
Image (a) and (b) show a transverse CT image revealing a contracted gallbladder with a stomach filled with food (orange). The oral cholecystogram shows a contracted gallbladder following a fatty meal.
Images courtesy of: Ashley Davidoff, M.D.
Size: Applied Biology
The size of the gallbladder is one of the more important determinants of the presence of disease in the evaluation of gallbladder.
The size of the gallbladder cannot be assessed by clinical examination since the gallbladder lies under the liver and only a small portion of the fundus is exposed. Therefore, under normal circumstances it cannot be palpated and is only palpable when it is significantly enlarged. For this reason, assessment of the size of the gallbladder requires the use of an imaging technique. This is best accomplished by ultrasound, since the true long axis and short axis can be defined by the ultrasonographer who is able to angle the transducer along the appropriate axis. The gallbladder is normally positioned at an angle that is off the horizontal, sagittal and coronal planes. The fundus is located relatively inferiorly, while the neck is positioned more medially and superiorly. Thus, by the nature of the transverse imaging of CT and usual orthogonal imaging of MRI, the true axis is not routinely defined by these methods. Although nuclear imaging can also assess the size of the gallbladder accurately, other factors such as wall thickness and probe tenderness cannot be evaluated. Thus, when assessment of the size of the gallbladder and associated features of wall thickness and probe tenderness is required, ultrasound becomes the procedure of choice.
From a practical and clinical standpoint, the clinician who suspects an enlarged gallbladder is really asking whether there is increased pressure in the gallbladder. The imaging technology uses size as an indirect measure of the intraluminal pressure since we would otherwise have to use invasive techniques to assess the pressure directly. Since there are situations where the gallbladder loses its tone (atonic or hypotonic gallbladder as a result of the aging process or diabetes) it can enlarge without an increase in pressure. On the other hand, there are situations when the gallbladder wall is fibrotic (chronic cholecystitis) and this results in a small contracted gallbladder which cannot dilate when the luminal pressure rises.
Multiple factors, therefore, have to be taken into consideration when assessing the size of the gallbladder.
Size: The Large Gallbladder
The large gallbladder is defined as a gallbladder that exceeds 4cm in the short axis.
The shape of the gallbladder becomes more rotund when it is enlarged. The gallbladder is normally ovoid in shape in the transverse plane.
Gallbladder enlargement is not necessarily pathological. In asymptomatic patients, enlargement can occur as a variant in people with asthenic builds, in older patients and in diabetics (atonic). It is suggestive of cholestasis in patients who are on a prolonged fast and those on hyperalimentation. An atonic or hypotonic ileus of the gallbladder is seen in patients following abdominal surgery, patients with gastrointestinal (GI) infections, hepatitis, pancreatitis, and bowel ileus, all of which can cause asymptomatic enlargement. In these patients there is no gallbladder tenderness, the wall is normal, but there may be thickened bile (sludge) in the lumen.
Pathological gallbladder enlargement is most often caused by mechanical abnormalities and usually by a stone that is impacted in the infundibulum, or cystic duct. If the obstruction results in inflammation, then the condition called acute cholecystitis results.
Acute Cholecystitis
In this artistic rendition, a small stone has become impacted in the neck of the gallbladder, resulting in obstruction and acute cholecystitis.

In this artistic rendition, a small stone has become impacted in the neck of the gallbladder, resulting in obstruction and acute cholecystitis.
Images courtesy of: Ashley Davidoff, M.D.
The stone can also lodge in the common bile duct (CBD) resulting in an enlarged gallbladder. In this instance, the patient presents with obstruction and if inflammation ensues, cholangitis results.
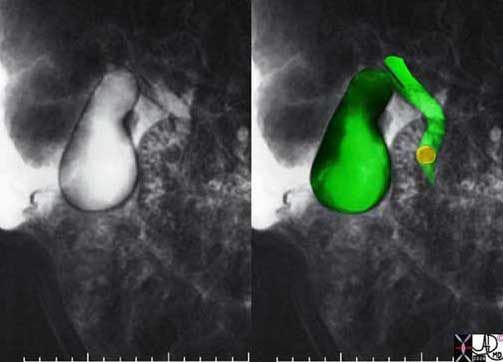
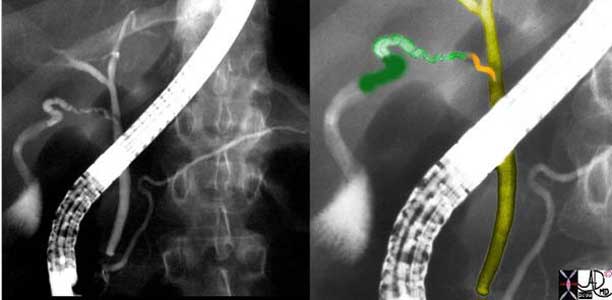
The MRCP performed using T2-weighted Fast Spin Echo (FSE) technique shows a common bile duct (CBD) stone associated with dilatation of the CBD, cystic duct and the gallbladder.
Images courtesy of: Ashley Davidoff, M.D.
Another common cause of an enlarged gallbladder is acalculous cholecystitis. It is an advanced form of cholestasis where inflammatory changes supervene as a complication. Patients who have a prolonged course in the intensive care unit (ICU) become cholestatic and with increased distension, inflammation ensues.

Acalculous cholecystitis is an inflammatory condition of the gallbladder that is caused by prolonged fasting. Absent stimulation by CCK is most commonly seen in patients in the ICU setting. The gallbladder enlarges, becomes rounded and the bile becomes black and thickened (sludge). The drawing on the left depicts the condition with a distended gallbladder, a thick slurry of bile, and inflammation in the walls. The photograph on the right is bile taken from a patient with acalculous cholecystitis. The bile which is usually a pale orange becomes as “black as crankcase oil”.
Courtesy Ashley Davidoff MD
Obstruction by pancreatic cancer, or less commonly by an ampullary tumor will result in an enlarged gallbladder as well. This results in a Courvoisier sign which is a palpable gallbladder in the presence of painless jaundice.

The patient presented with painless jaundice and a palpable gallbladder. (Courvoisier sign) The epicenter of the collage of images is in image c where the arrow points to a mass in the head of the pancreas that has caused obstruction of the pancreatic duct (seen upstream from the mass in (c)), gallbladder distension (a) and bile duct dilatation (a, b, & d). A percutaneous biliary drainage catheter has traversed the obstruction and is in the duodenum that will allow for decompression(d).
Images courtesy of: Ashley Davidoff, M.D.
Size: The Small Gallbladder
The small gallbladder usually is of lesser clinical significance than the enlarged gallbladder. The most common cause of a small gallbladder is recent ingestion of a meal. In chronic cholecystitis, the development of fibrosis results in a chronically contracted gallbladder. In HIV cholangiopathies or hepatitis, significant edema of the wall results in impingement on the lumen and the gallbladder which will appear relatively small.

The gallbladder in this patient is unusually small (white arrows b, c, d). There is some fluid and minimal solid content in the stomach that could have been the stimulus. We suspected a hypercontractile gallbladder.
Courtesy Ashley Davidoff Davidoff MD

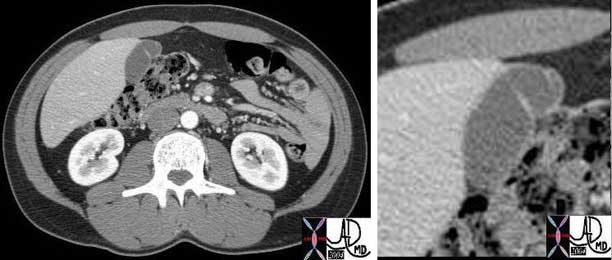
The CT scan shows a gallbladder that is small, contains a calcified stone and a hyperemic wall consistent with a fibrotic gallbladder of chronic cholecystitis. These patients are usually not symptomatic.
Images courtesy of: Ashley Davidoff, M.D.
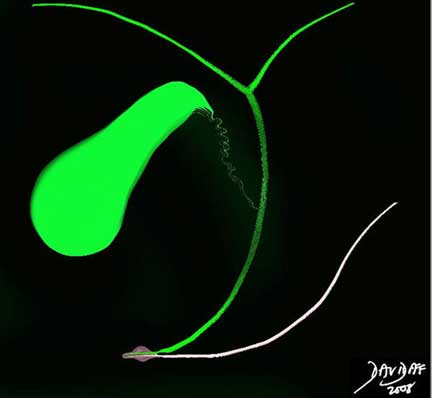
Shape
The gallbladder is characteristically a pear-shaped (pyriform), oval, or cone shaped structure, but may be rounded, elongated, or angulated. The fundus has the largest diameter and is in general spherical, while the shape of the body of the gallbladder varies between tubular and ovoid, and the neck tends to be triangular as it becomes narrow and tapered with an overall sigmoid curve with it terminating with a downward turn to meet the cystic duct. There is a progressive diminution of diameter from the fundus to the neck.
When viewed macroscopically the internal surface has fine mucosal folds, but when viewed in the distended state by imaging techniques it is smooth. The many normal variations of the shape of the gallbladder will be discussed as we delve into its depths in health and disease.
The classical pear-shaped form is not the classical shape seen in imaging. The normal gallbladder by ultrasound is usually more elongated and its shape is closer to a zucchini than a pear.

This ultrasound reveals a longitudinal view of the gallbladder in the fasting state. The classical pear (pyriform) shape of the gallbladder is not readily apparent and it looks more like a zucchini than a pear. However, when the gallbladder enlarges the fundus rounds out and the shape then becomes more reminiscent of a pear.
Images courtesy of: Ashley Davidoff, M.D.
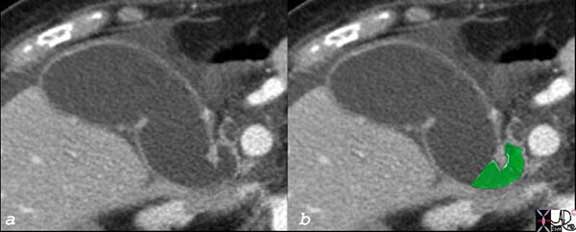
CT scanning is not performed along the long and true axis of the gallbladder and sometimes therefore the pear shape is apparent as an artifact of the inaccurate plane acquired.
The CT scan reflects an orthogonal view of the gallbladder which is not necessarily along its true axis. In this CT image the characteristic pear shape is noted.
Images courtesy of: Ashley Davidoff, M.D.
Shape: Variations
The phrygian cap is the most interesting shape of the gallbladder with a fascinating cultural history. It is a normal variant of gallbladder shape occurring in 4% of the population and is characterized by a fundus that is folded forward. It was first described by Bartel in 1916. The Phrygians were a primitive race that migrated into northern and central Asia Minor in the second millennium BC. The Greeks knew of the cap as an Oriental headgear that was tight fitting and conical in shape and was depicted in their art (Ober).
Images courtesy of: Ashley Davidoff, M.D.
The cap was a symbol of freedom and liberty. It was worn by King Midas who was cursed with donkey ears by Apollo. He used the Phrygian cap to hide his ears. It was subsequently worn by the Trojan hero Paris, was a symbol of freedom in the French and American revolutions, was depicted on coinage in the US, and also depicted on a variety of seals and flags throughout the world.
The CT scan shows a fundal fold creating a phrygian cap.
Images courtesy of: Ashley Davidoff, M.D.
Shape: Other Folds
Folds between the body and neck are also relatively common.
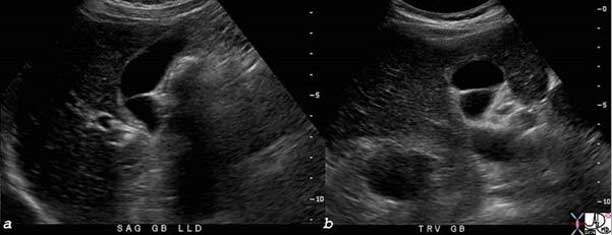
The ultrasound examination in both the sagittal and transverse plane shows a fold between the body and the neck of the gallbladder.
Images courtesy of: Ashley Davidoff, M.D.
There are a variety of shapes that are normal variants. The sigmoid-shaped gallbladder and the Zucchini gallbladder shown below are two of examples.

Images courtesy of: Ashley Davidoff, M.D.

With the aging process elasticity and compliance is diminished and the gallbladder can become voluminous, usually in the long axis. In the normally atonic bladder, seen in the elderly and diabetics, the transverse dimension is not usually larger than 4 cm.
Courtesy of: Ashley Davidoff, M.D.
Shape: Abnormal Shapes
When the gallbladder truly starts to look like a pear, with a rotund fundus it is usually a sign of enlargement. The diameter of the fundus is the largest diameter and by Lapalace’s law will have the highest tension on its walls and will, therefore, dilate first.

