|
The Common Vein Copyright 2008
Ashley Davidoff MD
Introduction
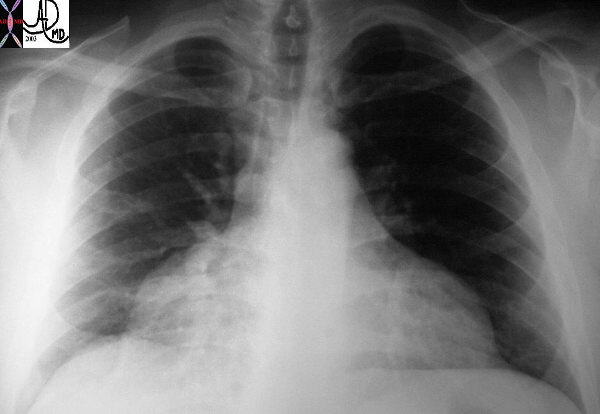
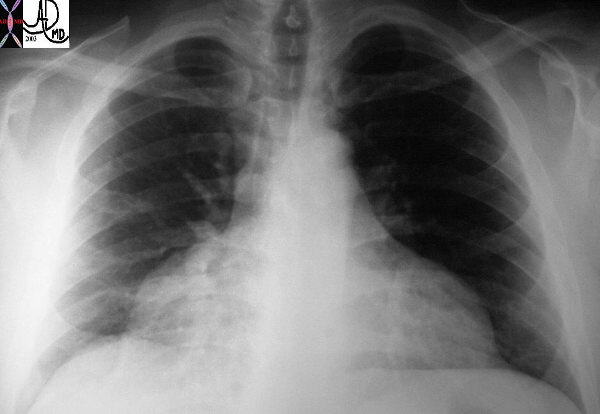
Unusual shape of the cardiac shadow characterised by a narrow nediastinum and a broad base caused by accumulation of fluid in the pericardial space
30095

Pericardial effusion
 
43704 43702
CAUSES
Infectious – viral, tuberculosis, HIV related Idiopathic
Virus – echovirus, influenza virus, and coxsackievirus group B.
Bacteria streptococci, staphylococci, and gram-negative bacilli. Haemophilus influenzae is a common cause in children
Inflammation
rheumatoid arthritis,
SLE
systemic sclerosis,
vasculitides
radiation
Neoplastic –
Malignant (20% of patients with malignancy have nmetastases to pericardium),
nonmalignant.
Not all cancer-associated effusions are malignant. Mediastinal lymphoma, Hodgkin disease, and metastatic breast cancer have been found to cause transient effusions, likely due to impaired lymphatic drainage, which do not cause long-term sequelae.
Metabolic
Myxedema
Uremia
Drugs
-
- Warfarin, heparin
- Penicillin
- Phenytoin
- Procainamide
- Hydralazine, minoxidil
- Cromolyn sodium
- Methysergide
- Doxorubicin
Mechanical
Postpericardiotomy syndrome
Trauma
penetrating or blunt
Circulatory –
Congestive heart failure, valvular disease
Idiopathic
PEARLS
Normal amount of fluid – 10-50ccs
The rapid accumulationamount of only 80ccs can lead to tamponade wheras a volume of up to 2 litres if slowly accumulated can be tolerated.
Malignant effusions
Up to 20 percent of autopsy series – lung breast and leukemias lymphomas
Infections HIV -40-80 PERCENT with or without AIDS –
Mycobacterium avium, M. tuberculosis, Nocardia, fungal infection, viral disease, lymphoma, or Kaposi’s sarcoma.
MI and pericardial effusions
early consequence of acute MI (10 to 15% of cases).
late post-MI syndrome (Dressler’s syndrome) 10 days to 2 mo post-MI (1 to 3%) -fever, pericarditis friction rub, pericardial effusion, pleurisy, pleural effusions, and joint pain.
rupture post-MI, causing hemopericardium. This usually occurs 1 to 10 days post-MI and is more common in women.
TB may not have pulmonary involvement |
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => table
[nodeValue] =>
The Common Vein Copyright 2008
Ashley Davidoff MD
Introduction
Unusual shape of the cardiac shadow characterised by a narrow nediastinum and a broad base caused by accumulation of fluid in the pericardial space
30095
Pericardial effusion
43704 43702
CAUSES
Infectious – viral, tuberculosis, HIV related Idiopathic
Virus – echovirus, influenza virus, and coxsackievirus group B.
