Hallmark findings of Interstitial edema include
- Prerequisites
- Left Atrial Enlargement
- Upper lobe PA:bronchial ratio >1
Characteristic findings of Interstitial edema include
-
- Fuzziness the edges of the blood vessels
- Peribronchial cuffing
- Kerley B lines
- Less commonly
- Kerley A lines
- Kerley C lines
- Effusion – Usually right sided, or dominantly right sided
-

NON-COMPACTION, CHF and interstitial edema
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA, Kerley B lines, and left atrial enlargement.
Prior to implantation of a dual lead pacemaker she had a gated cardiac CT to define the venous anatomy.
The scout film shows an enlarged left atrium and suggestion of LV enlargement.
Lung windows confirmed the presence of prominent interlobular septa and LAE.
Axial soft tissue windows confirmed a diagnosis of non compaction with non compaction thickness (NC) of 15mm and free wall thickness (C) of 6mm resulting an abnormal NC:C ratio of 2.5 (upper limits normal NC:C ratio = 2.3)
Volume measurements showed an end diastolic volume of 217mls, an end systolic volume of 159ccs, a stroke volume of 58ccs with a resulting ejection fraction of 26%.
Following placement of biventricular pacemaker CXR showed resolution of the heart failure, but persistence of the LAE.
Ashley Davidoff MD
NON-COMPACTION, CHF and interstitial edema
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA) Kerley B lines, and left atrial enlargement.
Prior to implantation of a dual lead pacemaker she had a gated cardiac CT to define the venous anatomy.
The scout film shows an enlarged left atrium and suggestion of LV enlargement.
Lung windows confirmed the presence of prominent interlobular septa and LAE.
Axial soft tissue windows confirmed a diagnosis of non compaction with non compaction thickness (NC) of 15mm and free wall thickness (C) of 6mm resulting an abnormal NC:C ratio of 2.5 (upper limits normal NC:C ratio = 2.3)
Volume measurements showed an end diastolic volume of 217mls, an end systolic volume of 159ccs, a stroke volume of 58ccs with a resulting ejection fraction of 26%.
Following placement of biventricular pacemaker CXR showed resolution of the heart failure, but persistence of the LAE.
Ashley Davidoff MD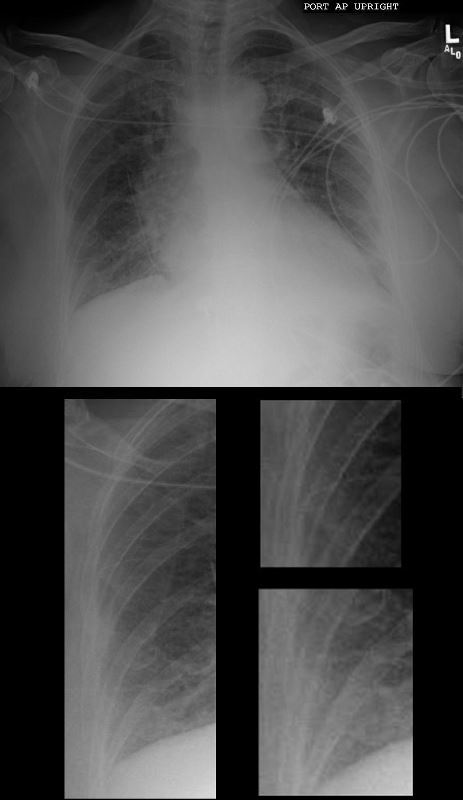
NON-COMPACTION AND CHF
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA) Kerley B lines, and left atrial enlargement.
Ashley Davidoff MD
NON-COMPACTION AND CHF
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA) Kerley B lines, and left atrial enlargement.
Prior to implantation of a dual lead pacemaker she had a gated cardiac CT to define the venous anatomy.
The scout film shows an enlarged left atrium and suggestion of LV enlargement.
