Learning Objectives
-
- Explain the pathology of pain
- Discuss the clinical approach to pain
- Describe the universal pain assessment tool
- Discuss the imaging techniques utilized
- Explain the therapeutic approach and options
Introduction
In the first introductory module, “Clinical Strategies – Anatomy and Physiology of Pain” we addressed the basic science of pain and explored the structural basis, the pathways and the physiological basis of pain. We identified the complex mechanisms and often individualized nature of the response to pain. In this second introductory module we apply the lessons learned in the first module, and explore the diseases that cause pain, how we in general approach the diagnosis of pain, both from the clinical aspect as well as from the imaging perspective, and lastly the basis for pain therapy. The series that follows thereafter take particular body regions or organs and provide a more detailed look at pain.
Diseases – Basis for Pain
As shown in the section on classification of pain in the basic science series and repeated in the diagram below, there are many disorders that cause pain.
Acute somatic pain signifies imminent and possibly dangerous bodily injury. Its presence evokes an immediate reaction either with a simple reflex or complex reaction. The pain comes and goes and the body as an organism proceeds in a normal fashion thereafter. The pain becomes an experience of the past and is memorialized as a learning experience in the brain. The result is a better prepared response to a similar insult in the future.
Disease, however, happens! It comes in the context of many pathologies and the body does not like it. Inflammation is commonly the underlying pathophysiology for many of the disorders. Disease is usually (but not exclusively) an intrusion of the visceral sensory system and although the discomfort is still classified as pain, the experience is very different from the acute somatic experience described above. The pain of disease begins as one experience, but may often fluctuate in parallel to the dynamic reactions of the body as it attempts to counteract the natural history of the inciting process.
Traumatic injury, as in the case of a bone fracture, is easily understood in this vein. On an average of 4-6 weeks healing time, the pain gradually subsides. The inciting injury and bodily response are both finite and predictable. If on the other hand a chronic progressive or slowly healing disease ensues, then the pain syndrome will reflect the net result of healing versus ongoing pathology.
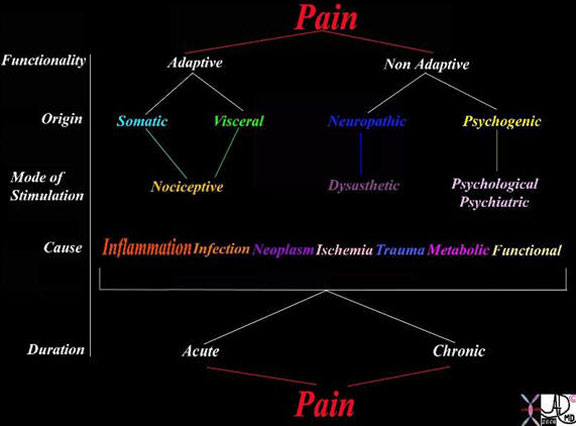
This table explores the variety of ways of classifying pain. The left hand column reveals the classification based on functionality, origin, mode of stimulation, pathological causes and relationship of pain to chronicity. As for functionality, it may be adaptive or non-adaptive. The pain may originate from somatic or visceral nociceptors or from damaged nerves in which case it is called neuropathic, or it may be psychogenic. The causes are usually via the inflammatory process but may result from any of the diseases listed.
Courtesy of: Ashley Davidoff, M.D.
However, when disease directly impairs the nervous system, the pain becomes neuropathic and not necessarily related to either the aggressiveness of the disease or healing. This is more complex and harder to treat. Such pain occurs with chronic inflammation, chronic ischemia and malignant disease, for example. This pain is less dependent on healing rates but more so on the premise of whether or not healing occurs at all. Neuropathic pain can become debilitating and sometimes unrelenting.The complexity that may be added by ongoing social, cultural, and psychological responses makes this the most difficult pain to comprehend on a physical level. We will discuss neuropathic pain in the organic disease section which follows.
Disease
The mechanisms through which patients experience pain differ according to the injurious process and tissue response. We will describe the classical disease processes, each with a unique mechanism and subsequent pain signal. The diseases that involve the somatic receptors tend to present with acute pain. Examples including skin lacerations, meningitis, pericarditis, pleurisy, peritonitis, and periostitis cause sharp pain. As you may have noted the suffix, “itis” in many of these conditions, tells us that these are all of an inflammatory nature.
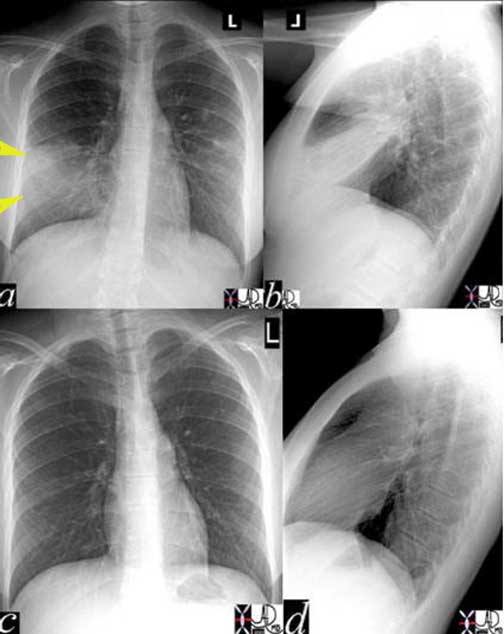
The chest x-ray in A-P and lateral projection show a pneumonia as a dense area in the right upper lobe (a and b). The pneumonia abuts the pleural surface and incites inflammation of the pleura and causes pain. Images (c) and (d) show return to normal 4-6 weeks after initiation of treatment after which time both the pneumonia and the pain have resolved.
Courtesy of: Ashley Davidoff, M.D.

The diagram shows an area of pneumonia (yellow) of the right upper lobe that touches the visceral pleura. The visceral pleura is in intimate contact with the parietal pleura and thus both components become inflamed. With normal breathing, these two surfaces rub each other, and in the case of inflammation they rub each other the wrong way, resulting in pleuritic pain. The pain restricts deep breathing in an attempt to “rest” the pleura, but a pleural effusion, commonly a result of pneumonia, would separate the two by creating a neutral zone between them, and thus prevent their physical contact. The concept of a neutral buffer zone is not a new concept in the ancient discipline of biology.
Courtesy of: Ashley Davidoff, M.D.
Diseases that incite the visceral nociceptors commonly evolve from an increase in pressure within an organ. Distension forces may cause physiological cramps due to “gas pain”, menstrual cramps, and labor. More serious cramps may be caused by obstructive disease processes like bowel obstruction, renal colic, and biliary colic. Many diseases like acute cholecystitis, appendicitis, and cholangitis are a combination of the two.
pain-004-1.jpg
Distension and PeritonitisThe CT scan through the abdomen is from a patient with acute cholecystitis. It shows a gallbladder that is distended and is associated with inflammatory exudate surrounding the gallbladder (arrows) and an inflamed area of peritoneum. The pain arises from both the visceral nociceptors due to increased luminal pressure and somatic receptors of the peritoneal lining. The latter pain is aggravated and induced during inspiration, particularly when the examining hand puts some pressure in the right upper quadrant (Murphy’s sign), or by pressure from the ultrasound transducer over the visualized gallbladder (sonographic Murphy’s sign).
Courtesy of: Ashley Davidoff, M.D.
Inflammation
The primary response to any injury in the human body is inflammation. This is an immune mediated defensive cascade of events, initiated by increased vascular perfusion and permeability to the area of insult. Next, a fusion of cellular migration and degranulation leads to a release of peptides that stimulate, among other things, specialized cellular pain receptors known as proteases. Inflammation can worsen pain by causing vascular leakage of fluid and edema, distention of tissue and/or promotion of anxiety. The subsequent signals generated by inflammation cause symptoms that include burning, aching and pressure.
Sensitization of Receptors With Tissue Injury – Changing Thresholds
Within the extracellular space, there are many substances that affect the sensitivity of the free nerve endings, usually to increase the sensitivity or lower the threshold to pain. Inflammation is a classic example as a phenomenon that characteristically induces the production of a variety of extracellular substances that either incite pain or sensitize the nerve endings to pain.
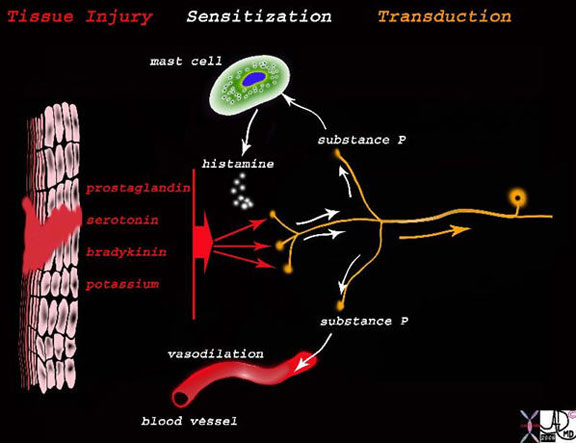
The diagram shows the effect of tissue injury (left side of diagram) that induces the release of prostaglandin, serotonin, bradykinin, and potassium which cause sensitization of the free nerve endings to pain which lowers the threshold to pain. In addition, they induce (red arrows) the axon reflex (white arrows) which causes the production and release of substance P from the free nerve endings, which cause the release of histamine from the mast cells. The histamine causes vasodilation and exudation into the damaged area. Three of the hallmarks of inflammation are explained in the diagram. Pain, swelling (edema) and hyperemia increased blood flow.
Pain, or its Latin equivalent “dolor”, is one of the classical hallmarks of inflammation as was described in the latter half of the second century, AD by Celsus, a Greek philosopher. Anti-inflammatory agents, mild heat, and cooling tend to reduce the inflammatory reaction and thus, reduce the pain. They provide relief by neutralizing the effect of the substances that sensitize or incite the pain.
The pain sensitizing peptide compounds released as a consequence of tissue injury include prostaglandins, serotonin, bradykinin and potassium. They, in turn, stimulate a local axonal reflex causing the free nerve endings to release substance P or calcitonin and some gene-related peptides (CGRP). Substance P and CGRP cause mast cells to release histamine which in turn causes vasodilation and local edema, other hallmarks of the inflammatory process. Some of these substances activate pain through the chemoreceptors including ATP prostanoids and hydrogen ions (acid PH).
This mechanism has one process in mind for you and that is to rest the injured part. A fractured arm becomes hypersensitive to touch or pressure and induces you to hold the part as still as possible, sometimes even employing your other hand and arm to hold the injury as still as possible. This forces one to pure rest to promote healing and to progress without further injury.
Infection
Infection most often manifests as inflammation. However, the pattern and subsequent pain are different. Infection by nature, delays healing. Pain complaints will therefore be more prolonged and progressive. Subsequently, inflammatory pain from infection will endure, deepen or spread until treatment and healing is initiated.