Images courtesy of: Ashley Davidoff, M.D.
The rounded shape of enlargement reflecting increased pressure is seen also in the body of the gallbladder in transverse projection in the case of acute cholecystitis below.
In this ultrasound of the gallbladder from a patient with right upper quadrant pain the gallbladder in the transverse plane measures 5cm and is round in shape rather than oval. The diagnosis was acute cholecystitis.
Images courtesy of: Ashley Davidoff, M.D.
A gallstone sometimes lodges in the fundus, induces inflammation and fibrosis and gets trapped in a fund

Sometimes a stone is trapped in the fundus of the gallbladder and it induces a chronic inflammatory process resulting in inflammation and subsequent fibrosis. A separate fundal chamber evolves, giving the gallbladder a figure of 8 appearance. In this oral cholecystogram a filling defect in the fundus of the gallbladder represents a stone and it is trapped by a ring of fibrosis it has induced.
Images courtesy of: Ashley Davidoff, M.D.

The CT scan shows a similar figure of 8 appearance of the gallbladder, but no radiopaque stone is visible.
Images courtesy of: Ashley Davidoff, M.D.
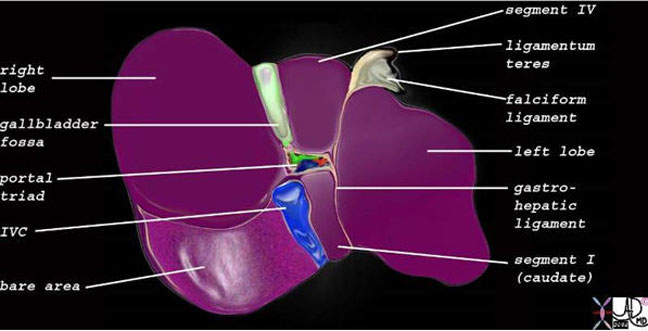
Position
The gallbladder lies within the abdominal cavity and in the peritoneal cavity on the undersurface of the liver in the gallbladder fossa between the right and left lobes.

Images courtesy of: Ashley Davidoff, M.D.
The Gallbladder Fossa on the Undersurface of the Gallbladder
The gallbladder fossa is a long and relatively narrow bed within which the gallbladder lies. It consists of loose connective tissue and vessels that anchor and connect the gallbladder to the liver.
Images courtesy of: Ashley Davidoff, M.DThe liver is divided into 5 major segments based on the hepatic venous anatomy. (Couinard) The gallbladder lies between segment V of the right lobe and segment IVb (also know as the quadrate lobe or the medial segment of the left lobe ).
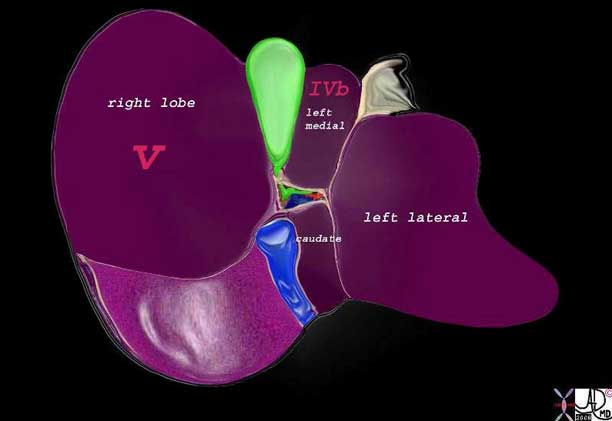
Using surgical terminology of Couinard, the gallbladder more specifically is situated between the right lobe (segment V) and the medial segment of the left lobe (segment IVb).
Images courtesy of: Ashley Davidoff, M.D.
Position: Cantlie’s Line
The gallbladder
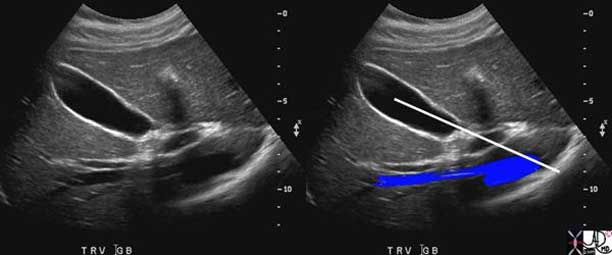
The ultrasound image taken in the transverse plane shows the gallbladder positioned between the right and left lobes. Cantlie’s line is an oblique plane drawn from the middle of the gallbladder to the left border of the inferior vena cava – generally considered a line of division between the right and left lobes.
Courtesy of: Ashley Davidoff, M.D.
position and axis can also be described as lying within Cantlie’s line which is an oblique plane drawn from the middle of the gallbladder to the left border of the inferior vena cava – generally and roughly considered a line of division between the right and left lobes.
The plane of the gallbladder also lies in the same plane as the middle hepatic vein which is the true and more accurate division of the right and left lobes.

Courtesy of: Ashley Davidoff, M.D.
The fundus of the gallbladder is the most anterior, lateral, and inferior part of the gallbladder.

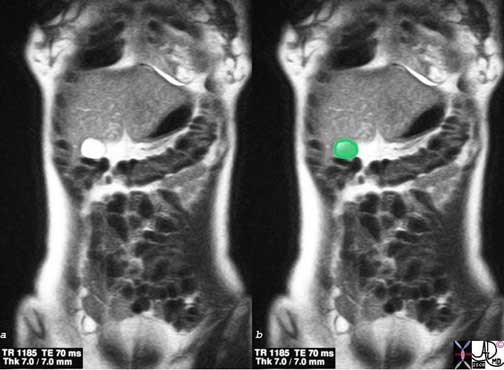
This T2-weighted MRI is acquired in the coronal plane showing the gallbladder (arrow) as an oval white structure. The fundus is lateral and inferior relative to the body and neck which lie medial and posterior.
Courtesy of: Ashley Davidoff, M.D.
The fundus lies just under the anterior abdominal wall and is the only portion of the gallbladder that lies unprotected. The exposed position of the fundus is well known to examining clinical hands as being ?below the liver’s edge, in the midclavicular line, just below the 9th rib.”
The body and neck lie medial, posterior, and superior to the fundus. In this position they are relatively protected by the liver. This is an important consideration since leakage of bile from traumatic injury into the peritoneal cavity can result in devastating and sometimes fatal peritonitis.
The position of the parts of the gallbladder in relation to each other is also very important in the functioning of the gallbladder. The body and fundus lie inferior to the neck and they accumulate, concentrate and store bile making its SG a slightly higher value than the “new” incoming bile. As bile is concentrated it sinks to the dependent portion of the gallbladder, which in the upright position is in the fundus. Stratification thus occurs dividing the bile into “old”, “new”, and “fresh”, each relatively positioned in the fundus, body and neck.
Courtesy of: Ashley Davidoff, M.D.

This ultrasound of a normal gallbladder of a 20-year-old male has been turned to simulate a standing and or seated position which is the dominant position during the day. The inferiorly positioned fundus and body enable a stratification of new and old bile. With the person in the standing or sitting position, the shape of this gallbladder allows new bile to come into the neck and then quickly spill over into the body where it will become layered on the top of the old bile since it has a SG that is lower than the concentrated bile. It will be the “new” within the body and fundus, and will then be subjected to concentration. Thus, the position of the gallbladder is designed to optimize the function.
Images courtesy of: Ashley Davidoff, M.D.
Position: Position of the Gallbladder in Relation to Other StructuresThe gallbladder’s immediate neighbors besides the liver lobes, include the porta hepatis which contains the portal triad (hepatic artery, portal vein, bile duct), lymphatics and nerves, surrounded by Glisson’s capsule (extension of the gastrohepatic ligament). More posteriorly the intrahepatic portion of the IVC is present.
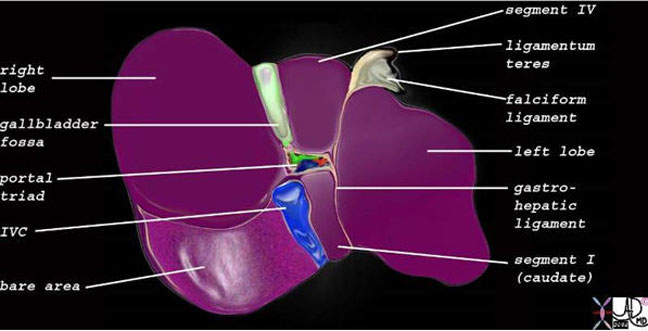
Images courtesy of: Ashley Davidoff, M.D.
Outside of the liver, an inferior neighbor of the fundus is the hepatic flexure, while the neck and body lie in close association to the descending portion of the duodenum
Images courtesy of: Ashley Davidoff, M.D.

to the Antrum and Duodenum
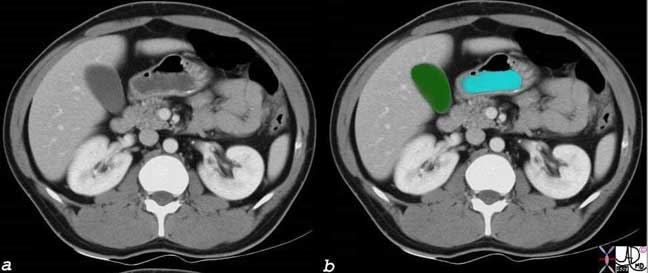
The ultrasound in this instance demonstrates a transverse view of the gallbladder (green) with antrum or duodenum (orange) noted medial to the body and neck of the gallbladder.
Images courtesy of: Ashley Davidoff, M.D.

This 89-year-old female has lost the elasticity to her gallbladder which has elongated and turned on itself ending up on the lateral border of the liver.
Images courtesy of: Ashley Davidoff, M.D.
Position: Applied BiologyThe gallbladder is not usually palpable but when enlarged it is felt just below the liver’s edge in the midclavicular line, below the 9th rib.
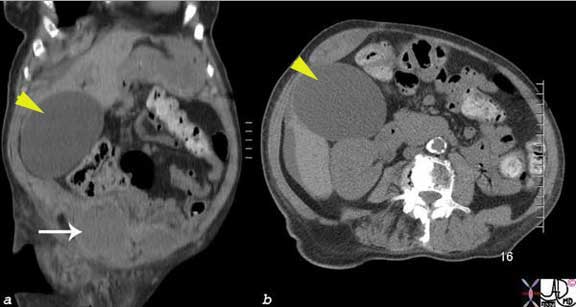
The sagittal image (a) from a CT scan and the transverse image reveal an enormous balloon like rotund gallbladder (yellow arrowhead) that was clinically palpable. This 80-year-old female had recently undergone cardiac catheterization and had a bleed (arrow) into the right rectus sheath.
Images courtesy of: Ashley Davidoff, M.D.
Murphy’s sign utilizes the position of the fundus to determine whether a patient has acute cholecystitis. As the patient inspires, the gallbladder moves down and forward and if the gallbladder is inflamed and distended then the examining hand in the midclavicular line below the 9th rib will induce pain and will cause the patient to stop inspiration in mid breath.
Courvoisier’s sign also uses the surface anatomy of the gallbladder fundus. It is stated that a palpable gallbladder in the presence of obstructive jaundice, is most commonly caused by pancreatic cancer, and sometimes caused by a cancer at the ampulla.
The close relationship of the gallbladder to the liver creates a potential pathway for the spread of disease. Thus extension of the inflammatory and infectious process of acute cholecystitis will be identified in the liver.
A gallbladder cancer (orange) has extended from the gallbladder (green) directly into the liver. Associated ductal obstruction is present.
Images courtesy of: Ashley Davidoff, M.D.
Position: Situs Ambiguous
Sometimes patients are born with an abnormal position of the gallbladder. This occurs with situs inversus but also occurs in rare instances in situs ambiguous states such as asplenia and polysplenia syndromes

In the CT scan through the upper abdomen complete situs inversus is noted. The liver (purple), gallbladder and IVC (navy blue) lie to the left. The pancreas, (pink) stomach (orange) and spleen (maroon) lie to the right. Ascites is present, and the left kidney is small and smooth.
Courtesy of: Ashley Davidoff, M.D.
Character
The gallbladder is a dark-green sturdy sac that looks like a deflated balloon when viewed anatomically. It has a soft leather feel due to its fibroelastic muscular wall and in essence can be described as distensible, muscular, and elastic.
It is often stained with bile and crystalline granules. Once these are washed away the mucosa is usually pink and smooth. When the wall is cut in cross section the 3 layers are too thin to be distinguished macroscopically but three obvious layers are present histologically. The epithelium is cellular and the lamina propria as part of the mucosa is probably the loosest layer of the wall . The muscularis provides the musculo-fibro-elastic properties, while the serosa/adventitia also has relatively loose consistency.
Character: Bile
The bile is a bitter yellow or green alkaline fluid. It contains a variable concentration of solutes and water that change its character and specific gravity (SG) which ranges between 1.010 to 1.040 or even higher. It has a freezing point of -.56 degrees centigrade.
As it enters the cystic duct as fresh bile it’s SG is closer to 1.010. When it enters the neck it mixes with mucus that is secreted in the neck resulting in a rise of SG. The gallbladder concentrates the bile by 5-6 times, eventually giving it an SG of about 1.040.
The principal constituents include salts of bile acids, bile pigments, neutral fats, lecithins, phosphatides, nucleoproteins, mucin and cholesterol.
Bilirubin gives bile its yellow-green color. It is the same pigment that gives the color to bruises and accounts for the yellow discoloration of jaundice. It is formed when hemoglobin breaks down.

