1) CHD. Remote large anterior MI, complicated by VSD (25years prior). Expedited VSD/aneurysmectomy repair
2) CHF. Combo LV syst.diast dysfn. TTE (6 years ago) with LVEF 30% and severely dilated chamber. Moderately dilated RV. Severe LAE. MiV with chrodal and papillary Ca++ and secondary2+ MR.
3) EHD. Remote VT-s. ICD placed 40 years ago Later m upgraded to CRT-D (4/2014). Permanent atrial fibrillaiton . Warfarin AC, later switched to DOAC with apixaban 2.5 mg twice daily. (lower diose B/c prior GIBs from Cecal AVMLBB and now Bi-v pacing .
4) VHD (2-3+ MR (see belwo)

Ashley Davidoff MD TheCommonVein.net 0

Ashley Davidoff MD TheCommonVein.net 002

Ashley Davidoff MD TheCommonVein.net 003

Ashley Davidoff MD TheCommonVein.net 001

Ashley Davidoff MD TheCommonVein.net 004

Ashley Davidoff MD TheCommonVein.net 005

Ashley Davidoff MD TheCommonVein.net 006
Ashley Davidoff MD TheCommonVein.net 007
5) Cecal AVM (angiodysplasia). Several laser fulgaratiosn for this . Parenteral iron Rx with Fe-Dextran infusions per HEME/ONc clinic. whre his HCT.Hgb is mointoed.
6) Prior colonoscopy with hyperplastic Polyps removed from transverse colon. Also; hemorrhoids; Diverticulosis Endoscopy NEG for h. Pylorii.
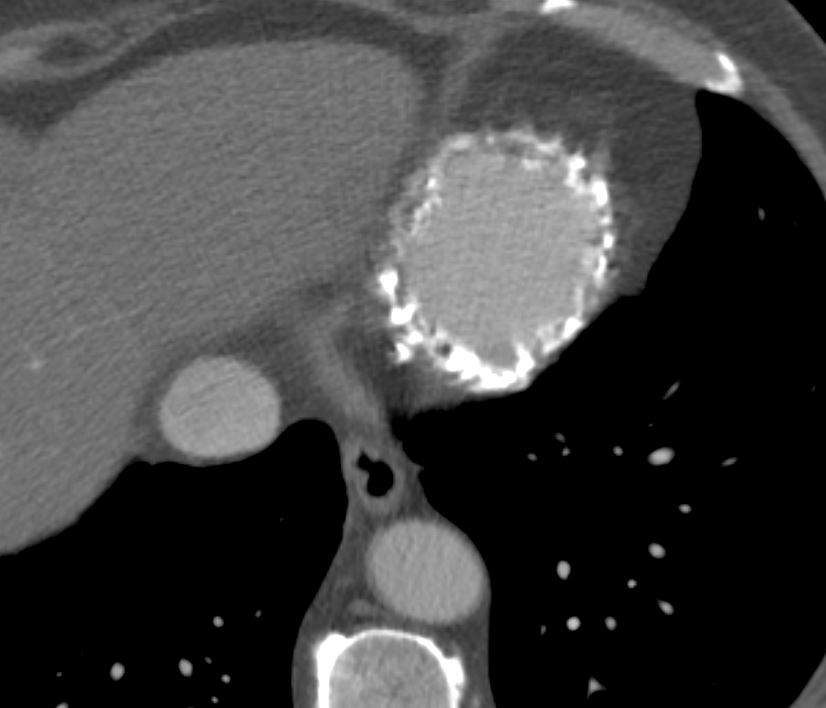
9) RECENT Bx of RLL nodule. PATH: MUCINOUS ADENOCARCINOMA
UPDATED TTE (THEN) LVEF 37% with severely ilated chamber.Scarred akientic base and mild inferior and inferoseptal hypokineisa. Other egions of LV move well. Severe LAE. 3+ posteriorly direct MR. Base on these findings cleared for lung surgery.
2 years ago VATS and RLL wedge resection for Stage 2A3 Adenocarconoma, of RLL. EPS briefly disabled his ICD, then rstored his CRT-D post op.
Echo 2 years ago
Severely dilated LV cavity size; the base- mid inferior wall and inferior
septum are thin, scarred and akinetic; the other walls move normally. No LV
apical clot..
Calculated LVEF (using 3D with post processing) is 37%.
Doppler indices of diastolic function are indeterminate.
RV size is normal but systolic function appears reduced. Pacing wire in right
heart.
Severely dilated LA ( 74 ml/m2); RA size is top normal.
The posterior leaflet of the mitral valve is tethered to the infarcted
posterior wall leading to 3+ posteriorly directed jet of MR ( E velocity 1.4
m/sec; ERO not evaluated).
Other valves appear structurally normal.
Insufficient TR Doppler signal to estimate PA systolic pressure.
IVC is dilated with normal respiratory variation suggesting an RA pressure of
5-10mmHg. No pericardial effusion.
Compared to prior report 4 years priorthe overall findings are similar; the LVEF is
higher on the present study ( previously 30%).