Bacteria streptococci, staphylococci, and gram-negative bacilli. Haemophilus influenzae is a common cause in children
Inflammation
rheumatoid arthritis,
SLE
systemic sclerosis,
vasculitides
radiation
Neoplastic –
Malignant (20% of patients with malignancy have nmetastases to pericardium),
nonmalignant.
Not all cancer-associated effusions are malignant. Mediastinal lymphoma, Hodgkin disease, and metastatic breast cancer have been found to cause transient effusions, likely due to impaired lymphatic drainage, which do not cause long-term sequelae.
Metabolic
Myxedema
Uremia
Drugs
Warfarin, heparin
Penicillin
Phenytoin
Procainamide
Hydralazine, minoxidil
Cromolyn sodium
Methysergide
Doxorubicin
Mechanical
Postpericardiotomy syndrome
Trauma
penetrating or blunt
Circulatory –
Congestive heart failure, valvular disease
Chylopericardium
Idiopathic
PEARLS
Normal amount of fluid – 10-50ccs
The rapid accumulationamount of only 80ccs can lead to tamponade wheras a volume of up to 2 litres if slowly accumulated can be tolerated.
Malignant effusions
Up to 20 percent of autopsy series – lung breast and leukemias lymphomas
Infections HIV -40-80 PERCENT with or without AIDS –
Mycobacterium avium, M. tuberculosis, Nocardia, fungal infection, viral disease, lymphoma, or Kaposi’s sarcoma.
MI and pericardial effusions
early consequence of acute MI (10 to 15% of cases).
late post-MI syndrome (Dressler’s syndrome) 10 days to 2 mo post-MI (1 to 3%) -fever, pericarditis friction rub, pericardial effusion, pleurisy, pleural effusions, and joint pain.
rupture post-MI, causing hemopericardium. This usually occurs 1 to 10 days post-MI and is more common in women.
TB may not have pulmonary involvement
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] =>
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
The Common Vein Copyright 2008
Ashley Davidoff MD
Introduction
Unusual shape of the cardiac shadow characterised by a narrow nediastinum and a broad base caused by accumulation of fluid in the pericardial space
30095
Pericardial effusion
43704 43702
CAUSES
Infectious – viral, tuberculosis, HIV related Idiopathic
Virus – echovirus, influenza virus, and coxsackievirus group B.
Bacteria streptococci, staphylococci, and gram-negative bacilli. Haemophilus influenzae is a common cause in children
Inflammation
rheumatoid arthritis,
SLE
systemic sclerosis,
vasculitides
radiation
Neoplastic –
Malignant (20% of patients with malignancy have nmetastases to pericardium),
nonmalignant.
Not all cancer-associated effusions are malignant. Mediastinal lymphoma, Hodgkin disease, and metastatic breast cancer have been found to cause transient effusions, likely due to impaired lymphatic drainage, which do not cause long-term sequelae.
Metabolic
Myxedema
Uremia
Drugs
Warfarin, heparin
Penicillin
Phenytoin
Procainamide
Hydralazine, minoxidil
Cromolyn sodium
Methysergide
Doxorubicin
Mechanical
Postpericardiotomy syndrome
Trauma
penetrating or blunt
Circulatory –
Congestive heart failure, valvular disease
Chylopericardium
Idiopathic
PEARLS
Normal amount of fluid – 10-50ccs
The rapid accumulationamount of only 80ccs can lead to tamponade wheras a volume of up to 2 litres if slowly accumulated can be tolerated.
Malignant effusions
Up to 20 percent of autopsy series – lung breast and leukemias lymphomas
Infections HIV -40-80 PERCENT with or without AIDS –
Mycobacterium avium, M. tuberculosis, Nocardia, fungal infection, viral disease, lymphoma, or Kaposi’s sarcoma.
MI and pericardial effusions
early consequence of acute MI (10 to 15% of cases).
late post-MI syndrome (Dressler’s syndrome) 10 days to 2 mo post-MI (1 to 3%) -fever, pericarditis friction rub, pericardial effusion, pleurisy, pleural effusions, and joint pain.
rupture post-MI, causing hemopericardium. This usually occurs 1 to 10 days post-MI and is more common in women.
TB may not have pulmonary involvement
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 40
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The Common Vein Copyright 2008
Ashley Davidoff MD
Introduction
Unusual shape of the cardiac shadow characterised by a narrow nediastinum and a broad base caused by accumulation of fluid in the pericardial space
30095
Pericardial effusion
43704 43702
CAUSES
Infectious – viral, tuberculosis, HIV related Idiopathic
Virus – echovirus, influenza virus, and coxsackievirus group B.
