See DB 135
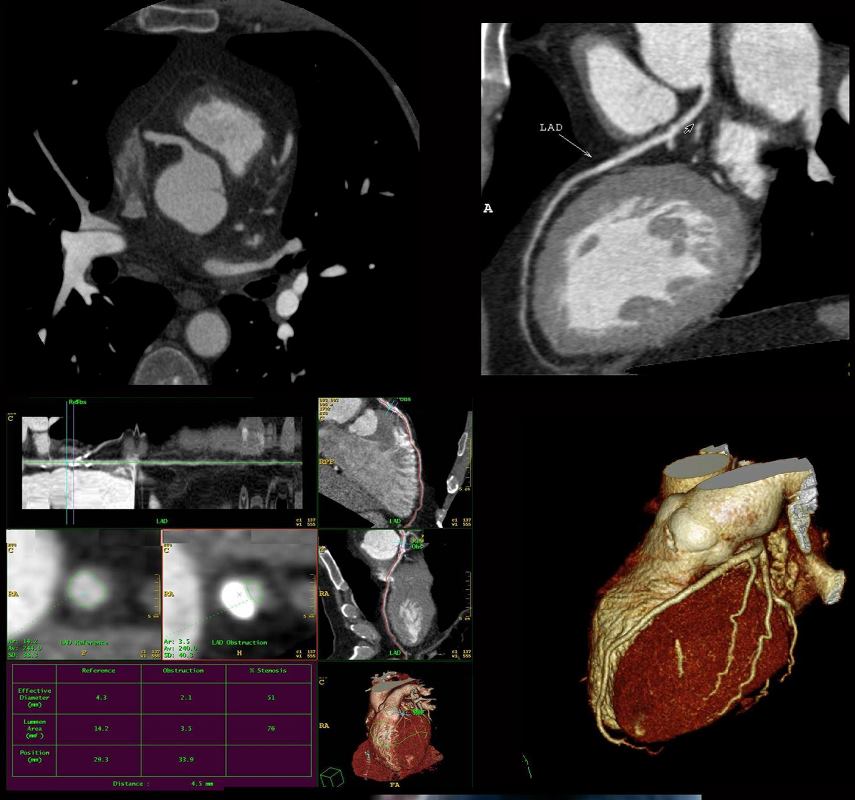
Axial images throughout the R-R cycle acquired in the axial plain and reconstructed in curved reformats and straight reformats and in 3D
Ashley Davidoff thecommonvein.net
-
Definition
- non-invasive imaging modality that
- uses computed tomography angiography (CTA) to obtain
- high-resolution,
- thin slice (sub-millimeter),
- three-dimensional (3D) images of the
- heart, its
- arteries, and the
- great vessels.
- to assess
- presence of CAD
- to evaluate the degree of stenosis
- to prognosticate – MACE
- CONFIRM Study Summary
- CONFIRM Min et al j.jacc.2011.
- Among individuals without known CAD,
- who present with typical or atypical chest pain
- higher rate of mortality
- nonobstructive and
- obstructive CAD by CCTA
- more vessels involved
- the higher the mortality
- CONFIRM Min et al j.jacc.2011.
- PROMISE Study Summary
- PROMISE jamacardiology
- Low intermediate risk
- CTA vs Functional testing
- see web image 258 Anatomic imaging is very sensitive as to who may have a CV event down the line Functional image not so much
- PROMISE jamacardiology
- SCOT Heart Study Summary
- SCOT HEART nejm Newby NEJM
- Primary Care
- Chest pain suspected CAD Stable
- Stress ECG
- CCTA + Standard CAre vs Standard Care
- SCOT HEART nejm Newby NEJM
- NICE Guidelnes Summary
- NICE Guidelines NICE Guidelines- Great Britain
- CONFIRM Study Summary
- to assess perfusion
- to characterize the plaque
- Validation of
- presence of CAD
- Prognostication
- Degree of Stenosis
- Perfusion
- Characterization
- Societal and Validation
- Britain
- Europe
- US
-
Indications
Chest pain no known CAD presenting with
- Stable Typical Pain
- Atypical Chest Pain
- thought to represent a possible anginal equivalent
- Chest Pain with known CAD presenting with
- Stable Typical Pain
- Atypical Chest Pain
- thought to represent a possible anginal equivalent
- Unclear or inconclusive stress test results.