The CT scan in this patient with severe back pain and fever shows destruction of the disc space of T7-T8 as well of both upper and lower involved thoracic vertebra (arrow in b). The transverse image through the space shows bony fragmentation and destruction of the vertebral bodies with bulging paravertebral soft tissue swelling of an evolving abscess (yellow). The red lines reveal somatic visceral periosteal layers that are involved in the inflammatory and infectious process. The pain likely arises from a combination of factors including the swelling caused by the infection (pressure) and involvement of the periosteal, pleural, and joint linings.
Courtesy of: Ashley Davidoff, M.D.
Neoplasm
Pain in the setting of neoplasm may be acute or chronic and variably related to the cancer. Somatic pain is most commonly related to metastatic, bony involvement irritating the periosteum. There may be tumor induced osteolysis with release of prostaglandin E2, which sensitizes the nerves. When the metastases are in the vertebral column, compression fractures or expansile mechanical changes may impinge on the nerves or spinal cord and induce neuropathic pain. Bone involvement may become manifest as a somatic throbbing or aching pain.
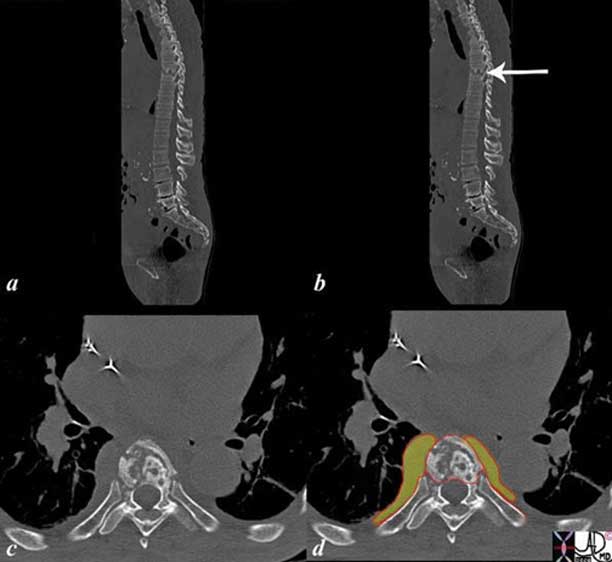
The sagittal reconstruction of a CT scan shows extensive lytic metastases throughout the thoracic and lumbar spine (green overlay in b). A lytic lesion is also noted in the pubic symphysis. The combination of somatic periosteal nociceptor involvement, mechanical nociceptors that sense the expansion, resulting tissue damage and the release of substances that incite the chemical nociceptors, and possibly damage to the spinal cord and resulting neuropathic pain mechanisms, give adequate cause for pain in this scenario.
Courtesy of: Ashley Davidoff, M.D.
When cancer pain is visceral in origin, it is due to pressure effects as the tumor occupies space. In this instance, mechanical nociceptors are stimulated. Alternatively, tissue damage may release a variety of chemicals including cytokines, K+, bradykinin, interleukin and growth factors that stimulate chemical nociceptors and promote inflammation and a decreased pain threshold. Impingement on nerves or the spinal cord may cause neuropathic pain.
Cancer therapy may also cause pain due to tissue burns from radiation or localized pain at the sight of a chemotherapy injection. Pharmacotherapy, specifically the vinca alkaloids platinols or tamoxifen may also cause pain that may be neuropathic.

In this case the 77-year-old female patient presents with right lower quadrant pain. The CT scan shows a napkin ring thickening (green) surrounding the region of the cecum subsequently proven to be carcinoma. When restricted to the cecum alone, the cecal carcinoma tends to be silent since there is neither significant distension nor peritoneal involvement to incite any nociceptors. These patients usually present when complications such as anemia or obstruction surface. In this patient the neoplasm incited an inflammatory reaction in the surrounding fat (pale see through red) and peritoneum (bright red line) witnessed as a subtle thickening of the peritoneum. This was sufficient to stimulate the nociceptors and incite pain.
Courtesy of: Ashley Davidoff, M.D.
Mechanical Disorders
Pressure sensitive nociceptors are positioned in both the somatic regions but predominate in the viscera. Stimulation of the pressure sensitive nociceptors is perceived as aching or throbbing and is characteristic of a range of cramps and colic that are “normal” day-to-day sensations to the more severe pain of childbirth.

The mechanical pressure sensitive nociceptors are dominantly located in the organs and are responsible for sensing pressure changes. The diagram shows a wave of increased pressure (pale yellow) impinging on the free nerve endings of the pressure receptors, with red nerve endings being stimulated by the pressure.
Courtesy of: Ashley Davidoff, M.D.
These pains, however, are seen in pathological situations and the word “ache” or “cramps” seemingly and incorrectly implies a lack of severity. Anybody who has experienced renal colic will tell you that the pain is probably the most severe pain they have experienced. In fact, the stone that can induce the worst pain need only be 2-3 mm in diameter or less.
Another pain pathway in the body arises from gamma sensors located in the muscle spindle apparatus of skeletal muscle. These receptors may be activated at rest or with motor function depending on the source. The most common form of muscular pain occurs after strenuous activity when muscle spindles have become relatively overused through stretching and contracting. The resultant achy pain associated with movement has often been controversially described as secondary to lactic acid and oxygen debt to the muscle fibers. One confounding factor, however, is that neuropathic pain is also transmitted in the same apparatus but at rest. Patients with spinal cord injuries may suffer from muscular pain as part of a syndrome called Central Pain.
Obstruction
Obstruction of any of the tubular systems within the body and particularly of the gastrointestinal tract can cause pain by stimulating mechanical and pressure sensitive nociceptors in the viscera. The afferent nerve fibers are situated within the viscera and are commonly carried by similar afferent fibers of the sympathetic system.
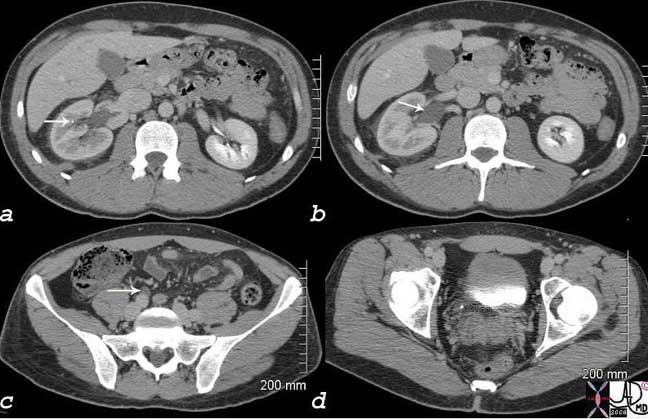
The worst pain of this patient?s life was caused by a 3mm stone in the right distal ureter seen on this non-contrast CT, as a white speck in image (d). In image (a), a similar stone remains in the kidney, (arrow) while image (b) shows mild hydronephrosis, and image (c) shows hydroureter (arrow).
Courtesy of: Ashley Davidoff, M.D.
Less severe forms of visceral pain also occur in other obstructive diseases such as small bowel obstruction. There may be many causes but the most common is adhesions from prior surgery. The pain is often accompanied by nausea and vomiting.

The plain film of the abdomen shows dilated loops of small bowel associated with a paucity of gas in the decompressed large bowel. These findings are consistent with small bowel obstruction and were associated with diffuse abdominal aching pain, nausea and vomiting.
Courtesy of: Ashley Davidoff, M.D.
Distension
The pain described previously is caused by distension but there are other causes of distension that can induce pain. The sudden stretching of a capsule induced by edema, hematoma, or a subacute accumulation of pus can induce pain that can be somatic or visceral.

The MRI through the liver is from a 40-year-old pregnant patient with acute abdominal pain, preeclampsia , elevated liver enzymes, low platelet count, and hemolysis. The MRI shows a 4 cm subcapsular, non-enhancing, subcapsular hematoma, anterior to the left lobe of the liver that caused acute stretching of the liver capsule and severe abdominal pain.
Courtesy of: Ashley Davidoff, M.D.
Trauma
Trauma can cause pain in many ways including local and systemic manifestations. Somatic, visceral, neuropathic, inflammatory, infectious, mechanical, metabolic, and chemical influences all can play a role.

The post operative angiogram of the hand is one of the most painful x-rays I have experienced in my career and the image is older than 30 years. The exact history eludes me but there has been obvious traumatic injury to the hand with multiple fractures (black arrows), a transverse skin incision that contains a broad band of air (white arrow), with probable debridement of the severely injured metacarpal row, and extensive pinning and wiring of the thumb following surgical trauma. The combination of the large somatic sensory nociceptor supply to the hand, with the extensive skin, bone, and tissue damage, creates a scenario of extreme pain. It is difficult to perceive the extent of the pain that this poor patient went through. The remarkable feature is the maintenance of blood supply to the hand, despite the extensive injury to harder but less pliable bones.
Courtesy of: Ashley Davidoff, M.D.
Ischemic Pain and other Circulatory Disorders
Insufficient perfusion of tissue leads to hypoxia which is usually manifested as pain. The discomfort may be somatic as in the classic muscular ache of claudication, or visceral as described by waxing and waning abdominal pain of ischemic bowel syndrome. The pattern of provoking or relieving factors are helpful descriptors in characterizing the supply and demand mismatch of compromised blood flow.
The biochemical changes by nature are complex, but include the loss of high-energy compounds and acidosis due to anaerobic production of lactate. Hydrogen ions are potent stimulators of pain nociceptors. Other algesiogenic chemicals include substance P, K+, kinins, interleukins, adenosine, histamine, and leukotrines. Adenosine has strong associations with ischemic pain as well.

