Atherosclerosis
The Common Vein Copyright 2007
Definition
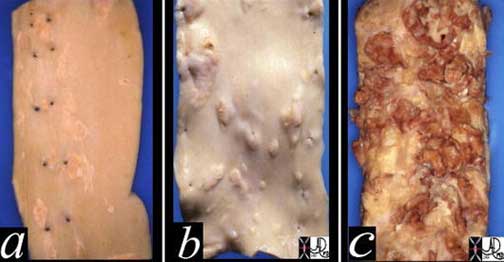
Athersclerosis is a degenerative disorder of the vascular wall characterised by a fibrofatty deposition (plaque) in the inner lining (subendothelial) of the artery.
History
Cause: It occurs as a normal course of aging, but it is accelerated by genetic, dietary and behavioral factors.
Result: The accumulation of plaque in the wall causes narrowing of the lumen of the arteries progressively restricting flow. In addition, the normal smooth and glistening lining of the arteries are replaced by a rough irregular inner wall that is a factor that predisposes to thrombosis, sometimes an acute life threatening event if the arteries of the heart or brain are affected.
Diagnosis: The clinical presentation depends on the organ involved and the degree of narrowing. In the heart for example simple narrowing results in chest pain called angina. When total acute obstruction occurs with thrombosis of the artery, severe unremitting chest pain occurs, and myocardial infarction ensues.Each organ has varied manifestations of clinical presentation, all relating to reduced perfusion of the end organ due to narrowing. Imaging plays an essential role in diagnosis. Ultrasound can directly view the lumen and wall of accessible vessels, while CT scan and MRI are advancing to be the mainstay of diagnosis for the deeper arteries. Angiography was the gold standard of the past, is still used and is invaluable in selected circumstances, particularly if therapeutic intervention is needed.
Treatment is usually directed at maintaining flow to the end organs. Medical therapy is often directed at the smooth muscle components of the vessel wall in order to dilate the vessels. Minimally invasive methods use angioplasty and stents to expand the narrowing directly, while surgery often employs bypass methods.
Courtesy: Henri Cuenoid, M.D. (coronaries-Philips-033)
Ashley Davidoff MD
32628c
#aorta #normal intima #intima

The histopathological specimen shows acute thrombosis of the coronary artery with red homogeneous thrombus (a) filling the lumen. B overlies the cholesterol plaque while c is fibrous plaque. D is the muscularis and e is the adventitia.
Courtesy of: Isabelle Joris, M.D.
Myocardial Infarction P 015
Circulating Lipo-proteins

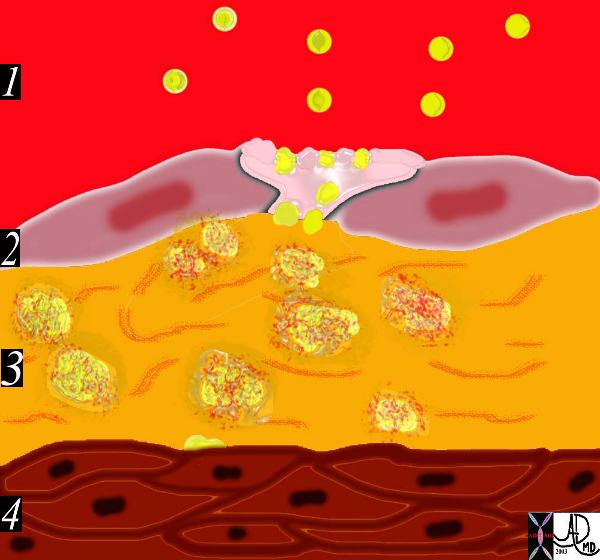
This image shows the lumen (red) single layer of the inner lining called the endothelium (pink) the muscular wall of a medium sized artery (maroon) and the yellow outer lining called the adventitia. There are lipoprotein molecules normally in the lumen. (yellow)The next step in atherogenesis is the accumulation of these lipoprotein molecules in the intima. Courtesy Ashley Davidoff MD. 33789 code heart artery wall histology normal drawing pathogenesis atherosclerosis atheroma
Atheromatous plaque is an accumulation of fatty and fibrous elements within the intima of the arterial wall. The multifactorial causes of atherosclerosis include age, sex, genetics, lifestyle and dietary factors. among many other unfolding factors. The recognizable “phases” of atherosclerosis include ;
1) Breach of the endothelium

In the early stages of atherosclerosis there is intimal injury and a breach in the endothelium. 33790 artery lumen intima endothelium internal elastic membrane media muscularis muscular layer external elastic membrane adventitia vavsa vasorum capillaries circulating phospholipids intimal injury normal anatomy histology drawing art Courtesy Ashley Davidoff MD thecommonvein.net
2) Migration of lipoproteins from the lumen into the intima.