Courtesy of Ashley Davidoff, M.D.
Character: Applied Biology
We approach the characterization of the gallbladder in the clinical realm using a limited clinical exam, blood tests to assess and classify jaundice and medical imaging. From the structural perspective, ultrasound is the best tool to characterize the wall and contents of the gallbladder.
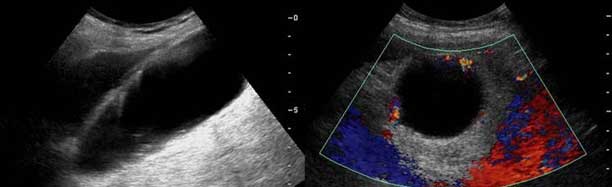
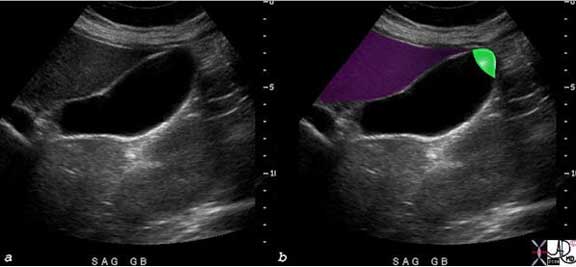
When the normal gallbladder wall is imaged by ultrasound in the fasting state, it stratified into its three layers. However, when it is in its contracted state, three definite layers are seen. The inner mucosal layer is echogenic, middle muscularis layer is hypoechoic and the outer serosal/adventitial layer is hyperechoic.
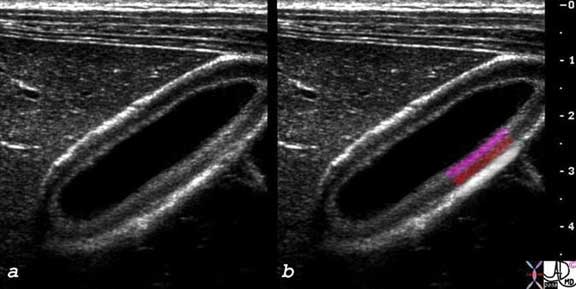
The layers of the wall are only seen when the gallbladder is contracted or thickened for any reason. The inner pink layer is the mucosa, the middle muscularis (red) and outer serosa/adventitial layer.
Courtesy of Ashley Davidoff, M.D.
The bile containing lumen is anechoic in both the fasting state and postprandially.

The sagittal view of the gallbladder shows a distended fundus and body of the gallbladder where contents (bile) have no echoes – clear fluid and the only visible part of the wall abutting the liver is a single layer.
Courtesy of Ashley Davidoff, M.D.
The most common abnormalities in the lumen include gallstones and sludge.

The sagittal view of the gallbladder shows a fluid-fluid layer with sludge (orange arrow) noted in the dependent portion, anechoic bile in the upper portion as the supernatant, and a shadowing stone (black arrow) lying dependently in the body.
Images courtesy of: Ashley Davidoff, M.D.
Parts
The gallbladder, like every organ in the body consists of its unique parts, a capsule, and its connection to other parts of the body, much in the way a house or building consists of its component parts, an outer covering and cable, electrical and sewer lines that connect it to the other parts of the community.
The gallbladder as a one compartment house consists of a fundus, body, and neck; its northern wall is protected by the liver, while its walls on the south, east and west side are covered by the visceral peritoneum. Its connections to the system at large are via the cystic duct, cystic arteries and veins, autonomic and hepatic lymphatic systems.
The gallbladder is divided into three general parts: fundus, body and neck. They are each very different in size, shape, and position and all relevant to the function of the gallbladder. The infundibulum of the gallbladder is part of the body and Hartmann’s pouch is part of the neck.

Courtesy of: Ashley Davidoff, M.D.
Fundus
The fundus has the largest diameter, is usually spherical in shape, and is the only portion of the gallbladder that is exposed and unprotected by the liver. It lies as the most anterior and rightward portion of the gallbladder. It lies superior to the hepatic flexure. As the most inferior portion of the gallbladder, it is the most dependant part during the day while the person is upright. Hence, the bile that is most concentrated with the highest SG will be found in the fundus. The blood supply is endarterial, meaning it is the last part of the gallbladder to receive its blood and therefore it is most vulnerable to ischemia. It is the only portion of the gallbladder that is completely surrounded by peritoneum. Since it is not attached to the liver it is relatively mobile so that when the gallbladder stretches in atonic conditions such as old age, it is mostly the fundus that stretches.
Just beyond the liver’s edge in the midclavicular line, and just below the 9th right rib, the fundus of the gallbladder lies unprotected and potentially palpable to the examining hand. However it is not normally palpable unless it is significantly distended. The body and neck lie more posterior and inaccessible to clinical examination even when enlarged.
Courtesy of: Ashley Davidoff, M.D.
The fundus is the only part of the gallbladder that potentially is clinically palpable, and in fact is only palpable when the gallbladder is significantly distended. When the pressure in the gallbladder rises, the tension on the fundus will be maximal according to the law of Laplace, since the tension on the wall for a given pressure is directly proportional to radius. Therefore the fundus with the largest radius will enlarge out of proportion in relation to the body and the neck. The site of rupture from distension therefore, will also be the fundus, not only because it has the most tension exerted on it but also because it is supplied by an end artery.

The MRCP (Magnetic Resonance Cholangiopancreatography) performed using T2-weighted technique shows a common bile duct (CBD) stone associated with dilatation of the CBD, cystic duct and the gallbladder. The shape change of the enlarged gallbladder is most profound in the fundus because of the increased tension exerted on the largest diameter of cylinder/sphere according to Laplace’s law.
Courtesy of: Ashley Davidoff, M.D.
Parts: The Body of the Gallbladder
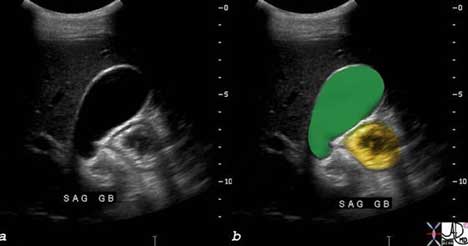
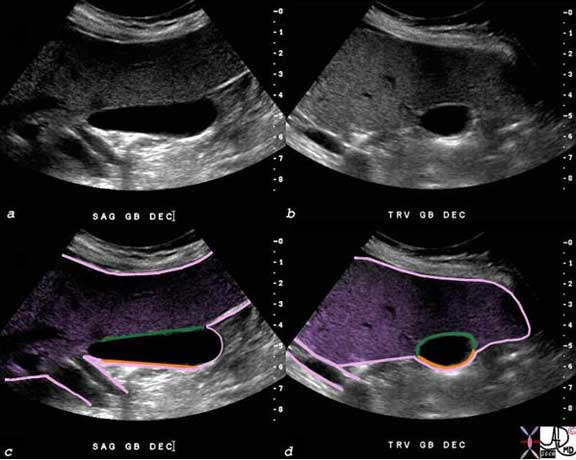
The body of the gallbladder is the most voluminous portion of the gallbladder. It is more cylindrical in shape but its diameter narrows minimally as it advances from the fundus to the neck. The most medial portion of the body lies opposite the fundus, is tunnel-shaped and is called the infundibulum.
The body of the gallbladder lies posterior to the liver and hence is relatively protected. The upper surface of the body lies in the gallbladder fossa and is free of a peritoneal covering. As a result of this attachment to the liver, the body is relatively fixed in position. The free surface of the body is covered by peritoneum and lies superior to and in close association with the duodenum. The muscular layer is best developed in the body of the gallbladder.
The body of the gallbladder is attached to the liver (purple). The US in sagittal section (a, c) and transverse section (b, d) shows the fixed portion (green) of the body attached to the gallbladder fossa and liver, and the free wall (orange) lying open to the peritoneal cavity. The image also reflects the megaphone or flask like shape to the body with a decreasing diameter as the gallbladder proceeds from the fundus to the neck.
Courtesy of: Ashley Davidoff, M.D.
When the gallbladder becomes inflamed, the dominant location of fluid accumulation is in the gallbladder fossa, where the body of the gallbladder is attached to the liver.
This US is from a patient who presented with classical signs of right upper quadrant pain and the edema of the gallbladder is predominantly in the gallbladder fossa since this is the location of the lymphatics and other congested vessels.
Image courtesy of: Ashley Davidoff, M.D.
Parts: Neck of the Gallbladder
The neck is the smallest part of the gallbladder both in diameter and in volume. It tends to be sigmoid in shape and at its most medial end it turns inferiorly as it joins the cystic duct. Sometimes a fold is found on the posterior wall of the gallbladder where the body and neck join. This fold is called a junctional fold and has no clinical significance.
It is the most medial part of the gallbladder and lies in close association with the porta hepatis.
The neck of the gallbladder is usually quite difficult to image. In this CT scan of an elderly female patient the gallbladder is dilated so its component parts are distorted and easier to visualize. The partial sigmoid shape of the neck is overlaid in green.
Image courtesy of: Ashley Davidoff, M.D.
The neck is the most posterior and medial portion of the gallbladder and is in close association with the porta hepatis which lies even more posterior and medial to it.
Images courtesy of: Ashley Davidoff, M.D.
The full extent of the neck is not routinely visualized on US because of its small size, tortuosity and the fact that it is nestled deep among other structures.
As the structure with the smallest diameter and most tortuous course, it is the site that has a predilection to stone impaction
The full extent of the neck of the gallbladder is not easily nor routinely seen on all ultrasound examinations because it is small, tortuous, and nestled among other echogenic structures that tend to camouflage it. In this instance, the neck (lightest green) can be seen between the infundibulum and the beginning of the cystic duct.
Images courtesy of: Ashley Davidoff, M.D.
Neck: Hartmann’s Pouch
Hartmann’s pouch, also known as the ampulla of the gallbladder, fossa provesicalis, or pelvis of the gallbladder, is a spheroidal or conical pouch at the junction of the neck with the cystic duct. It is an outpouching on the inferior surface of the neck that is thought to be acquired during life and caused by stone disease resulting in inflammation and secondary adhesions between the neck and the cystic duct.
Hartmann’s pouch (arrow) is an outpouching situated on the inferior aspect of the neck of the gallbladder that is caused by prior inflammatory and stone disease in the area.
Courtesy of: Ashley Davidoff, M.D.
Parts: Capsule of the Gallbladder
The gallbladder capsule is a protective covering consisting of loose connective tissue.
Structurally, the coverings on the free surface and the hepatic surface are different. On the free surface the loose connective tissue is covered and protected by the peritoneum and it is called a serosa. On the liver surface it is covered and protected by the liver and here it is called an adventitia. The fundus is totally surrounded by peritoneum. Occasionally the peritoneum almost totally surrounds the body of the gallbladder such that if one would place one’s thumb over the anterior surface and one’s index finger posteriorly they would meet separated only by a double layer of peritoneum. Usually though the gallbladder is bound down by the peritoneum so it remains snug and protected.
Functionally, the serous membrane formed by the visceral peritoneum covering is resilient, smooth and is richly endowed with nerves and lymphatics. It protects as well as connects the gallbladder with the other peritoneal covered organs of the abdomen. The adventitia acts more as a conduit to transmit fluids to and from the mother organ, the liver. It in fact, is the hilum of the gallbladder.
The diseases of the coverings are really a mirror of disease in the peritoneal cavity, from within the gallbladder or from the liver. Serosal implants from peritoneal carcinomatosis spread of inflammation from or to the liver, and spread of cancer of the gallbladder via the gallbladder fossa to the liver are some examples.
Treatments of the primary disease will therefore affect the way the capsule is treated.