Ashley Davidoff MD
MPA UPPER LIMITS NORMAL IN SIZE
NON-COMPACTION AND CHF
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA) Kerley B lines, and left atrial enlargement.
Prior to implantation of a dual lead pacemaker she had a gated cardiac CT to define the venous anatomy.
The scout film shows an enlarged left atrium and suggestion of LV enlargement.
Lung windows confirmed the presence of prominent interlobular septa and LAE with bilateral complex effusions.
Ashley Davidoff MD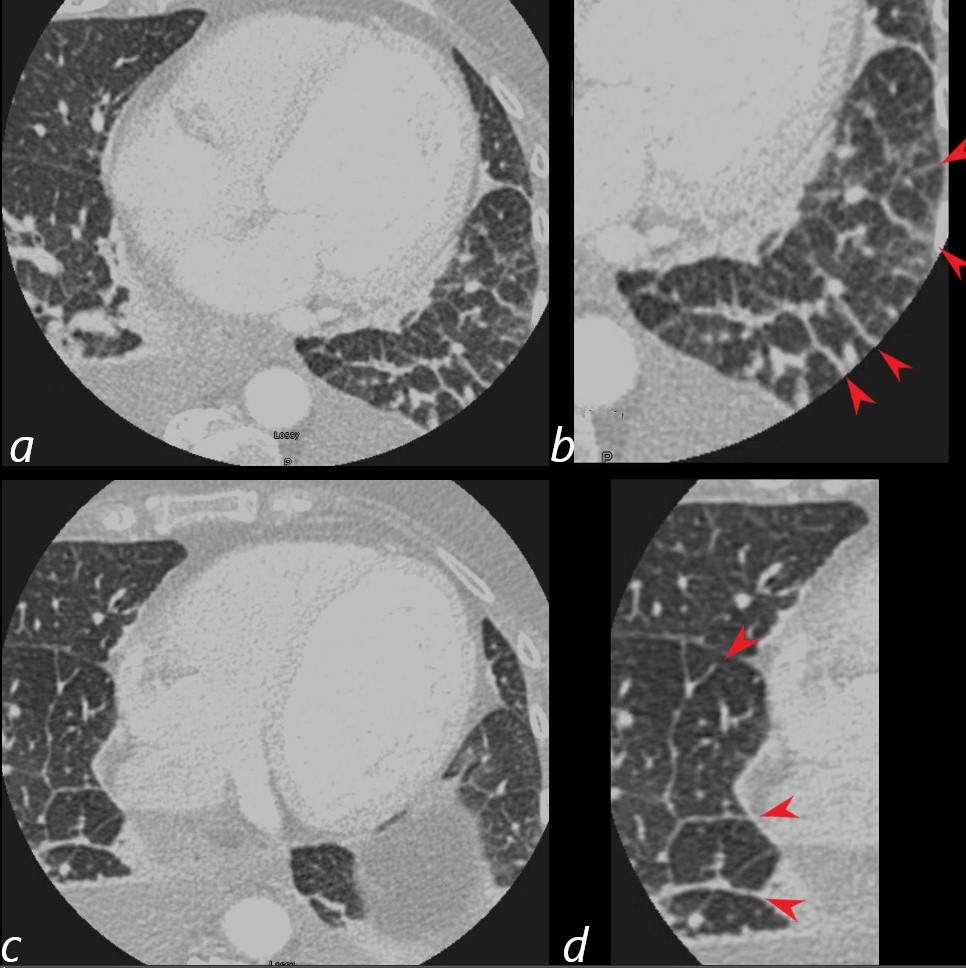
NON-COMPACTION AND CHF
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA) Kerley B lines, and left atrial enlargement.
Prior to implantation of a dual lead pacemaker she had a gated cardiac CT to define the venous anatomy.
The scout film shows an enlarged left atrium and suggestion of LV enlargement.
Lung windows confirmed the presence of prominent interlobular septa and LAE with bilateral complex effusions.