Courtesy of: Ashley Davidoff, M.D.
Angina is a common and often debilitating manifestation of ischemic disease. In this case, there is deficiency of oxygen to cardiac muscle inducing discomfort with exercise that is relieved by rest. The underlying cause is narrowing of the coronary arteries by atherosclerosis.
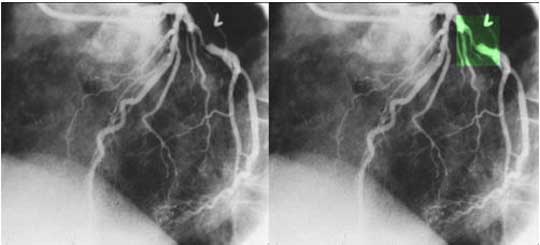
The coronary angiogram in the LAO projection shows a severe proximal stenosis (> 70%) of the circumflex with some post stenotic dilatation. The second image has a green overlay indicating the region of disease with the post stenotic dilatation. This lesion is considered hemodynamically significant. The narrowing causes angina due to poor oxygen supply and resulting depletion of high-energy compounds and acidosis due to anaerobic production of lactate, hydrogen ions, and adenosine.
Courtesy: Ashley Davidoff, M.D.
Other Vascular and Circulatory Disorders
Migraine
The blood vessel wall is richly endowed with nociceptors and the pain of migrainous headaches are thought to have a vascular origin. The newer neurovascular theory suggests that the inciting event is a cortical disorder that subsequently causes the vessels to vasodilate and constrict. It is these events which are responsible for the pain.
Venous Congestion
Venous congestion can cause pain on many levels. It is classically seen in patients with acute inflammation. Due to a combination of higher pressures, chemical forces and the vascular response, edema ensues, causing and contributing to the pain. In other patients, the venous congestion may cause swelling of the involved organ and an increase in visceral pressure thus stimulating nociceptors. In patients with acute tricuspid regurgitation, swelling of the liver causes distension of the liver capsule and a somatic type pain. Pelvic congestion syndromes seem to arise from pelvic varicosities commonly acquired during pregnancy and the source of a constant dull pelvic ache. A tiredness or discomfort of the legs is a similar symptom that patients with varicose veins complain of.
Other Vascular and Circulatory Disorders : Hemorrhage
Hemorrhage can cause a variety of pain syndromes ranging from no pain at all such as occurs in a GI bleed, to a mild visceral ache from a muscle bruise, to incapacitating headache pain caused by rupture of a berry aneurysm in the brain.
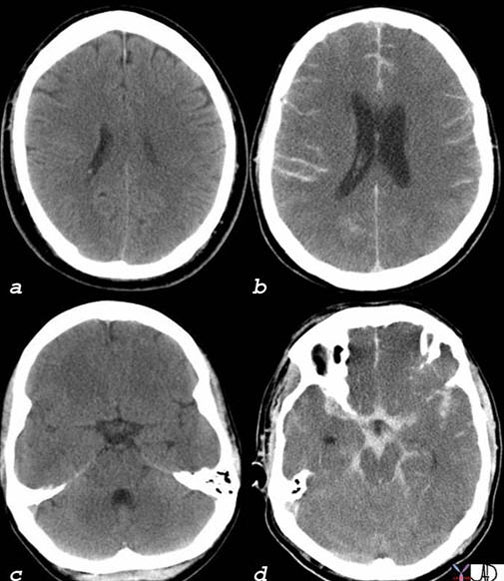
These two head CT’s are from two different patients who both presented with severe headaches. The first patient (a, c) had a normal study and the headache may have been caused by migraine, cluster, or tension headaches, for example. Although these headaches create significant morbidity they are relatively benign in that they are treatable. The second patient (b, d) had a life-threatening subarachnoid hemorrhage due to a ruptured aneurysm characterized by the white hemorrhage in the sulci (b) and within the subarachnoid spaces surrounding the midbrain and other structures (d). It is not practical to perform a CT on every patient who presents with a headache, since it is a very common condition. On the other hand, one does not want to miss a life-threatening condition that is potentially treatable. Meticulous clinical acumen and prudent clinical judgement is therefore necessary to direct management of patients with headaches and with patients who complain of pain.
The dura has the largest number of nociceptors of the meninges. In acute aneurysmal rupture, the severe pain is caused by stretching and distortion of the blood vessels that are accompanied by the nerves.
Courtesy of: Ashley Davidoff, M.D.
Other Vascular and Circulatory Disorders : Ruptured Aneurysm
The patient who presents with acute severe back pain, hypotension, and a pulsatile abdominal mass has a diagnosis of a ruptured abdominal aortic aneurysm until proven otherwise. Action should include a prompt and urgent phone call to the vascular surgeon, a phone call to the OR, and an immediate non contrast CT of the abdomen and pelvis. The pain is mostly caused, in this instance, by a sudden distension of the retroperitoneal tissues inciting deep muscle and connective tissue mechanoreceptors and presumably causing tissue damage with the release of chemicals that incite the chemoreceptors.
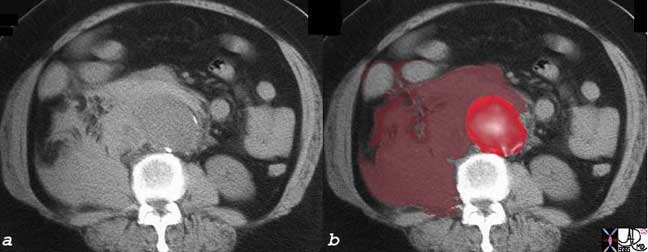
The abdominal CT is from an elderly patient who presents with acute, severe back pain and pulsatile abdominal mass. Findings include an abdominal aortic aneurysm (bright red ) and a retroperitoneal bleed toward the right side where there has been a rapid and painful accumulation of blood (maroon) that expands the retroperitoneum and invades and expands the right psoas muscle. This patient suffered from a rupture of an abdominal aortic aneurysm.
Courtesy of: Ashley Davidoff, M.D.
Acute Aortic Dissection
An acute aortic dissection is a cause of hyperacute back pain caused by rapid accumulation and distension of the aortic wall, with blood that incites the pressure receptors. In addition, there may be dissection across the intercostal arteries which become occluded. The pain is often somatic and lancinating due to resultant ischemia of the chest wall. When the dissection involves the ascending aorta, the pain is usually in the anterior chest, while if the dissection extends to the descending aorta, it may cause interscapular pain. The dissection can also involve and occlude the right coronary artery in which case it may cause classical cardiac ischemic pain.

This pathological specimen shows an aortic dissection starting at the root of the aorta and extending across the arch and into the descending portion. The false lumen is filled with clotted blood.
Courtesy of: Henri Cuenoud, M.D.
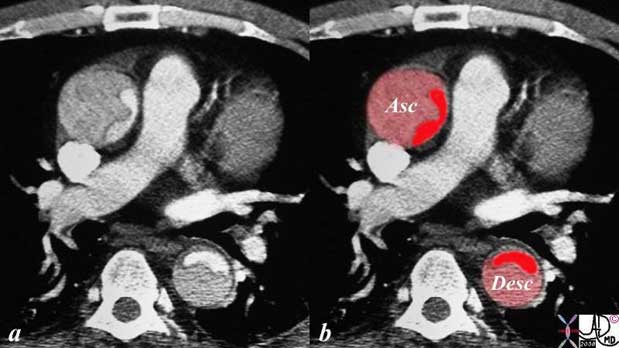
The CT image shows a dissection in the ascending and descending aorta. The lumen consists of the smaller true lumen (bright red) and the false lumen (larger with dull red) The patient presented with classical severe chest pain that radiated to the back. The involvement of the ascending aorta makes it a type A dissection and therefore treatment requires surgical repair. In this patient, however, the dissection extended to the descending aorta as well. Either way, a type A dissection requires surgery.
Courtesy of: Ashley Davidoff, M.D.
Other Hemorrhages and Ruptures
Pulmonary hemorrhage can be extensive but painless as the pulmonary parenchyma is not nociceptive. However, the pleura are richly endowed with nociceptors and when pleura is involved with inflammation as noted above, pain can be sharp and somatic.
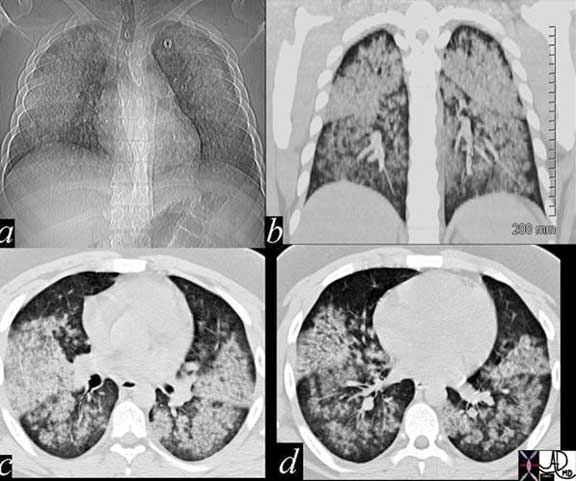
This 20-year-old male patient presented with hemoptysis and renal failure and following renal biopsy a diagnosis of Wegener’s granulomatosis was made. The CT shows extensive pulmonary hemorrhage characterized by white nodular infiltrates, but there was no pain associated with the extensive pulmonary findings.
Courtesy of: Ashley Davidoff, M.D.
Hemorrhage into the peritoneal cavity is also surprisingly non painful, though hemorrhage into the omentum as seen in trauma and following rupture of an ovarian hemorrhagic cyst can be extremely painful. The patient may present with peritonism and simulate peritonitis.

