- 75M
- PMH HTN, HLD, previous tobacco use COPD (previous exacerbations have required intubations), and chronic bronchiectasis, COVID-19 infection
- witnessed collapse with complaints of SOB,
- became unresponsive o
- found to be in VF arrest 2/2 inferior STEMI.
- 7 rounds epi, shocks; also given amio and lidocaine. Post-arrest ECG w/ STE in inferior leads, RBBB, and LAFB.
- cath lab,
- complete occlusion of the RCA, and stents were placed to proximal RCA.
- Right Dominant
Left Main: Normal
Left Anterior Descending: Appeared to be flush occluded at takeoff, no visible stump, not filling via collaterals.
Left Circ: Mild Luminal Irregularities less than 30%
RCA: Large ectatic vessel, difficult to enagage secondary to anterior and inferior take off. Extremely tortuous mid vessel. 70% proximal lesion. Totally occluded mid vessel.PROCEDURAL COMMENTS:
Pt had incessant VF in the ER requiring multiple shocks. EKG showed inferior ST elevations with IVCD. - TTE showed EF 60% with
- mild inferolateral wall hypokinesis and
- moderate inferior wall hypokinesis;
- RV systolic dysfunction was mildly reduced. T
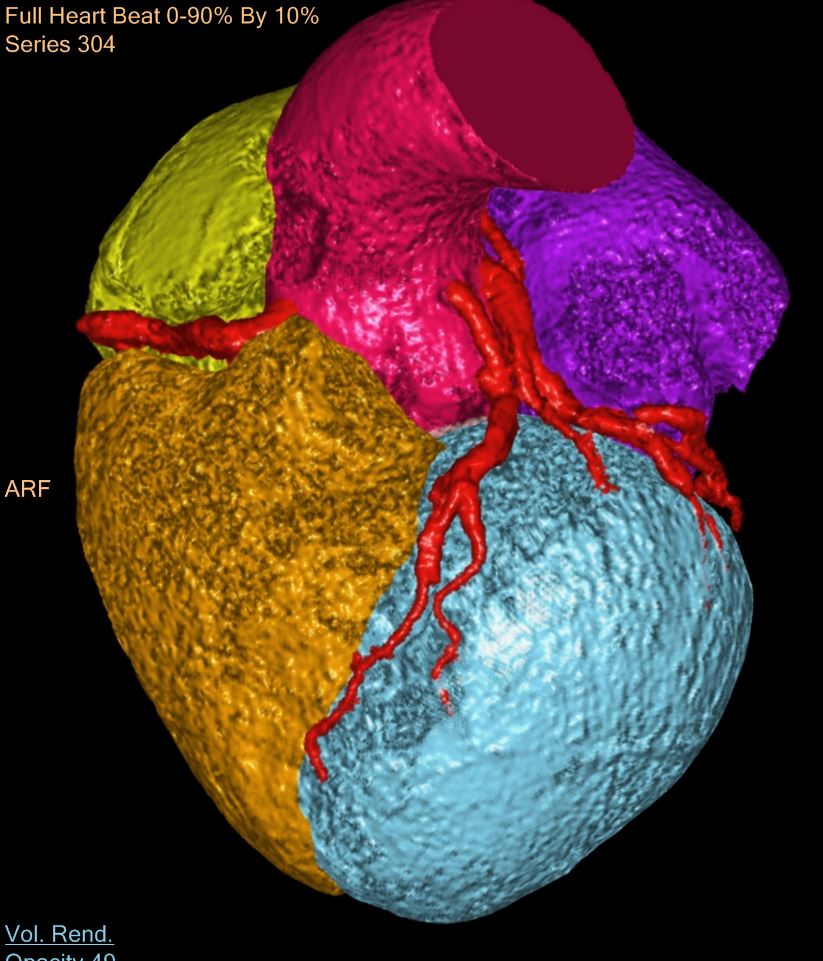
Ashley DAvidoff