The result is a breach in the intima and migration of lipoproteins into the subendothelial layer. The lipoproteins and proteoglycans form a complex compound that traps the fat complex in the subepithelial layer.
3) Formation of a lipoprotein-proteoglycan complex that traps the lipoprotein in the intima
Inflammatory response
4) Migration of monocytes and lymphocytes from the lumen into the intima.

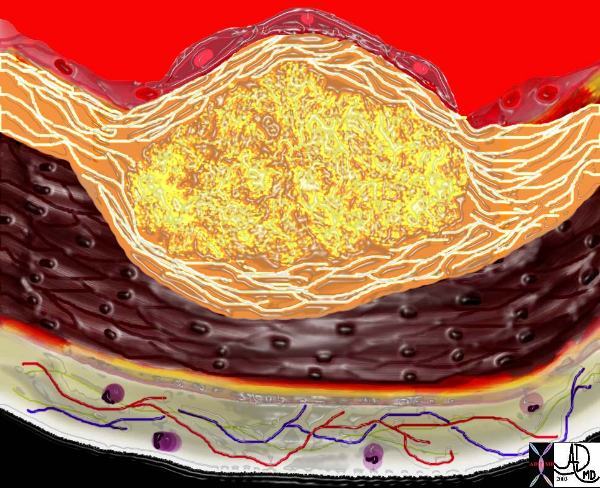
The diagram shows an evolving atheromatous plaque with inflammatory cells, monocytes, and lymphocytes infiltrating the intima which contains the lipoprotein- proteoglycan complex, extracellular lipid , and cholesterol crystals. 33792g Courtesy Ashley Davidoff MD. code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Ashley Davidoff thecommonvein.net
#Davidoff art #atherosclerosis
The next phase heralds the migration of leukocytes and platelets into the subendothelial layer.
5) Transformation of the monocytes into macrophages and phagocytosis of the fat complexes to form fat laden foamy macrophages. (33792h)

This drawing shows migration of the monocytes into the intima. These monocytes transform into macrophages in the intima and phagocytose the lipid products to become lipid laden foamy cells. The macroscopic correlate at this stage is the fatty streak. Courtesy Ashley Davidoff MD 33792h . code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff thecommonvein.net
The monocytes, phagocytose the lipoprotein-proteoglycan complex forming the lipid laden foamy histiocytes. These macrophages can apparently repllicate. At this stage the macroscopic appearance is the well known “fatty streak”.
6) Migration of smooth muscle cells from the media into the intima and transformation into fibrocytes. A fibrous capsule around the fatty complex is formed. (33792i, 33801b)

This diagram shows the reaction of the smooth muscle cells (b) to the formation of foam cells (a) in the subendothelial layer of the intima. The smooth muscle cells migrate from the muscular layer (4) into the intima. Here they undergo dedifferentiation into fibrocytes. 33792iCourtesy Ashley Davidoff MD.
endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
The next phase of atherosclerosis occurs following smooth muscle proliferation and migration from the media into the evolving plaque. Smooth muscle also undergoes apoptosis and death. The vascular smooth muscle produces the extracellular matrix has major contribution to the atheromatous lesion. Interstitial collagens (types I and III) and proteoglycans such and elastin fibers also accumulate in atherosclerotic plaques. Accumlation of cholesterol and cholesterol esters occur.
A fibrous capsule around the fatty complex is formed. (33792i, 33801b)
Smooth muscle migrates from the media into the intima and transform into fibrous elements both within the lesion as well superficial to the lesion forming a fibrous plaque.The monocytes and macrophages ingest the fat and foamy fat laden macrophages result. An inflammatory reaction evolves. Continued accumulation of lipid, macrophages, foamy cells, extracellular matrix result in a fibrofatty complex that grows in size over time. As it enlarges it bulges and thins the intima and eventually erodes the surface.