This football player presented with severe abdominal pain in the right upper quadrant and pain with peritonism following a football game. The pain was of such concern that he was taken to the OR where hemorrhage into the greater omentum was diagnosed. In this instance, pain was presumably caused by blood acting on chemoreceptors in the omentum.
Courtesy of: Ashley Davidoff, M.D.
Other Ruptures
Ectopic pregnancy is another clinical scenario where a combination of rupture and hemorrhage creates an extremely painful and dramatic clinical presentation.
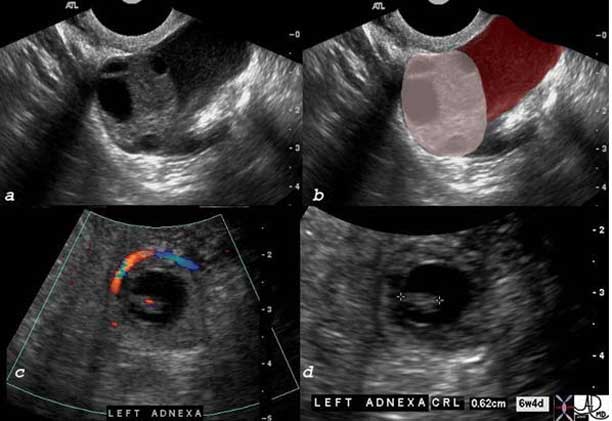
The ultrasound images from a 32-year-old female who presented with severe pelvic pain and a positive human chorionic gonadotropin (hCG). Image (a) shows a normal left ovary with follicles (overlaid in (b) with light pink) with fluid later shown to be blood laterally (maroon). Within the left adnexa, a gestational sac surrounded by a ring of blood flow surrounds a fetal pole within the sac (c). The fetal pole has a beating heart (red dot) in (c) and measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. The uterus was empty. These findings are consistent with an ectopic pregnancy.
Courtesy of: Ashley Davidoff, M.D.
Metabolic and Functional Causes
The metabolic causes of abdominal pain tend to be quite uncommon and include diabetic ketoacidosis where the pain may be caused by acute fatty change of the liver with swelling and capsular distension. Abdominal pain in an Addisonian crisis is also described but the condition is rare. Porphyria is another rare metabolic disorder that is a genetic defect resulting in a paucity of the enzyme porphobilinogen-deaminase. The deficiency causes an accumulation of precursors, porphobilinogen and aminolevulinic acid (ALA), which induce an autonomic neuropathy and hence pain.
Functional causes of pain are common and complex. It is often a diagnosis of exclusion and is a basket collection of many diseases that among other factors have psychosocial and psychocultural elements that are difficult to define and difficult to treat. Many headaches, tension aches, atypical chest pains, vague abdominal pains, irritable bowel syndrome, chronic functional abdominal pain, fibromyalgia, chronic fatigue syndromes fit into this category.
Pain is a common symptom and can reflect a wide variety of diseases. Inflammatory and mechanical disease categories are the most common causes of pain and chemical mediators produced by the disease entities either lower the threshold to pain or induce pain themselves. In general, however, the type of receptors is few. There are nociceptors sensitive to pricking or sharp objects, which are present in high concentration in the somatic structures and manifest with well-localized sharp pains. There are nociceptors that are sensitive to pressure, which are present in high concentrations in the viscera and present with ill-defined dull aches. Cross over situations occur and anybody experiencing gas cramps would agree that their pains are far from dull. In addition, there are many situations where somatic and visceral pains are both present as was described in the case of acute cholecystitis. Neuropathic pain is not as common as the somatic and visceral pain and together with functional pain are more chronic forms of pain. Functional pains are common and complex and difficult for both the patient and the caregiver. Often treatment of this pain type is multimodal and requires a combination of experts to direct management.
Approach to the Diagnosis of Pain
Diagnosis is a determination of the nature of a disease. An orderly and progressive algorithm must be followed to arrive at the most accurate diagnosis and subsequently institute the most effective treatment. Meticulous attention to the nature of the pain and its associated symptoms in the clinical history, a focused examination complimented by relevant laboratory investigation and appropriate diagnostic imaging is necessary. Of these, the most important is the clinical history.
History
As we have seen from the previous modules, pain is complex and often individualized. Acute pain tends to be more common and easier to deal with than chronic pain. In the acute situation when pain is purely somatic, it commonly follows relatively simple rules. It is well-defined, well-localized, and there is often a precipitating event. Visceral pain starts to add complexity as the pain is more vague, may manifest as discomfort, is poorly localized, and is often associated with other symptoms. As pain becomes chronic, whether somatic or visceral, neuropathic or psychological, diagnosis may be straightforward but treatment becomes more difficult.
Age of the Patient
Although we are really dealing with adults in this module, it is reasonable to frame pain in the context of age. It then becomes relevant to consider how perception of pain differs with age. For example, pain is a sensation that can be appreciated by mid to late gestation inferring that preterm infants can perceive pain. The newborn responds to pain with crying, body movements or facial expression. By one month, babies can be comforted when in pain as they start to recognize human interaction and comfort provided by a loving caregiver. Preschoolers can start to describe location and severity of pain and respond with crying and anger. Their memory of “shots” and avoidance in the future of such an experience is vivid. Children have two general responses to pain. They either develop an ability to “be brave” in the face of pain, or they may be overcome with fear. In adolescence, the two groups with black or white responses in their acknowledgement persist. As mortality and fear of disease becomes more realistic in adulthood, pain is either ignored or rapidly dealt with by a visit to the caregiver for the assurance that it does not represent a mortal illness. With aging, acceptance of pain as part of life becomes the common response.
Pain Descriptors
Pain descriptors are verbal terms used to characterize pain. Although they are subjective expressions of pain, descriptors can be organized into helpful tools when assessing a patient. The purpose of using pain descriptors is two fold: First, they provide structure to an otherwise subjective interview. Patient and clinician can systematically navigate through an organized array of terms to create a narrative that may define the pain source. For example, the pain of aortic dissection is often described as a ?tearing? sensation felt in the center of the chest and the very moment of onset is easily recounted.
The second effect of descriptors is that they prompt the patient to discuss more pain features than he/she might not have otherwise. This approach also invites the patient to express the pain without the clinician scripting the narrative. For example, a middle-aged male patient complaining of chest pain would raise serious concerns as an isolated descriptor for ischemic heart disease. However, when asked about aggravating factors, the patient links the pain to deep breathing and then remembers a blow to the chest from a softball the day before. The descriptor of aggravating factors prompted the patient to more accurately describe the pain and subsequently directed the clinician toward a probable non life-threatening source.
As with pain scales, there are many versions of descriptor tools tailored to age groups and medical specialties. These instruments are all designed to assess baseline and therapeutic pain descriptions. Although physical diagnosis texts vary, the most common descriptors include precipitating factors, duration, onset, character, situation, severity, aggravating and relieving influences, radiation and associated symptoms. The acronym is PDOCSSARRA. Other descriptors like pattern, location and level of impairment may be added to bring more depth to the patient?s story, keeping in mind the time constraints of the healthcare setting.
Precipitating Factors
“What were you doing when the pain started?” This is a good question to initiate the discussion because it represents the beginning of the patient’s story.
Precipitating factors describe the situations or circumstances that triggered the pain.
Examples where this question has relevance include exercise related pain which is typical of ischemic pain. In the case of angina, it is chest pain while walking that is typically relieved by rest. Abdominal angina is pain with eating and claudication is usually discomfort in the lower extremity induced by walking. Right upper quadrant pain precipitated by a fatty meal brings to mind acute cholecystitis, while right upper quadrant pain following an alcoholic binge may constitute acute fatty change of the liver. Acute back pain after “just picking up my young son” brings to mind a herniated disc.
Pain that awakens somebody from sleep usually is given serious consideration because it comes with no supratentorial element and is generated purely by something physical. It can herald a catastrophic event such as a rupture of a structure. Ruptured berry aneurysm, aortic dissection, acute myocardial infarction, ruptured ectopic pregnancy are considerations depending on the site of pain. Peptic disease is also classically described as pain that awakens a patient 2-3 hours into their sleep.
Sometimes the precipitating event concurs with a physiological event and this is viewed as a precipitating factor. Examples include menstrual cramps and mittelschmerz – which is mid cycle pain corresponding to ovulation. Excessive exercise is also a physiological event that may precipitate pain.
The onset of the spring or fall with dusts and pollens sometimes induces sinus headaches.
The precipitating factor as discussed above is often a major criterion on which the diagnosis rests. It is, of course, an essential question stated to open the dialogue and initiate the story of the pain.
Duration
Time and pain can be framed into two important contexts. The first is historical: “How long have you had the pain for?”. The second is: “How long does the pain last?”
There is a significant difference and clinical bias depending on whether the pain has come and gone for years, as opposed to pain that has just started. A patient who presents with chest pain that has come and gone for years is treated differently from the patient who has acute pain that started a few hours earlier. The latter history raises more serious concerns and life-threatening disease must be excluded, while the former may represent a serious condition like coronary artery disease, but the danger is not necessarily imminent.
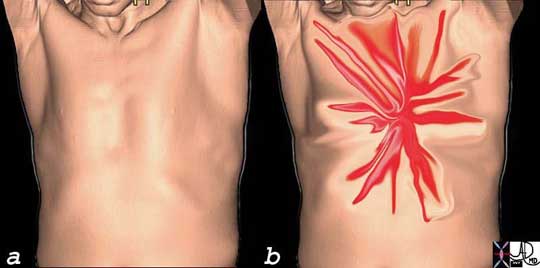
This image is intended to reflect the severe (bright red) lancinating, sharp, thunderbolt-like character (spiculated shape) of the chest pain that the patient with acute dissection may experience. One moment the patient is healthy without symptoms (a) and the next, there is catastrophic pain that reaches maximum intensity at the time of onset (b). This is one of the pain syndromes in medicine one fears. It represents one of the most severe forms of chest pain one can experience.
Courtesy of: Ashley Davidoff, M.D.
The second question of ?How long does it last?” also has significant relevance and we will use the chest pain example once again. Chest pain that lasts a few seconds and is fleeting is not angina and usually is not of clinical concern. Angina and ischemic pain, in general, are caused by the chemical build up of lactates which take time to accumulate and also time to disappear. Angina usually lasts from 1-15 minutes and may even go as long as 30 minutes. However, once chest pain goes beyond 20 minutes it becomes concerning and unstable angina is considered.
The relationship between time and pain is an important and essential characteristic for the clinician to elucidate and time periods will range from fleeting (measured in terms of seconds), to years. It is sometimes not easy for the patient to describe or remember when the pain started or how long it lasted and often the patient is required to correlate the pain event in light of other events in their life. We have developed a few charts that may help the patient describe and recall when the pain started.
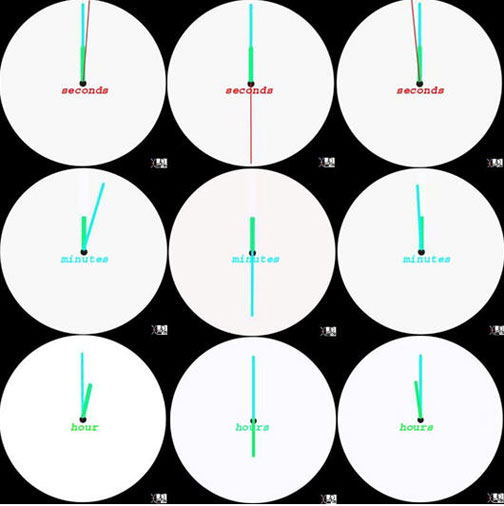
The chart describes acute pain in graphic terms. The top line shows the red hand representing seconds ranging consecutively from a few seconds (less than five) in the first image (top left) to 30, (middle top) and then to about a minute (right top). The second row with the long teal hand, represents the pain duration in minutes. The first left image is pain in the 5 minute range, the second in the 30 minute or less range, while the third represents pain going on an hour. The last row, with short green hand being relevant, represents pain that lasts an hour or two, (bottom left) the second represents pain in the 5- 6 hour range (bottom middle) and the last in the close to 12 hour range (bottom right).
The chart describes acute pain in graphic terms. The top line shows the red hand representing seconds ranging consecutively from a few seconds (less than five) in the first image (top left) to 30, (middle top) and then to about a minute (right top). The second row with the long teal hand, represents the pain duration in minutes. The first left image is pain in the 5 minute range, the second in the 30 minute or less range, while the third represents pain going on an hour. The last row, with short green hand being relevant, represents pain that lasts an hour or two, (bottom left) the second represents pain in the 5- 6 hour range (bottom middle) and the last in the close to 12 hour range (bottom right).
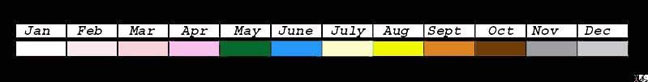
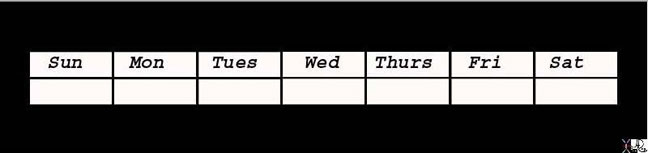
Months and Seasons
The third chart is in the form of an annual calendar and shows pain in terms of months and seasons. It is a graphic reminder for the patient who tries to remember which month the pain started and allows the patient to integrate the symptom with another event of the year. For example, “Oh yes, it started in the summer when we were at grandma’s barbecue”. Each season is represented by a different color.
Images courtesy of: Ashley Davidoff, M.D.
The distinction between and the implications of acute and chronic pain are therefore important and are defined by the above question; “For how long have you had the pain?” When pain lingers beyond a realistic healing time, the experience becomes chronic. Despite resolution of the injury, there is lingering activation of pain fibers perceived by the patient. Additionally, there are often disabling features beyond the sensory manifestations of chronic pain which can make treatment difficult. These include motor dysfunction, muscle tension, depression, personality changes, anorexia, and sleep disorders for example, all of which can be severely life altering to the patient.
Onset and Character
“Did it start suddenly or slowly?” or “Did it build up quickly to peak or slowly to peak?” are the type of questions that define onset. In general, pain that starts suddenly is somatic in origin, while pain that is gradual in origin is usually visceral.
“I was sitting having dinner with my family and suddenly developed the most severe headache of my life ” raises the question of a ruptured berry aneurysm.
“I woke up in the morning with a mild headache and it got worse during the day and is at its worst now, but I have had similar more severe headaches in the past” This does not sound like a berry aneurysm.
Thus “onset” describes the arrival of pain.
“What did it feel like? We are now getting to the exciting part of the story. Was it sharp, cutting, pinching shooting, stabbing, knife-like or dull and bruise-like? Was it throbbing, gripping, aching, tearing, lancinating or like lightning. Did it feel like pressure, heaviness, dull or nauseating or more like real piercing pain? Was is colicky, spasmodic or squeezing like bad gas cramps?” Was it tingling or numbing?
Each of these characteristics do not always imply a specific disease. In general, sharp pains tend to be somatic while dull aches tend to be visceral. Colicky pains tend to originate from structures that peristalse such as the bowel, biliary ducts and ureters. Lancinating pain in the chest or back suggests aortic dissection. Pain that is dull and deep in joints or limbs usually implies musculoskeletal origin. Pain that has numbness or tingling as an element may imply a neuropathy. Pain in the chest that has a pressure-like character raises concern for cardiogenic pain.
Situation and Severity
” Where exactly does it hurt? Can you point with a finger or is it easier to use your whole hand to define the position of the pain?” “Does it feel deep or does it feel like it is coming from the muscles or skin?”
Also called location, situation defines the affected area of the body and the depth of pain as either superficial or deep. The situation can vary from well-localized pain to that which is perceived to originate from a general area that is not well-defined.
Somatic pain tends to be well-localized in which case the patient points with a finger, while visceral pain tends to be more diffuse and the patient uses the whole hand to describe the location of the pain.
“How severe is the pain?” “Is it the worst pain of your life or is it only mild?” On a scale of 1-10 with 1 being mild and 10 being the worst, where does it fit into the scale?”
With the question of severity we start to get into individual perception of pain. What may be severe pain for one person may be mild for another. There have been several classifications used to evaluate the severity of pain
-
- grading based on the 1-10 Wong Baker scale
- grading based on mild, moderate, severe scale
- grading based on the facial illustration
- grading based on color
- grading based on the degree to which the patient is disabled by the pain
Pain Scales
There is no definitive pain scale across all medical fields. Instead, there are a multitude of scales specific to different medical areas. A cancer pain scale, for instance, may focus on degrees of bone pain and therefore, differ from that used for rheumatoid arthritis. To that end, the National Institutes of Health Pain Consortium recognizes six different scales to measure pain intensity and efficacy of treatment (NIH Pain Consortium).
The most patient friendly pain measure is the Wong-Baker Faces Pain Rating Scale, also called the Universal Pain Assessment Tool. The patient scores the level of discomfort from 1-10 in increasing intensity by selecting a facial expression diagram that best matches the experienced pain (see diagram below). Although there are many other examples, this is the most widely used pain scale given its simplicity across all patient populations.