TheCommonVein.net
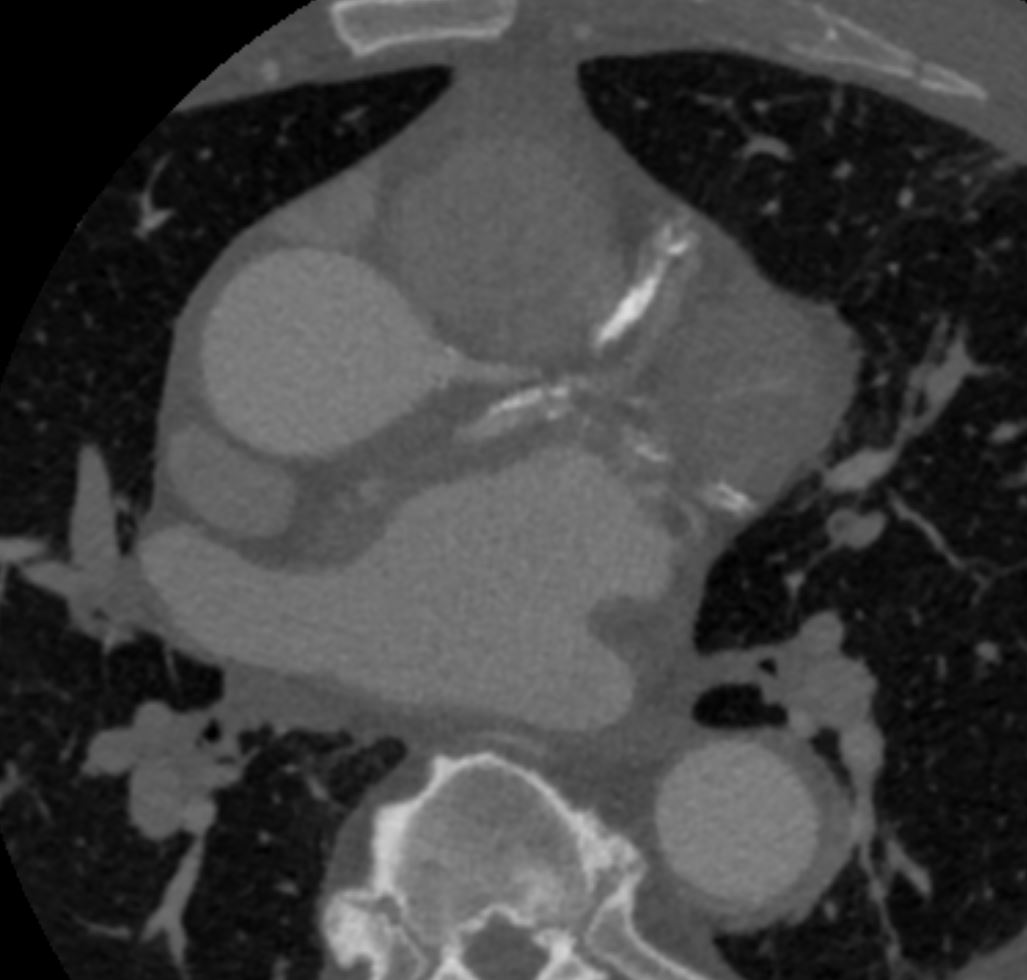
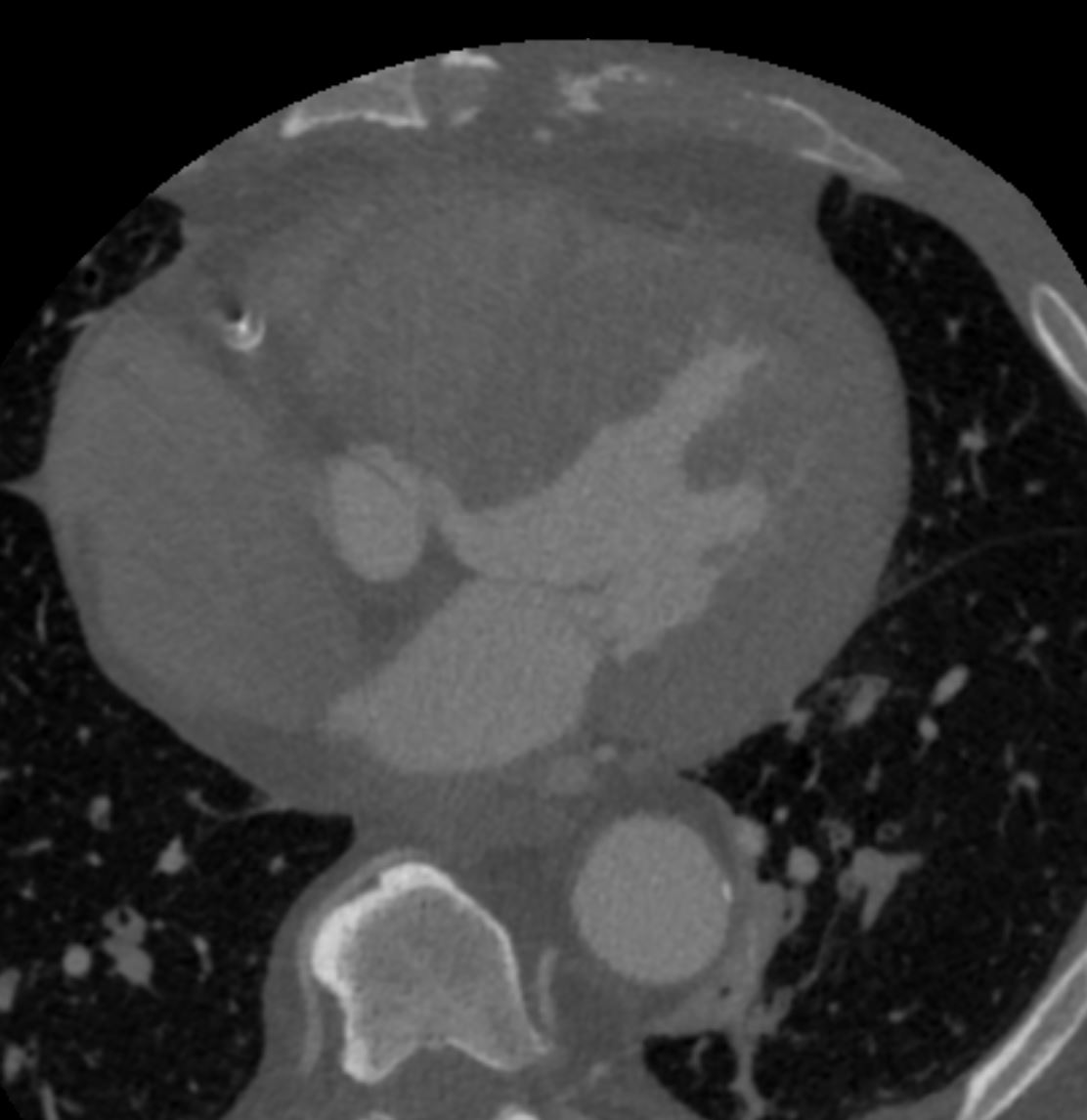
CTA coronaries
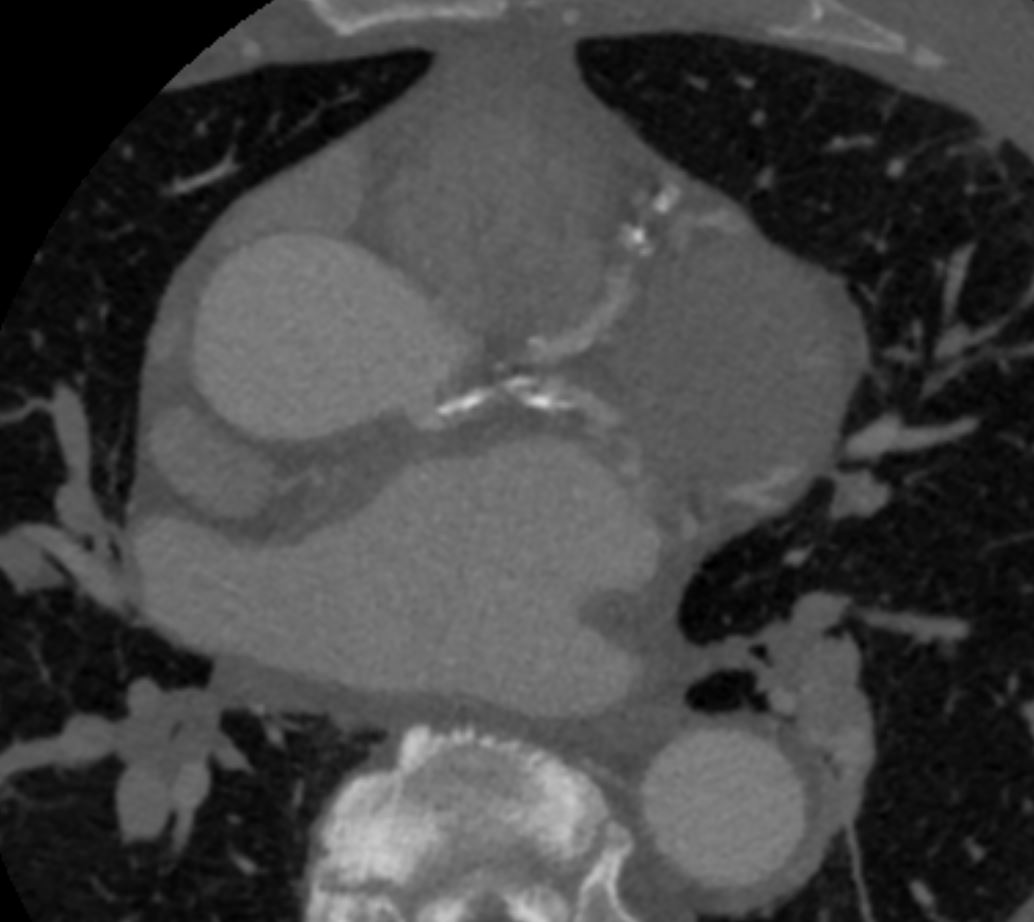
Ashley DAvidoff
TheCommonVein.net
CTA coronaries
Ashley DAvidoff
TheCommonVein.net
CTA coronaries
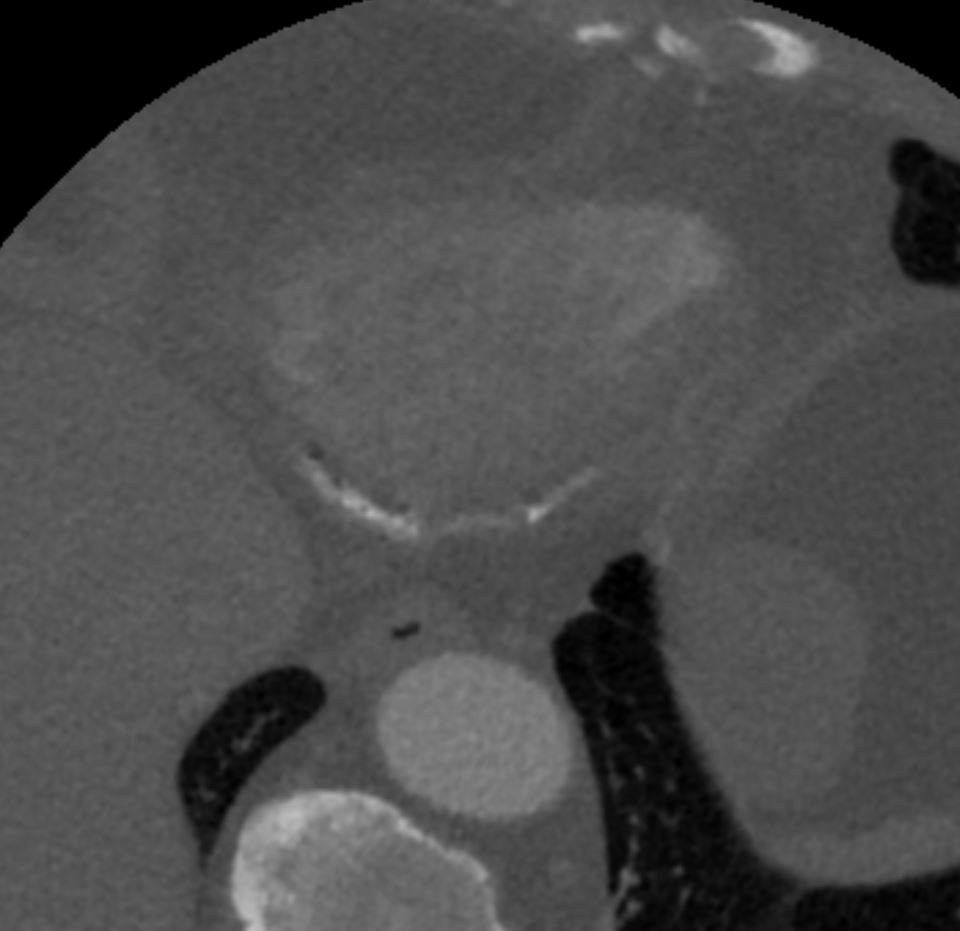
Ashley DAvidoff
TheCommonVein.net
CTA coronaries
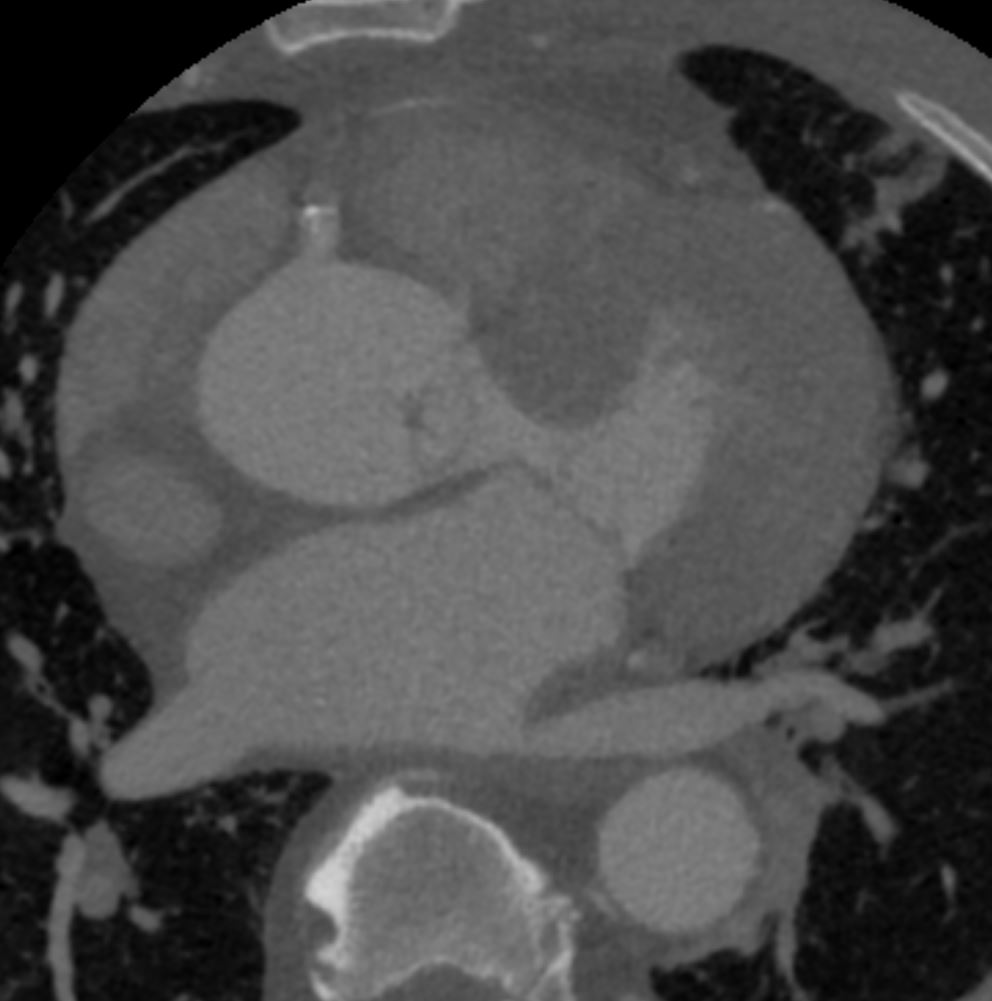
