In a Nutshell
-
End Diastolic Volume
-
120
-
-
End Systolic Volume
- 50ccs
-
Stroke Volume
- 70ccs
Volume at Peak Systole is About 1/3 the Volume of Diastole
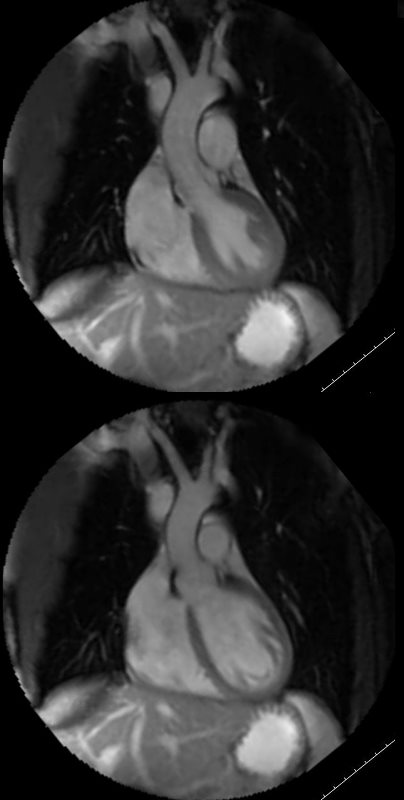
This is the MRI of a 19-year-old male who presented with syncope and the study was performed to identify a possible arrhythmogenic focus
White blood imaging of the LVOT view shows a normal sized ovoid LV in systole (above) and diastole (below). The walls appear normal thickness in the diastolic image, and the approximate residual volume of the LV at peak systole is about 1/3 the diastolic volume indicating an approximate ejection of 2/3 = 66% ejection fraction (EF).
Ashley Davidoff MD
Adult Male Non Indexed
End Diastolic Volume 102-235 (150)
End Systolic Volume 29-93 (70)
Stroke Volume 66-148 (80)
Ejection Fraction (55-73%) 55-60%
Adult Female Non Indexed
End Diastolic Volume 96-174
End Systolic Volume 27-71
Stroke Volume 62-110
Ejection Fraction 54-74
Adult Male Indexed
End Diastolic Volume
End Systolic Volume
Stroke Volume
Ejection Fraction
Adult Female Indexed
End Diastolic Volume
End Systolic Volume
Stroke Volume
Ejection Fraction
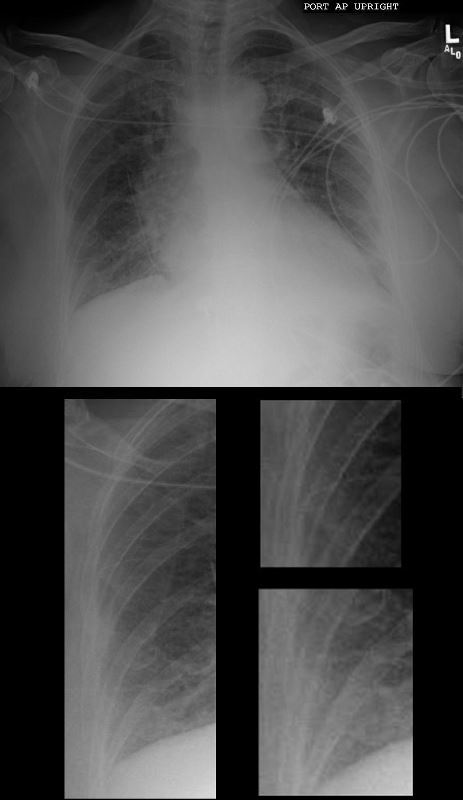
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA) Kerley B lines, and left atrial enlargement.
Ashley Davidoff MD

74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA) Kerley B lines, and left atrial enlargement.
Prior to implantation of a dual lead pacemaker she had a gated cardiac CT to define the venous anatomy.
The scout film shows an enlarged left atrium and suggestion of LV enlargement.
Lung windows confirmed the presence of prominent interlobular septa and LAE.