Wong Baker Pain Scale
The top row shows a numerical value for the pain with 1 being mild and 10 being the most severe. The next row uses a verbal descriptor. The next line is a facial grimace scale with specific colors representing degrees of pain and the next line shows activity tolerance related to pain and translations in subsequent rows to a variety of languages, which has equivalents in other languages lower.
The Wong-Baker Scale is an excellent, practical and comprehensive diagrammatic that describes the scale of severity well and is universally accepted. A simpler modified diagram is shown below that may be easier for some to use.
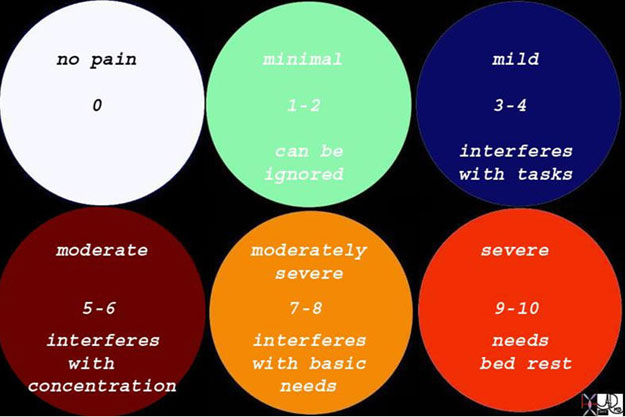
A modification of the Wong-Baker scale is illustrated above. It offers the advantage of being slightly simpler, but does not offer the facial grimace scale useful for children, nor the interpretation into other languages.
Courtesy of: Ashley Davidoff, M.D.
Aggravating and Relieving Factors
“What makes the pain worse?”
Aggravating factors is self-explanatory and describes activities or environments that intensify the pain. Plantar fasciitis pain is usually worse after prolonged rest, thus, hobbling its victims when they first ambulate in the morning. Deep inspiration aggravates pleuritic pain and movement in general, aggravates traumatic musculoskeletal pain.
“What makes the pain better?” “Does anything help the pain?” “What medicine have you taken and has it been effective?”
Relieving factors describe activities or environments that treat or attenuate the pain. Examples include angina that resolves with cessation of exertion or tendonitis pain that lessens ironically with use and worsens with rest. Sitting forward may relieve the pain of pericarditis. Anti-inflammatory agents relieve pain that has inflammatory causes, while nitroglycerine relieves angina and esophageal spasm.
Radiation and Associated Symptoms
“Does the pain radiate anywhere else in the body?”
Radiation identifies a part of the body to which the pain migrates. Sciatic pain from lumbar spinal nerve irritation will often radiate down the posterior aspect of the affected lower extremity. Appendicitis may start as a periumbilical pain, at which time it is visceral and by implication is referred pain, and then migrate to the right lower quadrant at which time it is somatic and has spread to the peritoneum.
“What other symptoms do you have with the pain?” “Are you nauseous?” Did you vomit? Did you sweat? “Did you faint?” Did you have diarrhea?” “Did somebody comment that you were pale?” Were you short-of-breath?
We have noted in the basic sciences of pain in part 1, that the autonomic and limbic systems are activated as the pain signal travels through the brain. In general, the sympathetic system is turned on accounting for anxiety, tachycardia, pallor, sweating, and sometimes associated with a sense of impending doom. In some patients, particularly when the pain is severe, vagal influences intrude and the patient may be nauseous, may vomit, and may even faint.
A patient who presents with pain reminiscent of a myocardial infarction and has associated shortness-of-breath suggests pump failure and a large infarction.
Clinical Examination – by Anatomical Regions
A brief outline of common clinical signs in the evaluation of pain follows. Head and Neck
Pain syndromes of the head and neck vary according to the degree and area of injury but are generally poorly tolerated due to the anatomical confines of these regions. The head and neck anatomy is highly vascularized and well innervated with both somatic and cranial nerve fibers. Pain symptoms, therefore, are often accompanied by neurological findings. Causes of head and neck pain include trauma, neoplasm, infection and treatment related syndromes after surgery or radiation therapy.
The clinical examination for pain in the head and neck region requires meticulous examination of the cranial nerves, evaluation for neck stiffness, extension, flexion and rotation range, evaluation of the temporal arteries, pressure palpation of the sinuses, and evaluation of the lymph nodes in the neck and occipital regions.
Chest
Due to the prevalence of cardiovascular disease and its common manifestation of thoracic symptoms, chest pain receives priority status when described by the presenting patient. Chest discomfort can also occur in the absence of objective findings; however, usually at the expense of healthcare resources to exclude the more serious etiologies as described in the chest pain module. Examination of the chest is not very helpful except in a few circumstances. When costochondritis is suspected, then pressing on the rib cage may induce pain. When pericarditis or pleurisy is considered, then a rub may be heard. New murmurs of valvular incompetence or a new 4th heart sound all implicate the heart as a cause of chest pain. Pleural effusion as depicted by dullness to percussion or pneumonia as depicted by whispering pectoriloquy are useful signs on the clinical examination for these disease entities.
Abdomen
Excluding direct trauma, abdominal pain is often visceral in nature and therefore difficult to delineate. Visceral pain receptors are stimulated by distension, contraction, inflammation and ischemia. An understanding of these characteristics and a sound knowledge of abdominal anatomy can be helpful in demystifying abdominal pain. Exquisite superficial pain induced by minimal focal palpation is reminiscent of peritonism and suggests peritonitis. Murphy’s sign with pressure exerted over the gallbladder region that induces pain on inspiration as the gallbladder comes down and forward is characteristic of acute cholecystitis. Focal tenderness in the region of McBurney’s point, 1/3 the distance between the anterior superior iliac spine and the umbilicus raises the possibility of appendicitis. Flank bruises in a patient with severe abdominal pain following an alcoholic binge is characteristic of Grey-Turner’s sign of acute pancreatitis.
Pelvic
The pelvis is another highly vascularized area comprised mostly of the reproductive organs and a multitude of lumbar and sacral nerve plexuses. Due to its anatomical proximity to the abdominal viscera, pelvic pain may often reflect an abdominal process.
Pelvic inflammatory disease is characterized by cervical tenderness and a discharge, while mid-cycle pain may reveal a large cystic mass in the adnexa.
Back
Back pain is significant in its societal frequency and impact on the workforce. There is a 90% lifetime incidence of back pain in the adult population and it ranks second only to the common cold for worker absenteeism. Although classically, back pain is a self-limited manifestation of muscle spasm in response to injury, disorders of the spinal structures and subsequent nerve roots can cause chronic, life altering pain and disability. Evaluation for muscle spasm, sensory and motor deficits and rectal tone are important clinical features in the workup of patients with back pain.
Extremity
The most common cause of extremity pain is injury to soft tissue, bone or cartilage that is either acute or repetitive. Pain radiation is common in the extremities due to alignment of sensory and motor nerves within the fascia. For example, repetitive stress injury to the forearm causing tendonitis in tennis players is often manifested as elbow pain, thus invoking the nickname “tennis elbow”. Degenerative joint disease in the elderly is a frequent source of chronic pain and disability often with surgery as the only remedy.
Examining the range of motion of joints, as well as the motor and sensory functions all need to be examined in patients presenting with limb pain. Neurological deficits in any part of the body associated with pain is a serious finding and probably the most important contribution of the clinical examination. Imaging techniques can find many abnormalities that are missed on clinical exam, but they cannot equal in any way the sensitivity of a neurological examination.
Laboratory Investigation
The laboratory investigation has its most important contribution in determining whether the disease is inflammatory or infectious. To this end, the blood count and specifically the white cell count are important. Erythrocyte sedimentation rate and C-reactive protein also help in defining activity and are elevated in both inflammatory and infectious diseases. When a patient complains of pain and if any of the aforementioned studies are positive, we know we have to take the patient seriously and a diagnosis should be pursued. Urinary examination is important in patients with renal colic or pyelonephritis. Chemical and cytological examination of pleural fluid or cerebrospinal fluid (CSF) in the appropriate clinical setting can be useful in diseases such as pleurisy and meningitis. The EKG is extremely important in the workup of the patient with chest pain, which if abnormal creates a cascade of events in the workup aimed at excluding a myocardial infarction.
Imaging Pain by Anatomical Locations
The advancement of technology over the last 15 years has enabled the medical world to evaluate morphological detail of the body to an exquisite degree. This has been a tremendous advantage and has avoided unnecessary surgery in some cases and directed appropriate surgery and treatment in other cases. To some extent, the evolution of imaging has also been to our disadvantage as a community as the images we see often have no relevance to the patient’s symptomatology. On the other hand, the reputation of imaging as an accurate diagnostic tool has created a reliance on imaging but also has resulted in abuse of the technology. Diagnostic imaging procedures like X-ray, CT, MRI, Nuclear Medicine and Ultrasound, as well as laboratory testing, have all been effective in diagnosing pain.
Pain in the Head and Neck
One of the first studies performed in the patient with a new headache, which is clinically concerning, is a CT scan of the head. CT is able to make the distinction between a life-threatening rupture of a ruptured berry aneurysm and a non-hemorrhagic condition. An example is shown below.
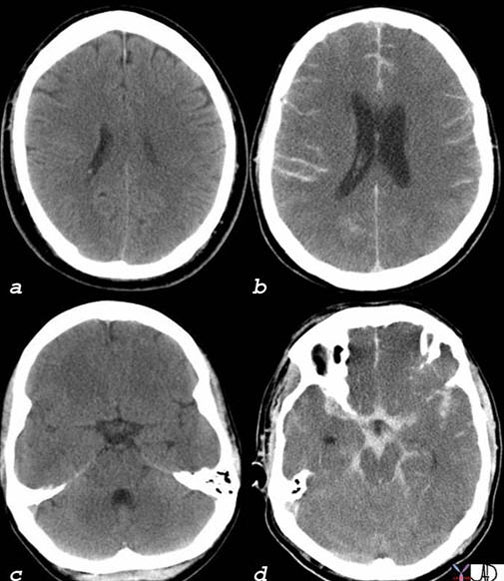
These two head CT’s are from two different patients who both presented with severe headaches. The first patient (a, c) had a normal study and the headache may have been caused by migraine, cluster, or tension headaches, for example. Although these headaches create significant morbidity they are relatively benign in that they are treatable. The second patient (b, d) had a life-threatening subarachnoid hemorrhage due to a ruptured aneurysm characterized by the white hemorrhage in the sulci (b) and within the subarachnoid spaces surrounding the midbrain and other structures (d). It is not practical to perform a CT on every patient who presents with a headache, since it is a very common condition. On the other hand, one does not want to miss a life-threatening condition that is potentially treatable. Meticulous clinical acumen and prudent clinical judgement is therefore necessary to direct management of patients with headaches and with patients who complain of pain.
The dura has the largest number of nociceptors of the meninges. In acute aneurysmal rupture, the severe pain is caused by stretching and distortion of the blood vessels that are accompanied by the nerves.
Courtesy of: Ashley Davidoff, M.D.
When a patient presents with a headache, sinus congestion, focal pain over the sinuses and a fever, the diagnosis of acute sinusitis is clinically apparent and no further workup is necessary. Sometimes the clinical presentation is less revealing and CT is highly sensitive to the diagnosis and is also able to reveal the extent of the disease.

