Applied Anatomy of the Pancreas

Learning Objectives
Describe the basic anatomy of the pancreas
Locate this organ within the abdominal cavity and identify the main structures of the pancreas utilizing cross sectional medical imaging
Discuss the pancreas’ function and its relation to the other organs in the abdominal region
Describe the basic pathological conditions of the pancreas and how these may affect its structure and function
Compare and contrast normal and abnormal images of the pancreas
Differentiate the role of CT, US, and MRI in imaging studies of the pancreas
A comprehensive course on the anatomy of the pancreas and how to apply that knowledge within medical imaging.
by Dr. Ashley Davidoff
Introduction
The word pancreas derives from the Greek words ?pan? meaning ?all ?and ?kreas? meaning ?meat ? since it was thought to be made of muscle. It is however not a muscle but an elongated glandular structure that is soft and fleshy, and is situated in the retroperitoneum behind the stomach and the duodenum. It secretes pancreatic enzymes into the duodenum which aid in the digestion of fat, proteins, and carbohydrates, and it is a key player in the control of glucose metabolism which it accomplishes by secreting insulin into the circulation. It thus functions as both an exocrine gland (secretes into ducts) and an endocrine gland (secretes into the circulation).
The pancreas was known as the ?hermit of the abdomen? since it was considered for many years a mysterious and lonely figure that lay deep in the abdomen. Over the years, knowledge of the function of the pancreas evolved, but it is only in recent years with the advent of, and advances in angiography, ultrasound, CT and MRI that it?s in vivo structure has become understood. It is well connected to many organs, and is central to many functions and structures. Together with the? all meat? misnomer its status as ?hermit of the abdomen? are mere historic curiosities at this time.
Principles
In this section we explore the principles that govern the gland hoping to give a perspective of the structural and functional features that are common to all glands and tubular systems in the body.
Since the pancreas is a gland it is, like all glands, composed of epithelial cells that are specialized to synthesize and secrete active substances that contribute to functionality in the body. It has both the endocrine type of gland that secretes insulin and glucagon into the blood and an exocrine portion that secretes digestive enzymes, proenzymes (zymogens), and an aqueous solution of bicarbonate into the ducts. The enzymes are secreted by the acinar part of the gland while the bicarbonate solution is secreted by the ductal portion of the gland. The stomach produces an acidic environment for recently ingested food to facilitate the function of one its major hormones called pepsin which breaks down proteins to peptides. The bicarbonates produced by the pancreas neutralize the acid PH of the chyme (partially digested food) of the gastric contents that enter the duodenum in order to optimize the PH for pancreatic enzyme function. About one liter of fluid is produced and transported per day.

Courtesy of: Ashley Davidoff, M.D. 39939b04
Glandular Principles

Courtesy Ashley Davidoff, M.D. 32645a06
The epithelial layers of both glandular systems are anatomically designed in ?clusters of grapes? formation, to increase the surface area available for rapid and efficient production and transport of hormones, enzymes and serous fluid.
As an endocrine gland, the pancreas is endowed with a rich blood supply since it has to secrete the hormones it produces into the circulation in order for the hormones to have a rapid and far reaching effect. The islets of Langerhans secrete insulin into the blood stream, very soon after ingestion of a meal in order to control blood sugar and intracellular glucose concentrations. The islets of Langerhans represent only 1-2% of the tissue volume of the pancreas, but play a vital role in body function and well-being. They are most numerous in the tail of the pancreas.
Glucagon is the second hormone that is secreted by the islets of Langerhans, and like insulin is also pivotal in glucose metabolism. While insulin serves to drive the blood levels of glucose down by shifting the glucose from the blood into the cells, glucagon serves to bring glucose into the circulation by stimulating the liver cells to break down glycogen and amino acids to form glucose.
Within the islets, there are four types of cells. They include the alpha cells, beta cells, delta cells and PP cells. The alpha cells secrete glucagon and make up about 15-20% of the cell volume. The beta cells are responsible for insulin secretion and make up 65-80% of cell volume. The delta cells secrete somatostatin,and make up 3-10% of cells volume of the islets. Somatostatin is responsible for inhibiting secretion of hormones including growth hormone, thyroid stimulating hormone (TSH), cholecystokinin (CCK), gastrin and secretin. The PP cells make up 1% of the islets and they secrete pancreatic polypeptide. The exact role of pancreatic polypeptide is unclear, but it seems to affect the secretion of pancreatic enzymes, water, and electrolytes.
The pancreas receives its rich blood supply from branches of both the celiac axis and the superior mesenteric artery (SMA).

