Intracranial Hemorrhage
Sumit Karia MD
Copyright 2010
Definition
Intracranial hemorrhage occurs when an intracranial blood vessel is ruptured. This rupture can be caused by trauma, stroke, spontaneous rupture (frequently aneurysms), neoplasms, vasculitidis. It results in accumulation of blood, either within the brain substance (intracereberal intraaxial) or it may collect between the meninges, or above/below them(extraaxial).
Structurally, the intracerebral intraaxial bleeds, extravasation of blood may compress the brain parenchyma and shift structures from the inside. It is characterized by the presence of clotted blood and surrounding edema. Extraaxial hemorrhage results from trauma and may be subdural, extradural, orsubarachnoid in location. A lateral skull fracture most frequently causes a laceration of the middle meningeal artery/vein; its leak results in an epidural hemorrhage hematoma (above the dura). A subdural hematoma can result from trauma as well, and the hematoma will be contained between the the dura and arachnoid.
Clinically, patients may have a variety of symptoms depending on the structures of the brain that are involved. The pathogenesis of the disease is also dependant on the presence or absence of ongoing bleeding. Sensory or motor symptoms commonly associated with a stroke are the signs of a hemorrhagic stroke and the hemorrhagic aspect is important to diagnose because it directs treatment. The clinical presentation of the extraaxial bleeds depend on the size of the hemorrhage, its location, the presence of ongoing hemorrhage. They therefore may present with loss of consciousness, initial or later in the course, with a possibility of a lucid interval while the bleeding develops; headaches, seizures and focal symptoms.
Diagnosis is made by CT or MRI.
Details can be found in their corresponding reviews.
Treatment is dependent on the cause. Surgical evacuation of large hematomas is indicated with the aim of decompression.
Intracerebral CT scan
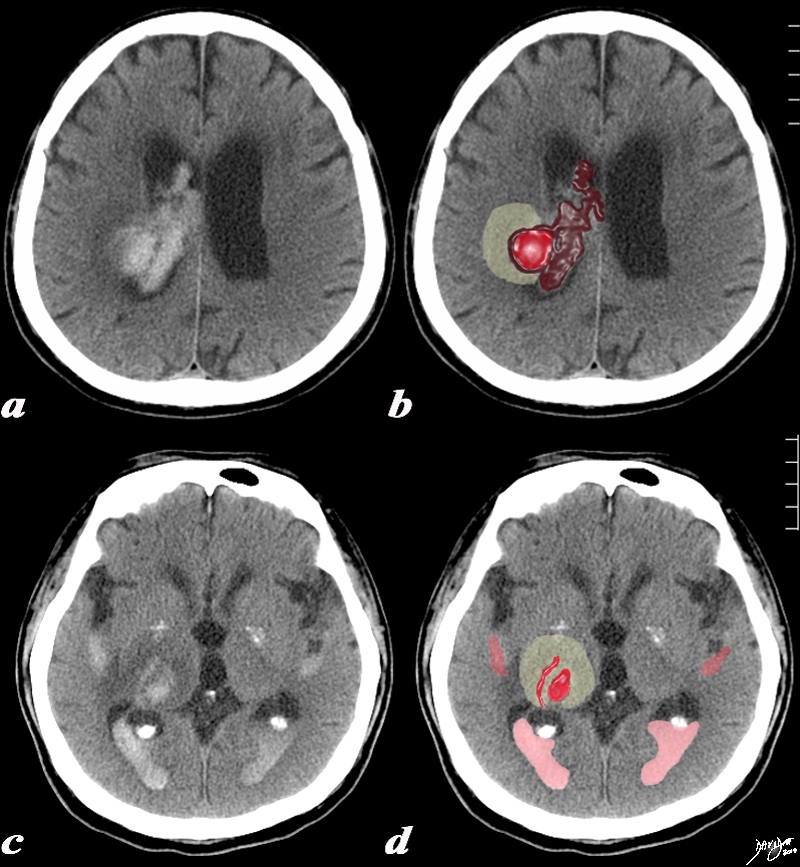
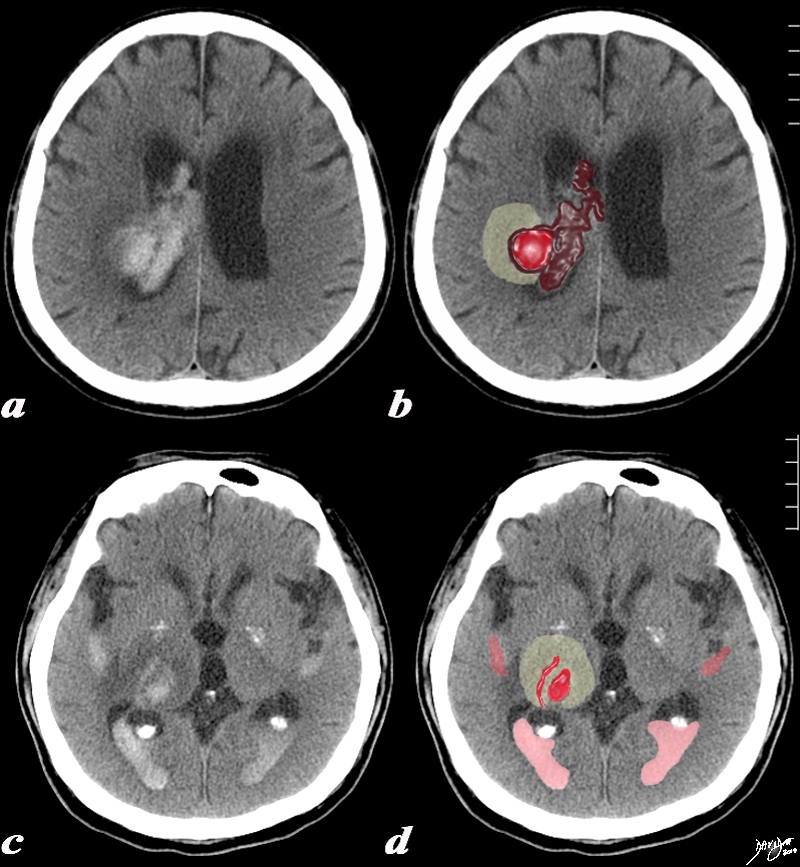
Acute Intracerebral Hemorrhage |
|
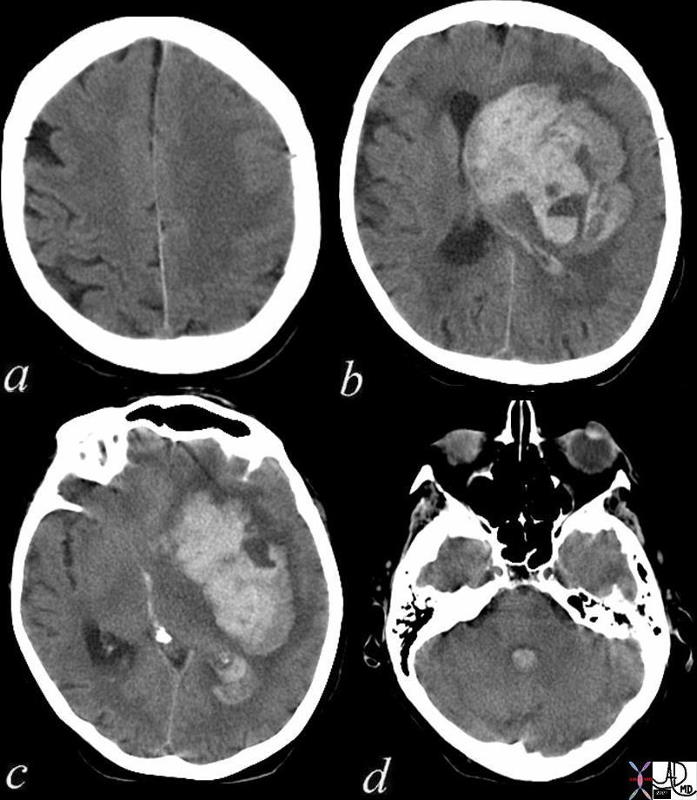
The CT is from a 77year old male with acute neurological deficit The epicenter of the disease is an acute hemorrhage in the right thalamus, bright red in (b,d) with extension of the clot into the ventricle (maroon). There is non clotted blood lying dependently in the occipital horns (dense on c) presenting as a CSF-blood level (light pink on black CSF) in (d). The hemorrhage is surrounded by a rim of edema (light yellow) as seen in b and d.
Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 90461c03.8s
|
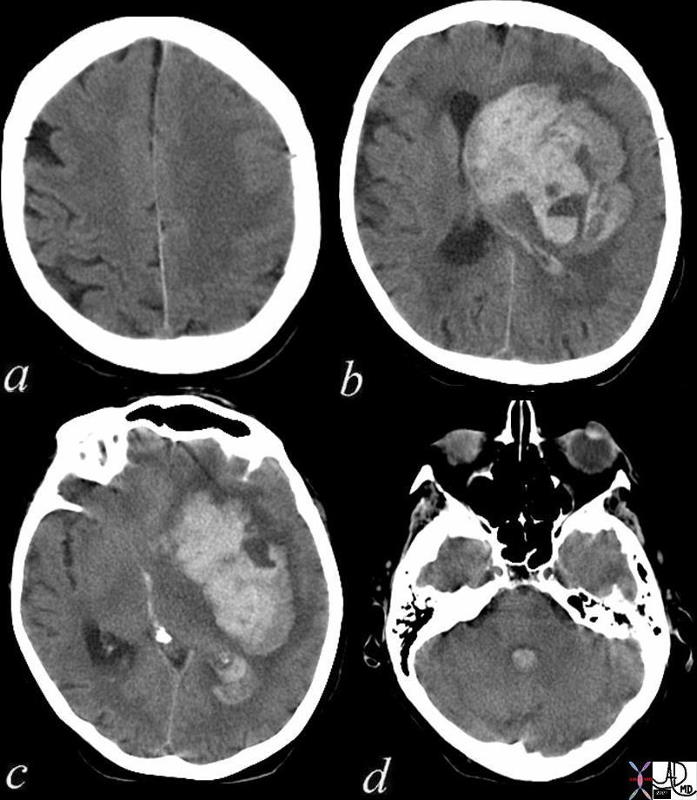
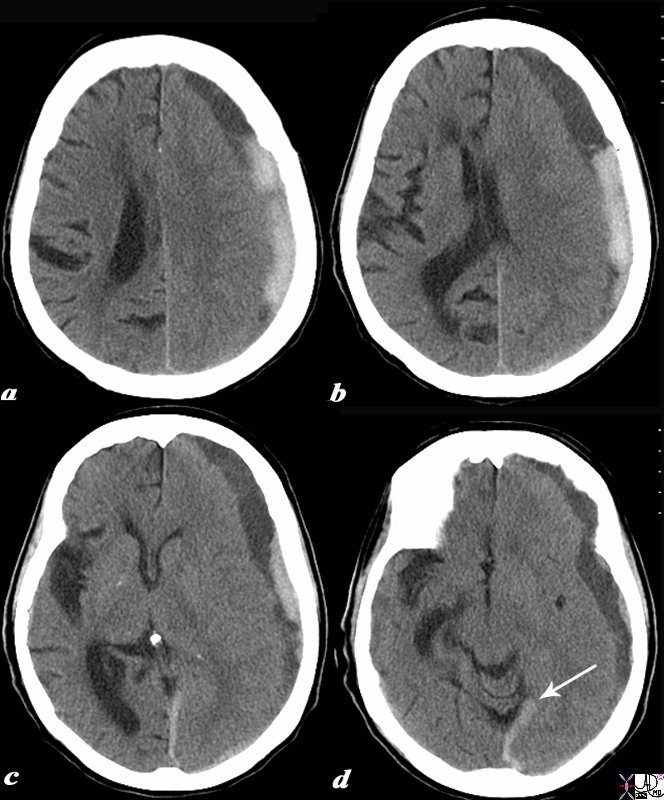
Acute Intracerebral Hemorrhage with Mass Effect and Rupture into the Ventricles –
CT |
|
This CT shows an acute hemorrhagic event originating in the frontoparietal region of the left cerebral hemisphere causing significant mass effect by compressing and displacing the ipsilateral lateral ventricle with significant midline shift. The hemorrhage has ruptured into the ipsilateral lateral ventricle and blood can be seen within the choroid plexus (b) in the posterior horn (c) as well as the 4th ventricle (d). The ipsilateral edema has caused loss of the gray white matter interface in the left parietal lobe
Courtesy Ashley Davidoff MD copyright 2010 72143c01
|
Intracerebral MRI
|
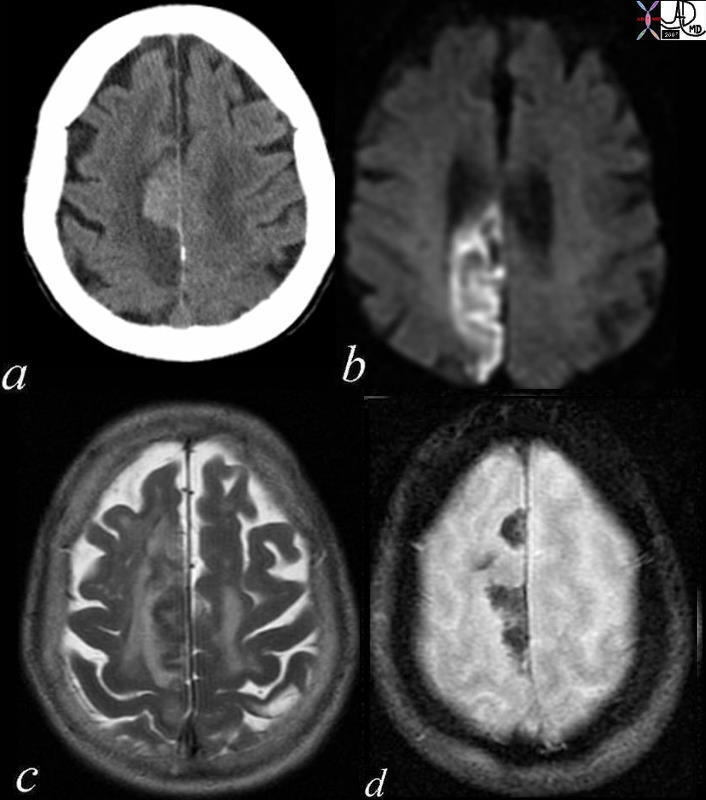
Acute Embolic Infarct High Parietal Region
CT and MRI |
|
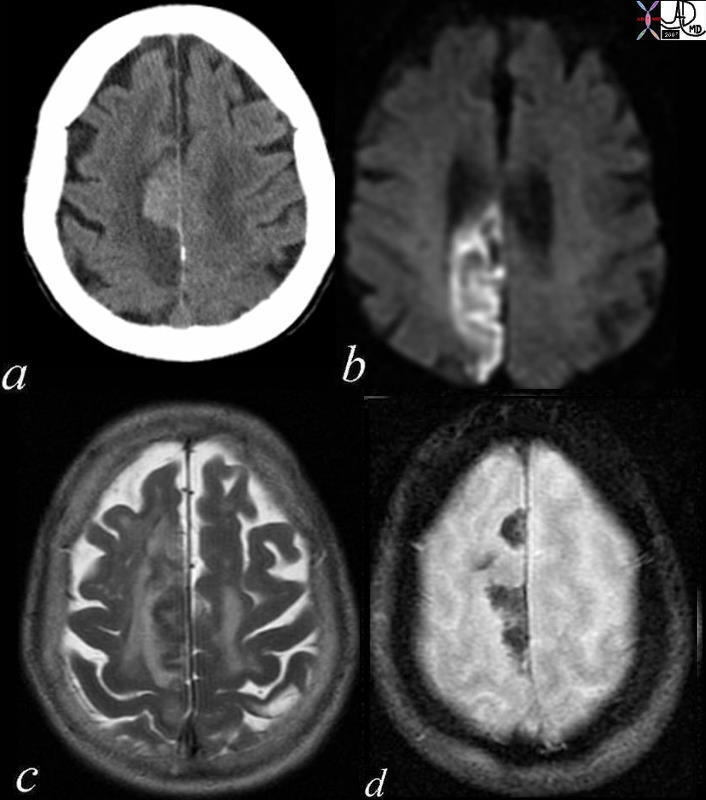
The axial images are from a patient with atrial fibrillation and neurological deficits.
Image a is a CT scan which shows a high density lesion i the vertex of the right pariettal lobe suggesting hemorhagic change.