Axial soft tissue windows shows LAE with A_P dimension of 4.7cms (upper limits of normal is 4cms)
Ashley Davidoff MD
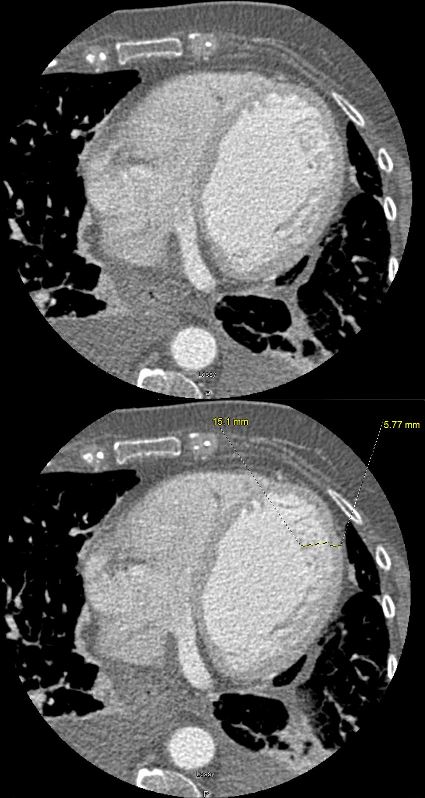
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA) Kerley B lines, and left atrial enlargement.
Prior to implantation of a dual lead pacemaker she had a gated cardiac CT to define the venous anatomy.
The scout film shows an enlarged left atrium and suggestion of LV enlargement.
Lung windows confirmed the presence of prominent interlobular septa and LAE.
Axial soft tissue windows confirmed a diagnosis of non-compaction with non compaction thickness (NC) of 15mm and free wall thickness (C) of 6mm resulting in an abnormal NC:C ratio of 2.5 (upper limits normal NC:C ratio = 2.3)
Volume measurements showed an end diastolic volume of 217mls, an end systolic volume of 159ccs, a stroke volume of 58ccs with a resulting ejection fraction of 26%.
Ashley Davidoff MD
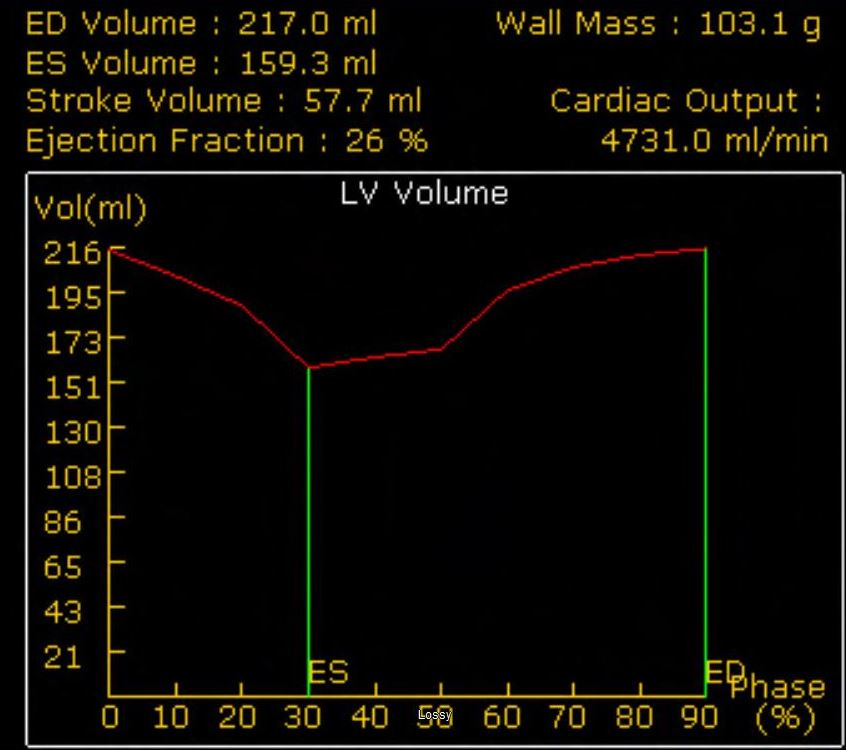
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Volume measurements based on the gated cardiac CT showed an end diastolic volume of 217 mls, an end systolic volume of 159ccs, a stroke volume of 58ccs with a resulting ejection fraction of 26%.
Ashley Davidoff MD
References and Links
- TCV
- Cardiomyopathies
- Case Studies