The CT scan is from a 28-year-old male who presented with headaches. The CT scan shows easily identified pansinusitis. Image (b) (reflects an overlay of image (a) and shows light yellow total opacification of the frontal sinuses, light orange opacification of the ethmoid sinuses, and dark orange opacification of the sphenoid sinuses. Image (d) is an overlay of image (c) and shows almost total opacification of the maxillary sinuses (darkest orange) as well as the ethmoids (light orange).
Images courtesy of: Ashley Davidoff, M.D.
Pain in the Chest
Chest pain is a common and concerning symptom. In the young, thin, tall male who presents with acute sharp chest pain and shortness-of-breath, an urgent chest x-ray is required to exclude spontaneous pneumothorax caused by rupture of an apical bulla.
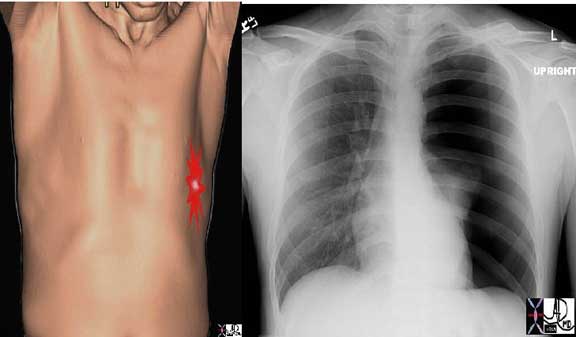
This is the type of CXR that sends shivers down the spine. The overall blackness of the left chest cavity, in association with a nubbin of lung tissue in the ipsilateral hilum and rightward mediastinal shift is characteristic of a tension pneumothorax with total atelectasis of the left lung. Immediate and urgent decompression with a chest drain is indicated. One must also remember that if a tall, thin, young patient presents with chest pain the diagnosis of dissecting aneurysm in a patient with Marfan?s Syndrome has to be considered.
Courtesy of: Ashley Davidoff, M.D.
In the older patient who presents with chest pain, the algorithm is directed toward excluding life-threatening myocardial infarction. As EKG and enzymes start to look like infarction, the question of cardiac catheterization to exclude the presence of acute thrombus evolves.

The above image of this cardiac catheterization of a patient who presented with an acute myocardial infarction (AMI) and shows a coned down left anterior oblique (LAO) projection of the LAD in a patient with acute thrombosis of the left anterior descending artery. The first image on the top left shows a coned down RAO (right anterior oblique) projection of the LAD (left anterior descending) in a patient with acute thrombosis of the left anterior descending artery. In the second image the thrombus in the artery is overlaid in maroon. Following thrombolysis, the third image shows minimal residual irregularity of the endothelium. This may be residual thrombus or the site of a plaque rupture.
Images courtesy of: Ashley Davidoff, M.D.
Pain in the Abdomen
The abdomen has the largest variety of organs of all the cavities and each organ and system has classical manifestations. In general, ultrasound is the technique of choice in the pediatric population, young adults and pregnant patients. It can also be a sensitive test in the evaluation of right upper quadrant pain. CT is used for pain in the left lower quadrant to exclude diverticulitis and in the right lower quadrant in the non-pediatric population where appendicitis is most common. CT is also effective for the patients where pain is vague and a global view of the abdominal contents is needed.
The biliary ducts are best evaluated initially with ultrasound and then by ERCP (endoscopic retrograde cholangiopancreatography) or MRCP ( magnetic resonance cholangiopancreatography). MRI otherwise does not have a large role in the assessment of pain in the abdomen.

This patient presented with right lower quadrant pain and CT scan shows an enlarged appendix in the right lower quadrant and is surrounded by induration in the surrounding fat. Edema in the fat of the abdominal cavity enables the visibility of small amounts of inflammatory edema and it is for this reason that CT is such an excellent study since small changes in the fat are easily visible and have diagnostic implications in inflammation, hemorrhage and malignant diseases.
Courtesy of: Ashley Davidoff, M.D.
Pain in the Pelvis
CT, MRI, and Ultrasound all have a role to play in the pelvis. Ultrasound is the study of choice in the evaluation of the uterus and adnexa as a first line, and if this fails, then MRI is used. CT is most useful for gastrointestinal disorders including colitis and diverticulitis.

This is the transvaginal ultrasound of a 23-year-old female who presented with right lower quadrant pain. Ultrasound is indicated and the study of choice in young female patients with pelvic pain. There is an echogenic mass (maroon) alongside the normal ovary (pink) positioned on the right side of the uterus. This mass represents a hemorrhagic abnormality called an endometrioma which accounts for the pain. Ultrasound is safe, relatively inexpensive and can reveal the female pelvic structures with exquisite detail, particularly when transvaginal technique is used.
Courtesy of: Ashley Davidoff, M.D.
Pain in the Back
Back pain is a common disorder and is most commonly caused by disc disease. It is imprudent to order imaging examinations on all patients with back pain. Generally, plain films are insensitive to the important soft tissue changes that have relevance to the pain. Extensive degenerative changes, as identified on plain film, may not be associated with any symptoms while a minimal disc bulge may only be apparent on MRI. Obtaining a normal plain film examination may cause significant symptoms. MRI should be reserved for those patients with associated symptoms and signs of sensory or motor compromise caused by pressure effects of the soft tissues on the nerve or in those patients in whom more serious disorders such as metastases are a consideration.
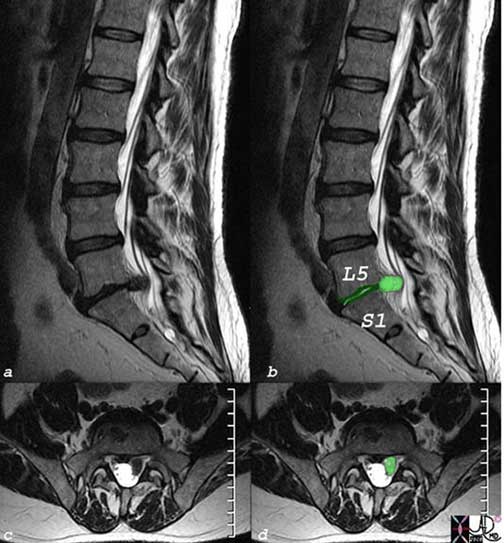
The T2-weighted MRI in the sagittal plane (a, b) and the axial plane (c, d) show a herniated and ruptured disc with the extruded fragment overlaid in lime green (b, d). The mass effect and effacement on the nerves seen in both the sagittal view where the lime green extruded segment impinges on the string-like nerves (black lines) while in the transverse plane the normal nerves are seen on the right and the effaced nerves are seen on the left. Additionally, the loss of height of the disc space (dark green) in (b) is apparent. The disc space of L5-S1 should be taller than the disc space above but degeneration and extrusion has reduced the height of the disc.
Courtesy of: Ashley Davidoff, M.D.
Pain in the Extremity
Sports injuries and chronic degenerative changes are the most common causes of extremity and joint pain. For the sports injuries, both plain films and MRI are utilized. Although plain films are sensitive to fractures, MRI is exceedingly sensitive to soft tissue injury and the associated presence of edema and hemorrhage. For the arthritides, plain films are excellent and often adequate.

