3 years ago
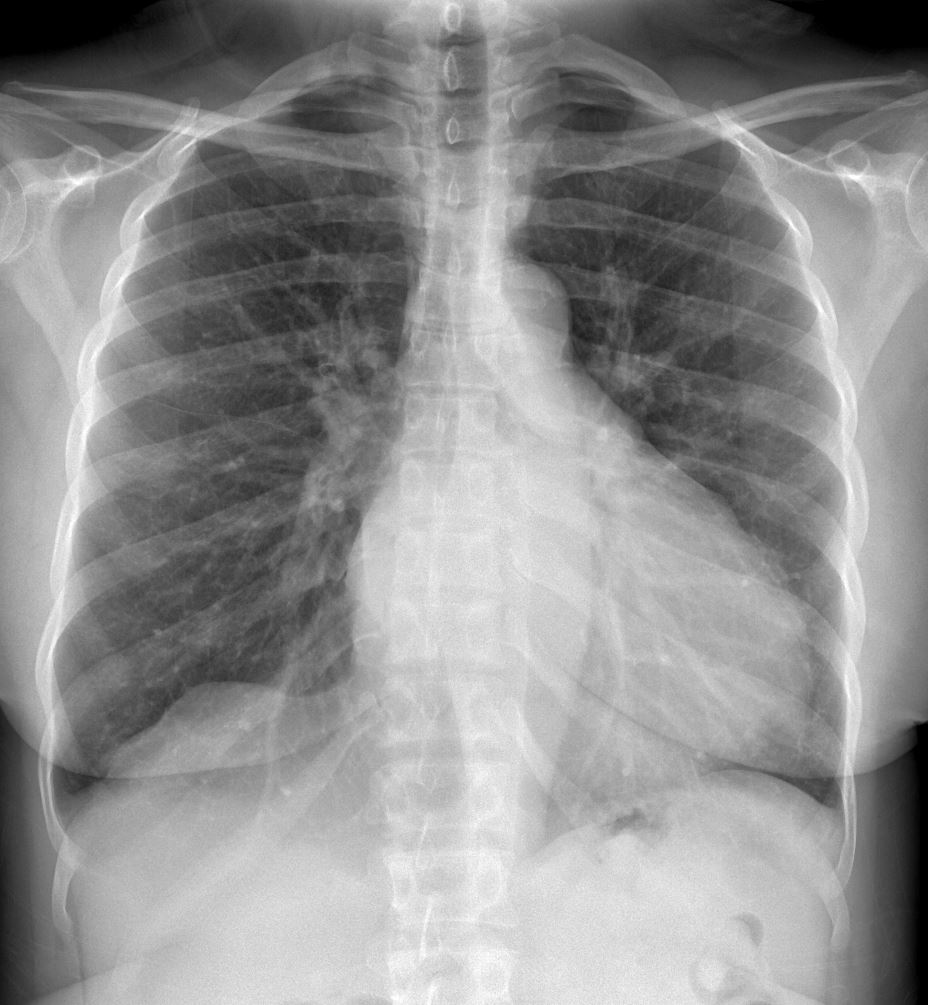
38 year woman with SLE, migraine, seizure, HTN, SVT (s/p ablation) asthma and PSA (crack cocaine and opioids) who presented to ER after a fall with transient LOC. Was brought to ER and noted to have R face/arm/leg weakness and dysarthria in setting of hypertensive emergency (SBP>220, troponemia). Was given IV tPA for NIHSS 11 after SBP controlled with labetolol. Multiple similar prior episodes prompting presentation for stroke work-up. Of note, tox screen +ve cocaine.
PMH: SLE, migraine, Seizure history, HTN, SVT s/p ablation, asthma, polysubstance abuse
The patient was critically ill with:
Acute right sided paresis
Acute on chronic kidney injury
Type II NSTEMI
Acute hypokalemia
Acute hypomagnesemia
Acute cocaine toxicity with acute hypertensive emergency.