- When considering evaluation for revascularization strategies
-
- ISCHEMIA Trial
-
- Selected asymptomatic high risk individuals
- Rarely appropriate
- very low risk symptomatic patients, e.g., <40 years of age with non-cardiac symptoms (chest wall pain, pleuritic chest
pain) - low- and intermediate risk asymptomatic patients
- very low risk symptomatic patients, e.g., <40 years of age with non-cardiac symptoms (chest wall pain, pleuritic chest
- Risk Stratification
- A strong family history of early heart disease.
- Multiple other risk factors for coronary artery disease (hypertension, diabetes, cholesterol abnormality, smoking)
- Ruling out significant luminal stenoses in stable patients with suspected coronary stenoses, but intermediate pretest likelihood of disease
- most useful in patients with a low-to-intermediate likelihood of CAD
- patients with left bundle branch block of unknown etiology
- patients with new onset heart failure
- Confounding Cath
- Interesting and important associations in syndromes
- polyarteritis (89H)
- congenital coronary artery disease
- congenital heart disease
- Anomalous coronary origins
- aneurysms
- Plaque characterisation
-
Contraindications
- Renal
- Excessive Coronary Calcification
- Relative
- patient?s heart rate,
- body weight, or
- ability to perform a breath-hold,
- contrast or problems with
- vascular access (which may make invasive angiography more prone to complication)?
-
Advantages
- high negative predictive value
- Provides high-definition 3-D images of the arteries feeding the heart and blockages at the earliest stages when they can be treated most effectively
- Most accurate noninvasive diagnostic test for coronary artery disease
- Measures both calcified and noncalcified plaques. Noncalcified plaques are more prone to rupture and cause heart attacks than calcified plaques. By assessing both types of plaque, coronary CTA analyzes your risk for a heart attack.
- Monitor the effectiveness of therapy since noncalcified plaques may shrink with effective treatment
- cross-sectional nature permits visualization not only of the contrast-enhanced coronary artery lumen, but also of the vessel wall (if image quality is adequate). In this way, atherosclerotic plaque can become visible, which is undetectable in the invasive coronary angiogram
-
Disadvantages
- lacking in
- speci?city ie lot of false positives
- positive predictive accuracy, ie lot of false positives
- which has led to the development of value added CTA strategies like fractional ?ow reserve derived from CT and CT perfusion.
- Radiation
- Goal median <5milliSieverts (15 5-10 years ago)
- NM 10-15 milliSieverst
- Limited temporal resolution can reduce image quality, especially if heart rates are above 60 beats per minute (bpm)
- Since data acquired over several heartbeats are necessary to acquire a complete data set, coronary CTA is not reliably possible in patients with arrhythmias (scanner design concepts with ?256 slices may help overcome this limitation).
- analysis was limited to segments of ?1.5 mm in diameter.
- Also, there is a tendency to overestimate the degree of stenosis in CT as compared with the invasive angiogram,
- extensive calcifications can render image interpretation impossible.
- In patients with a very low pretest likelihood, the false-positive rate may be too high,
- patients with a very high pretest likelihood, sensitivity may not be sufficiently high.
- patients with a high pretest likelihood of disease, performing an invasive, catheter-based coronary angiogram will often be much more appropriate because it offers the option of immediate treatment.
- lacking in
-
Aim
-
Method
- Patient Preparation and Patient Factors
- Equipment
- Contrast
- Technique
- Gating
- Calcium Score
- When is it too high
- Coronary Evaluation
- Axial
- MPR
- 3D
- Ventricular Evaluation
- LV
- EF
- mass
- LV
- Myocardial Perfusion
- FFR
-
Results
- Evolving technology
- Fractional ?ow reserve derived from CT
- Lesion specific stenosis
- Calcific plaque limits
- CT perfusion.