Courtesy of: Ashley Davidoff, M.D. 32164b02
Tubular Principles
The exocrine pancreas requires a tubular system in order to transport its hormones. Tubular systems are universal throughout the body. The arterial, venous, lymphatic, ductal, gastrointestinal, and genitourinary systems are classical examples.
As a serous exocrine gland, the pancreas secretes about a liter of relatively thin pancreatic juice into its ductal system per day. The epithelial cells secrete a fluid containing the enzymes and bicarbonate into the pancreatic duct, which like all the other tubes, is subject to the laws that govern flow in a tube. Some of the factors that need consideration relating to flow include:
-
- the radius and length of the tube
- the pressure differences between the upstream side and the downstream side of the tube
- viscosity of the medium that is being transported
- the friction that occurs between the fluid being transported and the lining of the tube
The flow in the duct is relatively slow and laminar and thus will be governed by Poiseuille’s law, which states that velocity of flow is directly proportional to the driving pressure.
Poiseuille’s law – for laminar flow
Volume flow rate = pressure difference
viscous resistance
= P1-P2
R
= ? X pressure difference X radius4
8 X viscosity X length
Quiz Me
How much pancreatic juice does the pancreas secrete per day?
(Note: You will be given 2 tries to answer this question, then the answer will be provided.)
1 gram
1 ounce
10 ounces
1 liter
Tubular Structure
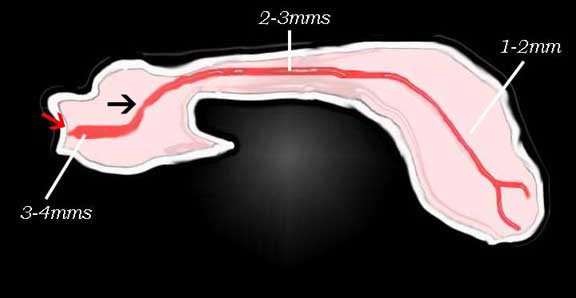
The main duct is relatively small measuring 1-2 mm in diameter and it measures between 10-20 cms in length, while the pressure difference between upstream and downstream portion of the duct is also very small compared to the vascular circulation, and the viscosity of the pancreatic fluid is also relatively low compared to blood.
Thus flow in the pancreatic duct is relatively straight forward, tends to be laminar (non-turbulent) and relatively slow compared to the circulation. The complexity of the flow and delivery in this system relates to the sluice (waterfall) gate called the ampulla which controls the flow into the duodenum.
The pancreatic duct has a common sphincteric mechanism which is housed in the ampulla, for the combined flow of bile and pancreatic juice. The sphincter is known as the sphincter of Oddi, which is under hormonal and autonomic nervous system control, responding to the digestive needs.
The pancreatic system is beautifully designed to enable rapid and efficient delivery of pancreatic enzymes in response to a reflex that identifies fat, protein or carbohydrates in the stomach and duodenum. Tactile stimuli, chemical stimuli, and autonomic nervous stimuli excite the glands to produce the serous fluid with appropriate enzymes. The vagus nerve begins the process by getting the engines of secretion fired up as the brain anticipates the start of a meal by thinking about, seeing, smelling, and tasting the food. The vagus is a parasympathetic nerve which innervates the pancreas. It is part of the autonomic nervous system.
Cholecystokinin (CCK) is a hormone that is secreted into the blood by duodenal cells in response to the presence of food in the duodenum. Once in the bloodstream it is activated, and subsequently hooks onto the receptors in the gall bladder wall, exocrine cells of the pancreas, and the sphincter of Oddi. It causes contraction of the gallbladder, stimulation of full production of pancreatic juices, and flow of both bile and pancreatic fluid by opening the sphincter of Oddi. Timing of the delivery of the fluid has to coincide with the passage of the chyme through the duodenum and small bowel. Unlike the biliary system which has a gallbladder for bile storage, there is no storage capacity for the pancreatic juices. The pancreas therefore has to go into full production and delivery on demand, in response to the presence of food in the stomach and duodenum.
Secretin is a second hormone produced by the duodenum, but it is secreted in response to the acidic PH of the chyme in the duodenum. Its presence in the circulation is identified by receptors in the ducts of the pancreas and stimulates them to produce the bicarbonate rich serous fluid that will neutralize the acid and provide an optimal PH for the enzymes to function.
Gastrin is the last major hormone that controls production and flow of pancreatic juices. It is produced by the stomach as a result of gastric distension. It helps initiate and control secretion and flow of pancreatic juice.
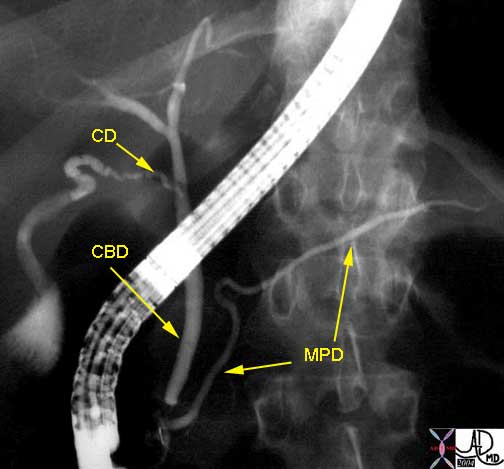
The sphincter of Oddi controls the flow. It consists of circular and longitudinal muscle bundles and is a common bundle that also individually surrounds the bile duct and the pancreatic duct within a common structure called the ampulla of Vater. The papilla is the end of the ampulla and is the only structure of the pancreaticobiliary system that is visible from the duodenum. The papilla is the structure that the endoscopist needs to identify in order to perform an ERCP (endoscopic retrograde cholangiopancreaticography). Once the papilla is identified the pancreatic duct and distal bile duct are cannulated and diagnostic and therapeutic maneuvers can be performed.

Courtesy of: Ashley Davidoff, M.D.
32645b04b04
Quiz Me
Which hormone causes contraction of the gallbladder, stimulation of full production of pancreatic juices, and flow of both bile and pancreatic fluid by opening the sphincter of Oddi?
(Note: You will be given 2 tries to answer this question, then the answer will be provided.)
Cholecystokinin (CCK)
Secretin
Gastrin
Somatotropin
Application to Diseases
In diseases such as cystic fibrosis the fluid being transported is significantly thickened and forms inspissated (thickened) concretions that not only are slow to move but also may eventually be unmovable, limiting upstream flow and causing obstruction. In diseases where the tube is damaged and narrowed such as in carcinoma of the pancreas, or pancreatitis, the resulting stricture will inhibit flow and the upstream component will be dilated and the downstream portion decompressed.
When there is malignant transformation of the cells in the pancreas, the likelihood of developing an adenocarcinoma originating in the exocrine portion is much higher than from the endocrine portion since the exocrine portion is so dominant by sheer volume. As stated, 98% of the cellular volume of the pancreas is exocrine and only 2% endocrine. Thus adenocarcinoma of the exocrine pancreas is far more common than the tumors of islet cell origin.
Adenocarcinoma of the exocrine pancreas also shows characteristic desmoplastic (fibrotic) response. This fibrotic response results in encasement of ducts, arteries, veins, and lymphatics and has important clinical, imaging and prognostic significance.
Quiz Me
The cellular volume of the pancreas is made up of 98% exocrine and only 2% endocrine?
True False
Application to Imaging
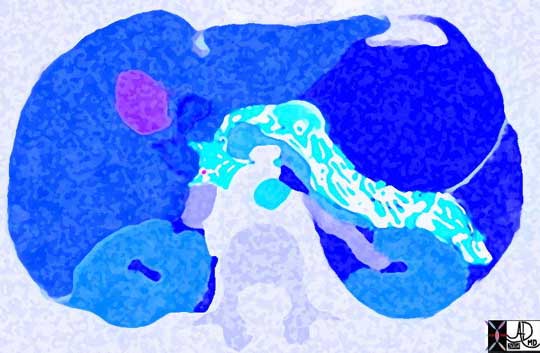
One of the main distinguishing features that separate endocrine tumors from exocrine tumors of the pancreas on CT, MRI, or angiography, is tumor vascularity. Since the endocrine system is so intimately related to the vascular system, it is not surprising that these tumors are hypervascular and therefore early arterial phase imaging in CT and MRI is important for diagnosis. They also tend to be larger when identified because unless they are functioning tumors they are relatively asymptomatic until late in disease. Additionally since the islets are more prominent in the tail of the pancreas, the endocrine tumors tend to be more common in the tail.
The exocrine tumors, which are the more common forms of cancer, are hypovascular and show characteristic fibroblastic reaction. Encasement of bile ducts, pancreatic ducts, arteries, veins and nerves is not uncommon. Strictures of the bile duct causes jaundice, and involvement of the nerves causes pain. Involvement of the blood vessels usually has no clinical correlate, but does have prognostic significance. As a result of the fibroblastic changes and strictures that form, exocrine adenocarcinomas present earlier when the tumor is relatively small. Despite this, the prognosis for this tumor is dismal.