Image b is a diffusion weighted MRI image at the level of the ventricles which shows a high intensity region in the parieto-occipital region suggesting acute infarction.
Image c is a axial T2 weighted image showing edema in the white matter of the right parietal lobe.
Image is aGRE image showing mixed heterogeneity with probable iron deposition suggesting subacute or chronic hemorhage.
Findings are consistent with old and new multicentric infarcts of the brain likely from the heart caused by atrial fibrillation
Courtesy Ashley Davidoff MD copyright 2010 71239c01
|
Aging the Hemorrhage on MRI
(T1/T2: II, ID, BD, BB, DD (I-iso, D-dark, B-bright)
Hyperacute – minutes to hours
T1 – hematoma (deoxyHb) dark => isointense
T2 – hematoma (deoxyHb) dark=> isointense
Acute – 0-2 days
deoxyhemoglobin is in intact RBCs with surrounding edema
T1- hematoma isointense, edema dark
T2 – hematoma dark, edema bright
Subacute – 2-14 days
deoxyhemoglobin changes to methemoglobin from outer to inner
T1 – outer core bright
T2 – outer core bright due to shortened T1, longer T2
Chronic – 14 days
hemosiderin laden macrophages at periphery
T1 – inner core bright, rim dark
T2 – inner core bright, rim has low dark
Chronic – months later
hemosiderin laden macrophages at periphery
T1- mostly iso-/dark, rim is dark
T2- markedly dark rim – “blooms” with greater T2-weighting
|
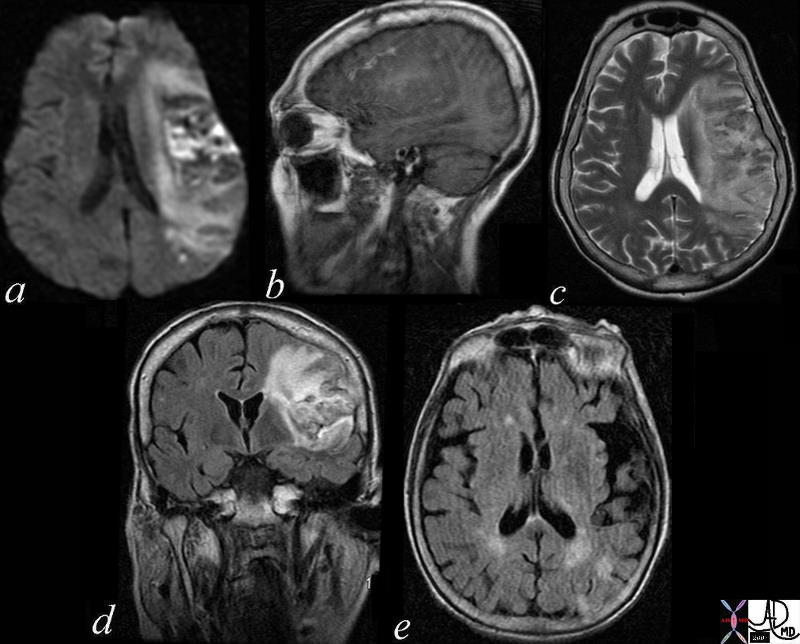
Subacute Hemorrhagic Infarct of the Parietal Lobe MRI |
|
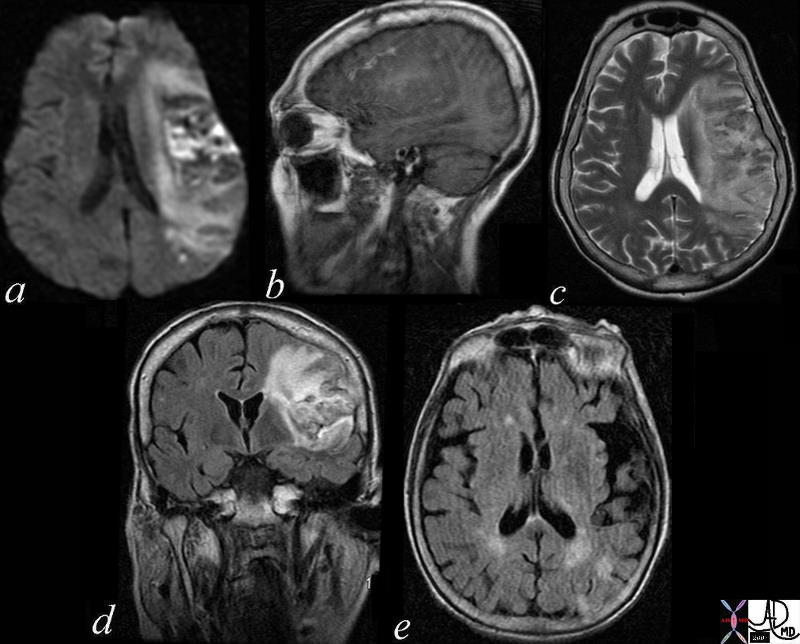