7) Cell death and destruction with associated formation of dystrophic calcification.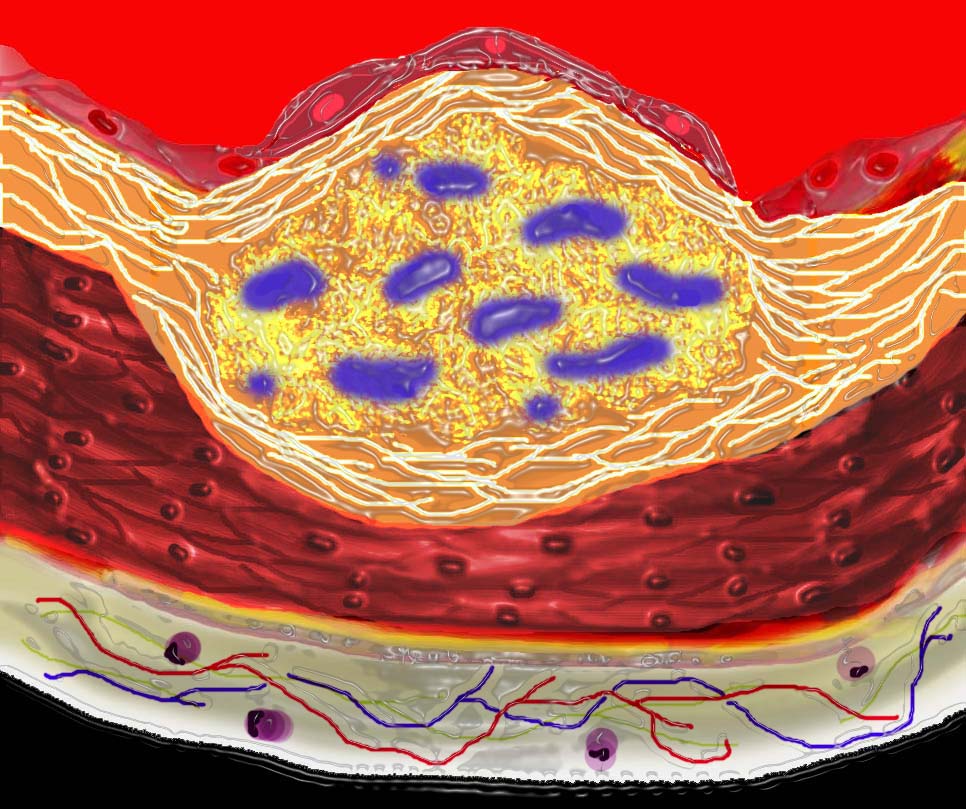
As the disease progresses, cell death within the plaque results, and dystrophic calcification
8) Growth of the atheromatous complex with impingement on the lumen. (33801b)
Progressive dystrophic calcification results in increase in the volume of the plaque. It may grow toward the external surfaceof the artery, in which case it has no hemodynamic significance or toward the lumen in which case it progressively impinges on the lumen
Ashley Davidoff
thecommonvein.net
The progressive impingement on the lumen causes reduction of blood flow, usually manifesting clinically with angina when the lumen is reduced by 70% of its original size.
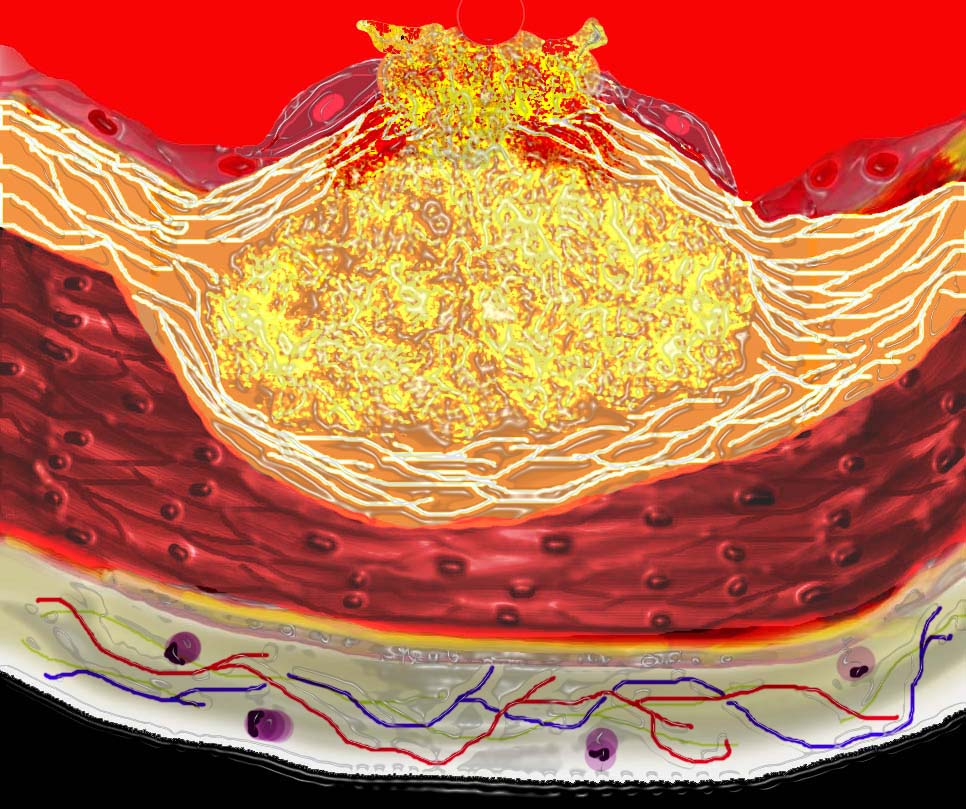
9) Potential of the complex to rupture.