Courtesy of: Ashley Davidoff, M.D. 05008
Quiz ME
Endocrine pancreatic tumors are hypovascular and show characteristic fibroblastic reaction.
True False
Size of the Pancreas
The variation of size and shape of the pancreas in the young and the old, males and females and among different individuals is remarkable and it is no surprise to find that each pancreas has a unique ?face?. Measurements should therefore only be used as a rough guide in the evaluation, and other factors such as patient profile, and the shape, character and perfusion characteristics of the gland are also important in the overall evaluation.
In young patients, the body or the tail may be larger than the head, whereas in people over 40 the head assumes larger proportions than the body and tail. When the pancreas is young, the surface of the pancreas is relatively smooth. As it ages the earliest signs of volume loss is development of a nodular shape of the surface. Thus, the shape deformity reflects an involutional process and assessment of the shape gives insight into the size and approximate age of the gland.
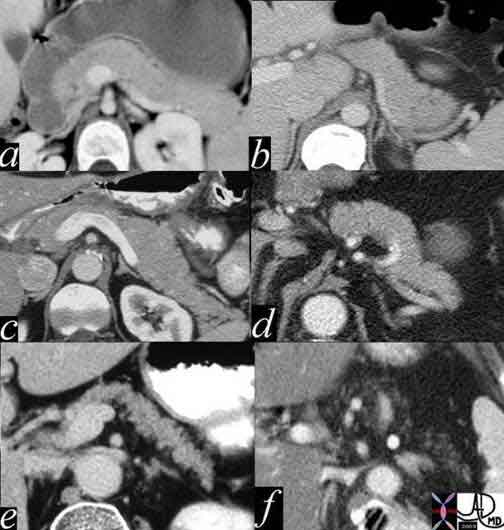
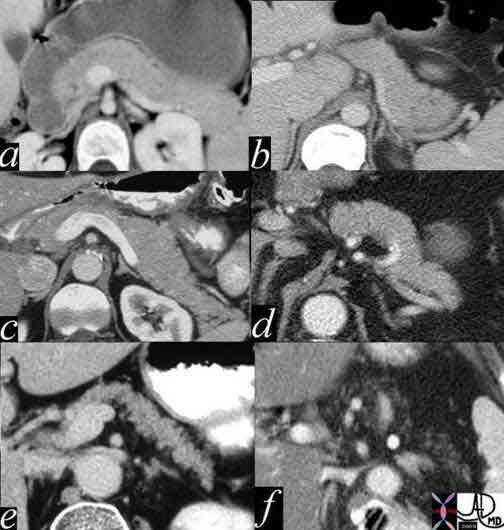
It is relatively large in youth and young adults (a= 12 year old female b= 30 year old female), starts to thin in middle age (c= 30 year old male d= 40 year old male), and atrophies in the elderly (e= 70 year old female f = 80 year old female).
Courtesy of: Ashley Davidoff, M.D. 1394size02
There are observed experimental changes in the size of the pancreas during differing physiological states. During digestive process, the gland is most active, and swells as it secretes hormones and enzymes. These changes are not visible on conventional imaging.
The involutional change with age is very common and most of the time has no clinical significance. In fact sometimes the pancreas is almost completely replaced by fat, and it still functions normally. For the pancreas to lose exocrine function, more than 90% of exocrine pancreatic tissue needs to be lost. This occurs with diseases of the pancreas exemplified by chronic pancreatitis. The patient would present with failure to thrive, steatorrhea, fat intolerance, abdominal pain, bloating, and flatulence.
With aging there is an increased incidence of type II diabetes. This is probably not only as a result of critical loss of insulin secreting beta cells from the islets, but also other factors that relate to decreased efficacy of the insulin.
Sometimes the pancreatic duct size gives a clue to pancreatic volume. Chronic obstruction of the duct will lead to atrophy of the gland. This may be due to a stone in the duct, or a neoplasm in the neck or head. A relative discrepancy in the size of the tail and the size of the head in the presence of a dilated pancreatic duct raises the distinct probability of an upstream pancreatic carcinoma or obstructing benign mass or stone. On the other hand when the primary entity is gland atrophy as seen with advancing age, the duct also appears more prominent.
Size Guidelines
There are approximate measurements that one can use if subjectivity of the size assessment fails. These measurements are outlined below.
A-P dimensions (approximations)
-
-
- head about 2.5 cm -3.5cms.
- neck about .8cms-1.5cms
- body about 1.5cm – 2.5cm
- tail about 1.5 cm-3.5cms.
-
Weight
-
-
- 60 to 100 gm
-
Length
-
-
- 12-15 cm in length
-
Application to Disease
In disease, a small pancreas is much more common than a large pancreas. However since the size of the pancreas is so variable and the pancreas decreases in size with age even a “small” pancreas could be normal. Overall volume loss of the gland is usually caused by aging, chronic pancreatitis, or by an obstructed pancreatic duct. Diffuse enlargement of the gland is an uncommon finding and may be caused by acute pancreatitis, lymphoma, and metastasis to the gland. If however, the duct is enlarged in the presence of the small pancreas, then an upstream obstructing pathological process such as carcinoma should be excluded.
Quiz ME
Decrease in size and overall volume loss of the pancreas is usually caused by ______.
(Note: You will be given 2 tries to answer this question, then the answer will be provided.)
aging
chronic pancreatitis
obstructed pancreatic duct
all of the above
Application to Imaging
Unlike most organs that are inflamed, the relative degree of swelling and enlargement of the pancreas in severe pancreatitis is minimal. This is probably because the pancreas has very little in the way of a capsule and most fluid that exudes from the pancreas leaks into the surrounding tissues causing a peripancreatic effusion.