The serosal surface of the gallbladder is covered by visceral peritoneum which then continues over the liver surface. the diagram shows the visceral peritoneum peeled back off the liver to expose the bare area of the gallbladder which is really its adventitial surface, and is synonymous with the gallbladder fossa and bare area of the gallbladder.
Courtesy of: Ashley Davidoff, M.D.
The visceral peritoneum (pink) encloses almost the entire liver, totally covers the fundus of the gallbladder as seen in the longitudinal view of the gallbladder (c), and then covers the free wall of the body of the gallbladder on the undersurface of the liver (c,d) after which it reflects off the liver to enclose the vessels of the porta hepatis Two tubular structures in the porta are surrounded by the same peritoneal lining.
When there is peritoneal carcinomatosis metastasis disease is able to settle and grow on the gallbladder. In the case shown below a metastasis is seen in the fundus of the gallbladder.
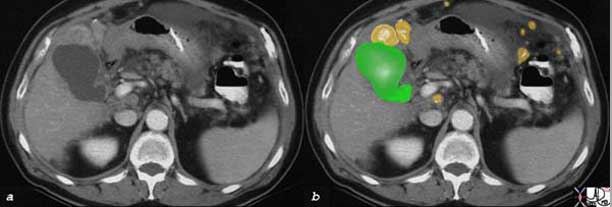
The CT scan in cross section shows a deformed fundus of the gallbladder (green) compressed by a metastasis (orange) in this patient who has peritoneal carcinomatosis. Other metastases are noted in the peritoneal cavity and are also overlaid in orange.
Images Courtesy of: Ashley Davidoff, M.D.
Blood Supply
The gallbladder is supplied by the cystic artery. The cystic artery is usually a branch of the right hepatic artery but can also originate from the left or common hepatic arteries, the gastroduodenal artery, or directly from the celiac trunk.
The cystic artery passes superior to the cystic duct and terminates in two branches called the anterior (superficial) branch that runs on the free wall of the gallbladder and the posterior (deep) branch that runs on the hepatic aspect of the gallbladder close to the gallbladder fossa. The cystic duct is supplied by two to four minor branches called Calot?s arteries that originate just proximal to the origin of the anterior and posterior vessels.
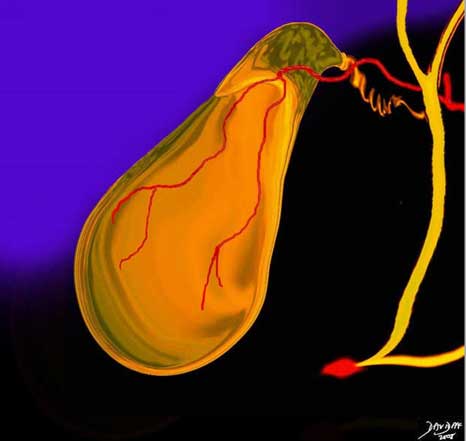
Cystic Artery off the Right Hepatic Artery
Images Courtesy of: Ashley Davidoff, M.D.
The vessel for most of its course runs in the triangle of Calot whose boundaries are the inferior border of the liver’s edge, cystic duct, and common hepatic duct.
Small arteries, veins and biliary radicals run between the liver and the gallbladder in the gallbladder fossa directly from the liver into the gallbladder.
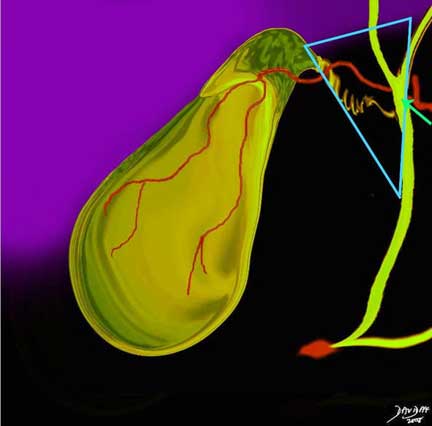
Courtesy of: Ashley Davidoff, M.D.

Arterioles of the Cystic Artery in the Submucosa; Deep and Superficial Branches
Image shows the hepatic artery in the porta hepatis, while (c) and (d), show the tiny vessels in the lamina propria (red dots) of the gallbladder since the edema in the wall has provided sufficient contrast to expose them.
red = hepatic artery, green = lumen of the gallbladder. Image courtesy of: Ashley Davidoff, M.D.
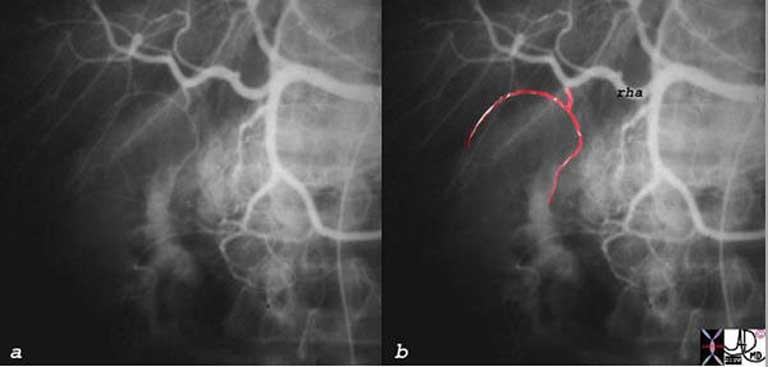
Blood Supply: Variations
In about 15% of patients the anterior and posterior arteries have separate origins and this entity is called double cystic artery. An example is seen below.
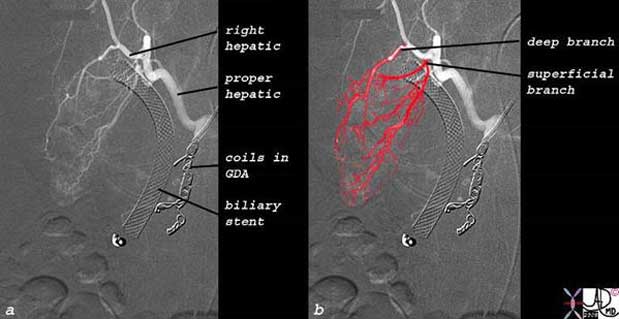
Angiogram of a 52-year-old male with HIV, cholangiopathy and cryptosporidium associated with a neoplastic mass in the CBD, and a fistula between the CBD and duodenum presents with uncontrolled hemobilia. Embolization of the gastroduodenal artery was successful. The follow up angiogram shows the catheter in the gastroduodenal artery (GDA) which has been occluded by coils, a stent in the CBD, and flow in the cystic circulation. The right hepatic artery gives rise to separate origins of the deep or posterior branch that runs close to the gallbladder fossa and the superficial or anterior branch that runs on the free wall of the gallbladder.
Courtesy of: Ashley Davidoff, M.D
Other variations of the origin of the vessel include its origin from the left or common hepatic artery, and it can course either anterior to or posterior to the common hepatic duct.
Blood Supply: Venous Drainage
The venous drainage of the gallbladder is unusual since the fundus and the body drain directly into the liver via the gallbladder fossa, which in turn drain into the intrahepatic portal radicals of segments V and IV of Couinard – the two segments between which the gallbladder lies. There is also direct drainage of the venules in the gallbladder fossa into the sinusoid, creating another unique portal circulation (Moore).
Venous drainage of the neck and cystic duct are drained by the posterior and anterior cystic veins which join with the gastric, duodenal, and pancreatic veins to empty into the right portal system.
The CT scan during portal venous phase shows a gallbladder with an edematous wall and contrast enhanced mucosa and small punctate vessels in the lamina propria. Some of these vessels are small and well-defined and are presumably arterioles (red), while others at the base of the gallbladder are slightly larger (blue), suggesting that these may be venules draining the neck.
Courtesy of: Ashley Davidoff, M.D.
The main final common pathway of gallbladder venous drainage is via the right portal vein which receives venous blood both from segments V and IV, and also directly from the cystic veins at the base of the gallbladder. Once the portal venous radicals perfuse the sinusoids, blood reaches the middle or right hepatic veins before entering the inferior vena cava.
Blood Supply: Applied Biology
Circulatory and inflammatory diseases result in venous and lymphatic congestion leading to an increase in extracellular fluid. In right heart failure for example the increased right-sided pressures reflect in venous congestion of the liver and gallbladder edema can result. This is especially prominent in patients with right heart failure and with tricuspid regurgitation.
Inflammation of the gallbladder and liver are also characterized by exudation of fluid due to hyperemia, and increased capillary leakage as a normal response by the body to the noxious agent. The increased extravascular fluid, may accumulate either by design to dilute the noxious agent or as a result of decreased drainage of an overwhelmed lymphatic system that fails to drain effectively. As a result fluid may accumulate in the soft tissues of the gallbladder and the fluid is often visible on radiological imaging.

This 32-year-old female has scleroderma and her disease is characterized by interstitial basal lung disease (a, b) with normal anterior lung fields and fibrotic posterior lung fields, enlargement of right heart structures (maroon in (d)), pericardial effusion (light yellow in d), pleural effusions (dark yellow in d) and an edematous wall (orange, in (f)) of the gallbladder (lumen is green). As a result of her lung disease she developed pulmonary hypertension, right heart failure and tricuspid regurgitation and this led to the gallbladder edema.
Courtesy of: Ashley Davidoff, M.D.
Venous varicosities are formed as a result of portal hypertension or portal vein occlusion with the development of new collaterals that encompass the gallbladder.
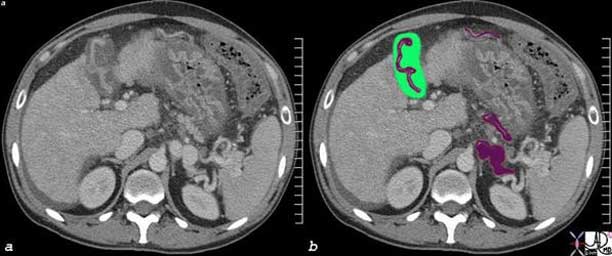
In this CT scan through the upper abdomen, portal hypertension is also manifested with patent venous varicosities (maroon) in the splenic hilum, over the gallbladder and with an enlarged gastroepiploic vein The stomach shows signs of a hypertensive gastropathy with thickened wall and hyperemic mucosa, there is a small amount of ascites behind the liver, and the caudate lobe is enlarged. These findings are consistent with cirrhosis and portal hypertension.
Ashley Davidoff, M.D.
Lymphatic Drainage
The gallbladder is drained by lymphatics that arise from the lamina propria and serosal adventitial layers and become confluent over the anterior and posterior surfaces of the gallbladder, much like the distribution of the arteries. Lymph also drains via lymphatics in the gallbladder fossa directly into the lymphatics of the liver.
From the anterior and posterior wall the main drainage is along the cystic duct to their first nodal station – Calot’s node located within Calot’s triangle near the neck of the gallbladder.

Calot’s triangle is an anatomic space bordered by the common hepatic duct medially, the cystic duct inferiorly and the liver superiorly. The cystic artery usually passes through the triangle and Calot’s lymph node (bright yellow) is also within this triangle. It is an important landmark to recognize during laparoscopic cholecystectomy. The primary pathway of lymphatic drainage of the gallbladder once the lymph reaches the Calot’s node is along the cystic duct, bile duct and toward the nodes that lie behind the head of the pancreas and duodenum. In this diagram one of these nodes is seen as the largest node in close association with the ampulla (red) and pancreatic duct (light pink).
Ashley Davidoff, M.D.
From the Calot’s node, there are then two major pathways sometimes via the hepatic nodes. The dominant pathway of lymphatic drainage is the cholecystopancreatic nodes. This pathway courses along the cystic duct and common bile duct and then to nodes that are posterior to the pancreas and the duodenum.
The second pathway is the cholecystoceliac where the lymphatics drain from the hepatic nodes and the cystic node; they pass along the hepatoduodenal ligament close to the foramen of Winslow and drain into the celiac nodes.
The third pathway is the cholemesenteric pathway via the posterior pancreatic nodes and then to aortocaval and para-aortic nodes.
The lymph nodes of the hilum of the liver are usually involved also in the drainage of the gallbladder.