801d) Acute rupture of a plaque predisposes to superadded thrombosis and occlusion of the lumen.
Plaque Rupture
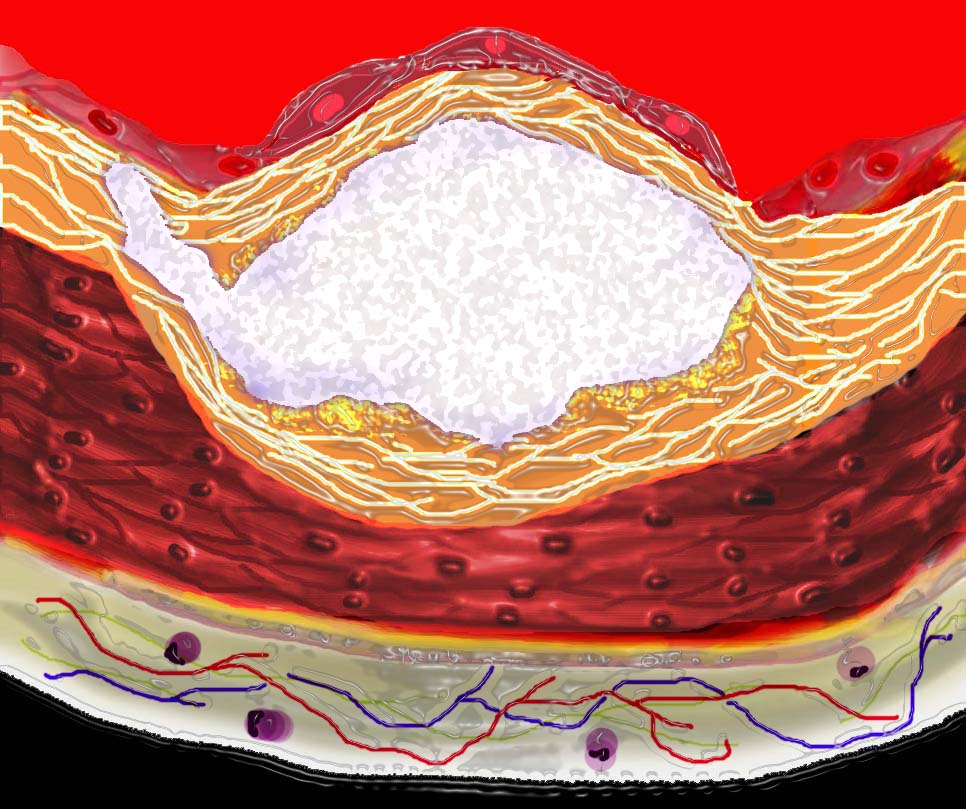
This diagram shows denudation of the endothelial layer with exposure and rupture of the contents of the atherosclerotic plaque in volcanic fashion into the lumen. This event is catastrophic and can result in acute thrombosis and may even be a fatal event. 33801d Courtesy Ashley Davidoff MD. code heart artery atherosclerosis atheroma vulnerable plaque drawing Davidoff art
Ashley Davidoff
thecommonvein.net
Acute myocardial infarction and death are complications of this event. The initial phase of endothelial injury has multifactorial contributing factors including hypertension, hemodynamic factors, hyperlipidemia, homocysteine, smoking, toxins, immune reactions, and viral disease.