Plain film examination for pain in the arthritides. In the case above, the plain X-rays of the hands demonstrate severe rheumatoid arthritis. The plain film demonstrates the characteristic features of the disease as well as the extent of joint involvement.
Courtesy of: Ashley Davidoff, M.D.
In the clinical realm of pain, the medical history is probably the most important part of the diagnostic workup. It is thus imperative for the clinician to actively and meticulously question and listen to the patient during the history taking and examination. The subsequent use of laboratory examinations helps direct the workup and identify those pains that may be inflammatory or infectious in origin. Modern imaging techniques have advanced the accuracy of diagnosis significantly, but they are expensive and should be used prudently.
Basis of Pain Therapy
A pain experience for an equal degree of injury will vary among patients. So, too, will the treatments they receive. In more pedestrian cases of pain, simply removing the offending agent will suffice. However, in many instances this simple and logical process does not suffice and modern medicine has developed a science of pain management in order to relieve patients the burden of pain. The science of pain is based on many of the principles discussed in the first modules relating to the anatomy, physiology and diseases associated with pain. We will review these principles briefly in order to frame the manner in which pain management is utilized.
Basis of Pain Therapy: Structural and Functional Considerations
There are many orders of structural complexity in the pain process, but in general we can view pain stimulus as being received and transported by first order neurons to the spinal cord, which synapse with second order neurons in the dorsal horn. The second order neurons transport the pain to the thalamus. The third order neuron takes the pain stimulus to various parts of the brain where perception takes place and a variety of reactions to the pain are expressed.
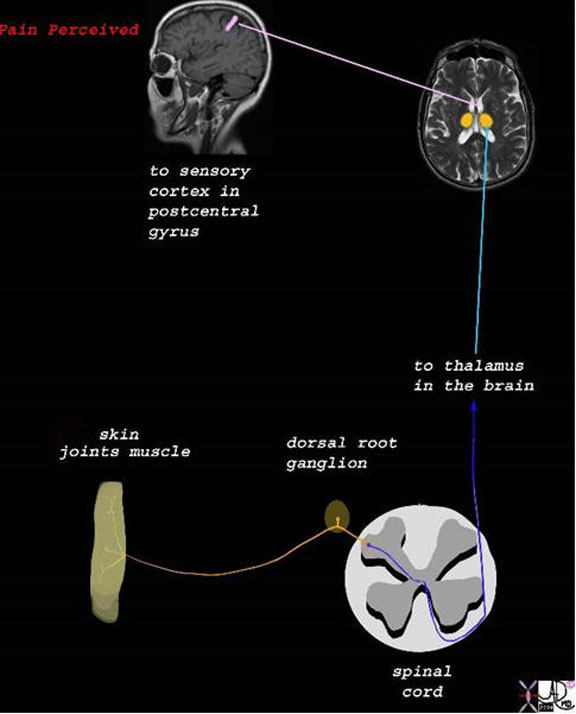
The stimulus is converted into an electrical impulse which is taken by a first order sensory nerve (orange) to the spinal cord (dorsal root ) which in turn transports the impulse via second order neuron (dark blue and light blue) to the thalamus,. The third order neuron (pink) transports the impulse to the somatosensory cortex.
Courtesy of: Ashley Davidoff, M.D.
We reviewed the many mechanisms by which the pain experience was modulated and how the body modified and individualized the pain experience. The electrical mechanisms and neurotransmitters are numerous and complex, but this allows the application of a variety of techniques and options to deal with pain.
Lastly, we reviewed how disease processes modified the threshold of pain, and in particular how inflammation via a variety of mechanisms lowered the threshold to pain. Some pain is best treated by targeting and reducing the inflammatory response.
Basis of Pain Therapy: Considerations in Treatment
Based on the science, it becomes intuitive to aim treatment at the brain, spinal cord, or at peripheral nerves and their ganglia.
Pain control can be non-specifically directed at the nervous system resulting in the loss of a variety of sensations including pain. This is called anesthesia which by definition means loss of sensation. As a result of the anesthesia, whether administered locally or generally, pain is controlled, and in the case of general anesthesia there is associated loss of consciousness. It is usually used preemptively for surgical intervention. Analgesia is another variant of pain control, usually used after the injury or disease has occurred and without altering consciousness. There are many agents specifically designed to treat pain mechanisms.
Considerations in Treatment: Anesthesia
Local and regional anesthesia aim therapy at the nerves and ganglia. The anesthetic in these instances is injected locally and directly into the tissue or nerve involved. Spinal anesthesia (subarachnoid anesthesia) and epidural anesthesia are directed at the nerve-spinal cord interface. The anesthesia in these instances are administered locally and directly by a needle directed into the spaces surrounding the cord. Anesthetic agents administered intravenously or via the airways may take the form of general anesthesia, deep sedation, conscious sedation and minimal sedation. These agents that act on the brain alter the level of consciousness.
However, when dealing with pain in the context of disease and long term relief, we are in general dealing with the field of analgesia, since anesthesia is in general short lived.
Considerations in Treatment: Analgesia
Briefly, the pain signal is initiated by a noxious insult or process causing cellular depolarization of peripheral nociceptors. The signal then propagates as a tsunami of depolarization along the process of a neuron. With the help of neurotransmitters, the wave front crosses neurosynaptic bridges transmitting over additional neurons as it travels centrally to the dorsal horn of the spine. At this level, the signal receives input from other biochemical and mechanical influences. The signal then travels up the spinal cord to the brain where it is dispersed among the anatomical centers that comprise the limbic system. Here begins a competitive interaction of pain promotion by biogenic amine neurotransmitters (acetylcholine and norepinephrine) secreted from the hypothalamus and reticular activating system (RAS) versus pain suppression by indolamines (serotonin), dopamine and morphine-like B-endorphin peptides called enkephalins from the periventricular gray matter. The limbic system thus modifies, then finalizes the perception of the pain signal and incorporates its interpretation with emotion and behavior to elicit a response. Analgesics provide a pharmacological means of intervening upon the different components of this pain cascade.
Basis of Pain Therapy: Modifying Inflammation
Parallel to the pain pathways, tissue injury promotes the synthesis of prostaglandins peripherally and centrally. These compounds play many vital roles in the body but are the main biochemical component of inflammation. As described in the functional pain module, inflammation is the primary tissue response to disease or injury. This response, however, is mediated by the local release of prostaglandins. Their presence promotes vasodilation and edema. The consequence of this tissue infiltration is further stretching and stimulation of peripheral pain receptors and increased pain intensity. Analgesics provide a pharmacological means of intervening upon the various components of this pain cascade.
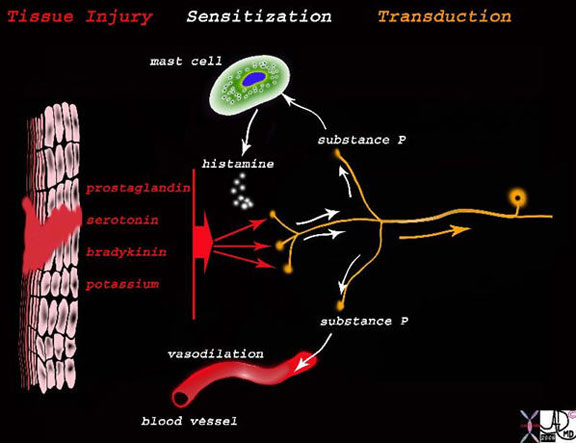
The diagram shows the effect of tissue injury (left side of diagram) that induces the release of prostaglandin, serotonin, bradykinin, and potassium which cause sensitization of the free nerve endings to pain which lowers the threshold to pain. In addition, they induce (red arrows) the axon reflex (white arrows) which causes the production and release of substance P from the free nerve endings, which cause the release of histamine from the mast cells. The histamine causes vasodilation and exudation into the damaged area. Three of the hallmarks of inflammation are explained in the diagram. Pain, swelling (edema) and hyperemia increased blood flow.
Centrally, prostaglandin synthesis is intimately tied to the emotional response to pain as the associated anxiety promotes its production from the hypothalamus. These substances also intensify pain in the limbic system especially in cases of repeated insult or injury.
The first therapeutic approach to somatic pain from inflammation is to immobilize the area if possible and to apply cold compression and elevation. This therapy provides mechanical modification to the pain receptors by minimizing vasodilation and promoting venous return thereby decreasing edema. In addition, nociceptor activity is directly down, regulated by the local hypothermia of an ice bag.
For visceral or intense somatic pain, drugs with anti-inflammatory activity can significantly improve the experience. There are four main groups and six sub-groups of these agents, each with its own unique effect on inflammation.
Basis of Pain Therapy: Anti-Inflammatory Agents
Corticosteroids are endogenous compounds secreted from the adrenal glands. Their synthetic versions are effective analgesics that regulate inflammation directly by down regulating the immune response and indirectly by decreasing the body’s overall stress response to pain. They are also useful adjuncts to other analgesics by their positive effects on mood and appetite. Corticosteroids can be administered orally or injected locally in combination with other pain relievers especially in cases of chronic joint pain. Systemic use of these agents requires caution as their chronic use creates a negative feedback loop to the adrenal glands, thereby suppressing endogenous corticosteroid production. There are a number of side effects with these agents and they include gastrointestinal irritation, osteopenia, leukocytosis and immunosuppression.
Salicylates (e.g. aspirin) inhibit prostaglandin synthesis both in the central nervous system (CNS) and in the periphery. Aspirin remains the oldest and cheapest salicylate analgesic available and its use remains high due to its additional antiplatelet, anti-cancer and antipyretic properties. Unfortunately, aspirin’s antiprostaglandin effects are universal as prostaglandins that are protective to the mucosal lining of the stomach are also inhibited. The major side effect of this agent, therefore, is gastritis and potentially life-threatening gastrointestinal (GI) bleeding.
Acetaminophen (e.g. Tylenol®) is an effective antipyretic and analgesic agent that primarily inhibits prostaglandin activity within the CNS but not peripherally. Acetaminophen, therefore, does not reduce inflammation at the site of injury but is an effective pain reliever nonetheless. Higher doses of this agent can be toxic to the liver and kidneys.
Nonsteroidal anti-inflammatory drugs (NSAIDS, for example, aspirin, ibuprofen and naloxen) are a diverse class of drugs that combine anti-inflammatory, analgesic and antipyretic effects with varied potencies and mechanisms of action on prostaglandin activity.
Proprionic acids (ibuprofen, fenoprofen, proxen, fenbufen, ketoprofen, birbuofen proquazone and oxaprozin) are the most popular nonsteroidal anti-inflammatory preparations. At lower doses, these compounds exhibit adequate analgesic activity especially in the CNS. However, their “forte” of potent anti-inflammatory activity is not experienced until higher doses are consumed. Again, GI side effects from prostaglandin inhibition are a correlative risk. Often, concomitant use of acid reducing agents and/or limitations on therapy duration are recommended.
Indoleacetic acid (indomethacin) exhibits potent and nonspecific prostaglandin inhibition and is effective for cases of acute somatic pain especially in rheumatoid arthritis exacerbations or conditions of inflamed visceral linings. For example, effective relief of pleuritic chest pain from pericarditis is often responsive to this drug. GI irritation is unfortunately, fairly common with this agent and therapy should thus be short-lived.
Idene acetic acids (sulindac, zomepirac), phenylacetic acid (diclofenac) and pyrrole acetic acid (tolmetin) are chemically related to indomethacin and thus have similar global antiprostaglandin properties. Their efficacy is thus, tempered by the same potential toxic GI side effects.
Benzothiazine (piroxicam) is a stable compound with a longer half-life and thus, anti-inflammatory effects last over a 24 hour period.
Anthranilic acid (meclofenamate) is a unique anti-inflammatory analgesic in that it competitively inhibits prostaglandin receptors in the periphery.
Pyrazolines (phenylbutazone, azapropazone) are primarily anti-inflammatory with only minimal analgesic activity rendering these agents specific to only a few pain related entities. Toxicity from these drugs includes hematological abnormalities and edema. Duration of administration is therefore short-term except for the treatment of ankylosing spondylitis.
Basis of Pain Therapy: Modifying Pain Perception
The key to analgesic efficacy within the pain centers of the brain is the ability to offset the balance of pain stimulation and suppression in favor of the latter. The more intense or prolonged the pain experience, the lower the pain threshold and the higher the sleep deprivation, anxiety and depression. Analgesic agents that augment the pain suppressing neurotransmitters serotonin, dopamine, and catecholamines can effectively change the perception of pain. The most effective way to increase neurotransmitter levels is to inhibit their synaptic reuptake. When a neuronal signal has crossed the synapse, facilitated by the presence of neurotransmitters, these compounds are quickly restored in the neuron via cyclic adenosine monophosphate (cAMP). By competing with the receptors that promote this peptide transporter, the reuptake mechanism of serotonin and acetylcholine can be inhibited and the pain experience, thus modified.
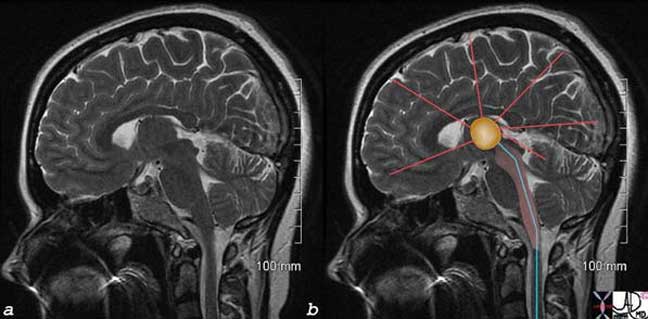
The image represents a coronal cut of the brain attained using T2-weighted MRI technique. It reveals a second order neuron (blue) traversing the medulla, pons, and midbrain, and in its path the fibers activate the RAS (pink). The stimuli reach the thalamus (orange) which not only activate the sensory cortex but also other parts of the cortex as well, as shown by the red lines. As a result, the limbic system and autonomic system are activated.
Courtesy of: Ashley Davidoff, M.D.
Basis of Pain Therapy: Antidepressants
Tricyclic antidepressant medications are essentially designed to suppress the synthesis of indolamines and catecholamines in the CNS to improve mood and decrease anxiety. A second function of these drugs is to provide cAMP inhibition and thus, increased synaptic concentrations of serotonin and acetylcholine leading to better regulation of sleep patterns and an increase in pain threshold. Their third property is to increase concentrations of enkephalins in the periventricular areas of the brain and provide a morphine-like effect.
Another class of antidepressants known as selective serotonin reuptake inhibitors (SSRIs) enhance serotonin levels even more than the tricyclics because they can specifically target the presynaptic serotonin mechanism. Postsynaptic inhibition can increase catecholamine levels and offset the analgesic result.
Anxiolytics
This group of compounds known commonly as sedative tranquilizers exhibits various mechanisms of action that mitigate the anxiety that complicates pain. The first of these agents are the phenothiazines. They have direct and indirect analgesic effects and are indicated for chronic pain. The second group is the benzodiazepines, indicated only for acute pain therapy due to their long-term addictive hypnotic and withdrawal properties. Benzodiazepines are considered indirect analgesics because they only treat the sequelae associated with pain. Two other categories of drugs with anxiolytic effects are azapirones and hydroxyzine, an antihistamine.
Phenothiazines
The phenothiazine class (fluphenazine, trifluoperazine, and perphenazine) have a minimal, net analgesic effect as they block both postsynaptic dopamine, an analgesic and norepinephrine, a pain promoter. They do, however, inhibit the enzymatic degradation of enkephalins thus increasing their morphine-like effects. These agents also block postsynaptic noradrenergic receptors, thereby lessening the pain intensifying effect of the sympathetic nervous system. Finally, when used in combination with tricyclic antidepressants, phenothiazines exhibit their strongest influence on pain by decreasing anxiety and promoting sleep. Medications from this class are relatively free of addictive properties and are therefore frequently an important component of the drug regimen for chronic pain patients.
Benzodiazepines
The benzodiazepines including midazolam (Versed), alprazolam (Xanax), flurazepam (Dalmane), diazepam (Valium), chlordiazepoxide (Librium), oxazepam (Serax), chlorazepate (Tranzene), lorazepam (Ativan) and clinidium bromide (Librax) aid in the treatment of pain in two indirect ways. First, they act on specific receptors in the CNS to reduce anxiety. Second, they competitively inhibit glycine receptors at the level of the spinal cord to reduce spasm, a major contributor to somatic pain. These drugs therefore have some use for pain in the acute setting. However, there are many potential problems with this drug class, especially in the treatment of chronic pain.
We know that serotonin is an effective pain reducing neurotransmitter in the CNS. Benzodiazepines actually lower serotonin levels thereby decreasing its pain dampening effects and the overall pain threshold. This is achieved via a third mechanism of action, inhibiting gamma aminobutyric acid (GABA) receptors that normally facilitate the presynaptic release of serotonin. These agents also reduce rapid eye movement (REM) sleep, another serotonin building process. Benzodiazepines are unfortunately also highly addictive for their sedative effects. In addition, their activity on GABA receptors can be anticonvulsive, similar to alcohol or phenobarbitol. Consequently, sudden withdrawal from these agents can cause seizures.
Hydroxyzine (Vistaril) is an antihistamine that plays an important role in reducing acute anxiety associated with chronic pain flare-ups. More importantly, however, this special antihistamine reduces the experience of drug withdrawal especially from benzodiazepines by rebalancing REM sleep patterns.
The azapirones include buspirone, gepirone and ipsapirone and are another class of anxiolytics that potentiates the expression of the serotonin specific 5-HTIA receptor. These drugs therefore contribute to reducing pain anxiety and also exhibit antidepressive effects.
Muscle Relaxants
Muscle spasm is a mechanical pain response and is often a major contributor to an already unpleasant experience. Muscle relaxants can work centrally in the spinal cord or peripherally. The central agents like baclofen in the treatment of multiple sclerosis, for example, act similarly to the benzodiazepines inhibiting glycine and GABA receptors and reducing the involuntary spasms associated with this disease. The most common peripheral muscle relaxant prescribed is cyclobenzaprine (Flexeril). Its mechanism of action is not well-understood but is related to increasing local levels of norepinephrine within the muscle spindle. This agent, however, has some central effects as its common side effects include drowsiness, blurry vision and depression.
Anticonvulsants
Carbamazepine (Tegretol) in the treatment of trigeminal neuralgia and valproic acid and gabapentin (Neurontin) for other post-therapeutic neuralgias are effective suppressors of non-nociceptor neuronal pain. Their mechanisms are not well-understood. Neurontin is also very effective for diabetic neuropathy.
Special Considerations
Other agents effective for specific pain syndromes include propranolol for chronic vascular headaches, phentolamine for reflex sympathetic dystrophy, mexiletine for diabetic neuropathy and L-dopa in the treatment of bone metastases. Again, their mechanisms of action are poorly understood and many of the therapeutic indications lack prospective randomized trials.
Modifying the CNS – Opioids
Opioid medications include morphine and several other synthetic and naturally occurring narcotics. These analgesics have a far different pharmacologic mechanism for reducing pain than previously mentioned. Opioids bind specifically to a heterogeneous group of receptors in the CNS but cast their analgesic effects both centrally and peripherally on nociceptive first and second order neurons.
Peripherally, opioid receptors exist in their highest concentrations within the presynaptic terminals of first order neurons within the substantia gelatinosa in the dorsal horn of the spinal cord. They are also plentiful on the postsynaptic dendrites of the second order and interneurons that modify the pain signal during spinothalamic transmission. Via their competitive affinity for the presynaptic receptors, opioids inhibit the release of substance P and glutamate into the synapse of afferent neurons thus mitigating the action potential of the pain signal. This phenomenon occurs with nociceptive, sympathetic and motor neurons.
Centrally, opioids dampen the limbic system response and the emotion, anxiety and sleeplessness of pain. They also activate descending pain inhibitory pathways from the medulla and periaqueductal gray matter which attenuates ascending nociceptive transmission. Lastly, opioids can provide direct inhibition on the first order neurons in the spinal cord.
Opioid receptor binding is a steric specific phenomenon. There are multiple subtypes of these receptors and a variety of molecular structures comprising synthetic and natural opioid compounds. Once bound, the receptor/opioid complex undergoes a morphological change that minimizes potassium and sodium ion channels and therefore directly inhibits conduction of the pain impulse. At the nociceptor level, the action potential is blunted in amplitude and duration thereby reducing calcium ion influx and the subsequent release of substance P and glutamate.
The physical and chemical properties of the opioids determine the speed of onset, duration and potency of the analgesic effect. Some drugs of this class may completely override the pain signal while others may require adjuvant anti-inflammatory or anesthetic agents. Pure agonists have the strongest affinity for receptors that influence the presynaptic terminal to produce a purely opioid effect. Morphine, fentanyl and hydromorphone are the naturally occurring pure agonists. Codeine, oxycodone (1 ½ times the potency of morphine) and hydrocodone are synthetic examples of pure agonists. Severe acute pain and chronic cancer pain are the afflictions most commonly treated with these analgesics.
Opioid antagonist activity in contrast is a property of the drug nalaxone, used to reverse the narcotic effect of morphine-like drugs in overdose situations. Nalaxone has no intrinsic anti-analgesic activity but competitively displaces the opioid from its receptor. It is commonly available in urban emergency rooms for obtunded addicts.
Agonist/antagonists have hybrid binding owing to the steric heterogeneity of the opioid receptors. Pentazocine, butorphanol, nalbuphine, and buprenorphine define this class. Their analgesic properties have a ceiling that limits their use in cancer pain for example. Higher doses of this opioid class may also have psychogenic effects.
Modifying the CNS – Opioids: Opioid Side Effects
The use of opioids requires careful consideration and review of a patient?s pain scenario due to their potentially dangerous side effects and the risk of tolerance and addiction.
Unfortunately, opioid receptors exist in the GI tract and their suppression can inhibit motility leading to the most common side effects ranging from constipation to nausea and vomiting. When severe enough, bowel obstruction may occur. Opioid receptors also exist in the respiratory centers of the brain and opioid analgesics may consequently inhibit proper respiratory drive, especially in high doses. Other negative side effects exist and should be reviewed prior to their use. All opioid analgesics must be administered carefully so as to maximize safety.
Tolerance to opioids is a phenomenon where a patient chronically taking an opioid gradually loses the ability to obtain an analgesic effect. There are two tolerance classifications. The first is behavioral tolerance. At low or less frequent dosing intervals, this phenomenon usually occurs as a consequence of habitual associations. The tolerance is more of a learned behavior. Pharmacological tolerance on the other hand is seen in higher and more consistent dose intervals. This is truly a drug interaction where physiological adaptations of the opioid receptors occur. When withdrawal of the opioid causes stressful physiological sequelae and craving, the situation may be described as physical dependence. The point where drug seeking behavior is constant and life-altering is known as addiction. The patient is overwhelmed by the need to fulfill the analgesic effect. Drug addiction is a reality in any clinical setting where chronic pain therapy is administered. Prompt recognition and communication among colleagues, patients and their families is essential in getting those who are within its grasp into a harmonious balance of pain control and independence.
Modifying the CNS – Opioids: Administering Opioids
Intraspinal
Opioids have a wide range of effects on neuronal excitability predicated on their preparation and the route of administration. Their bioavailability increases their potency in correlation to the level of invasiveness of drug delivery. One of the most common therapies for severe acute pain, especially with obstetric labor, is intraspinal therapy. The opioid is delivered via a small catheter placed in the spinal or epidural space within the spinal column. Chronic back pain treatment can be administered with the use of an implanted spinal infusion pump. The advantages of intraspinal therapy are more complete analgesia at lower doses of opioid and fewer of the sedating or GI side effects of the drug.
Tramadol is a synthetic opioid analog that achieves central analgesic effects without binding to opioid receptors. It is the only one of its kind and is indicated for many pain syndromes, especially neuralgias. Although it may also cause GI and respiratory side effects, they are less severe and without the hazards of drug dependence.
Local Injection
Opioids are often formulated with an anesthetic and/or steroid for injection or infusion to a body area for chronic pain. These cocktails often provide effective analgesia especially in inflammatory or neuronal pain syndromes. The honeymoon relief, however, usually has an endpoint and repeated therapeutic injections are common.
Injectable analgesic preparations are also useful as regional blocks where a nerve plexus or ganglion is causing chronic pain. Stellate ganglion block for cervical radiculopathy is a good example. Nerve block therapy may also provide relief to areas that cause visceral pain. Chronic pelvic pain can improve with hypogastric plexus block and celiac plexus block is sometimes useful for chronic abdominal pain. There are risks to these procedures including dysfunction of adjacent organs or systems.
The use of these techniques, especially for the treatment of chronic pain, has generated an entire field of medicine due to its prevalence in society and the inherent risks of addiction. The evolution of anesthesiologist directed pain clinics where these procedures can be performed safely has dramatically improved the support network for chronic pain patients.
Opioids: Surgical and Interventional Techniques
Surgical treatment is commonly indicated to relieve pain. Decompression of localized skin abscesses brings rapid relief. Surgical procedures that reduce or treat distension or obstruction always bring pain relief. The treatment may be as simple as placing a nasogastric tube to reduce the distension of bowel obstruction, but may require more complex surgery such as removing a tumor that has created the bowel obstruction. Sometimes the relief comes from treating disease that has its origins in obstruction as well as inflammation and/or infection. Acute cholecystitis and appendicitis are such instances. The organ is initially distended by an obstructive cause and then it becomes secondarily infected. Removing the gallbladder or appendix treats the root cause of pain and then the healing process will need medical support for pain relief. Ischemia is another cause of pain that can be treated by the surgeon or minimally invasive interventionalist. Stenosis of an artery will cause ischemia and pain such as in angina. A few treatment options are available including angioplasty, stent placement or bypass, each of which will restore normal flow and treat the pain. Infarction is also painful, and in the case of bowel infarction the injured bowel has to be surgically removed. The pain from trauma is multifaceted but includes somatic and visceral pain from tissue injury, and continued tension from swelling, hematoma and misaligned bones for example. With accurate diagnosis, the approach to trauma and treatment of pain in these patients is also multifaceted.

