- 48 year old male without significant PMH who presents with subacute dyspnea on exertion.
- sporadic episodes of palpitations with light-headedness.
- past few weeks
- new progressive dsypnea on exertion
- most prominent when he climbs the stairs
- new orthopnea,
- episodes of PND
- intermittent dizziness
- RUQ pain, and nausea and vomiting
- denies
- LE edema,
- CP,
- syncope.
- new progressive dsypnea on exertion
- mildly tachycardic (100s)
- hypertensive (140s/100s),
- satting well on RA.
- Exam
- epigastric tenderness.
- Labs notable
- unremarkable CBC, CMP, d-dimer 1000, troponin 0.033 to 0.040, BNP 515.
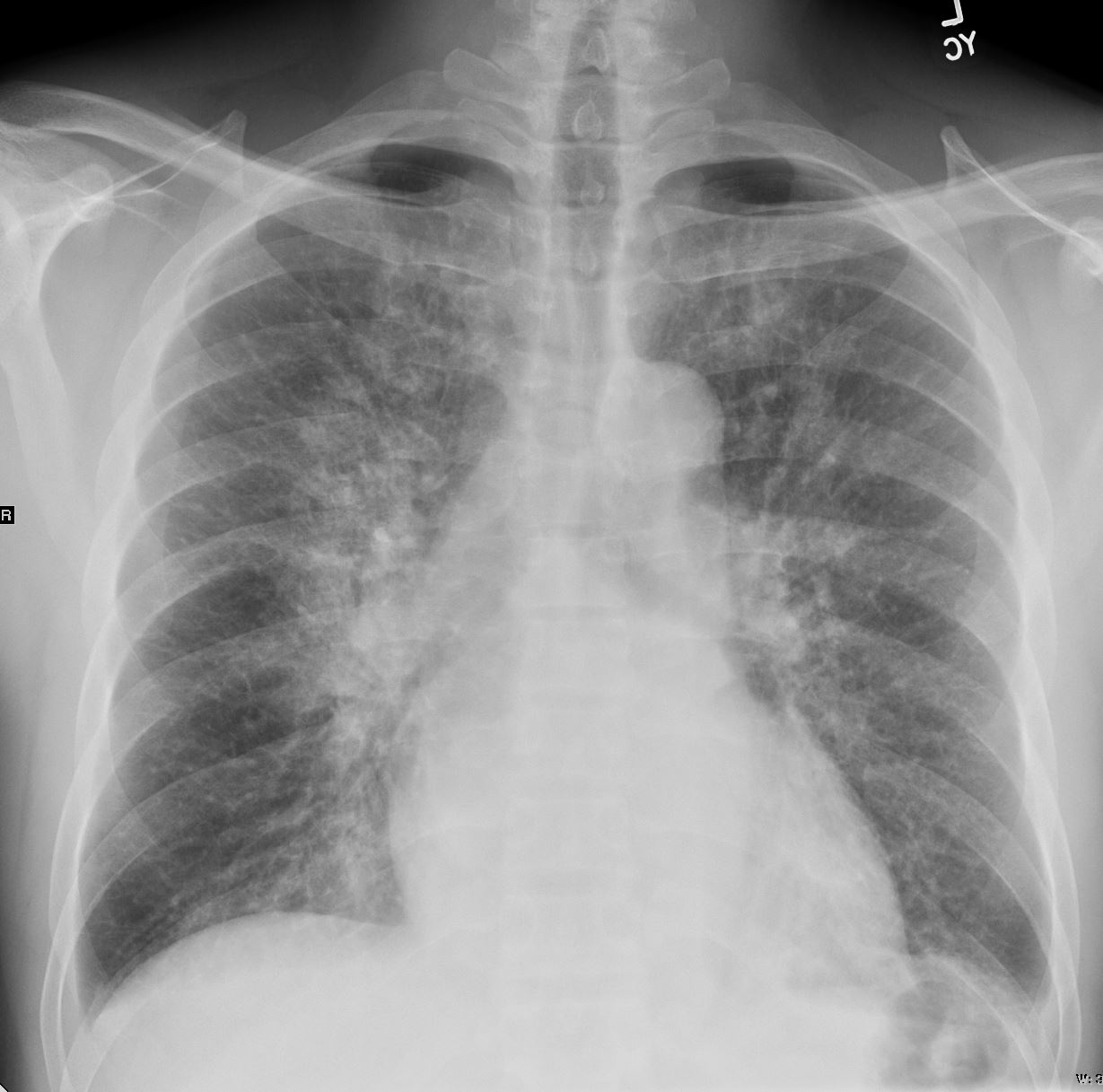
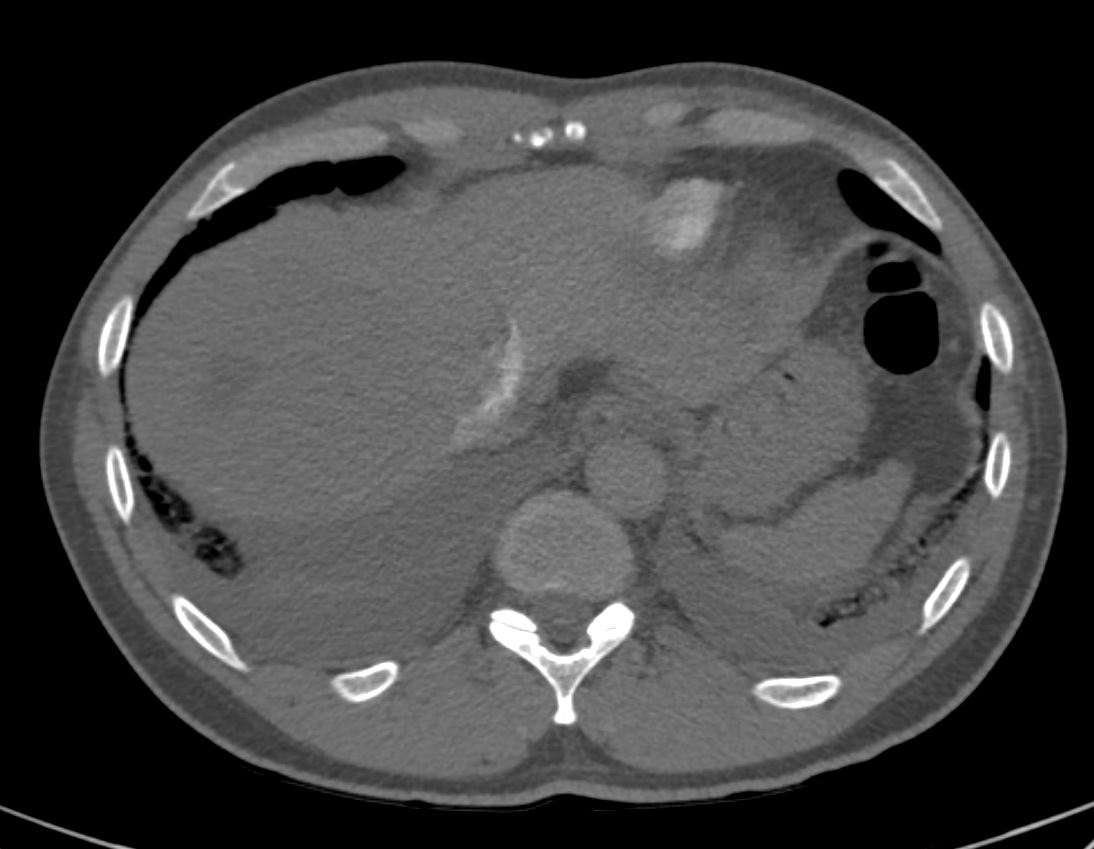
- CXR showed cardiomegaly and increased interstitial markings, small bilateral pleural effusions,
- h/o hepatic hemangioma and tobacco use (3 cig/day) who presented with new HFrEF diagnosis and volume overload associated with elevated troponin and intermittent runs of Vtach.