The CT scan is from a patient with Hodgkin’s lymphoma whose lymph nodes in the abdomen are enlarged. Nodes relevant to gallbladder drainage include Calot’s node, the hepatic node, peripancreatic nodes, and para-aortic nodes.
Ashley Davidoff, M.D.
Nerve Supply
The autonomic nervous system is an involuntary nervous system which is responsible for the minute to minute as well as the day to day functions of the body systems. It is activated mainly by centers in the hypothalamus, brain stem and spinal cord but is influenced to some extent by the cerebral cortex.
Sensory signals from the viscera travel to the spinal cord, brain stem and hypothalamus, and appropriate responses are returned to the viscera. This pathway is called a visceral reflex.
In the sympathetic chain there is an intermediary step between the viscera and spinal cord – a “halfway house” if you will, that runs alongside the spinal cord, and it is called the sympathetic chain. There is therefore a neuron that carries the signal from the spinal cord to the sympathetic chain called the preganglionic neuron, and one that carries the signal between the ganglion of the chain to the organ called the post ganglionic neuron. The preganglionic fiber is short and the post ganglionic fiber is long.
In general the sympathetic nerves of T1 go to the head, T2- T6 to the thorax and T7 -T11 to the abdomen. The nerves of T12, L1 and L2 go to the legs. This distribution is an approximation and there is a large cross over of geographic coverage from person to person. The innervation in large part is governed by the embryological origin of the tissues. Since the heart for example had its origins in the neck of the developing fetus, sympathetic innervation is from the neck segments. Similarly the foregut organs arose from the chest endoderm/mesoderm tissues and so innervation is from the lower thoracic region.
The parasympathetic system is designed differently. It executes its function through the cranial nerves and through sacral segments. Most of its function, however, is executed through the vagus nerve which covers both the chest and abdominal cavities. It also has a system of preganglionic and post ganglionic fibers but the preganglionic fibers usually pass into or close to the organ and post ganglionic fibers are dominantly within the organ. Therefore, unlike the sympathetic system, the preganglionic fiber is long and the post ganglionic fiber is short.
Within the gastrointestinal tract, the parasympathetic system accelerates digestion by increasing peristalsis and opening valves and sphincters, and increasing blood flow to the digestive organs. In essence it promotes digestion and absorption, which is best done while the person is resting. The sympathetic system is the ?fight or flight? component and directs energy and blood to skeletal muscle and other organs that need energy when a person is active, and in turn directs energies away from the gastrointestinal tract. Thus in the digestive system, it slows things down by slowing peristalsis, closing valves and sphincters, and decreasing blood flow to the digestive tract.
The nerves for the gallbladder run with the cystic artery so that they travel with the celiac axis, and then the right hepatic artery and finally with the branches to the gallbladder.
Nerve Supply: Parasympathetic System
The function of the parasympathetic system with regard to the gallbladder and biliary system is to accelerate the production and delivery of bile to the duodenum so contraction of smooth muscle in the gallbladder is facilitated while the sphincter of Oddi relaxes so as to open the juice gates. The vagus nerve is the parasympathetic component and it arises from both vagal trunks via anterior and posterior trunks. The anterior trunk (left vagus) is connected to the hepatic plexus and is the major supply to the gallbladder. The posterior trunk (right vagus) utilizes the celiac plexus and controls the sphincter of Oddi.
Injury or surgical vagotomy to the anterior trunk will reduce gallbladder contractility, promote stasis and predispose to cholelithiasis.
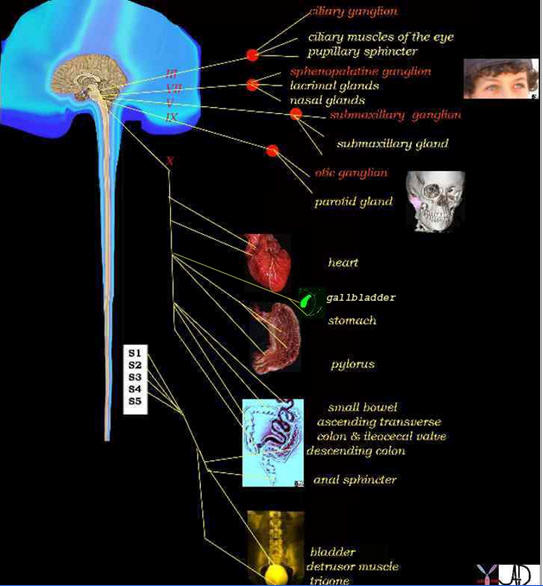
The vagus is the parasympathetic nerve that innervates the gallbladder and it has two trunks. The anterior trunk innervates the gallbladder smooth muscle and the posterior trunk innervates the sphincter of Oddi. The diagram shows the vagus (cranial nerve X) and the extent of its parasympathetic innervation.
Ashley Davidoff, M.D.
Nerve Supply: Sympathetic System
The function of the sympathetic system is to slow digestion and hence it inhibits gallbladder emptying by increasing the tone of the sphincter of Oddi (hepatopancreatic sphincter) and by stimulating the release of vasoactive intestinal polypeptide (VIP) at nerve terminals to inhibit gallbladder contraction.
Sympathetic fibers arise from the celiac plexus. They travel with the cystic artery. The sympathetic innervation comes chiefly from T2-T10 and reaches the celiac ganglia via splanchnic nerves.
The greater splanchnic nerves for the biliary system receive sympathetic supply from T7-9 and the lesser splanchnic nerves from T10 and T11 while the least enters the cord at T12. The celiac plexus transmits afferent fibers from the foregut organs including the gallbladder, reaching the spinal cord through the greater splanchnic nerve and via the thoracic sympathetic chain.
Sympathetic fibers originate in the intermediolateral corneal cells in the spinal cord. They traverse out of the spinal column and can travel up, down, or in the region where they exit. These nerves provide the efferent innervation. The afferent signals travel back, much along the same route, but enter the spinal cord through the posterior spinal nerve roots. This afferent/efferent communication is the key to proper muscle contractions.
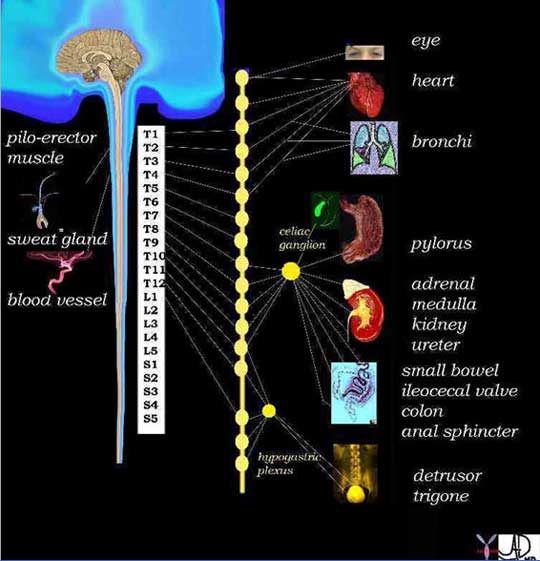
From the spinal cord the sympathetic neurons travel to the sympathetic chain that lies along the spinal cord (line of “yellow buttons”). This chain is an intermediary step between the viscera and spinal cord – a “halfway house” There is therefore a neuron that carries the signal from the spinal cord to the sympathetic chain called the preganglionic neuron, and one that carries the signal between the ganglion of the chain to the organ called the post ganglionic neuron. In general T1 goes to the head, T2- T6 the thorax and T7 -T11 the abdomen. T12, L1 and L2 go to the legs. This is an approximation and there is a large cross over. The innervation depends on the embryological origin. Since the heart originated in the neck of the fetus the innervation for the heart is from the cervical segments. Similarly, the foregut organs arise from the chest endoderm/mesoderm and so innervation is from the lower thoracic region.
Ashley Davidoff, M.D.
The somatic nerves of the gallbladder are from intercostal nerves T8, T9, and T10 spinal segments which supply the parietal peritoneum. The phrenic nerve is formed from C2, 3, 4 and 5 supplying the diaphragm, underlying peritoneum, and gallbladder.
Pain arising from the gallbladder or surrounding peritoneum can be carried by the sympathetic afferent fibers or by the somatic fibers and will be felt in the corresponding somatomes or dermatomes. Thus pain from the gallbladder is most commonly felt in the right upper quadrant but may be felt in the epigastric area, right shoulder, or anterior chest.
Cystic Duct of the Gallbladder
The cystic duct is the duct that connects the gallbladder to the bile duct. It is part of the biliary system and is characterized by its position and by its double spiral and serpiginous nature.
It consists of two parts. The proximal portion is called the spiral portion (pars spiralis) and as its name implies is tortuous and contains the spiral valves of Heister. They appear to regulate flow into and out of the gallbladder but their true function is not truly known. The distal part is straight, usually short and smooth and is called the pars glabra. This portion in some patients can be extremely long if it joins with the bile duct at its distal downstream end.
The structure of the cystic duct is quite unique, puzzling, variable and interesting. It is usually 2-4cm long but can be up to 10cms. It is usually 1-5mm wide. It is a tube with a course that proximally is usually tortuous or serpentine, much like the splenic artery. Therefore, it is a tube with double spiral morphology. It has 4-10 internal spirals of Heister and its overall proximal course shows tortuosity. It lies relatively posteriorly at the medial end of the gallbladder in close association with the portal triad with its surrounding Glisson’s capsule. It also runs in close association with the cystic artery. The cystic duct is supplied by 2 to 4 minor branches called Calot?s arteries that originate just proximal to the origin of the anterior and posterior branches of the cystic artery.
The cystic duct usually enters the bile duct halfway between the porta hepatis and the ampulla, but it may enter the bile duct at the porta hepatis or low down near the ampulla. It most commonly enters the bile duct on its lateral (right) side, but can enter medially, posteriorly or anteriorly. As it enters it changes the name of the bile duct from the upstream common hepatic duct to the downstream common bile duct.
The function of the cystic duct is clearly to transport bile to and from the gallbladder and bile duct. Its spiral forms are structurally interesting but functionally a puzzle. The closest one comes to is that the spiral valves of Heister create a resistance to flow that prevents overfilling and over distension of the gracile bile ducts at the time of gallbladder contraction.
The most common diseases of the cystic duct are of a mechanical nature and are as a result of small stones getting stuck and impacted in the duct and resulting in obstruction of the gallbladder. When inflammation supersedes this event then acute cholecystitis occurs. Cholecystitis is most commonly caused by by stones impacted in the neck or cystic duct. Treatment of cystic duct disease is usually surgical.
The proximal portion is called the spiral portion, (pars spiralis) and as its name implies it is tortuous and contains the spiral valves of Heister. They appear to regulate flow into and out of the gallbladder but their true function is not known. The distal part is straight, usually short and smooth and is called the pars glabra. This portion in some patients can be extremely long if it joins with the bile duct at its distal downstream end.
neck = dark green
spiral portion = light green,
straight portion = orange
common hepatic duct = light olive
common bile duct = dark olive
Courtesy of: Ashley Davidoff, M.D.
Cystic Duct: Applied Biology
There are a variety of normal variants of the cystic duct including its length and insertion point into the bile duct. An important and well known variation is the long smooth portion of the duct that runs parallel to the bile duct and finally inserts, usually on its left side, at a variable distance from the ampulla.

In this ERCP the straight portion of the cystic duct (orange) inserts into the medial aspect of the common hepatic duct (light olive) to form the common bile duct (dark olive) just proximal to the ampulla. This example is a variant of normal. Its increased length, parallel and medial course, and distal medial insertion are characteristic. As a result, the common hepatic duct will be long and the common bile duct will be short.
Ashley Davidoff, M.D.
Small Stones in the Cystic Duct
The most common disease affecting the cystic duct is impaction of small stones. This results in obstruction and bile cannot get in or out. The gallbladder becomes inflamed, acute cholecystitis manifests with exudation of fluid and the gallbladder becomes distended.