Image a: There is extreme atrophy of the gland, but with a normal duct. This finding may be normal. The pancreas can barely be identified between the contrast filled stomach anteriorly and the splenic vein posteriorly.
Image b: There is atrophy associated with an abnormally dilated duct. This finding is usually abnormal and is usually caused by pancreatitis or carcinoma.
Image c: Hemorrhagic pancreatitis. The pancreas has areas of subtle increase in density reminiscent of hemorrhage. There is an anterior pancreatic effusion.
Image d: Pancreatitis in a transplanted kidney. In this instance the pancreas is swollen.
Image e: von Hippel Lindau syndrome Subcentimeter low density tumors are scattered throughout the gland.
Image f: Metastatic enlargement of the pancreatic lymph nodes in this patient with metastatic Merkel cell tumor has resulted in a global enlargement of the gland.
Courtesy of: Ashley Davidoff, M.D 41394size04
As a retroperitoneal organ behind the stomach and framed by gas filled small and large bowel, the pancreas sometimes is sub optimally visualized by ultrasound. This is particularly true in diseases such as pancreatitis when small bowel ileus results in gas filled bowel, which inhibits the interrogating ultrasound wave and hence the view of the pancreas. Filling the stomach with water sometimes does aid in the examination by acting to improve ultrasound transmission. The tail of the pancreas is sometimes hidden from view in the epigastric window, and can sometimes be only visualized when the spleen is used as an imaging window.
CT is far better suited to provide consistent imaging of the retroperitoneum. It easily can circumvent the problems discussed with ultrasound transmission. The MDCT technology has allowed exquisite detail to be portrayed by CT, and it promises only to improve in the future. The presence of disease is sometimes only suggested by subtle thickening of Gerota’s fascia or the lateral conal fascia – detail that can only be portrayed by CT. For the retroperitoneum – MDCT is both the king and the queen of pancreatic imaging.
Quiz ME
A gas filled small bowel can make it difficult to view the pancreas on ultrasound?
(Note: You will be given 2 tries to answer this question, then the answer will be provided.)
True False
Shape of the Pancreas
In a word, the shape of the pancreas is ?odd?. The pancreas has been compared to many objects including an elongated comma on its side, an elongated number 9 on its side, a prism, a banana, an inverted and curved upside down tobacco pipe, and even an old fashioned revolver. Placing a seahorse or a woodpecker with head down and tail up probably brings us closest to the complex shape of the pancreas. The objects used for description are so varied, that one wonders if we truly have a grasp of the shape of this organ. A more practical way to look at the shape of the organ is to define the shape of its component parts.
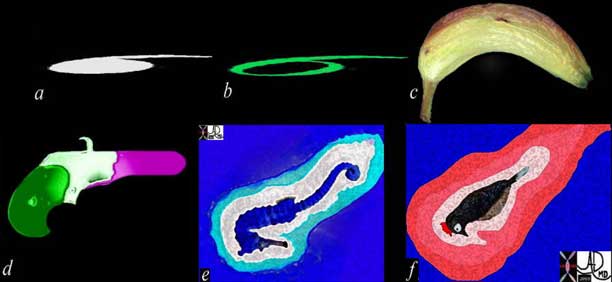
Courtesy of: Ashley Davidoff, M.D. 1502
We will devote some time to the description, because subtle change in the shape may reflect important underlying disease. Identification of this alteration can mean the difference between making an early diagnosis of pancreatic carcinoma and saving a patient from a horrible disease, or missing the diagnosis and losing the opportunity. Adenocarcinoma of the pancreas is usually a rapidly fatal disease but the few who are fortunate to survive the illness have had the diagnosis made early, when surgical resection was feasible. It is imperative that routine assessment of the pancreas should focus on subtle shape and textural changes.

Courtesy of: Ashley Davidoff, M.D. 25034f
The Head
The head has the most complex shape. It is generally considered to be globular as viewed in the coronal and A-P projection, while it is almost teardrop in shape when viewed in the sagittal plane. It is the medial and lateral extensions of the head that contribute to its complexity.
The uncinate process is the medial extent of the head and true to the origin of the word is hook shaped. In Latin ? ?uncus? means “hook”. It shares its Latin origins and shape with at least six other structures in the body, including the uncus of the hippocampal region in the brain, as well as multiple bones including the ethmoid, cervical vertebra, scapula, hamate, and third phalanx of the foot.
The head of the pancreas lies within the duodenal curve, and is surrounded by many important structures including the antrum of the stomach, the posterior aspects of the liver, the anterior aspects of the kidneys, the hilum of the spleen. Blood vessels including the splenic vein, splenic artery, SMA, SMV portal vein, IVC and aorta, are intimate relations while within it lie the distal bile duct, terminal portions of the major and minor pancreatic ducts.

Courtesy of: Ashley Davidoff, M.D. 39864b
The Head Continued

Courtesy of: Ashley Davidoff, M.D.

Courtesy of: Ashley Davidoff, M.D. 41502c02
The Neck
The neck of the pancreas usually merges imperceptibly with the body and head. In general as we view the pancreas in the transverse plane, the neck is marked by a point where the globular head transforms into the more rectangular shaped neck.
Anteriorly its rightward border is marked by the gastroduodenal artery and the groove for this vessel sometimes forms a distinct notch in the neck in which case the border is delineated by a focal constriction. The outer anterior border may be rounded or flattened. The left margin anteriorly is marked by the tuber omentale, a focal prominence, which abuts the posterior surface of the lesser omentum. The inner posterior border is grooved by the superior mesenteric vein (SMV) with the portal vein confluence, and has a concave shape that runs parallel to the anterior border.
Like the neck of most structures its overall size is less than the head and the body, the two structures which it connects. It can however be short and fat or long and thin.
The neck is about 2-2.5cms cm long, and projects forwards, upwards, and to the left from the head, merging imperceptibly into the body.
The neck of the pancreas is at special risk following blunt abdominal injury.