Ashley Davidoff thecommonvein.net

Ashley Davidoff thecommonvein.net

Ashley Davidoff thecommonvein.net

Ashley Davidoff thecommonvein.net
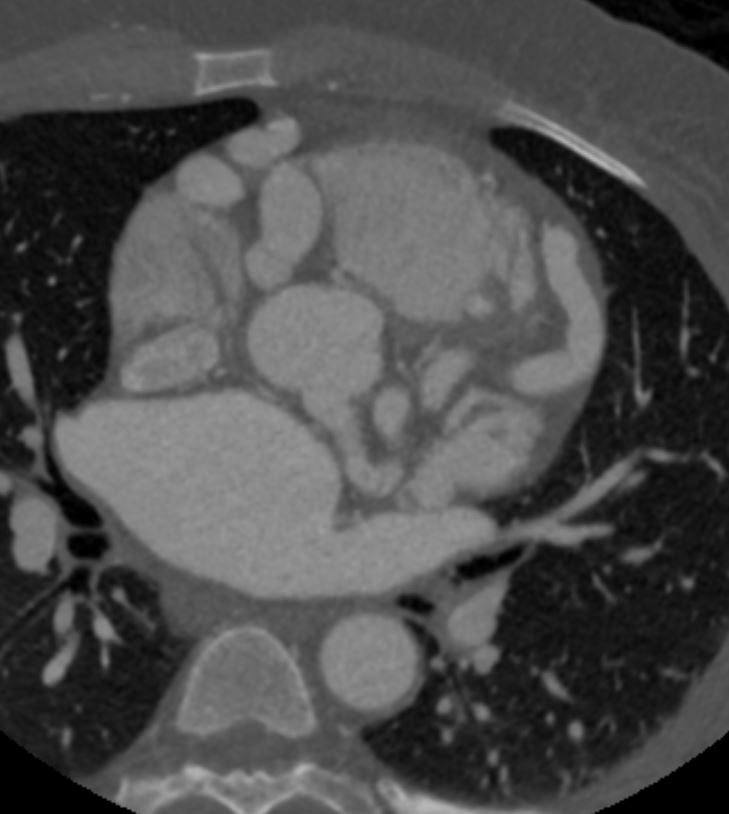
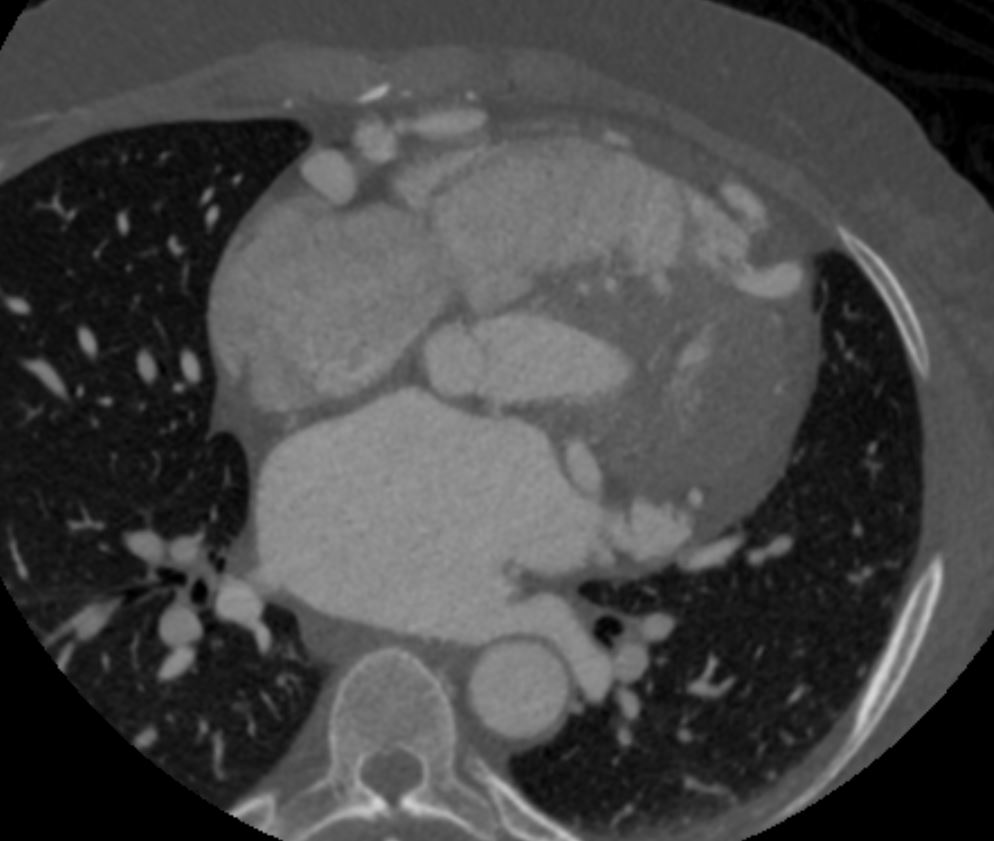
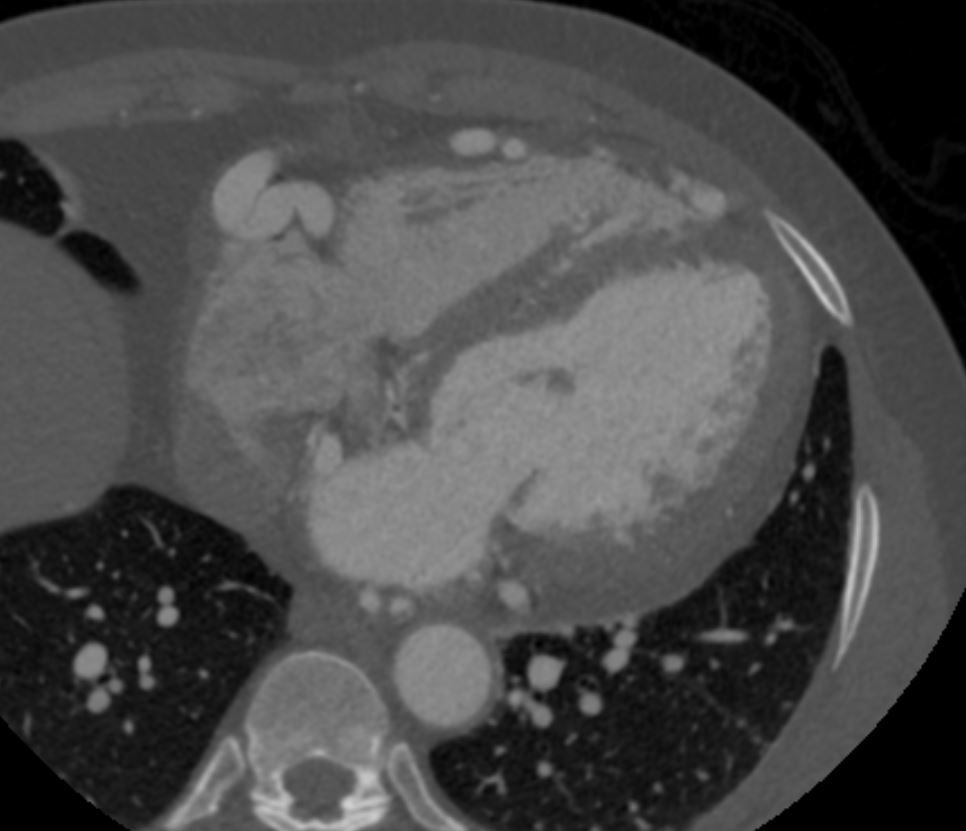