The American Heart Association classification divides atherosclerotic lesions into six types; foam cells ( fatty dots) – Type I fatty streaks, – Type II atheromas, – Type III fibroatheromas, – Type IV complicated lesions (Stary)
This diagram shows the yellow spheroidal lipoproteins traverse the injured epithelium (2) from the lumen (red) and binding to the linear shaped proteoglycan molecules in the intimal layer. (3) In essence the lipoprotein is “captured”, because it has been altered structurally and is unable to return to the circulation. Courtesy Ashley Davidoff MD. 33792e code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing
The diagram shows an evolving atheromatous plaque with inflammatory cells, monocytes, and lymphocytes infiltrating the intima which contains the lipoprotein- proteoglycan complex, extracellular lipid , and cholesterol crystals. 33792g Courtesy Ashley Davidoff MD. code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing
This drawing shows migration of the monocytes into the intima. These monocytes transform into macrophages in the intima and phagocytose the lipid products to become lipid laden foamy cells. The macroscopic correlate at this stage is the fatty streak. Courtesy Ashley Davidoff MD 33792h . code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing
This diagram shows the reaction of the smooth muscle cells (b) to the formation of foam cells (a) in the subendothelial layer of the intima. The smooth muscle cells migrate from the muscular layer (4) into the intima. Here they undergo dedifferentiation into fibrocytes. 33792i Courtesy Ashley Davidoff MD. code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing
The diagram shows the atherosclerotic lesion in the subepithelial layer of the intima which at first bulges toward the media or muscular layer. 33801a Courtesy Ashley Davidoff MD. code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing
The diagram shows the atherosclerotic lesion in the subepithelial layer of the intima which is bulging both toward the media and toward the lumen. There is a central core of fat and necrotic debris, surrounded by fibrous elements which give the plaque its hardness to the feel. The accumulation of fibrous tissue heralds an advanced atherosclerotic lesion. 33801b Courtesy Ashley Davidoff MD. code heart artery

key words heart cardiac artery ramus medianus coronary artery circumflex coronary artery LAD left anterior descending coronary artery mild atherosclerosis calcific plaques CTscan volume rendering 3D Courtesy Ashley Davidoff MD thecommonvein.net
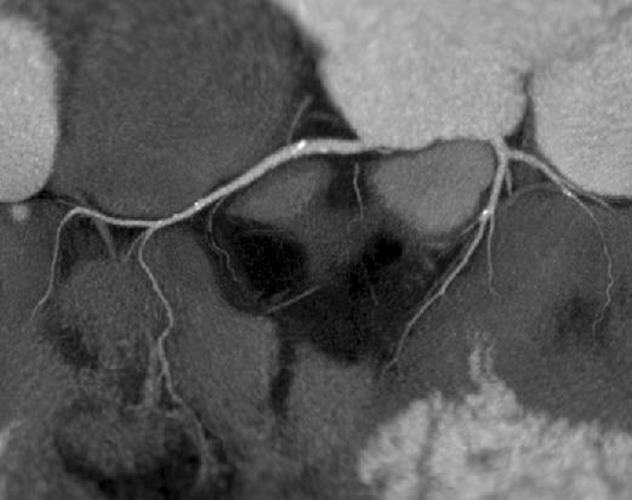
Reconstruction of the coronary CTA shows a calcified non stenotic plaque n proximal LAD, Circumflex and RCA