The artistic rendition shows a small stone impacted in the spiral valves of Heister, with inflammation of the wall and upstream distension due to exudation of fluid. The gallbladder enlarges, becomes rotund, and the upstream cystic duct distends. New bile cannot enter and bile cannot leave the gallbladder.
Courtesy of: Ashley Davidoff, M.D.
Cancer
The other relatively common disease that results in disease of the cystic duct is cancer of the head of the pancreas. This usually causes obstruction of the pancreatic duct, common bile duct, and by default the cystic duct and gallbladder as well.
Dilated Cystic Duct Pancreatic Carcinoma
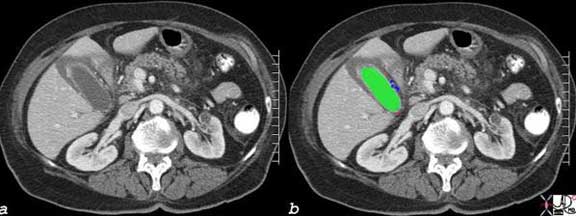
The transverse section of the base of the gallbladder shows the distended body (darkest green) and sinusoid neck of the gallbladder (intermediate green) connected to the similarly distended spiral portion of the cystic duct (light green) in this patient with carcinoma of the head of the pancreas. The cystic duct is dilated and therefore visualized. The cystic duct is not normally visualized for a number of reasons. It is relatively small (1-2mm), lies deep in the porta hepatis surrounded by the echogenic Glisson?s capsule and other structures of the porta and it is of itself echogenic because of the many valves which reflect echoes as well. All the echogenic structures prevent resolution of the small duct. Because the bile duct is obstructed by the pancreatic cancer, all the upstream components have become distended and the patient as a result becomes jaundiced.
Courtesy of: Ashley Davidoff, M.D.
Duplicated Gallbladder
Sometimes the pars cystica, the precursor for the gallbladder, divides in two rather than remaining one entity, forming a duplicated gallbladder usually with one cystic duct. This results in a duplicated gallbladder.
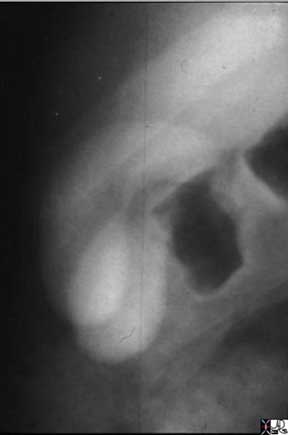
The oral cholecystogram shows two gallbladders lying side by side. This duplex system consists of two fundi and two bodies. The cystic duct is not appreciated in this example, but it is commonly a single entity.
Ashley Davidoff, M.D.
The CT scan in axial section also shows two gallbladders – a duplicated system. It is slightly harder to appreciate the two fundi and bodies. It is impossible to appreciate the cystic duct. The dark green represents the posterior and seemingly smaller gallbladder while the light green reveals the larger anterior gallbladder.
Images courtesy of: Ashley Davidoff, M.D.
Function of the Gallbladder – Receive, Process, and Export
The function of every biological unit in the body is based on its ability to receive a product, process it, and deliver the new product efficiently and effectively to where it is used and needed.
The gallbladder receives bile produced by the liver, processes it by concentration and storage, and delivers it on demand to the duodenum via the bile duct, so that the digestion of fat can be optimized.
The process of bile production occurs in two stages;
-
primary production
-
concentration
The gallbladder has no part in the primary production but is essential for the concentration. Bile is produced 24 hours a day, but seemingly is only needed for three short periods during mealtimes. On the other hand, it is also provides a route for the excretion of end products of hemoglobin breakdown and to some degree excretion of cholesterol.
With its simple design of a musculomembranous bag and single duct it is able to receive and concentrate 24 hours a day and deliver the bile via seemingly complex contraction patterns. Although it is not an essential organ, it does help optimize the function of the digestive process. People who have had a cholecystectomy do and can live an otherwise normal life and seemingly have no untoward effects without it.
Receive, Process, and Export: Bile
Bile is a yellow or green bitter fluid that is smooth, sterile, relatively thick, and sticky, with “spinnbarkeit” character. Spinnbarkeit is a German word that means ability to be spun and it infers that when bile is pulled apart it forms a continuous thin thread much like thin nasal mucus. The specific gravity ranges between 1.010 to 1.040 but can be as high as 1.059.
Structurally, it consists mainly of water, cholesterol, bile pigments, and bile salts. It is continually produced by the hepatocytes. It contains no enzymes and it is only the bile salts that are important in digestion. The end products of cholesterol are the bile acids (also know as bile salts) which are synthesized by oxidation of cholesterol in the liver and then conjugated with taurine or glycine. The major primary bile acids are chenodexycholic acid and cholic acid. When the bile acids mix with the alkaline milieu of the duodenum they become bile salts. About 20-30gm of bile acids are produced per day, but 90% are reabsorbed via the enterohepatic circulation where they are reused and recycled 10-12 times per day.
Bile has two main functions: It aids the in the solubilization and digestion of fats including cholesterol and fat soluble vitamins, and it eliminates certain waste products – mainly hemoglobin and excess cholesterol from the body. Within the bile itself, the bile acids and phospholipids solubilize the cholesterol, thus preventing its precipitation.
While bile acids are important in fat digestion, they do not actually digest it. Rather, they help emulsify fat particles into smaller particles to facilitate the digestive process. The net effect is to expose active receptors that enable the pancreatic lipases (enzymes) to act. They also continue to facilitate polar-non-polar molecular interactions by aiding in the absorption of these digested fat products through the intestinal mucosa and into the lymphatics of the small bowel.
Bile salts are also an important vehicle for excretion. Two important excreted solutes are bilirubin (which once conjugated is not water-soluble and thus can not be excreted through the kidneys) in appreciable amounts, as well as cholesterol.
Bile is a noxious substance when not confined to the tubes of the digestive tract. Bile in the peritoneal cavity causes bile peritonitis which is a potentially fatal disease. Jaundice is a clinical sign indicating excessive bilirubin in the serum. This has many causes but in general is obstructive, hepatocellular or hemolytic in origin.
From a diagnostic point of view, excessive bilirubin in the body is diagnosed clinically by looking at the sclera and skin color, and by evaluation of serum bilirubin. Ultrasound is helpful to exclude obstructive causes.
The treatment of jaundice depends on the cause, with surgical treatments usually indicated for obstructive causes, and medical treatments for hepatocellular or hemolytic causes.
Receive, Process, and Export: Bile Handling by the Gallbladder
The gallbladder is central to bile concentration and delivery. As we have learned in the module on structure, its design provides certain features that optimize its function. It consists of an incomplete muscular wall, which at a histological level contains mucosal fronds that absorb water and concentrate the bile. It has an unusual spiral cystic duct that optimizes the transport of bile to and from the gallbladder. The size, shape, and position of its component parts are optimized to enable the receipt, concentration, storage, and transportation of bile.
The gallbladder has to store and concentrate bile and this occurs in the same chamber. The more capacious fundus and body lie relatively inferiorly. During the day, with the person in the upright position the fundus will contain the oldest and most concentrated bile because of its most caudal and gravity dependant position.
Courtesy of: Ashley Davidoff, M.D.
Receive, Process, and Export: Receiving
As the bile secretion flows from the hepatocytes to the bile ducts via the bile canaliculi, a secondary secretion of water containing sodium and bicarbonate ions from the epithelial cells lining ductules occurs, resulting in a total volume for an average human adult of between 600-1000mL daily. The bile ducts are gracile and of low volume, with a maximum normal pressure of about 20cm of water when the sphincter is closed, and which falls to 10cm of water or less as the sphincter opens. With the sphincter of Oddi closed and the cystic duct open, overflow of bile into the cystic duct occurs as a result of the small rise in pressure.
The cystic duct has an upward course to reach the neck of the gallbladder since in the upright position, the neck of the gallbladder is more cranial than the cystic duct/bile duct junction. During the day we are upright, whether we are walking, standing, or sitting it is an uphill climb for bile to reach the cystic duct.

The biliary system is a low pressure system under normal circumstances. The upward direction for the bile, from the bile duct to the cystic duct is against gravity and there is no pump to push it nor a mechanism to pull it . While the sphincter of Oddi is closed between meals, nature has devised a way to ensure that bile reaches the gallbladder with the least effort on its part. Nature and not Archimedes nor Nebuchadnezzar was the first to think of the water screw. It is simply elegant!
Ashley Davidoff, M.D.
The spiral valves of Heister have been a puzzle for many years. We theorize that they have been ingeniously designed to hold and pass on the bile during this ascent against the forces of gravity, in much the same way that Archimedes design of the water screw helped the delivery of water from a low source to a high receptacle, also going against the force of gravity, and with the least energy expenditure.
In the body there is no handle to turn the valves (screws ) of Heister. There are hydrostatic forces from below caused by the continued 24hour production of bile by the liver at about the rate of 1/2cc per minute. (approximately 800ccs in 24 hours, = approximately 1/2cc per minute)
The maximum secreting pressures of bile from the hepatocytes is approximately 30cm of water. The resting pressure of the sphincter of Oddi is 12-15cm of water, the opening pressure of the cystic duct is 8cm of water and the opening pressure of the gallbladder is 10cms of water. Thus when the sphincter is closed the lowest pressure is in the cystic duct and hence filling of the cystic duct occurs. (Clavien)
As the new drop of bile spills into the bile ducts it will cause a minute rise in pressure against the closed sphincter of Oddi. Flow in the system is directed toward the cystic duct offers the least resistance as described above. Bile will therefore fill the first valve which will push the bile upward to the second valve and so on. With this repeated many times, each valve is filled until the bile reaches the top of the ladder after which it will spill over like a waterfall into the neck, and then body, and finally into the fundus.
The sphincter of Oddi is composed of a ring of circular and longitudinal muscle at the distal end of the common bile duct which has a phasic resting pressure of about 13mmHg. It has a cyclical pattern during fasting that works in concordance with the intermittent myoelectric migratory complex of the intestinal tract (IMMC), as well as a pattern specific to the presence of CCK and the parasympathetic nerve supply.
The common bile duct unites with the pancreatic duct to form a common channel called the ampulla of Vater which empties into the duodenum at the papilla which is seen as a small nipple in the middle of the descending duodenum.
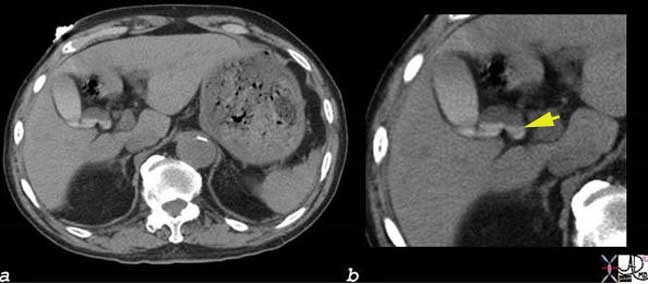
The CT scan through the liver and gallbladder shows contrast layering in stepwise fashion in a dilated cystic duct. The contrast in the gallbladder is from a recent CT scan. This entity is called vicarious excretion of contrast and represents the normal excretion of intravenous contrast by the liver cells seen as dense material within 24-48 hours following intravenous injection. It becomes more prominent in patients with renal failure. The stepwise appearance of the contrast as a fluid-fluid level, adds credence to the theory of the parallel drawn and mechanism of function of the valves of Heister and Archimedes water screw.
Images courtesy of: Ashley Davidoff, M.D.
Receive, Process, and Export: Mechanisms of Control
In between meals the sympathetic nervous system governing the gallbladder is relatively active and the parasympathetic system and CCK hormone are inactive. Hence the sphincter of Oddi under the sympathetic control of the greater splanchnic nerves is contracted, and the gallbladder smooth muscle is relaxed. With a fatty meal, release of CCK is instituted and it acts as the primary mechanism of smooth muscle and sphincter control. The parasympathetic system provides accessory control with the right (posterior) vagus causing the sphincter to relax and the left vagus causing the gallbladder wall to relax.
It is becoming more apparent that the neural and hormonal control of bile release into the duodenum is not as tightly regulated by meals and that the sphincter of Oddi has periods between meals when it is relaxed and the gallbladder has phases when it contracts and partly empties between meals as well. It is also well known that only half the bile produced by the liver enters the gallbladder and so it infers that the ampulla opens intermittently between meals to allow non concentrated bile into the duodenum. We alluded to the intermittent myoelectric migratory complex of the intestinal tract (IMMC) which is a cyclical contraction pattern that coordinates muscular activity of the bowel and has emptying effects on the biliary system.
Receive, Process, and Export: Processing – Concentration of Bile
The shape and position of the gallbladder are well designed to enable bile concentration. The bile in the fundus and body is mostly “old bile” and represents about 90% of the gallbladder volume since they are the most capacious parts of the gallbladder, most dependent in position, and contain the heavier, already concentrated bile.
The new bile which is delivered to the gallbladder is small in volume, relatively dilute, has a relatively low specific gravity, and consists of water (97% ), bile acids (1-2%), and other metabolites and electrolytes that make up the remaining 1-2%. The “other” components include cholesterol, phospholipids, bile pigments, sodium and chloride. The major cation is sodium and the dominant anion is chloride. Small amounts of potassium, calcium, and approximately 20?50 mM bicarbonate are present. Bile acid concentration is approximately 30-50mM. Hepatic bile is isotonic with plasma.
Once the bile comes into contact with the mucosal surface, about 90% of the water is reabsorbed, allowing the large volume of biliary secretions to be stored and concentrated in a space that can accommodate only 60-80cc. The concentration is achieved by the active absorption of electrolytes and passive absorption of water. Typically the gallbladder can concentrate the bile from 5-6 fold, but this can increase to 10-12 fold. Thus for every 100ccs of dilute bile received, between 10 and 20cc of concentrated bile is produced. It is now becoming apparent that only half of the bile production goes through the gallbladder so the gallbladder may only “see” and concentrate between 250-500cc per 24 hour period. The concentration of bile acids increases by 10 fold, and the sodium and chloride concentrations are reduced significantly. The concentration of divalent calcium although low, is relatively high when compared to monovalent anions because phenomenon called the Gibbs-Donnan effect which favors the relative accumulation of divalent anions in the proteinaceous milieu that exists.
From a practical perspective, it is routine to have a patient fast (usually overnight) for 8-12 hours before an ultrasound exam when the gallbladder is optimally distended without being dilated. The wall is better evaluated in full distension, and stones that may hide in the neck or infundibulum are seen to better advantage as they are surrounded by the anechoic bile.
Receive, Process, and Export: Storage
The storage of bile is not as static as one would imagine. During fasting, there is continued cyclical myoelectric activity in synchrony with duodenal activity called intermittent myoelectric migratory complex of the intestinal tract (IMMC) which we have discussed above. This results in gallbladder contraction between meals, with an open sphincter and with 15-20% emptying. Motilin is a polypeptide secreted by the small intestine probably as a result of an alkaline PH in the duodenum and is associated with the IMMC. Despite the cyclical contractions, there are still prolonged periods of “down time” of muscular activity where storage of the bile occurs enabling the process of bile concentration to occur.
Static bile accumulates in the fundus and spends the majority of time in the fundus since we are in the upright position most the time. Sediments of bile salts, stones and inflammation are therefore dominant in the fundus and it is not surprising therefore to find that 60% of gallbladder cancers occur in the fundus, 30% in the body, and the least (10%) originating in the neck.
Receive, Process, and Export: Export Function
While we have stressed the apparent simplicity of gallbladder function, the muscular function of the gallbladder brings this notion to a screeching halt. Even during the fasting state bile is delivered through the ampulla at about the rate 0.5 to 1ml/minute. At peak flow postprandially, this may increase to 2-3ml per minute.
The engines of delivery start to rev up even as we think of the meal we are about to partake in. This is called the cephalic phase of digestion and it affects the gallbladder as well. The mere thought, sight, or smell of food stimulates the parasympathetic neural axis to the gallbladder resulting in stimulation of the vagus nerve and its effects on the smooth muscle.
When the fat-rich or protein rich foods reach the duodenum (typically 30 minutes postprandially), CCK, the primary regulator of gallbladder contraction and Oddi function is released by the duodenum into the blood stream resulting in a serum CCK that rises over 15 to 30 minutes and then slowly plateaus. The response is not all contraction by gallbladder muscle nor all relaxation by the sphincter. Instead there is a contraction and relaxation pattern designed to provide a sustained, slow and steady stream of bile, with emptying occurring over two hours.
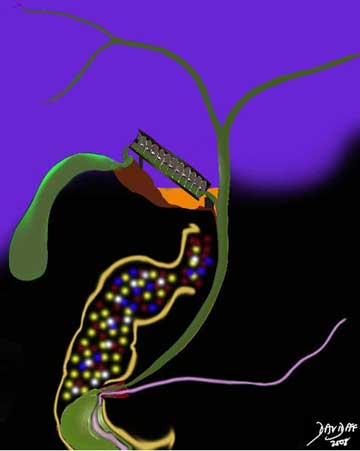
The delivery of bile and pancreatic secretions are slow and steady in response to fat (yellow) protein (red) in the diet which causes the release of CCK into the blood which in turn acts on the smooth muscle of the gallbladder and sphincter resulting in open juice gates and steady flow of bile and pancreatic enzymes over two hours. The spiral valves (downhill Archimedes water screw) prevent over distension of the bile duct during the delivery phase. Carbohydrates (white) have little effect on CCK.
Courtesy of: Ashley Davidoff, M.D.
The contraction pattern is even more complex it seems. During the postprandial phase a triphasic pattern; early emptying, early refilling, and late emptying seems to be an overall pattern. Duration of each of the triphasic phases includes emptying (40 minutes), refilling (10 minutes), and emptying again (100 minutes) and it takes over two hours to occur during following a meal.
In addition to the triphasic pattern there also appear to be contraction and relaxation phases that occur minute to minute and are of a rhythmic nature.
The spiral valves of Heister prevent the rapid over distension of the bile duct during the phases of contraction and also play a part of providing the slow and steady stream of bile into the bile duct and therefore into the duodenum.
CCK also affects the acinar cells of the pancreas and stimulates the production and transport of pancreatic juices to the duodenum at the same time. these juices among many enzymes also contain lipases.
The gallbladder in the fasting state is distended and its ability to deliver bile and contract can be evaluated by ultrasound or by nuclear medicine techniques. Pre (fasting) and post prandial volumes can be assessed.