The series of MRI images from a 70 year old male who by history suffered a stroke 1 month ago and has new onset symptoms. the series of images reveal complex changes of a subacute hemorrhagic infarct. Image a is from a DWI sequence and it shows a heterogenous increase in signal some of which represents T2 shine throughand sopme of which is bright raising the question on an acute on subacute entity. Image b is a sagittal T1 weighted image which shows areas of vague increase in density suggesting hemorrhage. Image c is a T2weighted sequence and shows some increase in water but the granular low intensity suggests hemosiderin deposit. Image d is FLAIR sequence showing increase brightness to the lesion in the left parietal lobe and image e is an axial FLAIR sequence The findings suggest extensive infarct in the left MCA territory which has mild mass effect on ventricles with petechial hemorrhage as seen on T2 and FLAIR and hyperintense T2 shine through on diffusion weighted images The punctate areas in left parietal lobe with restricted area of diffusion raises the question of a recent small infarct less bright regions on DWI suggests a subacute hemorrhagic infarct.
Courtesy Ashley Davidoff MD copyright 2010 71000c03
|
Extraaxial Hemorrhage
Subdural Hematoma

Bilateral Acute Subdural Hematomas |
|
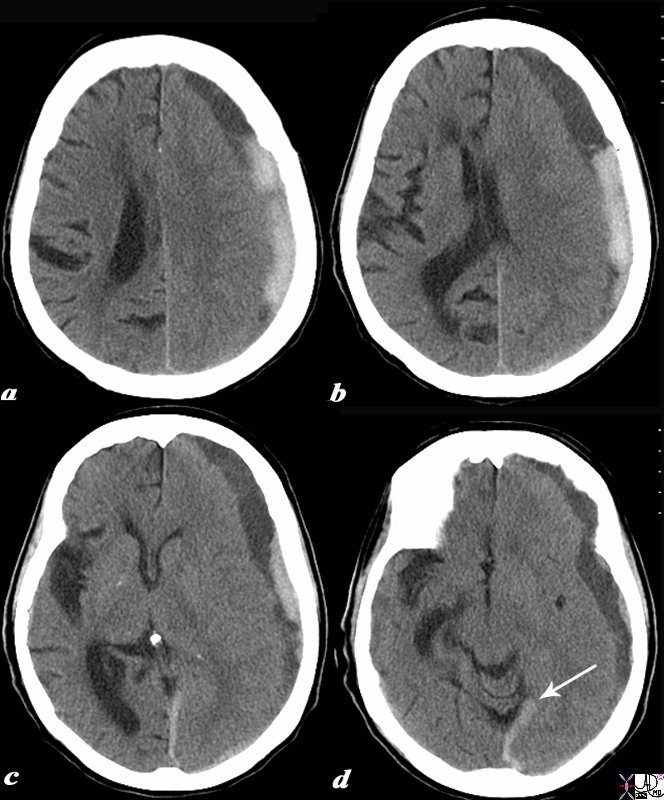
In this patient the non contrast CTscan reveals small bilateral subdural hematomas . In the left frontal region there is a subgaleal hematoma and underlying the hematoma there is a small hyperdense subdural hematoma in the region of the Sylvian fissure. A contracoup injury manifesting also as a subdural hematoma is seen in the right posterior parietal region. There are linear hyperdensities overlying the frontal lobes bilaterally that may represent small acute hemorrhages as well.