- CHF service consulted for new acute heart failure of unclear etiology. Pt is s/p left and right heart cath which showed no CAD and low cardiac filling pressures consistent with euvolemia/mild hypovolemia 2/2 diuresis. Pt now on oral medications and started on GDMTProblem Course:
V-tach
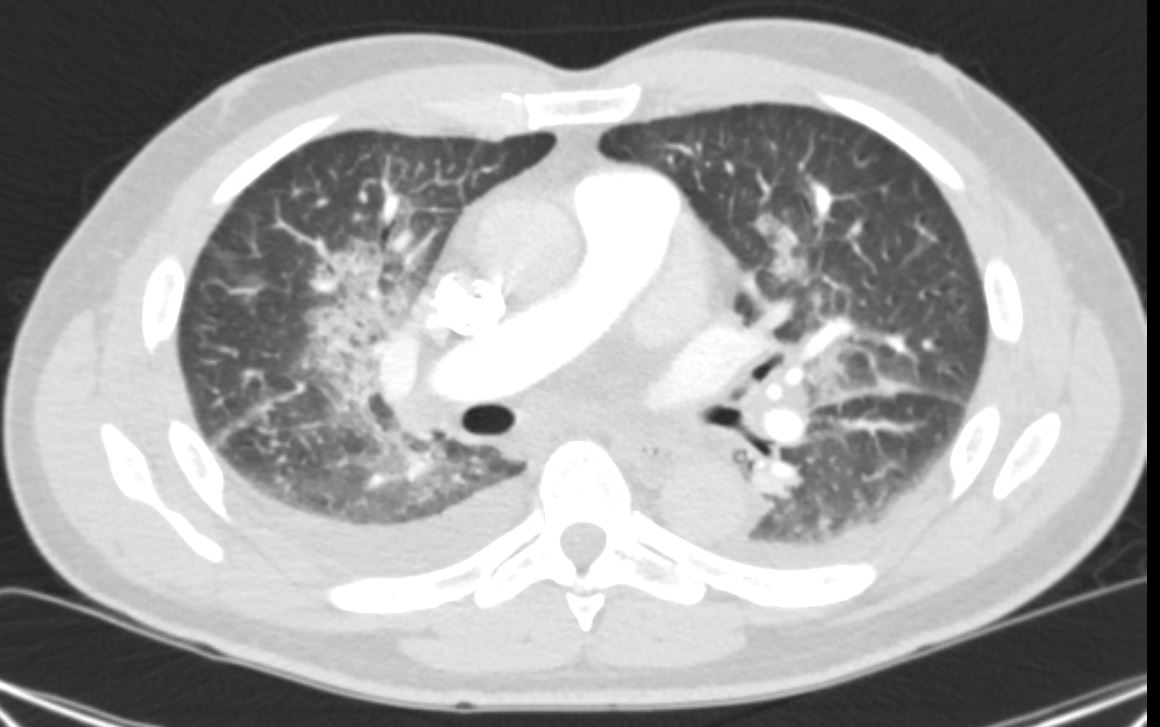
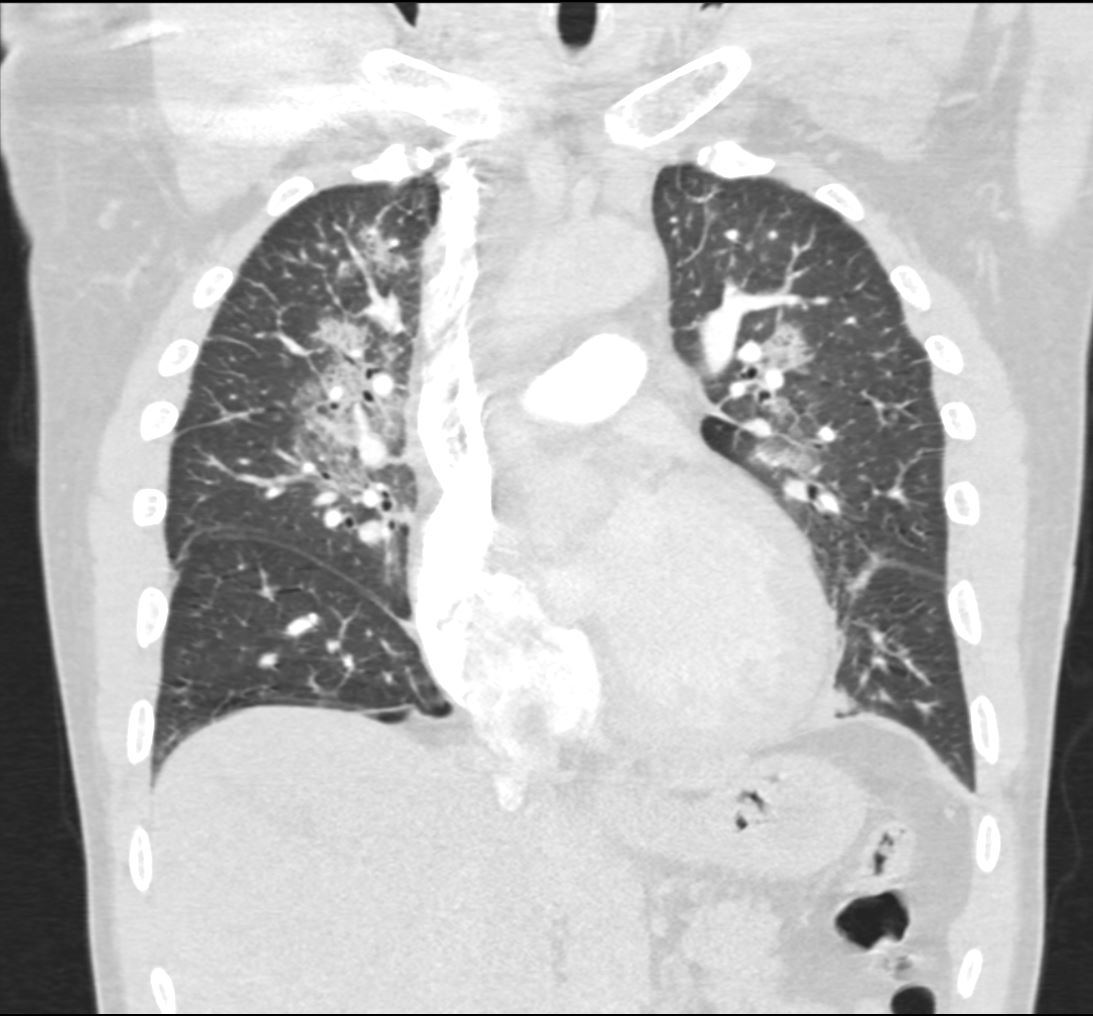
intermittent 8-12 beat runs of Vtach since admission. Concern for underlying ischemia and/or ? Sarcoidosis as etiology for CM
TSH was normalTobacco use
patient reports smoking 3 cigarettes per day since age 16 – denies smoking more than 3 per day over this time* Acute HFrEF (heart failure with reduced ejection fraction)
acute exacerbation with volume overload. New diagnosis. Etiology is broad but most likely 2/2 ischemic CM vs hereditary vs other infiltrative process (HH, sjogren’s, other autoimmune processes).