Courtesy of: Ashley Davidoff, M.D. 38025c003
Quiz Me
The anterior left margin of the pancreatic neck is marked by the __________, a focal prominence which abuts the posterior surface of the lesser omentum.
(Note: You will be given 2 tries to answer this question, then the answer will be provided.)
tuber omentale
uncus
ampulla
islets of Langerhans
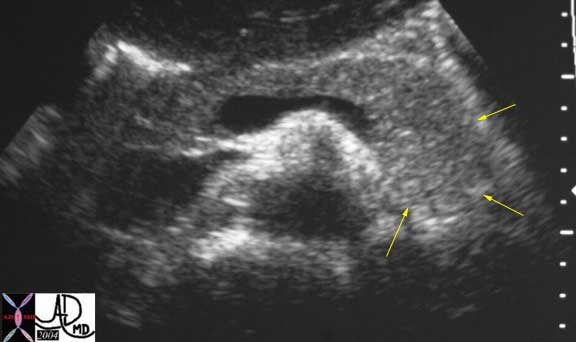
The Body
The body and tail of the pancreas are less complex and form an elongated and irregularly prismatic structure. In cross section, the body and tail have an anterior, posterior, and inferior surface making up the three borders of the 3-sided prism. This prismatic shape is best appreciated on a longitudinal view of the pancreas using ultrasound. (see ultrasound image below) The superior aspect of the pancreas is not usually appreciated on axial imaging due to its narrowed format and the intimate association with the splenic artery which partially volumes the interface. At the neck body interface anteriorly, a small protrusion called the omental tuberosity or tuber omentale, arises from its superior and anterior border, just inferior to the origin of the celiac axis.

Courtesy of: Ashley Davidoff, M.D.
Courtesy of: Ashley Davidoff, M.D. 41505c02
The Tail
The tail is a continuation of the three-sided prism. It is usually narrowed and thinned and sometimes almost pointed at the left extremity. In the young, it is more commonly thickened, flattened, or bifid. The tail usually reaches the inferior part of the gastric surface of the spleen. It is contained between two leaves of the splenorenal (lienorenal) ligament together with the splenic vessels. Its end usually contacts the hilum of the spleen. The exact junction of the body and tail is not defined anatomically. Its size and shape is variable and it may be narrow and pointed, thick and rectangular, or even bifid.

Courtesy of: Ashley Davidoff, M.D. 41505c03
Courtesy of: Ashley Davidoff, M.D. 25043
Application to Disease and Imaging
The shape of the pancreas as noted previously, has wide variation depending on the part of the pancreas under consideration, age of the patient, body habitus, and normal and abnormal structures surrounding the pancreas. In general it is reasonable to divide the pancreas into two parts for the evaluation; the neck, body, and tail as one entity, and the head, uncinate process, and ventral remnant as the second entity. The reason for doing this is that neck, body, and tail can usually be evaluated as one entity over a short craniocaudad distance and usually have similar texture and character. The head is usually the most inferior part, lies in a different axial plane, and is slightly more complex in its structural makeup. It has a wide range of variability and has the added component of the bile duct and ampulla to consider since they are so intimately related and connected.
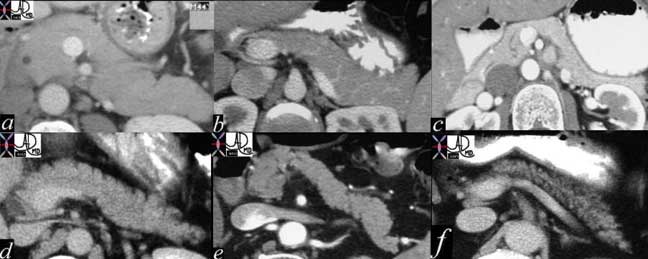
Probably the most important and most difficult challenge in pancreatic evaluation is the need to identify an early asymptomatic carcinoma of the pancreas. Shape deformity and aberrance in enhancement pattern are the key issues to keep in focus. The ductal acinar carcinoma represents the most common form of carcinoma. Its most important characteristic is that it has poor blood supply and presents as a hypovascular mass. In the body and tail it is not difficult to identify, but in the head and uncinate process the “normal heterogeneity of the head, created by the distal bile duct, downstream pancreatic ducts, and a limited space where so many structures are converging. Meticulous attention to technique with a contrast filled and distended duodenum, optimal vascular opacification and slice collimation, and compulsive observation are required to make an early diagnosis of this disease. The exophytic lesions are also important to focus on. Make sure in the evaluation that you evaluate beyond the immediate borders of the pancreas. There are tumors that have fooled the most experienced of observers because they were exophytic and removed from the usual domain of the pancreas.
Position
In this section we consider the position of the pancreas in the abdominal cavity. The head, body, and some of the tail are located within the retroperitoneum, while the distal tip of the tail is enveloped in the splenorenal ligament and thus considered intraperitoneal. There are few structures that share the duality of being both an intraperitoneal and retroperitoneal structure. What makes any structure an intraperitoneal structure? – When more than 2/3rds of the organ is covered by peritoneum it is considered peritoneal.
The pancreas has been described as the hermit or hidden organ of the abdomen. It is surrounded on all four sides by parts of the gastrointestinal tract and has the stomach and lesser sac covering its anterior surface with the liver forming a second anterior and lateral layer. The spine, aorta, IVC, splenic vein, and left renal vein lie directly posterior, while the kidneys lie posterior and lateral to it.
On its right side is the antrum-descending duodenum and right lobe of the liver with the right colon, and on its left is duodenum, proximal small bowel, colon, and spleen. Superiorly the splenic artery and body of stomach protect the gland. Inferiorly lays the transverse duodenum.
The pancreas cannot be palpated clinically and even when the abdomen is opened, the surgeon has difficulty in seeing or even fully palpating the pancreas.
As the central organ in the upper abdomen it crosses the abdomen from the right side of the retroperitoneum where the head lies to the right of the spine at about L2 level and to the left for about 10 cms in an upward course to the hilum of the spleen at the L1. It thus is mostly leftward in its position, and covers the area known as the transpyloric plane (L1-L2).
The retroperitoneum is divided into three major compartments – the anterior pararenal space, the perirenal space and the posterior pararenal space. The pancreas lies in the anterior pararenal space, and shares this space with the transverse duodenum and great vessels.
In the coronal plane the tail lies superior to the head, while in the axial plane the tail lies posterior to the head. Thus it is rare to visualize the entire pancreas on a single axial or transverse image.
Quiz Me
The pancreas can be palpated by a clinician by feeling the central area of the abdomen under the stomach.
True False
Accessory Pancreas
Accessory pancreatic tissue is an uncommon congenital anomaly where a focus of pancreatic tissue ranging in size from a few mms to 5 cm is displaced and remote from the normal pancreas. It is most commonly found in the submucosa or the subserosal layers of the stomach, duodenum, and jejunum, but may also be found more rarely in the gallbladder, spleen, small bowel mesentery, Meckel?s diverticulum, or ileum. Ductal tissue may be present and the ectopic tissue may also contain islets of Langerhans. They are mostly asymptomatic, but may undergo any of the diseases that affect the normal pancreas including the development of pancreatitis, pancreatic carcinoma, or even islet cell tumors.
Parts of the Pancreas
We will now discuss the small parts of the organ, as seen and evaluated by histology. Next, we discuss the capsule and supportive elements of the gland.
Courtesy of: Ashley Davidoff, M.D. 38025b13
Small Parts of the Pancreas: Histology
At the histological level the pancreas is made up of compound glands in “bunch of grapes” fashion.
Conceptually the organization of functional units around a ductal system is the same as the lung but the “alveoli” are filled with solid cellular tissue rather than air. Interspersed among the clusters of exocrine glands are the sparse accumulations of Langerhans glands. Between the glands is an interstitial fluid that is gel like in the young and with advancing age is replaced by fat that creeps in from the retroperitoneum. The little protection afforded by the flimsy pancreatic “capsule” makes this infiltration easy. Similarly when disease occurs in the pancreas there is little to hold the disease within the confines of the pancreas so that exudate or malignancy extends outward early in the natural history of the disease process. This has very important clinical implications.
There are 20-35 secondary ducts that arise in herringbone fashion, almost at right angles off the main duct. The acini accumulate around the ductules and their branches to form lobules.
Eighty per cent of the parenchyma consists of lobules of pancreatic acini that are responsible for the exocrine secretions. Approximately 18% of the gland is derived from ductal system and interstitium, while the islets of Langerhans makeup only 2% of the gland. Richly innervated peripancreatic areolar tissue penetrates the parenchyma as thin septa, dividing it up into lobules, is drained by a small branch of the pancreatic duct; dips in between lobules.