Ashley Davidoff, M.D.
Cholelithiasis
Cholelithiasis or gallstones are the result of a metabolic disorder of bile metabolism caused by an increase in the insoluble portions of bile relative to the solutes which keep them in solution, and resulting in precipitated solutes of biliary secretions in the gallbladder. Gallstones are more common in women, and are associated with diseases relating to cholesterol metabolism, diabetes mellitus, hemolytic anemia, and cirrhosis.
The resulting concretions (formation of solid material into particles) are common in the Western world, (8% in the population at large and 10-15% in ages 40-60)) and more commonly than not of no clinical significance. However, occasionally they may impact in the neck, cystic duct or common bile duct, causing obstruction in the biliary tract. The obstruction progresses to inflammation and acute cholecystitis, or cholangitis may result.
There are three forms of stones:
- Cholesterol
- Pigment
- Mixed
The most common stones are cholesterol stones, which account for 75-80% of cases. The next most common are pigment stones, which account for approximately 15% of all cases. The remainder of the cases are mixed stones, representing a combination of cholesterol and metabolic varieties. An aberration of cholesterol metabolism causes an imbalance between cholesterol and the bile acids, phospholipids and lecithin which keeps the cholesterol in solution. Similarly, increased bilirubin metabolism from the breakdown of hemoglobin, usually due to hemolysis, causes an increased excretion of bile pigments, leading to stone precipitation. These are called black pigment stones. An additional type of pigment stone is the brown pigment stone. This is associated with intra-hepatic infection, and is seen mostly in Asian populations.
Structurally, cholelithiasis is characterized by the presence of rock-like crystals in the dependent portion of the gallbladder. There is no characteristic change in the size or shape of the gallbladder unless an obstruction occurs. The stones vary from small crystals in the sub millimeter range to very large stones which may occupy the whole gallbladder. They may be round, oval, or faceted. Calcification may be dense, or minimal, diffuse, laminated, or heterogeneous.
Although there is no functional change with the presence of stones in the gallbladder itself, in later phases obstruction can impair excretion of bile salts and digestion. Aberrations in metabolism of cholesterol and hemoglobin predispose to the formation of gallstones.
Cholelithiasis : Clinical Presentation
Clinical presentation of patients varies with the staging of disease:
- Asymptomatic: stones are merely present in the gallbladder and may be incidental findings on abdominal imaging.
- Symptomatic: patients may have colicky RUQ pain, often radiating to the right shoulder (transient impaction without inflammation)
- Complicated: RUQ pain, fever/leukocytosis (impaction with inflammation)
The symptomatic stage is characterized by 1-5 hour bouts of pain, usually after meals, and may recur. It may progress to the complicated stage, where pain is of longer duration and accompanied by symptoms of infection.
Stones are easily diagnosed by ultrasound, (95%), but are seen by CT as well (80-85%). The stones that are not seen by CT are usually cholesterol stones which are isodense with bile and very small, non calcified stones. In the absence of obstruction, scintigraphy with HIDA scan provides little information, though in patients who have progressed to symptomatic and complicated stages, it is the most specific study for the diagnosis of an impacted stone in the neck or cystic duct.
Treatment depends on the staging. If asymptomatic and found incidentally, patients may be followed. If symptomatic, patients may have elective cholecystectomy. In the complicated stage, patients are hospitalized, and treated with IV antibiotics. Elective cholecystectomy is performed after a ?cool-down? period.

This photograph shows examples of the most common gallstones, which are a mixture of bilirubin, cholesterol, calcium carbonate and other components. They are usually multiple, multifaceted, and about 0.5 ?1.0 cm on a side. Note the small stone cut across which has a yellow rim and a dark green center. This is a combined stone with a bilirubinate center and a cholesterol-containing rim.
Courtesy of: Barbara Banner, M.D.
Cholelithiasis : Imaging Stones
The size of gallstones can vary from tiny submillimeter crystals to stones that occupy the entire gallbladder.

The smallest gallstones are seen as sub millimeter, floating, echogenic foci that represent crystals of cholesterol. They may show comet tail artifact, and as in this case can occupy the entire lumen of the gallbladder.
Courtesy of: Ashley Davidoff, M.D
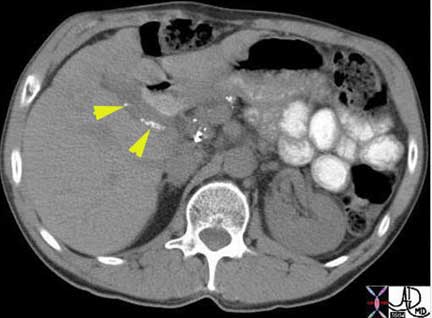
Small calcified stones are more common than floaters, and in this case can be seen lying dependently in the infundibulum of the gallbladder but at least three other smaller stones and two larger are seen in the region of the neck and cystic duct.
Ashley Davidoff, M.D

Medium sized gallstones are seen on this longitudinal view of the gallbladder lying dependently in the neck.
Ashley Davidoff, M.D
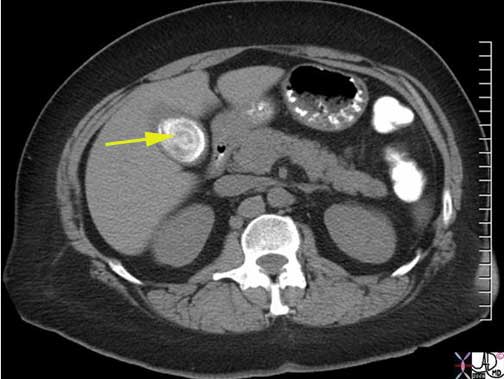
The CT scan shows a large, calcified, layered stone occupying almost the entire lumen of the gallbladder.
Ashley Davidoff, M.D
Acute Cholecystitis
Acute calculous cholecystitis is an inflammatory condition of the gallbladder caused by obstruction of the cystic duct, usually by small gallstones.
Structural changes include an inflamed, and distended gallbladder with a hyperemic wall. There is no specific functional impairment per se as a result of the disease, except that less concentrated bile reaches the duodenum.The disease may be complicated by perforation and bile peritonitis, and sometimes by empyema.
Clinically, the patient presents with RUQ pain, with malaise and usually a fever. A positive Murphy’s sign is almost pathognomonic.
The diagnosis is best made by combining the clinical presentation of right upper quadrant pain, positive Murphy’s sign, history of cholelithiasis, with ultrasound findings of a distended hyperemic gallbladder that contains stones, fluid or complex stranding in the gallbladder fossa and probe tender gallbladder. The stones when impacted in the cystic duct are rarely visualized.
When the diagnosis requires confirmation, the most specific study is a HIDA scan. CT scan is helpful to evaluate for local perforation, a diagnosis that is suspected when the pericholecystic fat is indurated.
Treatment is usually with elective surgery. In the acute phase the patient is treated conservatively with antibiotics and analgesics.
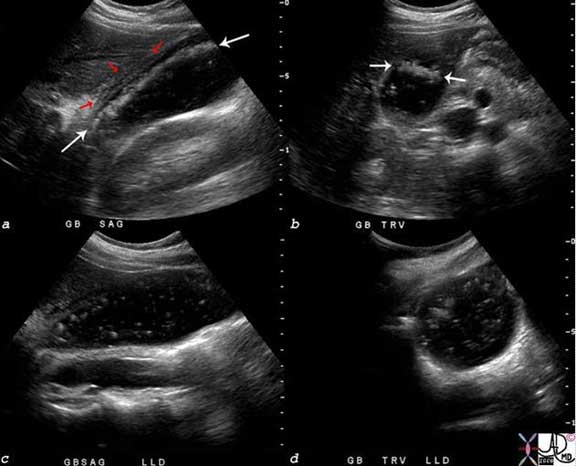
The ultrasound scan is from a young female who presented with right upper quadrant pain and positive Murphy?s sign ? a clinical sign that is consistent with acute cholecystitis. The scan shows multiple floating stones (white arrows) in the longitudinal view (a) and in the transverse view (b). There are complex changes in the gallbladder fossa (red arrows) characterized by fluid and linear echoes, both characteristic of acute cholecystitis. Perturbation of the stones disturbed the layering effect and the crystals were seen floating throughout the lumen.
Ashley Davidoff, M.D
Acute Cholecystitis: Imaging
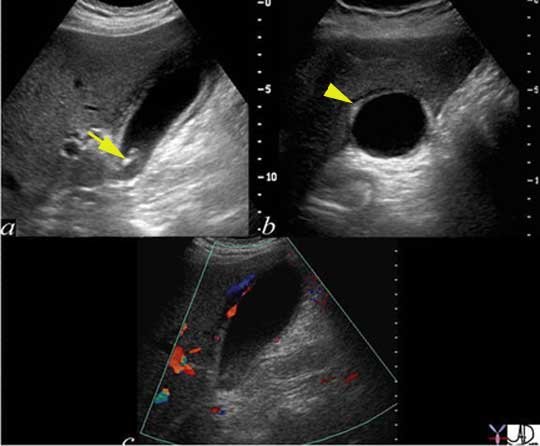
The three images depicted above are from a patient with acute cholecystitis. The image (a) shows the gallbladder in longitudinal axis, with shadowing stones (arrow) in the neck of the gallbladder, a thickened wall, and complex fluid (arrowhead) in the gallbladder fossa. Image (b) shows the gallbladder in transverse view and again shows the complex fluid and soft tissue changes in the gallbladder fossa alongside the liver. Image (c) shows a longitudinal view of the gallbladder with hyperemia in the gallbladder wall abutting the gallbladder fossa, as depicted by color flow doppler.
Ashley Davidoff, M.D
The most sensitive examination for acute cholecystitis is the HIDA scan, which when normal will show the gallbladder filling approximately 30-60 minutes following technetium injection. If the gallbladder does not fill, it correctly implies that the cystic duct is obstructed. In the appropriate clinical setting, the lack of filling of the gallbladder is pathognomonic for acute cholecystitis.
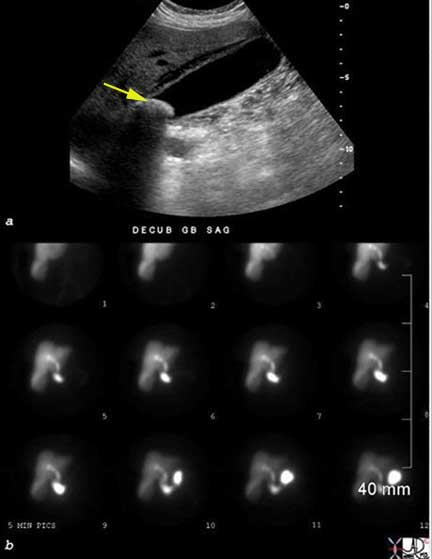
This young patient presented with right upper quadrant pain. A fairly large stone (arrow) impacted in the infundibulum on the longitudinal view of the ultrasound is shown. Fluid is also noted in the gallbladder fossa. The HIDA scan shows non visualization of the gallbladder at 60 minutes, despite the filling of the small bowel. These findings are consistent with the diagnosis of acute cholecystitis.
Images of: Ashley Davidoff, M.D.
If the inflammation and ischemia are ongoing the wall breaks down and transudation or leakage of fluid occurs in the pericholecystic fat. This is best visualized by CT scan. This finding suggests an advanced form of the disease and treatment becomes emergent.
A second complication to consider although not as common, is abscess formation which most commonly occurs in the gallbladder fossa. The fluid that has collected in the gallbladder fossa becomes secondarily infected and an abscess forms. This needs to be drained and percutaneous techniques are best suited to do this.
Acalculous Cholecystitis
Acalculous cholecystitis is an inflammatory disease of the gallbladder that is not related to stone disease and is primarily and initially a consequence of atony of the gallbladder caused by prolonged fasting and a consequent lack of CCK stimulation. The patients who have prolonged stay in the ICU and more specifically those who have sustained burns, trauma, or major surgical intervention – all entities that require prolonged ICU courses, are at risk for this entity. Although it often occurs in the inpatient setting, it may occasionally occur in outpatients. Patients with hyperemesis gravidarum for example can present with acalculous cholecystitis.
Structurally, the gallbladder shows distension and is without cholelithiasis. The lack of CCK stimulation results in a gallbladder which is atonic, and which becomes distended, since bile is continually produced and not distributed.
Functionally, the gallbladder is atonic and fails to transport bile to the ampulla.
The tension on the wall renders it ischemic and susceptible to infarction, infection and bile infiltration. An inflammatory process supervenes.
The clinical presentation is one of an ICU patient who has a fever of unknown origin or who has right upper quadrant pain or tenderness usually with a positive Murphy’s sign.
From an imaging standpoint, ultrasound is the study of choice since it shows findings similar to acute cholecystitis but no stones are present. The gallbladder is distended, the wall may be thickened, and there may be fluid in the gallbladder fossa. Hyperemia is usually present, and probe tenderness is commonly elicited when the patient is conscious and communicative. CT is also useful particularly for the evaluation of changes in the surrounding fat which if present would suggest rupture of the wall.
Acalculous cholecystitis may be complicated by gangrenous changes in the wall which could manifest radiologically with extremely thin walls, empyema, abscess formation or perforation with bile peritonitis.
Acalculous cholecystitis is best treated with percutaneous cholecystostomy, which serves to decompress the gallbladder.

