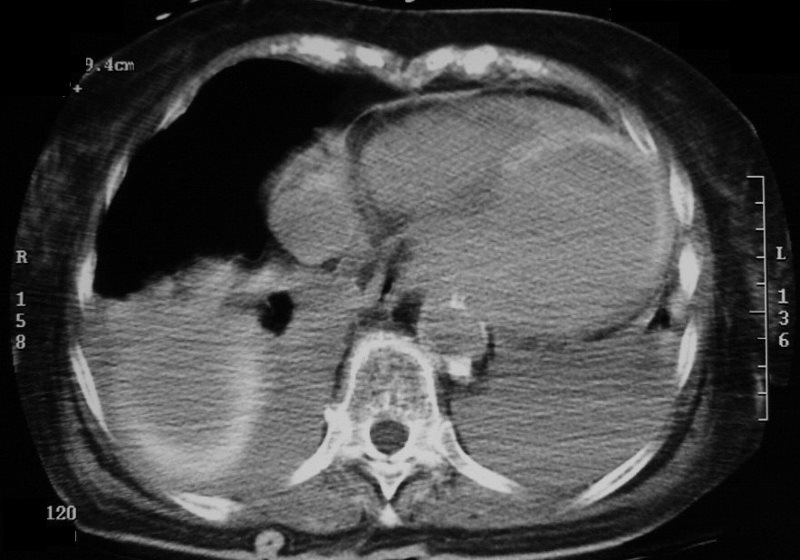
028h 83fF post MI post cath LV Contrast
83-year-old female with a previous history of CHF, CAD, with prior MI 9 years prior presented with chest pain and finding consistent with an acute anterior MI. Peak CK was 3967 and peak troponin was 7.41 A recent echo showed an EF of 10%
Cardiac catheterization showed acute thrombotic occlusion of the LAD, 95% stenosis of the circumflex and complete occlusion of the RCA. The LAD was recanalized, dilated, and stented
At the same time, it was elected to treat a 95% stenosis of the circumflex. During this latter procedure the patient aspirated and required intubation.
During the catheterization her systemic pressure was 140/90, wedge pressure was 10 mmhg (mean) and RV pressure was 30/8 mmHg
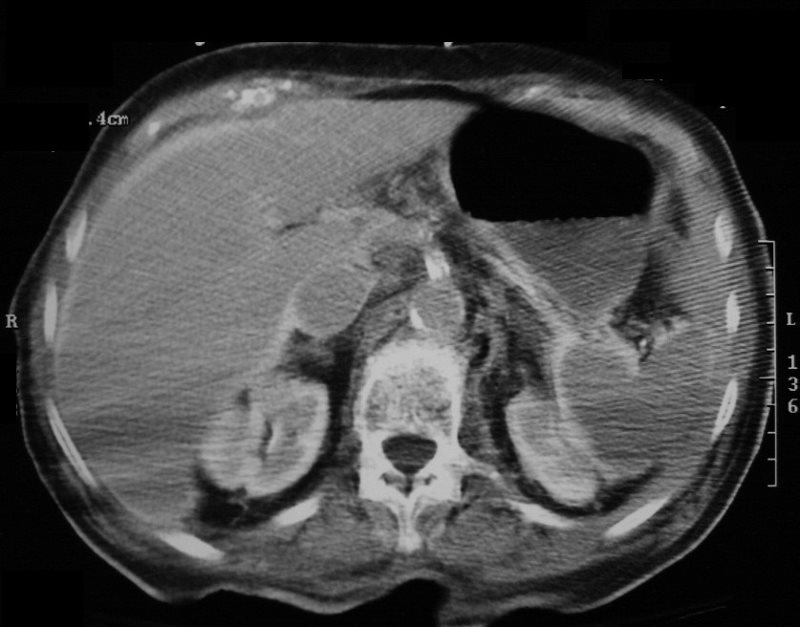
A subsequent ?non contrast? CT following the catheterization showed enhancement of the dilated LV myocardium, left atrial enlargement, bilateral pleural effusions retained contrast in the kidneys splenic capsule, liver capsule. There was severe calcification of the LAD circumflex and the left atrium was enlarged. Moderate sized bilateral pleural effusions were present with compressive atelectasis. At this time, she was in acute on chronic renal failure with findings suggestive of acute tubular necrosis. Cr was 2.4 and BUN was 70 showed
CXR and CT 4 years later showed almost complete resolution of the parenchymal findings and the CT findings except for minimal reticulation and scarring in the subpleural regions

ACUTE MI S/P CATH AND HYPOTENSION
Ashley Davidoff MD
Ashley Davidoff MD
Ashley Davidoff MD
The high density ascites reflect a mechanism of contrast secretion when the kidneys have failed