Ashley DAvidoff
TheCommonVein.net
CTA coronaries
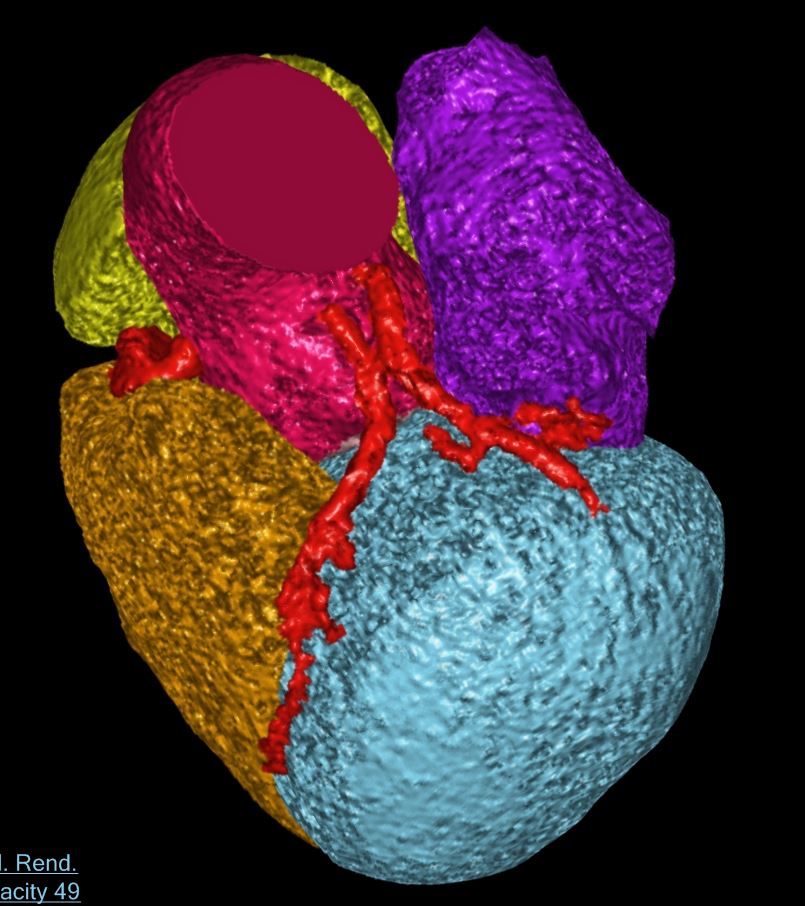
Ashley DAvidoff
TheCommonVein.net
CTA coronaries
His LAD appeared to be ostially occluded on angiography; however, the anterior wall appeared to move well on echo. He underwent coronary CT angiogram to further evaluate, revealing “extensive calcified plaque in the LAD, RCA and left circumflex coronary arteries. I
-
-
- study extremely limited for evaluation of stenosis/luminal narrowing…
- LAD arises directly from the aortic root just above the sinus of Valsalva and has a sharp acute course at the origin between the aorta and main pulmonary artery.”
- Lcx arises separately from the left coronary cusp
- EF 50%
- study extremely limited for evaluation of stenosis/luminal narrowing…
-
DB136