The CT scan is from a 33-year-old homosexual patient who presented with severe rectal pain and fever. He was unable to bear even the slightest weight on his perineum and had been sleepless. The CT scan shows a small fluid collection in the rectal wall (a, b, orange matrix with surrounding red inflamed wall). CT guided percutaneous aspiration with the patient in prone position (c, d) and drainage of 10 cc of pus resulted in immediate relief of his pain. The tip of the needle (c and arrow in d) is in the completely drained small abscess cavity. The location with both somatic and visceral nociceptors and distension caused exquisite pain and required decompression for immediate relief.
Courtesy of: Ashley Davidoff, M.D.
Conclusion
The treatment of pain is a challenge to all caregivers. Knowledge of the pain pathways, their physiology, the pathophysiology of pain and the treatment options is necessary for those involved in the diagnosis and treatment of pain.
Treatment sometimes involves the mere removal of a noxious element. At other times it is the preemptive use of anesthesia, while at others it is the prudent use of appropriate analgesia. Pain, of course, may underlie serious disease, and before embarking on therapy it behooves the caregiver to be aware of life-threatening diseases that if they go undiagnosed, and furthermore masked by premature treatment, a fatal outcome is possible.
The creation of a comprehensive pain treatment plan requires a thorough understanding of the pain source, the pharmacological properties of any proposed analgesics and the patient?s background. Once implemented, social support and close patient surveillance will optimize outcomes and minimize risk. One must remember, however, that across all patient cohorts, pain is both a necessary evil and a valuable tool requiring medical knowledge, measured inquisitiveness and empathy. As clinicians navigate through the various pain modules of this site and gain practical experience, it will become apparent that pain and its treatment are rarely the same among patients. This imperfection is one of many in medicine but it underscores the artistry necessary to practice the discipline.