Ashley Davidoff MD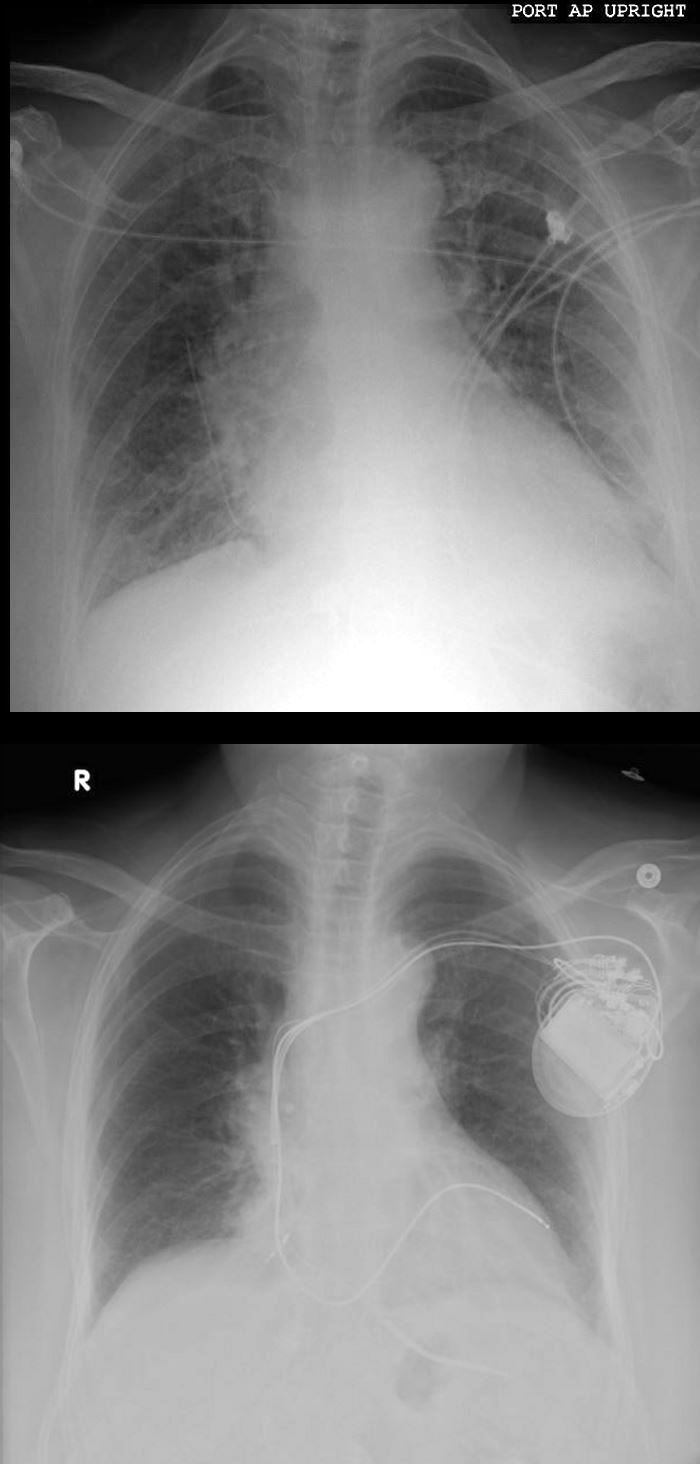
NON-COMPACTION, CHF PRE AND POST BIVENTRICULAR PACEMAKER PLACEMENT
74-year-old female presents in CHF and an echo showing reduced EF (35%) and non-compaction.
Initial CXR shows findings consistent with interstitial edema, (redistribution, fuzzy borders of the vessels and descending RPA) Kerley B lines, and left atrial enlargement.
Volume measurements showed an end diastolic volume of 217mls, an end systolic volume of 159ccs, a stroke volume of 58ccs with a resulting ejection fraction of 26%.
Following placement of biventricular pacemaker CXR showed resolution of the heart failure, but persistence of the LAE.
Ashley Davidoff MD