- Global
- Tissue Characterization
- Fractional ?ow reserve derived from CT
- CAD RADS
- Linking reporting to Management Situations
- 1-5
- 2 Atheroscleosis
-
Conclusion
-
Summary
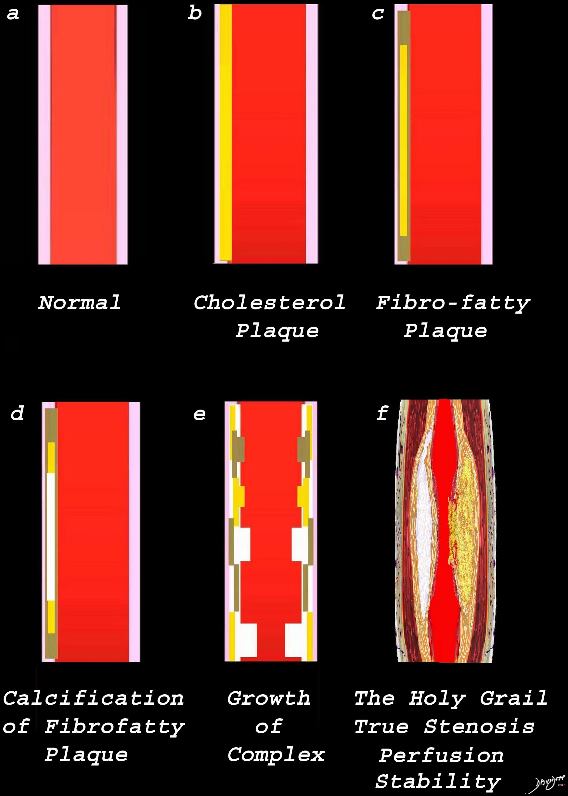
Image a is a normal artery – The wall is overlaid in pink. Image b reflects the early atherosclerotic process with cholesterol infiltration creating the cholesterol plaque (yellow). Image c shows the yellow plaque with beige fibrotic infiltrate resulting in the fibro-fatty plaque. Image d is a later form of the process where dystrophic calcification starts to be laid down (white overlay. In image e, the individual processes grow resulting in mass effect on the lumen, either as a fatty plaque (yellow) fibrotic plaque (beige) calcific plaque (white) or a mixed process. Image f reflects the holy grail of CT imaging. ? accurate luminal evaluation, perfusion, and characterization of the plaque to determine stability, or lability.
Ashley Davidoff MD thecommonvein.net
- Evaluation of stable chest pain often
-
- requires diagnostic testing with the
- goals of
- detecting coronary artery disease (CAD)
- non obstructive
- obstructive
- assessing the risk of a
- future major adverse cardiovascular event (MACE),
- death,
- myocardial infarction, or
- unstable angina
- future major adverse cardiovascular event (MACE),
- detecting coronary artery disease (CAD)
- Functional Testing
- stress
- EKG
- Echo
- Nuclear Medicine SPECT
- PET
- Structural testing
- Coronary Angiography
- Structure
- CT mostly being used in the low pretest probability
- IVUS
- plaque characterization
- Coronary Angiography
- stress
-
- The predictive value of
- coronary CTA for MACE is similar to that of conventional func- tional testing. PROMISE, SCOT
- However more than 50% of MACE’s occurred in patients with non obstructive CAD Hoffman
- (PROSPECT) trial, studied coronary plaques using
- intravascular ultrasound in survivors of acute coronary syndrome (ACS),
- plaque characteristics (eg, a thin-cap fibroatheroma and a plaque burden >70%) were associated with
- 2.5-fold to 5-fold increased risk of repeat events.(Stone)
- intravascular ultrasound in survivors of acute coronary syndrome (ACS),
- patient Stable CAD Pain in out
- CTA
- CONFIRM Min et al j.jacc.2011.02.074
- 2011 -Multicenter multinational trial
- Aim
- Examine mortality (or prognostic implications)
in relation to coronary artery disease (CAFD
- Examine mortality (or prognostic implications)
- Method
- 23,854 patients
- consecutive cohort of 24,775
- without known CAD
- who met inclusion criteria.
- chest pain atypical or typical
- Time to mortality was estimated using multivari- able Cox proportional hazards models.
- Aim
- CTA
-
-
-
- Results
- Identified and classified CAD
- none (0% stenosis),
- mild (1% to 49% stenosis),
- moderate (50% to 69% stenosis), or
- severe (>70% stenosis).