Although ischemic is most likely pt had Cardiac Cath on which showed no CAD therefore not 2/2 ischemia.Other diagnoses include hereditary, idiopathic, or infiltrative
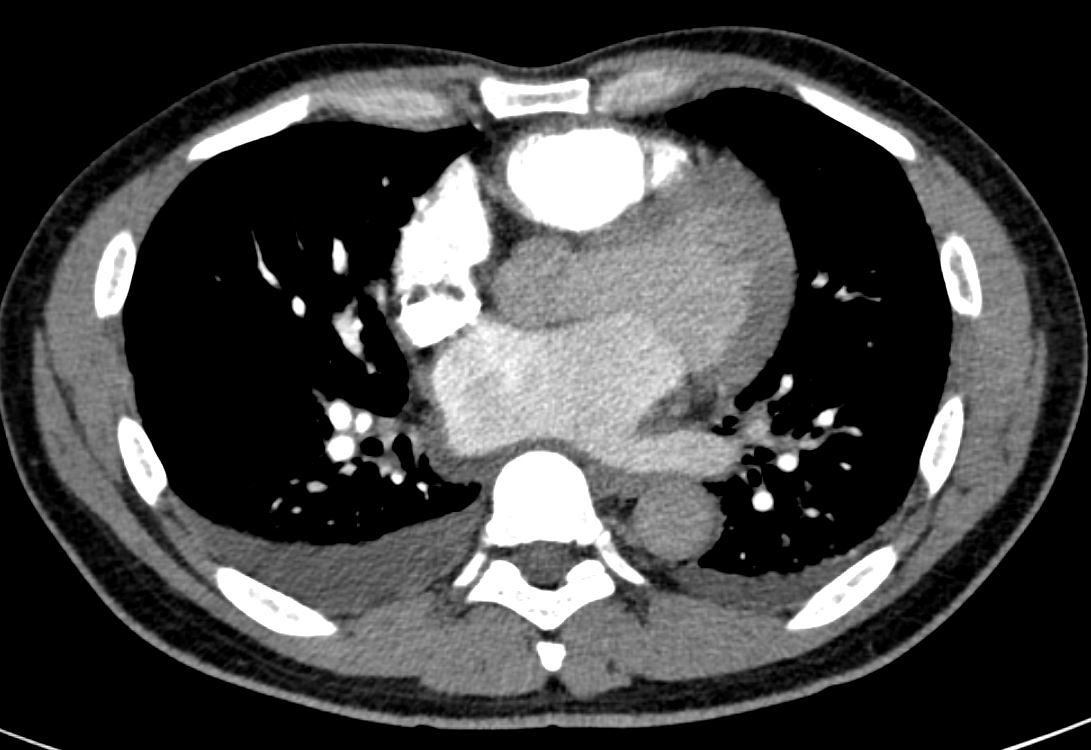
TTE showed EF 15-20% with indeterminate diastolic dysfunction
BNP was 515 on admission
CXR showed interstitial markings and small bilateral pleural effusions
TSH was normal. Patient denies etoh / substance use
Unknown dry weight
Perihilar interstital opacities are consistent with pulmonary edema.
Mild emphysematous changes at bilateral apices
Bilateral pleural effusions R>L
11mm R Hilar Node
Cardiomegaly.