Acini and Islets
Acini
The acini are rounded or have a short tubular form and consist of single rows of epithelial cells lying on a basal lamina. Lining the lumen of the acinus are pyramidal acinar cells. There are in addition unique cells called the centroacinar cells. The lumen of the acinus connects with the intralobular ducts to form the interlobular ducts. These ducts join to form the main pancreatic duct. Lining the ductules are columnar cells, goblet cells, and occasional argentaffin cells. The larger ducts are surrounded by a prominent layer of connective tissue. Thick layers of connective tissue and elastic fibers surround the large ducts.
Islets of Langerhans
The endocrine portion of the pancreas consists of about one million islets of Langerhans, which are distributed throughout the gland but are relatively concentrated in the tail of the pancreas. The islets are surrounded a rich capillary plexus.
About 75% – 80% of islet cells are insulin secreting beta cells, and they lie centrally in the islet. 10% -20% of the islet are alpha cells which lie in the periphery and secrete glucagon. Delta cells are interspersed throughout the islet, compose about 5% and secrete somatostatin.
The Capsule
The pancreas is characterized by its lack of a discrete fibrous capsule. It is surrounded by a sheath of areolar tissue or a thin connective-tissue capsule, which sends a fine process and septa between its lobules, and these septa carry into it the blood vessels and nerves. The posterior peritoneum also acts as a barrier between the pancreas and the peritoneal cavity.

c= transverse colon
s = stomach
gcl = gastrocolic ligament
go = greater omentum
tm = transverse mesocolon.
This is a very important diagram, which is used repeatedly to define the omental and ligamentous relationships between the pancreas, colon, and stomach. The posterior peritoneum (yellow around the pancreas) lies partially surrounding the anterior portion of the pancreas and gives rise to the transverse mesocolon, which forms a double layered ligamentous attachment to the transverse colon. Disease of the pancreas can thus reach the colon by this route.
Courtesy of: Ashley Davidoff, M.D. 01443b05
The transverse mesocolon attaches to the anterior surface of the head and the inferior aspect of the body and tail. The posterior surface of the gland is devoid of peritoneum except for the tail. Thus, the head and body are retroperitoneal, and the tail is intraperitoneal, since it is covered within the splenorenal ligament. It is connected to the splenic flexure by the splenorenal and phrenicocolic ligaments.
Quiz Me
Disease of the pancreas can spread directly to the colon.
True False
Application to Imaging
In acute pancreatitis, although the pancreas can be severely involved, most of the accompanying edema exudes beyond the flimsy pancreatic capsule and the peripancreatic changes are often more impressive than the changes in the pancreas itself.

Courtesy of: Ashley Davidoff, M.D. 15730
Pancreatic Duct
There is a main pancreatic duct and an accessory pancreatic duct. The main pancreatic duct (MPD) assumes almost all the responsibility of draining the pancreas including the tail, body and the ventral portion of the head. The accessory duct has variable connection to the MPD, and variable independent connection to the duodenum and usually assumes very little responsibility for drainage.
The main pancreatic duct joins with the common bile duct to form the ampulla, which opens into the duodenum. This configuration occurs in 90% of people.
The minor pancreatic duct usually enters independently into the duodenum 2cms cranial to the major papilla. An accessory pancreatic duct (persistent duct of Santorini) that drains into the minor ampulla is present in 44% of individuals. The duct of Santorini provides the major drainage route in 9% of people.

Courtesy of: Ashley Davidoff, M.D. 22391RW3
Pancreatic Duct: Duct of Wirsung – The Main Pancreatic Duct
The main pancreatic duct, also known as the Duct of Wirsung, is composed of the dorsal duct of the tail and body, which has joined the ventral components of the duct that drains the head and uncinate process. The pancreatic duct receives 20?35 short tributaries that enter at right angles. Interlobular ducts are found between lobules, within the connective tissue septae. They vary considerably in size. The smaller forms have a cuboidal epithelium, and the larger interlobular secondary ducts are lined by columnar epithelium. Intralobular ducts transmit secretions into the interlobular ducts.
Courtesy of: Ashley Davidoff, M.D. 29247
Duct of Santorini – Accessory Pancreatic Duct
The accessory duct of Santorini (APD) is a remnant of the former main pancreatic duct, which embryologically was connected to the duct of the neck, body, and tail – all originating from the dorsal anlage. During development the duct of Santorini becomes disconnected from the duct of the body and tail and remains a relatively small component of the system at large, while the duct from the ventral portion of the head connects to the duct of the body and tail.
Its persistent connection to the duodenum via the minor papilla is seen in 50-70% of patients. When it is not connected to the duodenum it serves as an accessory branch connected to the main ductal system. The accessory pancreatic duct of Santorini usually communicates with the main duct and passes transversely to the right in the upper part of the head of the pancreas. The duct of Santorini lies anterior to the intrapancreatic common bile duct and usually opens into the proximal portion of the second part of the duodenum at the minor papilla, proximal to the main papilla.
In summary, the accessory duct may be blind, keep some connection with the main duct, retain a full embryologic connection with the duct of the body (pancreas divisum) or drain independently into the duodenum.