The longitudinal view and transverse view of the gallbladder shows a mass-like tumefactive bile. This is a sign of advancing cholestasis. The wall is not thickened and there is no fluid in the gallbladder fossa. Cholestasis and not cholecystitis is apparent.
Ashley Davidoff, M.D.

Ashley Davidoff MD
Hyperplastic Cholecystoses
The hyperplastic cholecystoses represent non inflammatory gallbladder disorders including cholesterolosis and adenomyomatosis that are grouped together under the name but are structurally and pathologically quite different. While cholesterolosis is an accumulation of cholesterol deposits in macrophages of the lamina propria, adenomyomatosis is a hyperplastic disorder of the mucosa where diverticula of the mucosa protrude outward. They will be discussed separately.
Hyperplastic Cholecystoses: Adenomyomatosis
Adenomyomatosis is a hyperplastic disorder of the mucosa.
The cause is uncertain, but it has been linked with increased intraluminal pressure in the gallbladder and to hyperconcentration, hyperexcretion, and hypercontractility of the gallbladder.
Structurally, the disorder is characterized by a proliferation of surface epithelium, extending into the muscularis resulting in diverticuli called Rokitansky-Aschoff sinuses. The epithelial layer and lamina propria invaginate and penetrate through the lamina to the muscular layer which often is thickened up to 3-5 times normal. The abnormality may be localized or generalized. The fundus is usually involved in the localized variety.
Functionally, no changes in biliary or hepatic function are present, and hypercontraction is not always present.
There is no definite clinical correlate but it may be the cause for otherwise unexplained right upper quadrant pain and bloating.
Imaging by oral cholecystography was in the past diagnostic, but US and CT now offer the studies which best demonstrate the disorder.
Treatment is not described for asymptomatic patients. If no explanation for persistent right upper quadrant is found and there is evidence of adenomyomatosis, cholecystectomy may be helpful. Medical therapy is not indicated.
Hyperplastic Cholecystoses: Cholesterolosis
Cholesterolosis is a proliferative disorder of the gallbladder mucosa and is part of a disease group called the hyperplastic cholecytose
The cause of the entity is not known but it occurs more commonly in females in 4th-5th decade and is seen commonly (30%) in cholecystectomy specimens.
The result is the deposition of deposits of lipid, comprised of cholesterol esters and triglycerides in macrophages within the lamina propria and mucosa. Aberrant cholesterol metabolism and the subsequent sequestration of lipids in macrophages (foam cells) is a process similar to that in atherosclerosis, but is of unknown clinical significance in this organ.
Structurally, there may be localized accumulation or diffuse distribution. In the localized form the polyps can vary in size from 1-10mms. The polypoid form may demonstrate echoes projecting into the lumen of the gallbladder.
In the diffuse form the yellow accumulations are often seen in the background of a hyperemic mucosa so that the appearance macroscopically is reminiscent of a strawberry.
There seems to be no functional correlation.
The diagnosis is often made by US scan or CT. US has a fairly characteristic appearance. The polyps are seen as echogenic foci in or on the mucosa, and the polyps show no shadowing and are attached to the wall of the gallbladder.
The entity is not usually treated since most believe there is no clinical significance. In patients with right upper quadrant pain that cannot be explained and who have cholesterolosis some data suggests that cholecystectomy may be beneficial.

Note the yellow cholesterol deposits on the bright red inflamed and congested mucosa resulting in an appearance reminiscent of a strawberry
Ashley Davidoff MD
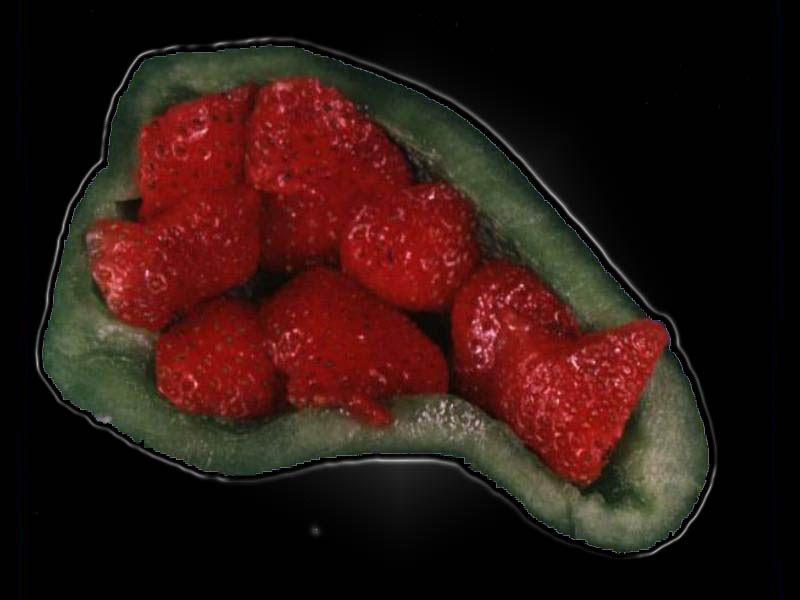
Ashley Davidoff MD

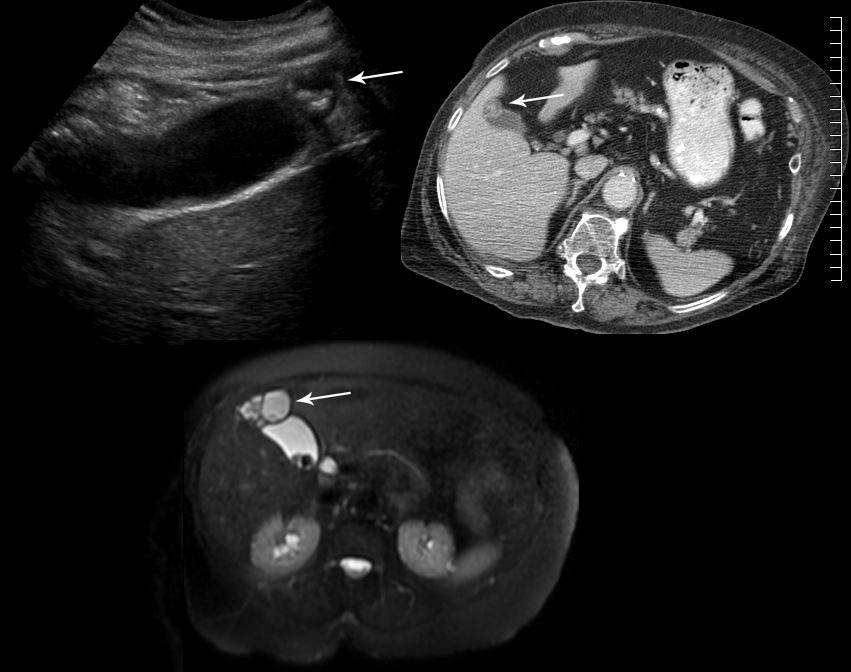
Courtesy Ashley Davidoff MD
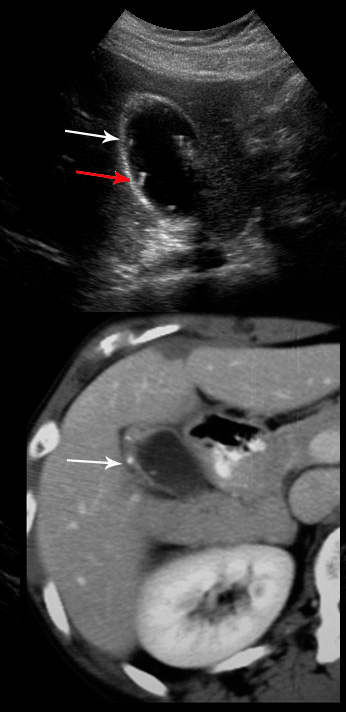
Courtesy Ashley Davidoff MD
Summary
In summary, the gallbladder proves to be quite a marvelous organ. Its shape and size are reminiscent of the uterus and they have both been assigned the givers and receivers of life in some way by ancient medicine, and also by the Sangoma who is the Zulu witchdoctor who wears the gallbladders of goats in her headdress as a reflection of this notion. Gall and bile are used extensively in literature and it seems remarkable that Shakespeare knew that the pigeon did not have a gallbladder. Its position and shape are well designed to support its function which in the end seems not particularly vital as we understand it. Yet structure and function are quite elegant. The valves of Heister are a marvelous invention of nature, revealing that receiving, processing and delivery of bile by the gallbladder is not a simple black and white process. It requires complex interactions of neural, hormonal and muscular actions exerted on a structure that is more than a musculomembranous sac with a duct. Many people accumulate gallstones of wide variety and acute cholecystitis is therefore relatively common. It is caused by a stone getting stuck in the narrow outlet channels of the gallbladder. Acalculous cholecystitis caused by prolonged fasting usually in the ICU is a challenging disease as well. Contemporary imaging seems to be able to diagnose most conditions of the gallbladder with ultrasound being the workhorse modality. Treatment is usually surgical but interventional radiology is an essential arm in treatment, particularly of acalculous cholecystitis.