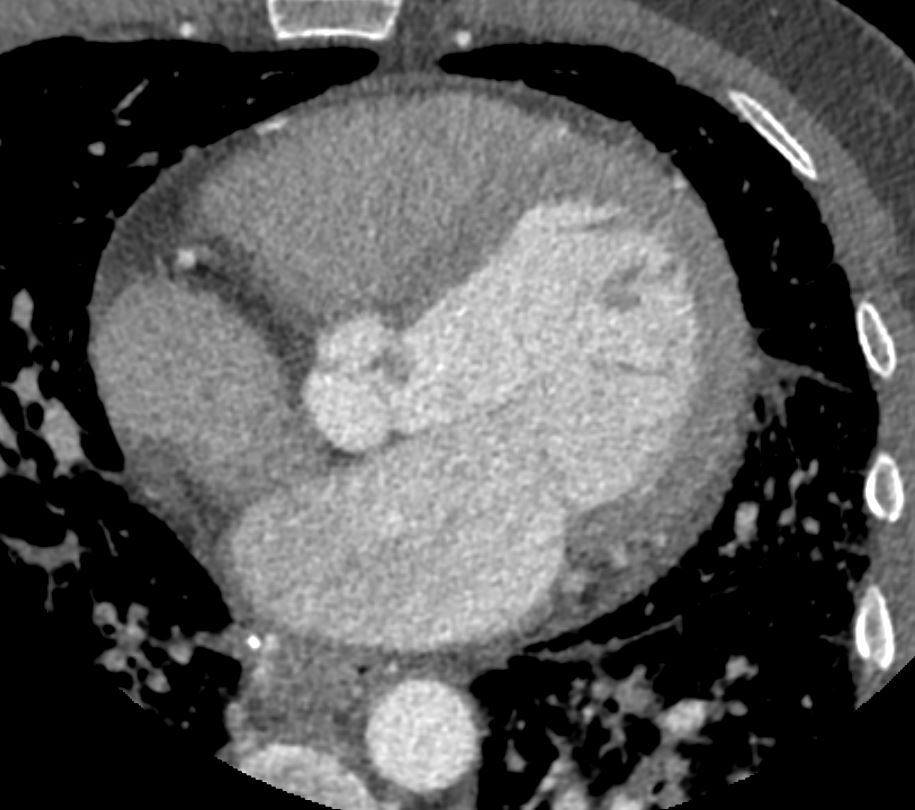
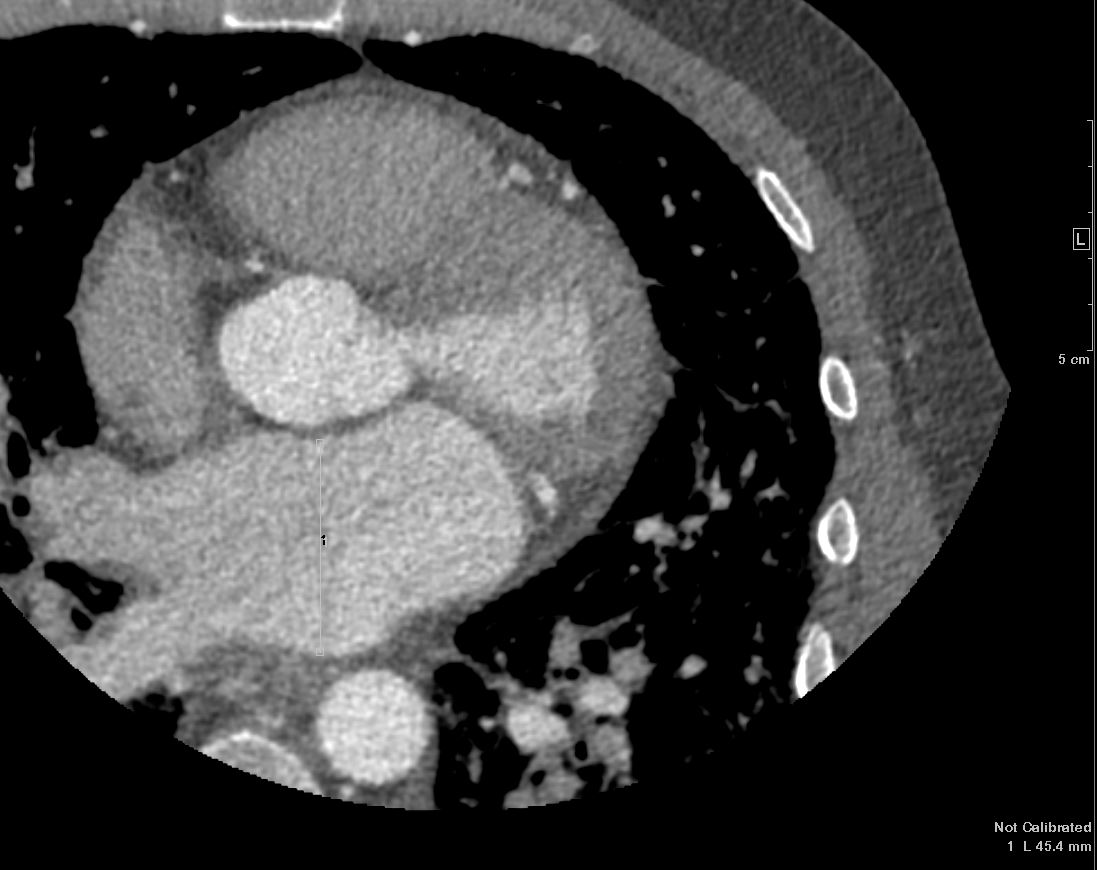
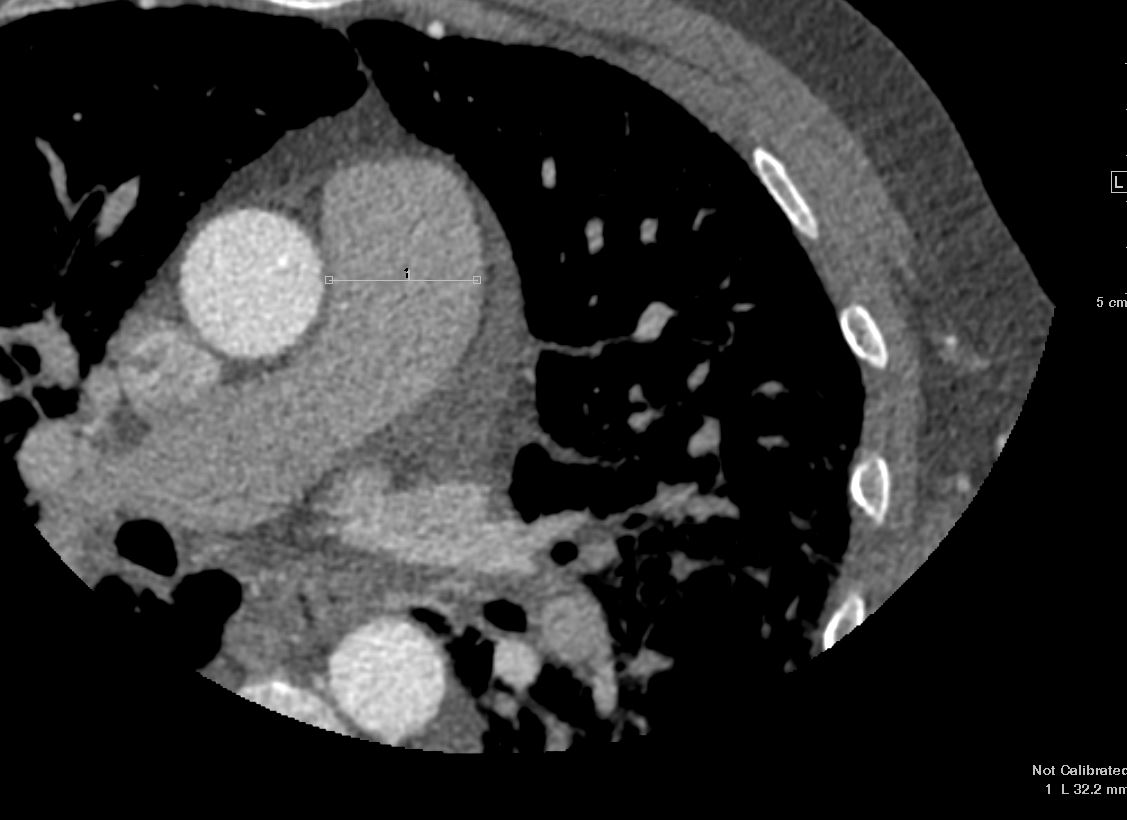
- 51 yoM with a
- PMHx of sarcoidosis on prednisone who presented t
- Rothia bacteremia and
- splenic infarcts.