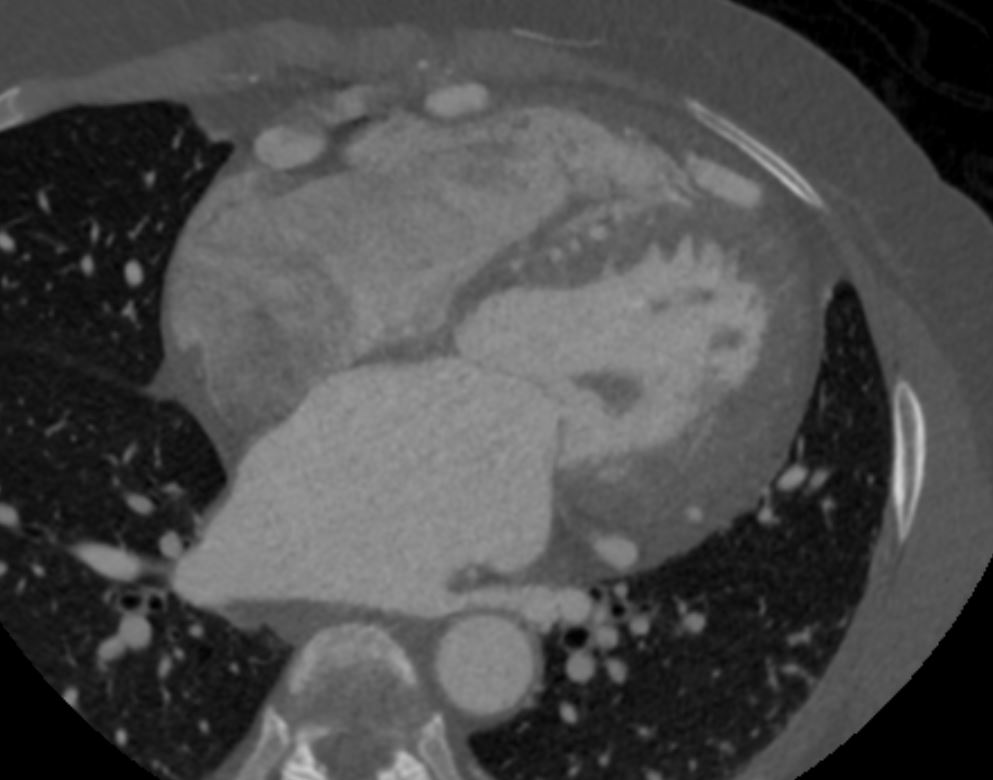
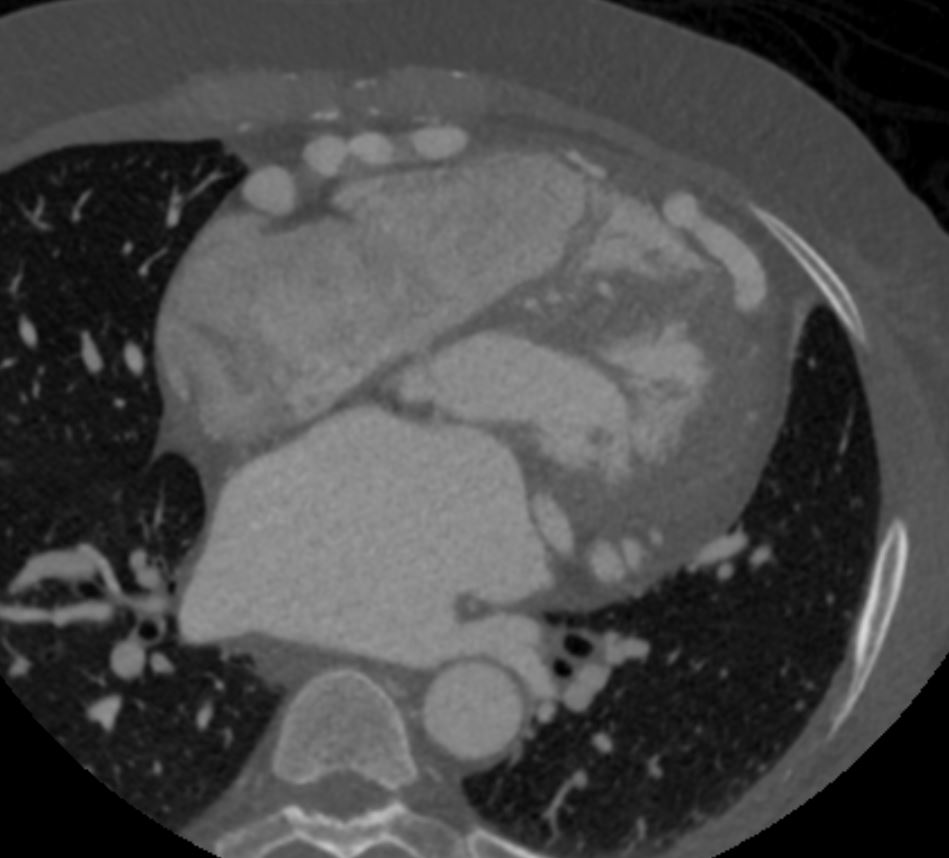
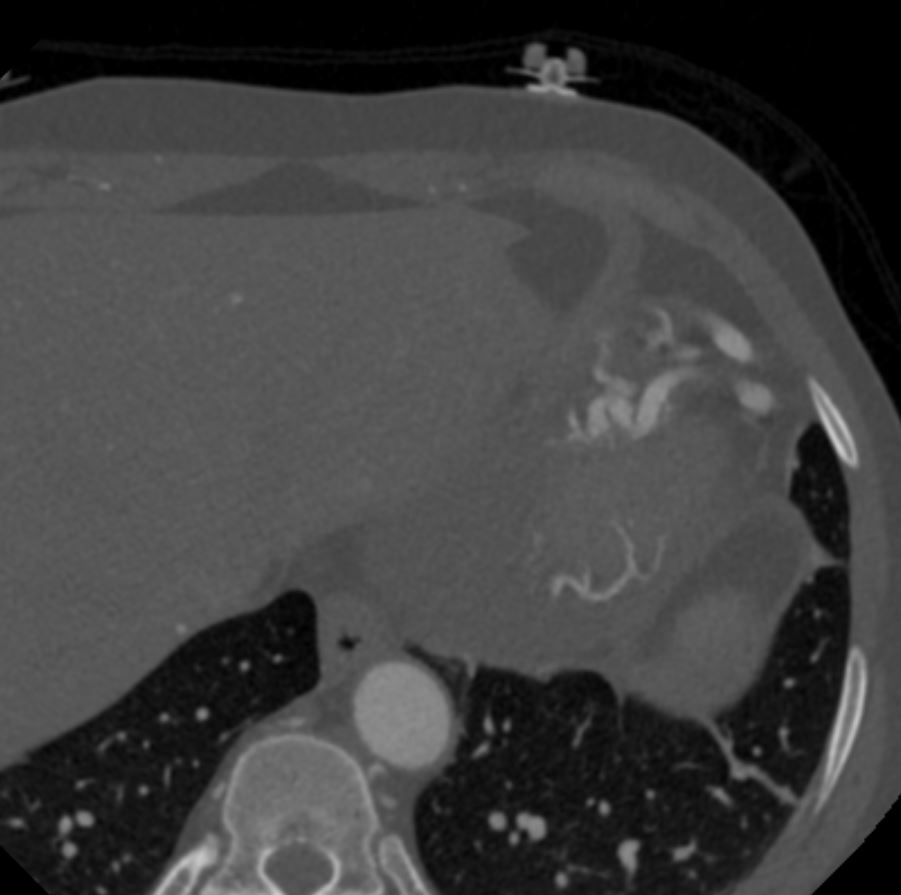
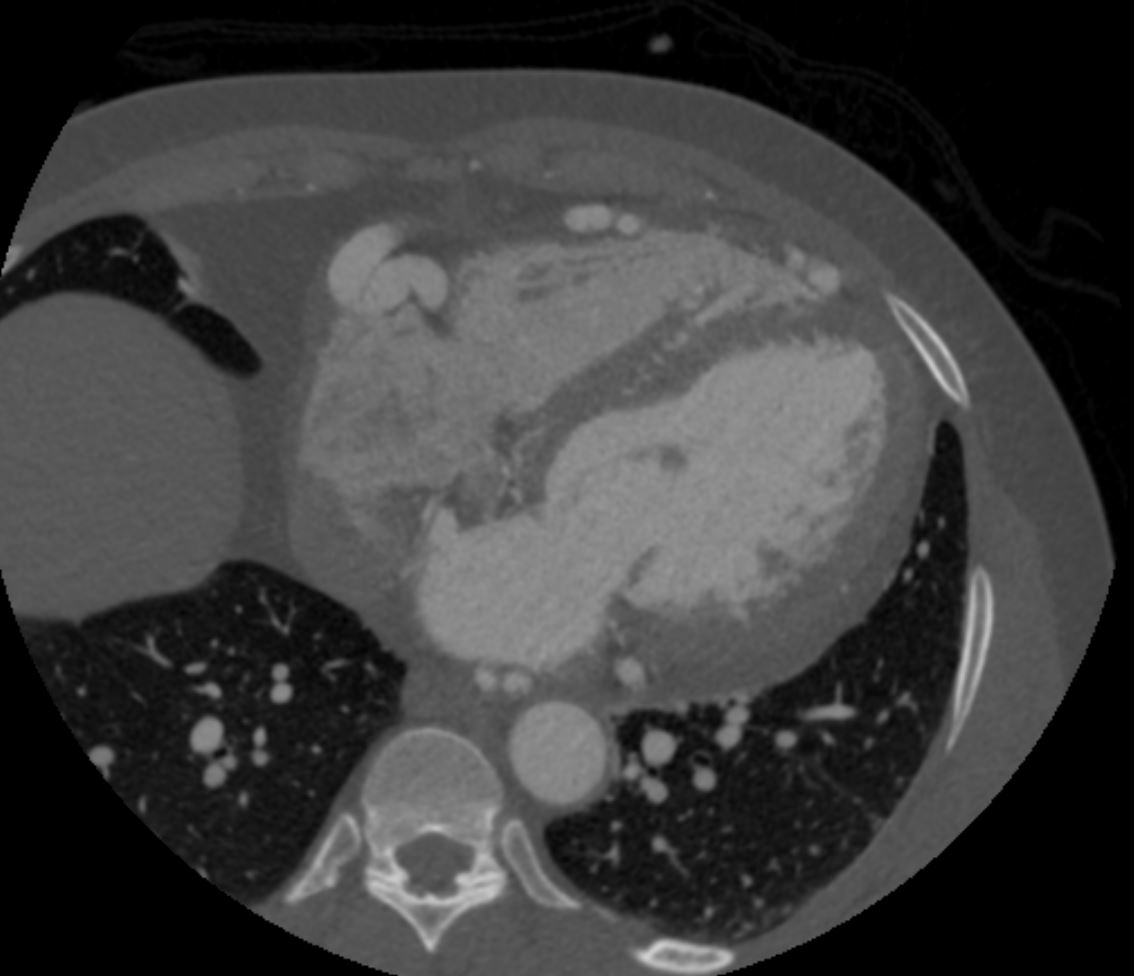
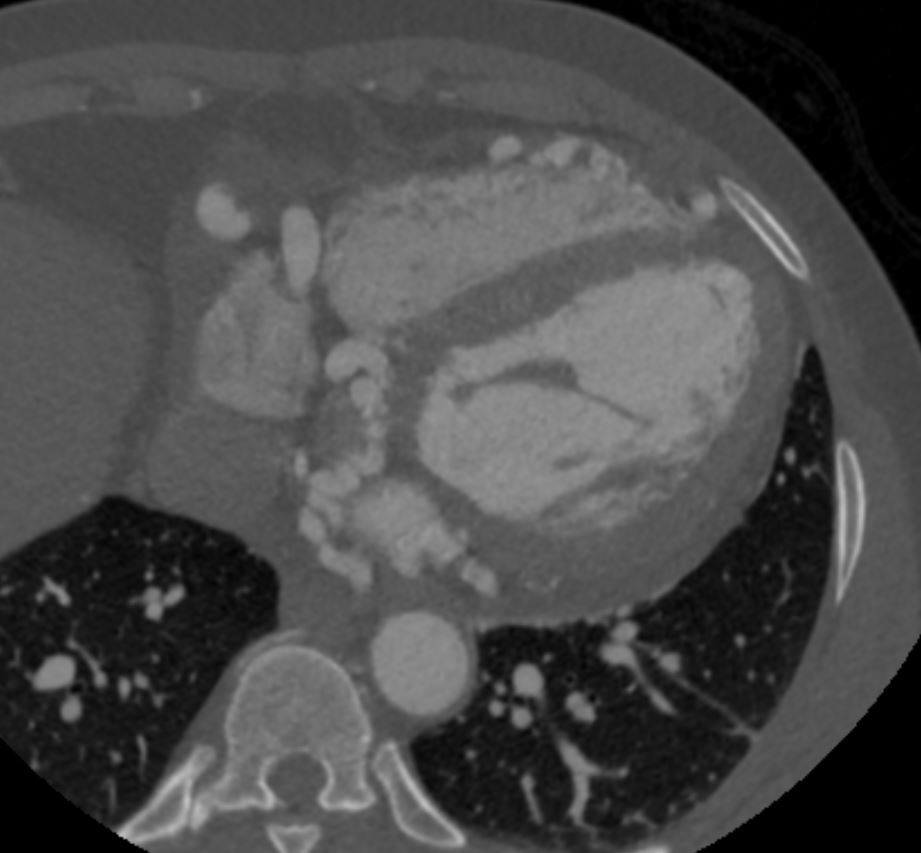
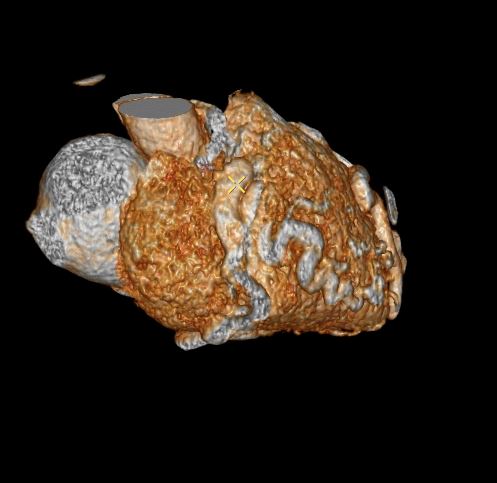