Courtesy of: Ashley Davidoff, M.D. 04184

Courtesy of: Ashley Davidoff, M.D. 9963c01
Quiz Me
The accessory pancreatic duct of Wirsung usually communicates with the main duct and passes transversely to the right in the upper part of the head of the pancreas.
True False
Shape of the Ducts
In general the main pancreatic duct (MPD) is “S” shaped and may have some normal narrowing in the expected location where the dorsal and ventral components of the ducts fuse. The pre-ampullary region may become fusiform in shape and mildly dilated. There is sometimes a normal loop to the duct in the head of the pancreas.
When the main duct is joined by the parts of the duct in the head and uncinate process, it becomes Y-shaped. Within the head, the main pancreatic duct turns inferiorly and comes into close relationship with the bile duct. Usually, these two ducts become surrounded by the sphincter of Oddi in the ampulla of Vater. They may remain as two separate channels (42%), form a common channel within the pailla (38%), form a common channel about halfway into the ampulla (14%) or become confluent for the whole ampulla (3%).
The sphincter around the hepatopancreatic ampulla is called the hepatopancreatic sphincter (of Oddi), which controls both the flow of pancreatic juice and bile.
The duct in the region of the tail usually has a bifid pattern and it may fan out into three or more branches.

Courtesy of: Ashley Davidoff, M.D. 39962

Courtesy of: Ashley Davidoff, M.D. 39962b04
The shape and course of the pancreatic duct varies greatly among individuals. The main pancreatic duct usually ascends from the neck to the tail in about 50% of cases, is horizontal in about 35%, sigmoid in about 10%, and descends in about 5%.

Courtesy of: Ashley Davidoff, M.D. 41389

Courtesy of: Ashley Davidoff, M.D.

Courtesy of: Ashley Davidoff, M.D. 41409c02
Size and Normal Narrowings
The length of the MPD varies between 10 and 20 cms, which is quite a wide variation in size. The length of the duct has no functional nor anatomic significance.
The generally accepted size of the pancreatic duct using ultrasound is less than 2mm, and up to 3mms in the head. The size does increase with age and the duct dilates in patients with gallstones. In acute pancreatitis the duct also enlarges up to 3mm and regresses in size as the patient improves. However it may not return to normal following the episode.
There are normal narrowings to the duct. The first and most obvious is at the ampulla where the duct narrows as the sphincter of the pancreatic duct just before it joins the bile duct. The second is not as common but is important to recognize as a variant. It occurs at the junction of the dorsal and ventral ducts in the head of the pancreas. When the narrowing is a normal variant there will be no upstream dilatation and the post drainage study will show clearing of the contrast from the system.
Courtesy of: Ashley Davidoff, M.D.
41394size002b04L
Secondary Side Branches
There are a few generally accepted normal morphologic features of the secondary branches. They are too small to measure but the downstream portions are larger than the upstream branches. In general the side branches in the body and tail arise at approximately 90o to the axis of the MPD and have fairly uniform spacing between each branch.

Courtesy of: Ashley Davidoff, M.D. 05008
Application to Imaging
It is extremely important to know and recognize the normal size, shape, position and character of a structure. When there is morphological change due to disease these are the aspects that will change.
The changes in chronic pancreatitis include contour irregularities, and dilatation of the main pancreatic duct as well as dilatation of the side branches. The side branches are not normally seen on MRCP and if they are visualized by implication they are dilated. In severe cases, there is marked dilatation of the side branches resulting in the “chain of lakes” appearance. Other findings in chronic pancreatitis include stricture formation and intraductal calculi.

Courtesy of: Ashley Davidoff, M.D. 40046c
Blood Supply
The pancreas has a very rich blood supply from both the celiac axis and the superior mesenteric artery (SMA). Typically (in 90% of people), the celiac axis divides into the common hepatic, splenic, and left gastric arteries. The common hepatic artery gives rise to the gastroduodenal artery (GDA), and then turns upward to the porta hepatis. The GDA courses from its origin behind the first part of the duodenum and, after giving off the superior pancreaticoduodenal artery, lies on the anterior surface of the head of the pancreas. At the lower border of the first part of the duodenum, it branches into the right gastroepiploic artery and the superior pancreaticoduodenal artery.
The superior pancreaticoduodenal artery gives off two major branches – the anterior pancreaticoduodenal and the posterior pancreaticoduodenal artery. These two latter vessels form an arcade around the head of the pancreas and reform inferiorly as the inferior pancreaticoduodenal artery. The inferior pancreaticoduodenal artery is a branch of the SMA.
For the most part, the head of the pancreas and the duodenum have a common blood supply called the anterior and posterior pancreaticoduodenal arcades.
The body and tail also have dual blood supplies receiving blood from both the splenic artery and from the SMA.
Celiac Axis

Courtesy of: Ashley Davidoff, M.D. 39762

Courtesy of: Ashley Davidoff, M.D.
Celiac Axis Continued
The celiac axis supplies the pancreas from both the common hepatic artery as well as the splenic artery. The splenic artery supplies 3 major branches to the body and tail. These include the dorsal pancreatic artery, (DPA) pancreatica magna (PM), and caudal pancreatic artery. (CPA)

Courtesy of: Ashley Davidoff, M.D. 39842b

Courtesy of: Ashley Davidoff, M.D.