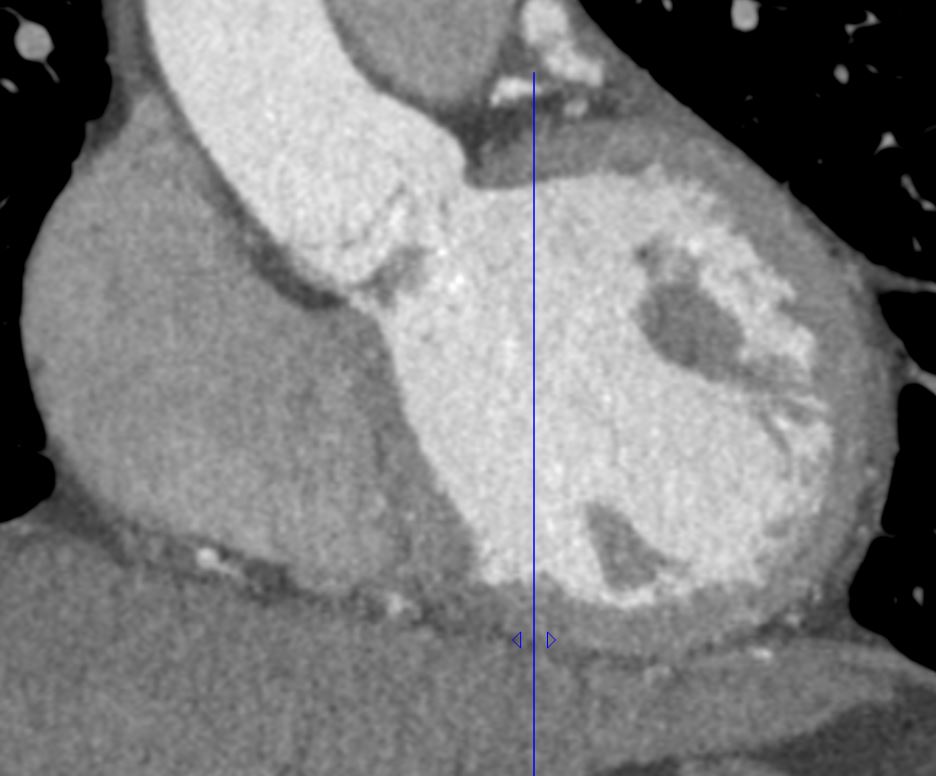
- moderate size vegetation or mass on the aortic valve measuring 1.2 cm on a TTE c
Echo
The left ventricle is severely dilated. There is normal left ventricular wall thickness. Left ventricular systolic function is normal. Left ventricular ejection fraction calculated by modified Simpson’s method is 69%. There are regional wall motion abnormalities as specified. Assessment of diastolic parameters indicates normal left ventricular diastolic function and normal
filling pressures.
Left Atrium
The left atrium is severely enlarged.
Right Atrium
Normal right atrial size.
Right Ventricle
Normal RV size and function.
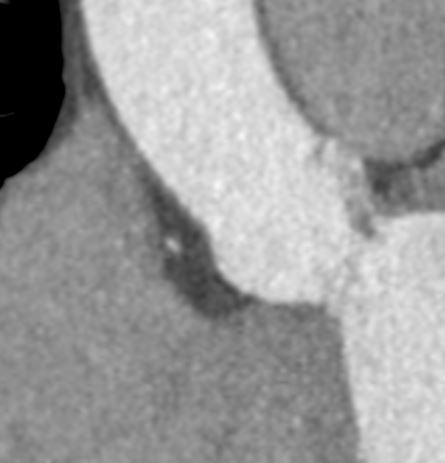
Aortic Valve
The aortic valve is trileaflet and structurally normal. Severe aortic
regurgitation. There is no aortic valve stenosis. There is a moderate size vegetation or mass on the aortic valve. There is a vegetation or mass on theaortic valve measuring 1.2 cm.
1. The left ventricle is severely dilated (101 ml/m2) with normal systolic function. No focal wall motion abnormalities identified. Calculated LVEF: 69% using the modified biplane Simpson’s method. Indices of diastolic function are normal.
2. Normal right ventricular size and systolic function.
3. Moderately to severely increased LA indexed volume (49 ml/m2).Grossly
normal RA size. There is no interatrial shunt flow seen on color Doppler
interrogation. There are late appearing bubbles in the LV after injection of
agitated saline in the resting state, suggesting normal transpulmonary transit; however, after repeat bubble study with Valsalva, there appears to bebubbles in the left heart 4-5 beats after opacification of the RA, suggesting a PFO.
4. The aortic valve cusps are not well visualized. There is an ill-defined, mobile echodensity on the LV side of the aortic valve that is suspicious for vegetation (12 mm in the apical 3 chamber view). AI is present, is difficult to quantify on color Doppler imaging, but appears to be severe (end diastolic Ao-LV gradient is 20 mmHg, there is pandiastolic flow reversal in the proximal descending thoracic aorta and early to mid diastolic flow reversal in the
abdominal aorta). The peak velocity across this valve is elevated at 2.4 m/sec, likely reflecting high transvalvular flow, not stenosis (mean gradient 12 mmHg; DVI: 0.57). Other valves appear structurally normal with trace MR and
trace TR.
5. The IVC is dilated with blunted respirophasic variation c/w elevated RA
pressure. Unable to estimate PA systolic pressure owing to inadequate TR jet.
6. There is no pericardial effusion.
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net

Ashley Davidoff MD TheCommonVein.net
Pulmonary Hypertension
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
Aortic-Valve-Endocarditis-CHF-58M-sarcoidosis-prednisone-009-vegetation-CT--e1675311373109.jpg
Vegetation on the Aortic Valve Right Sinus of ValsalvaAshley Davidoff MD TheCommonVein.net

Splenic Infarct
Ashley Davidoff MD TheCommonVein.net