Courtesy Philips Medical Systems
44157
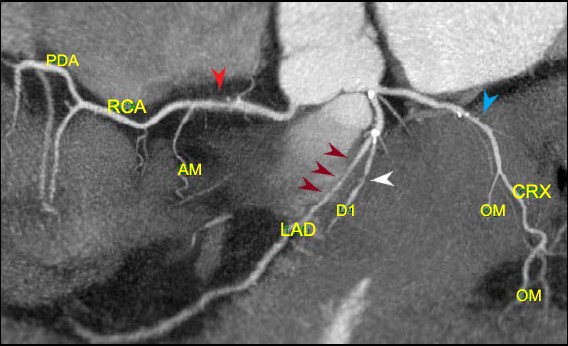
Reconstruction of the coronary arteries shows predominantly non calcified plaque resulting in an elongated stenosis of the proximal LAD (maroon arrows) and short segment stenoses of the proximal RCA (red arrow) circumflex (blue arrow) and diagonal (white arrow) Scattered calcifications are lees prominent in the RCA and circumflex lesions
Ashley Davidoff thecommonvein.net
44047b
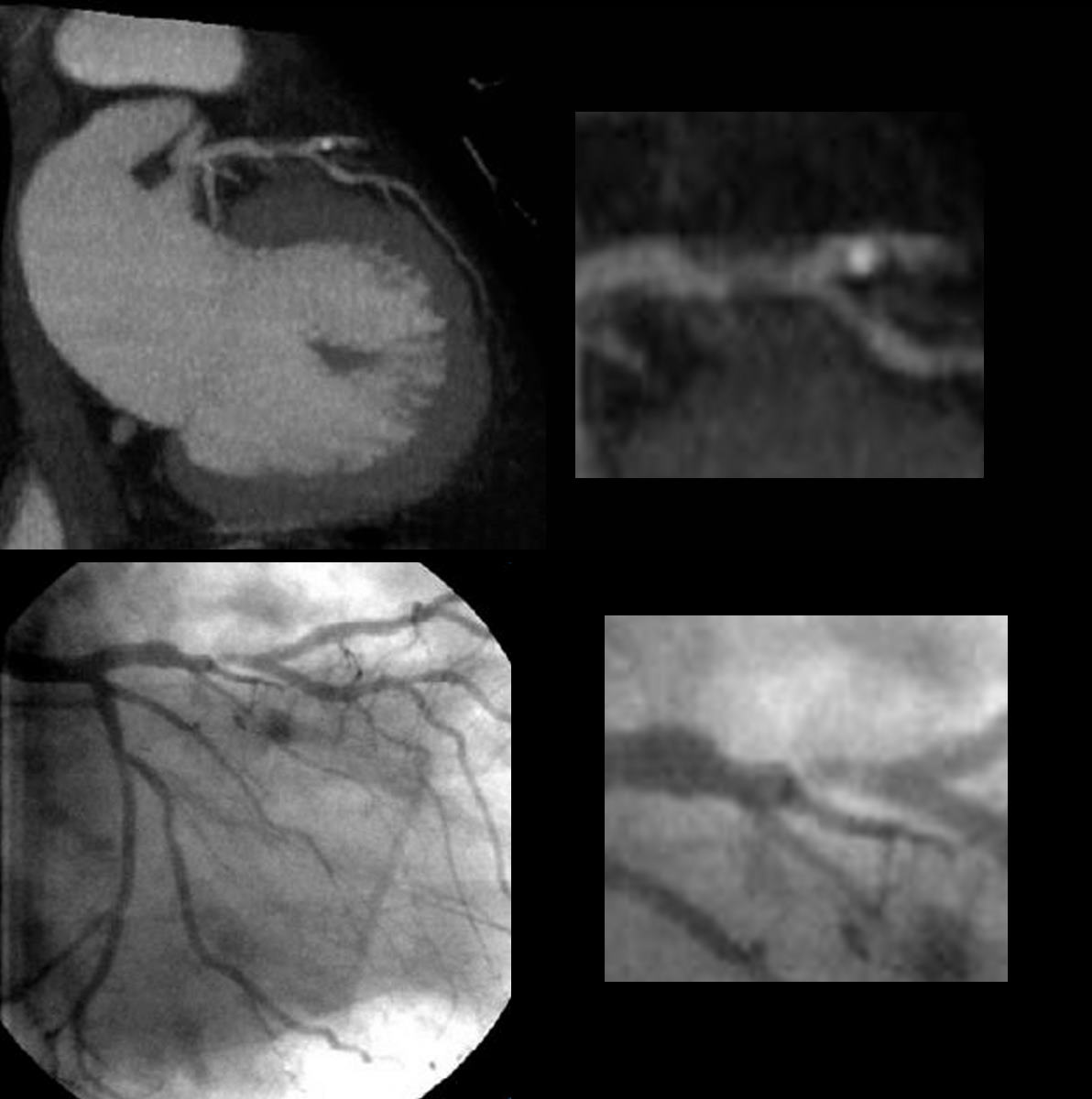
Reconstruction of the coronary CTA (above) shows a predominantly non calcified plaquein the proximal LAD resulting in an elongated stenosis. Scattered calcifications are lees prominent in the RCA and circumflex lesions
The coronary angiogram below confirms the stenoses
Courtesy Philips Medical Systems
44137c
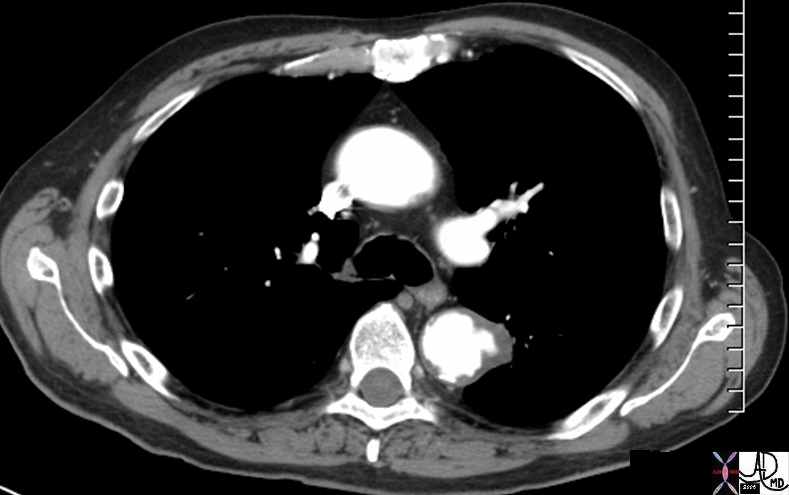
descending thoracic aorta fx aortic ulcer fx atherosclerosis atheroma fx penetrating ulcer
atherosclerosis CTscan
48363
Courtesy Ashley Davidoff MD
thecommonvein.net
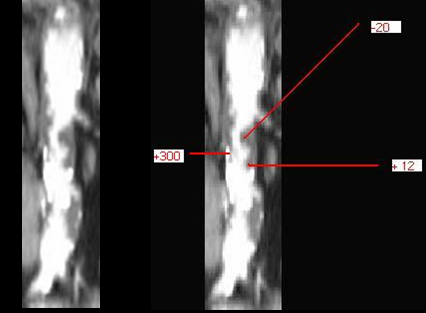
The CYT scan of the abdominal aorta shows severe atherosclerosis. The volume of disease enables measurement of density showing calcified plaque (300 HU) cholesterol plaque (-20HU) and mixed cholesterol and fibrous plaque (20HU)