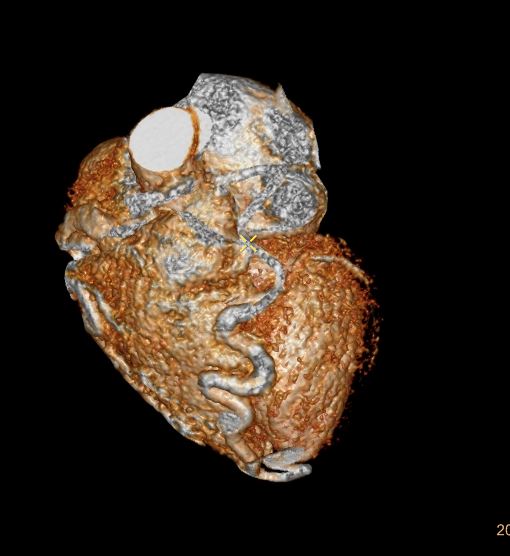
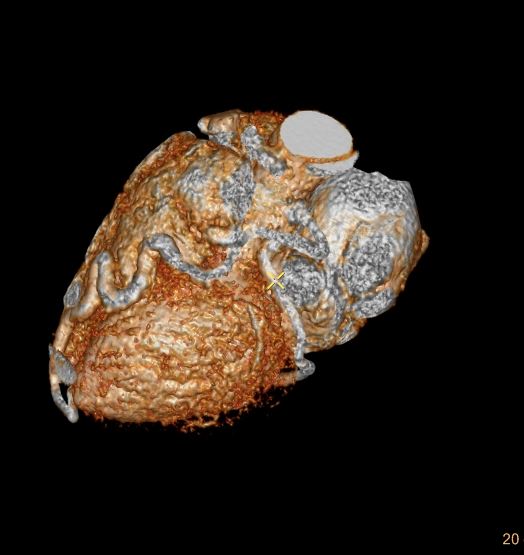
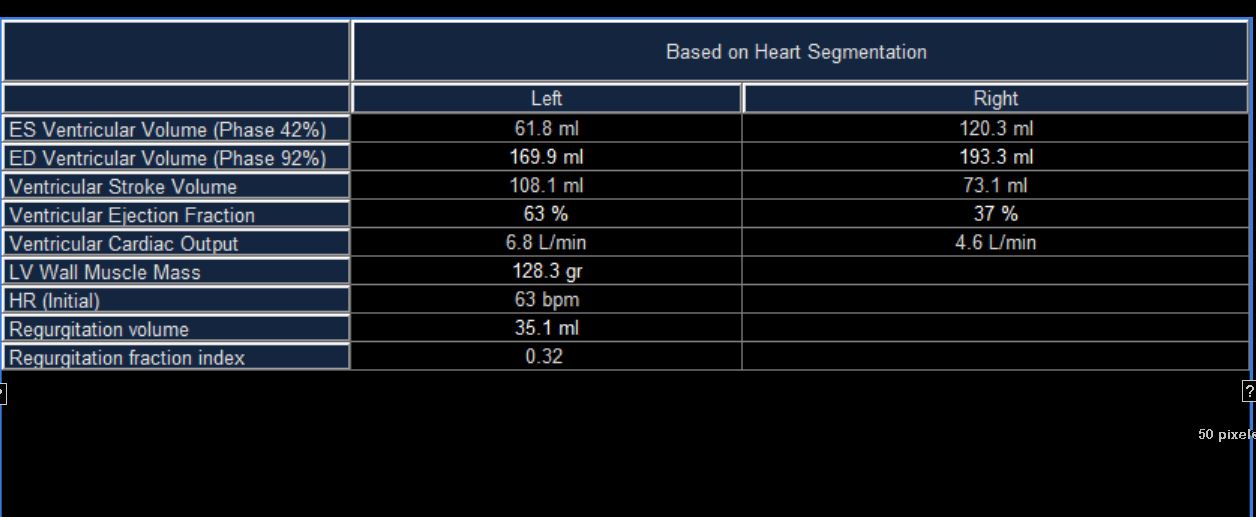
CTEcho at the time
Normal LV size with mildly increased wall thickness; LV
systolic function is normal with estimated LVEF 60%; all walls move normally.
RV size and systolic function are normal.
Severely dilated LA ( 60 ml/m2); RA is moderately dilated.
The pulmonary artery and pulmonary flow are not adequately
evaluated.
Valves appear structurally normal, but there is 2+ MR and 2+ TR;
Estimated PA systolic pressure is 35 mmHg assuming an RA pressure of 3 mmHg. IVC is normal size with normal respiratory variation suggesting normal RA pressure.
No pericardial effusion.
Color flow Doppler of the interventricular septum throughout the
study, but especially on images #82 and #93 demonstrate several
color Doppler continuous signals that are low velocity and are most consistent a coronary-cameral fistula (coronary to RV chamber).
Note that recent Coronary CT Pulmonary Antiogram has demonstrated massive dilatation of the coronary arteries, which would be consistent with the probable presence of coronary -cameral fistula).
Ashley Davidoff thecommonvein.net

Ashley Davidoff thecommonvein.net

Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
Ashley Davidoff thecommonvein.net