Courtesy of: Ashley Davidoff, M.D.
Superior Mesenteric Artery (SMA)
The superior mesenteric artery (SMA) contributes to the blood supply of the head of the pancreas as well as the tail. The head receives a branch from the SMA called the inferior pancreaticoduodenal artery which divides into anterior and posterior branches, each of which connects to the anterior and posterior branches of the superior pancreatic branch from the GDA. The head of the pancreas is thus well supplied with blood in the form of a pancreaticoduodenal arcade.
Quiz Me
The tail has a dual blood supply receiving blood from both the SMA and _________.
(Note: You will be given 2 tries to answer this question, then the answer will be provided.)
gastroduodenal artery
pancreaticoduodenal
splenic artery
celiac axis
The Pancreaticoduodenal Arcade
This arcade has both an anterior component and a posterior component. The anterior component is formed by the anastomosis of the anterior branch of the superior pancreaticoduodenal artery, which is a branch of the gastroduodenal artery, and the anterior inferior pancreaticoduodenal artery, which is usually a branch of the superior mesenteric artery.
The posterior pancreaticoduodenal arcade is formed by the anastomosis of the posterior branch of the superior pancreaticoduodenal artery, usually a branch of the gastroduodenal artery, and the posterior branch of the inferior pancreaticoduodenal artery, which usually arises from the SMA. The posterior branch of the superior pancreaticoduodenal artery courses to the right and anterior to the common bile duct, and provides blood supply to the extra hepatic duct. During sphincterotomy this vessel can be severed and be a major source of bleeding.
The duodenum and head of the pancreas share their blood supply and the duodenum can be compromised by total pancreatectomy. Additionally if a patient requires embolization for a pseudoaneurysm in the pancreatic head (a rare complication of pancreatitis), embolization must be approached from both the celiac axis and the SMA because of the dual and connecting blood supply.

In this injection of the SMA the pancreaticoduodenal arcade is well demonstrated. The inferior pancreaticoduodenal artery arises from the SMA and gives off branches to the duodenum and the pancreas.
Courtesy of: Ashley Davidoff, M.D.
Venous Drainage
The final common pathway of pancreatic venous drainage is via the portal vein, which receives venous blood from the superior mesenteric vein and the splenic vein. Venous drainage of the body and the tail of pancreas drain into the splenic vein and then into the portal vein which takes the blood to the liver. The head of the pancreas drains into tributaries of the gastroepiploic vein, gastric vein, superior mesenteric vein, and portal vein.

In this CT the small venules draining the pancreas can be seen throughout the body and tail of pancreas in this early arterial-venous phase. Arches of venules connect with a larger vein that runs the length of the body of the pancreas.
Courtesy of: Ashley Davidoff, M.D. 25235_1
Lymphatic Drainage
The lymphatic channels originate around the acini and initially following the capillaries and subsequently following the arterioles and arteries. No lymphatics are found around the islets of Langerhans. The lymphatics of the pancreas follow the branches of the celiac axis and the SMA that supply the pancreas, with the nodal supply of the head following the hepatic artery and the supply of the body and tail following the splenic artery. The final regional pathway for the celiac nodes and the SMA nodes will be to the para aortic nodes.
The nodes of the hepatic vessels completely surround the head, and are found anterior, posterior, superior, and inferior to the head. The head of the pancreas shares these nodes with the duodenum with which it is intimate contact.
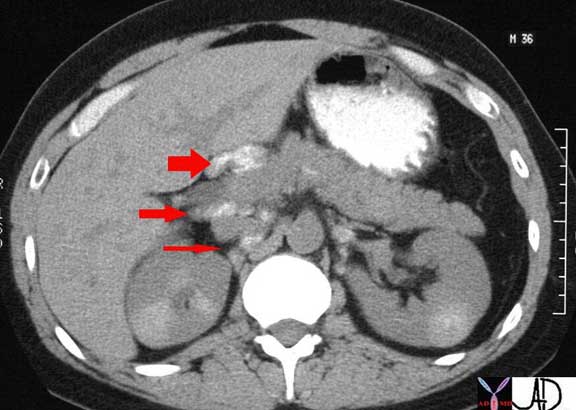
The CT through the mid abdomen and kidneys is from a patient with sarcoidosis in whom there is extensive but fine calcifications in the kidneys and the celiac axis lymph nodes surrounding the pancreas. These are abnormal lymph nodes but the case serves to demonstrate the lymphatic associations of the head of the pancreas. There are nodes anterior to the head in the porta hepatis (fat arrow), and in the portocaval space posterior to the head. (middle arrow) More posteriorly (thin arrow) small calcified nodes are seen between the IVC and the right crus of the diaphragm.
Calcifications in the lymph nodes and kidneys are related to sarcoidosis.
Courtesy of: Ashley Davidoff, M.D.

In this CT of the same 36 year old patient with sarcoidosis a small calcified intrapancreatic node is seen at the junction of the neck and body of the pancreas. There are also nodes anterior and posterior to the head in the porta hepatis and more posteriorly small calcified nodes are seen between the IVC, the right crus of the diaphragm and the right kidney.
Courtesy of: Ashley Davidoff, M.D.
Nerve Supply
The nerves are derived form the vagus and the splanchnic nerves. The sympathetic and parasympathetic fibers reach the gland by passing along the arteries of the celiac and superior mesenteric plexuses.
Aging of the Pancreas
In the young there is a tendency for the tail to be relatively large and the head to be relatively small. With age the reverse is true with the head appearing relatively large and the tail relatively small.

Right Image: This CT scan through the pancreas in an older patient shows an atrophied body with a prominent head.
Images courtesy of: Ashley Davidoff, M.D. 41394size02
Conclusion
The pancreas as you have now learned is neither ?all meat? nor a hermit. However, it is an organ of duality with some unique structural features. As a gland it has both endocrine components as well as exocrine components. While the insulin secreting components only make up 2% of the gland, failure of their function leads to the devastating consequences and complications of diabetes mellitus. The pancreas has a dual blood supply and an extensive collateral arterial network ensuring that blood supply is always available, giving it the opportunity to keep its ?finger on the pulse? of glucose metabolism.
Diseases such as pancreatitis and carcinoma are not uncommon and the absence of a capsule results in early spread to surrounding organs with devastating results. Modern imaging has facilitated accurate evaluation of structural changes and so diagnosis and complications of disease can be accomplished with greater accuracy. The degree of spread of disease has significant impact on management and so better imaging has brought improved management.
At this stage one can only wonder where imaging will take us next. We are in the mode now of combining functional imaging with structural imaging. We may not have a full sense of where the future of imaging will go but we do know that the imaging will always be based on structure, function, and pathology. It cannot be therefore overstated that it behooves us all to continue to acquire and retain a solid knowledge of anatomy, physiology and pathology.