- 3 year survivalwithout known CAD
- Identified and classified CAD
- Results
- Conclusion
-
-
-
-
- Among individuals without known CAD,
- nonobstructive and
- obstructive CAD by CCTA
- are associated with
- higher rates of mortality,
- Importantly, absence of CAD is associated with a very favorable prognosis.
- Implications for the radiologists to report
- presence of CAD, and also the number of vessels involved in all the CT scans that we read that
- Among individuals without known CAD,
-
-
-
- PROMISE NEJM Douglas P Hoffmann U et al
- 2015 10,003 patients
- Aim
- Outcomes of Anatomical versus Functional Testing for Coronary Artery Disease
- Low intermediate risk
- Method
- CTA vs Functional testing
- Results see web image 258 Anatomic imaging is very sensitive as to who may have a CV event down the line
- Conclusions
- In symptomatic patients with suspected CAD who required noninvasive testing, a strategy of initial CTA, as compared with functional testing, did not improve clinical outcomes over a median follow-up of 2 years.
- SCOT HEART nejm Newby NEJM
- 2018 4146 over 3-5 year
- Primary Care
- Chest pain suspected CAD Stable
- Stress ECG
- CCTA + Standard Care vs Standard Care
- The primary end point was death from coronary heart disease or nonfatal myocardial infarction at 5 years.
- Conclusions
-
CTA in addition to standard care in patients with stable chest pain resulted in a significantly lower rate of death from coronary heart disease or nonfatal myocardial infarction at 5 years than standard care alone, without resulting in a significantly higher rate of coronary angiography or coronary revascularization.
-
- PROMISE NEJM Douglas P Hoffmann U et al
-
- NICE Guidelines official
- NICE GuidelinesNICE Guidelines- UK
- 2016
- removal of the pre-test probability model
- use of CTCA as the first-line investigation
- patients with
- atypical or typical angina symptoms or
- asymptom-atic with suggested EKG changes for ischemia
-
-
- FFR CT
- 05 NXT FFR CT 2014
- Aim
- FFR vs FFR CT
- Multicenter 254 patiientsx
- Conclusions
- FFRCT provides high diagnostic accuracy
- for diagnosis of hemodynamically significant CAD
- comparable with
- with invasive FFR as the reference standard.
- When compared with anatomic testing by using coronary CTA,
- FFRCT led to a marked increase in specificity.
- FFRCT provides high diagnostic accuracy
- Aim
- 05 NXT FFR CT 2014
- FFR CT
-
-
- PACIFIC Trial ACC
- PACIFIC Trial No PDF Just a short commentary
- CT Perfusion
- core 320 study Pub Med Link Full Text
- PERFECTION Study CTp vs FFR CT (Pub Med)
- Impact in hard events
- Cost Effectiveness
-
- TISSUE CHARACTERIZATON
- intravascular imaging has defined characteristics of coronary plaques
- a large necrotic lipid pool,
- a thin fibrous cap, and a
- large plaque burden) that are associated with sudden cardiac death and ACS.(Virmani and Bom)
- Coronary CTA
- can characterize coronary plaques, including the
- detection of
- high-risk features such as
- positive remodeling,
- change in the vessel diameter
- at the plaque site in comparison to the
- reference segment set
- proximal to the lesion in a
- normal-appearing vessel
- low computed tomography (CT) attenuation,
- <30HU
- lipid core was
- 11 +/- 12U (range -15 to +33HU)
- fibrous plaques 78 +/- 21HU (range 32 to 130 HU), and
- calcified plaques 516 +/- 198 HU (range
221 to 1,134 HU); - the density of the lumen was 258 +/- 43HU
HU (range 174 to 384 HU).
- lipid core was
- Based on IVUS studies
- proposed 30 HU as the cutoff point for the detection of lipid
- sensitivity and specificity of 91% and 100%
- <30HU
- or napkin-ring sign. (Motoyama, and Puchner) Motoyama PDF
- Nice image. Williams Scot 2019
- positive remodeling,
- high-risk features such as
- detection of
- can characterize coronary plaques, including the
-
- Abdelraman et al JACC 2020
- Ferencik Extension of PROMISE
- Guidelines
- October 2021
- Reference
- Serruys et al State of the Art JACC
Blankstein Blankstein Training Cardiologists
- Serruys et al State of the Art JACC