Bacteria streptococci, staphylococci, and gram-negative bacilli. Haemophilus influenzae is a common cause in children
Inflammation
rheumatoid arthritis,
SLE
systemic sclerosis,
vasculitides
radiation
Neoplastic –
Malignant (20% of patients with malignancy have nmetastases to pericardium),
nonmalignant.
Not all cancer-associated effusions are malignant. Mediastinal lymphoma, Hodgkin disease, and metastatic breast cancer have been found to cause transient effusions, likely due to impaired lymphatic drainage, which do not cause long-term sequelae.
Metabolic
Myxedema
Uremia
Drugs
Warfarin, heparin
Penicillin
Phenytoin
Procainamide
Hydralazine, minoxidil
Cromolyn sodium
Methysergide
Doxorubicin
Mechanical
Postpericardiotomy syndrome
Trauma
penetrating or blunt
Circulatory –
Congestive heart failure, valvular disease
Chylopericardium
Idiopathic
PEARLS
Normal amount of fluid – 10-50ccs
The rapid accumulationamount of only 80ccs can lead to tamponade wheras a volume of up to 2 litres if slowly accumulated can be tolerated.
Malignant effusions
Up to 20 percent of autopsy series – lung breast and leukemias lymphomas
Infections HIV -40-80 PERCENT with or without AIDS –
Mycobacterium avium, M. tuberculosis, Nocardia, fungal infection, viral disease, lymphoma, or Kaposi’s sarcoma.
MI and pericardial effusions
early consequence of acute MI (10 to 15% of cases).
late post-MI syndrome (Dressler’s syndrome) 10 days to 2 mo post-MI (1 to 3%) -fever, pericarditis friction rub, pericardial effusion, pleurisy, pleural effusions, and joint pain.
rupture post-MI, causing hemopericardium. This usually occurs 1 to 10 days post-MI and is more common in women.
TB may not have pulmonary involvement
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The Common Vein Copyright 2008
Ashley Davidoff MD
Introduction
Unusual shape of the cardiac shadow characterised by a narrow nediastinum and a broad base caused by accumulation of fluid in the pericardial space
30095
Pericardial effusion
43704 43702
CAUSES
Infectious – viral, tuberculosis, HIV related Idiopathic
Virus – echovirus, influenza virus, and coxsackievirus group B.
Bacteria streptococci, staphylococci, and gram-negative bacilli. Haemophilus influenzae is a common cause in children
Inflammation
rheumatoid arthritis,
SLE
systemic sclerosis,
vasculitides
radiation
Neoplastic –
Malignant (20% of patients with malignancy have nmetastases to pericardium),
nonmalignant.
Not all cancer-associated effusions are malignant. Mediastinal lymphoma, Hodgkin disease, and metastatic breast cancer have been found to cause transient effusions, likely due to impaired lymphatic drainage, which do not cause long-term sequelae.
Metabolic
Myxedema
Uremia
Drugs
Warfarin, heparin
Penicillin
Phenytoin
Procainamide
Hydralazine, minoxidil
Cromolyn sodium
Methysergide
Doxorubicin
Mechanical
Postpericardiotomy syndrome
Trauma
penetrating or blunt
Circulatory –
Congestive heart failure, valvular disease
Chylopericardium
Idiopathic
PEARLS
Normal amount of fluid – 10-50ccs
The rapid accumulationamount of only 80ccs can lead to tamponade wheras a volume of up to 2 litres if slowly accumulated can be tolerated.
Malignant effusions
Up to 20 percent of autopsy series – lung breast and leukemias lymphomas
Infections HIV -40-80 PERCENT with or without AIDS –
Mycobacterium avium, M. tuberculosis, Nocardia, fungal infection, viral disease, lymphoma, or Kaposi’s sarcoma.
MI and pericardial effusions
early consequence of acute MI (10 to 15% of cases).
late post-MI syndrome (Dressler’s syndrome) 10 days to 2 mo post-MI (1 to 3%) -fever, pericarditis friction rub, pericardial effusion, pleurisy, pleural effusions, and joint pain.
rupture post-MI, causing hemopericardium. This usually occurs 1 to 10 days post-MI and is more common in women.
TB may not have pulmonary involvement
)