thecommonvein.net
44217c
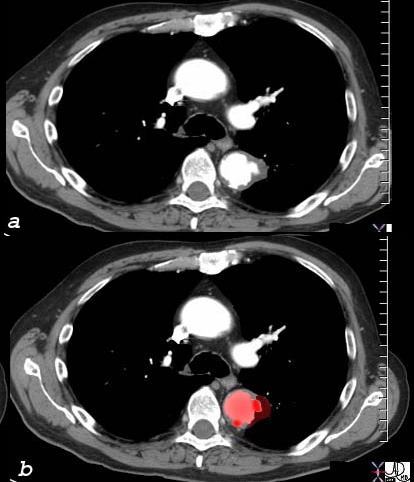
48363c01v
Courtesy Ashley Davidoff MD
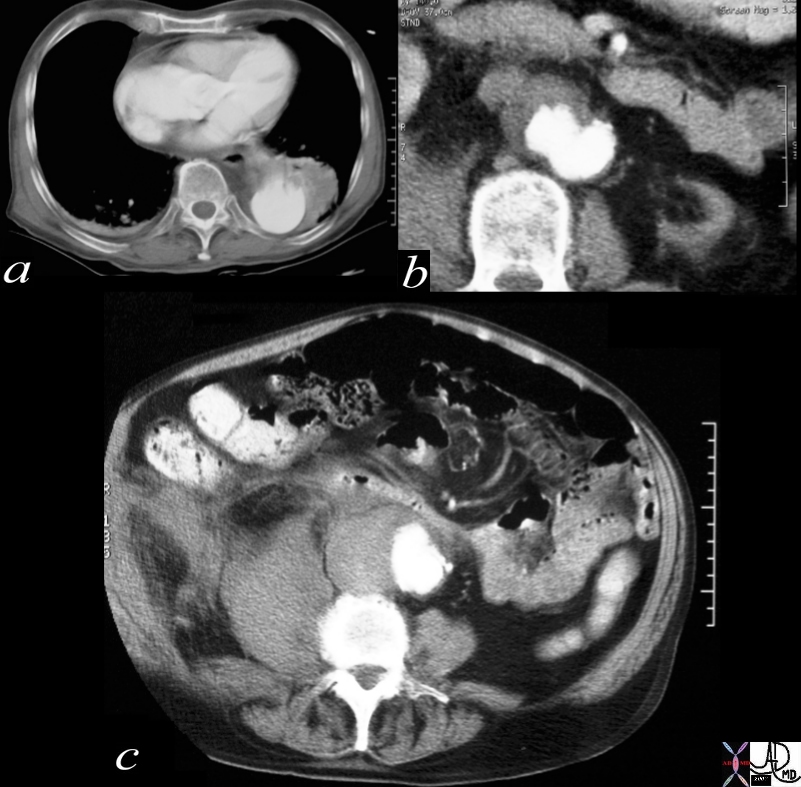
Courtesy Ashley Davidoff MD thecommonvein.net

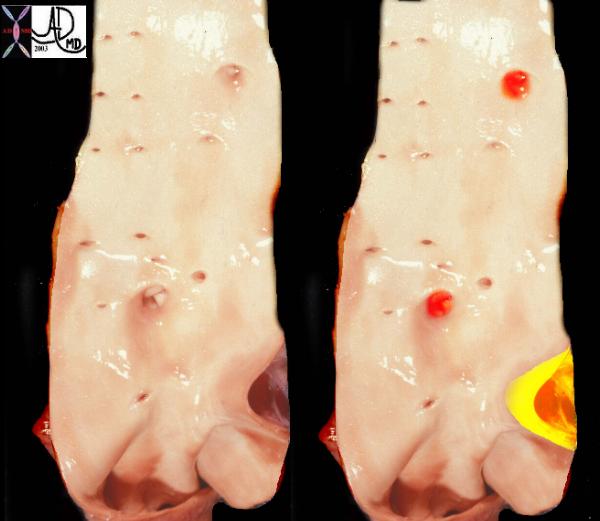
This image reveals the devastating manifestations of aberrant glucose metabolism as a result of insulin insufficiency, with consequent effects on the small vessels throughout the body. In this instance the diabetic arteriopathy is characterised by calcific atherosclerotic diease seen as calcification of the digital artery in b with subsequent ischemia to the foot. The poor nutrition has resulted in infection and ulceration of skin and bone, with poor healing and a need to amputate irrecoverable tissues.
Courtesy Ashley Davidoff MD thecommonvein.net 48471c01
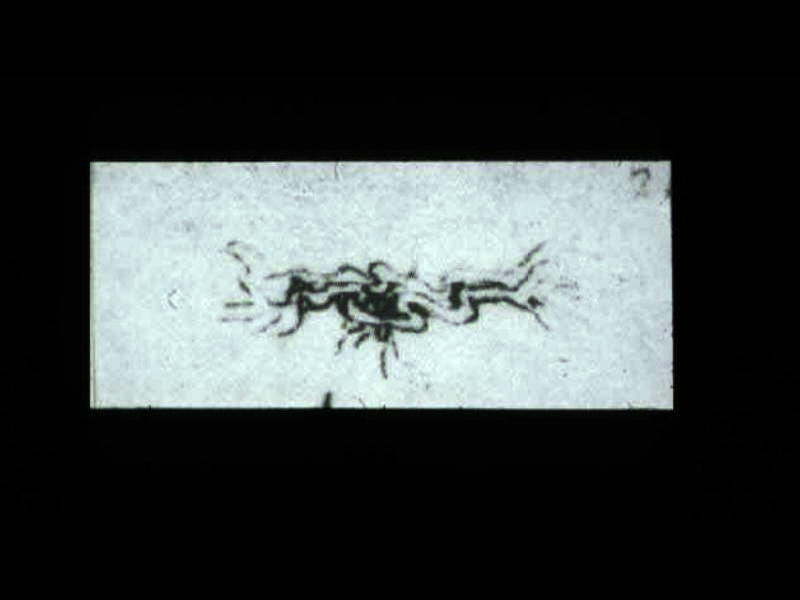
This is a drawing of the “meseraic vessels” – presumably the celiac axis. Da Vinci was able to interview and perform an autopsy on a centenarian. He describes the dessicated and tortuos state of the vessels of this patient accurately depicting the atherosclerotic process. He describes the narrowed lumen and the consequences of poor blood flow.The translation of da Vinci’s text accompanying this one inch image is remarkably insightful and pioneering. (see atherosclerosis hisrorical da Vinci) 13045b