Image Courtesy Davidoff MD 70000.800
|
Acute on Chronic Subdural Hemorrhage
CTscan |
|
The CTscan without contrast is from a 88 year old male who has a history of falling who recently sustained head trauma and was complaining of a severe headache. The scan shows a collection in the left fronto-parietal collection with both high density and low density components. The left frontoparietal collection is subdural hematoma since it crosses suture lines, with the outer border conforming to the shape of the skull . Associated findings include flattening of the right sided frontal sulci and parietal sulci (a,b,c) as well as shift of the midline structures typified by the displacement of the septum pellucidum (b) and effacement of the left lateral ventricle(a,b,c). In image d, the hemorrhage has extended into the leaves of the posterior falx and inferior sagittal sinus (white arrow). The combination of low density and high density fluid in the subdural collection is consistent with an acute on chronic accumulation
Courtesy Ashley Davidoff MD Copyright 2010 97737c.8s
|
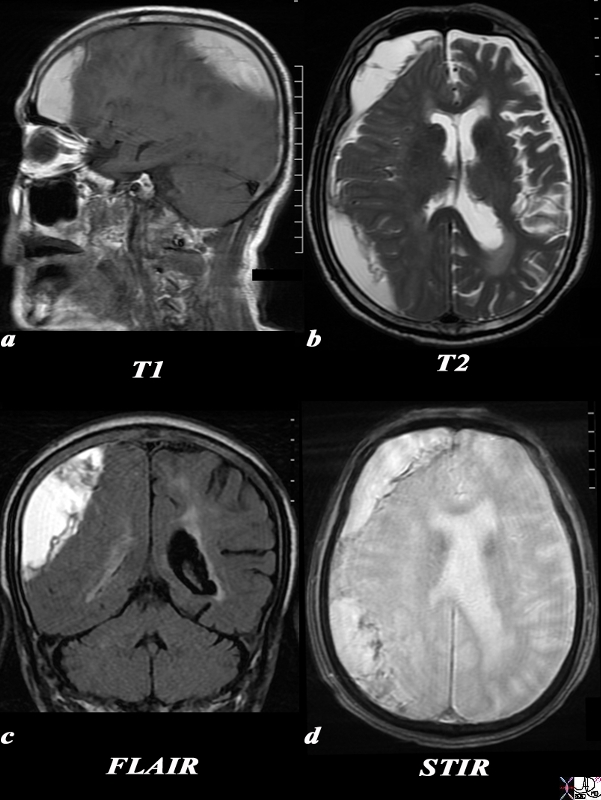
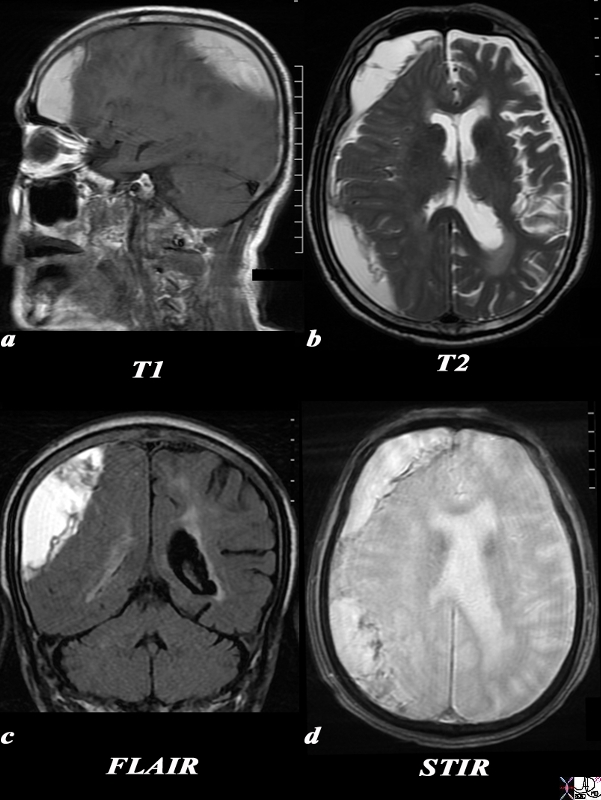
Acute Subdural MRI |
|
The MRI scan is of a 75year old male and was performed following trauma and change in level of consciousness. The MRI confirms the presence of a large collection overlying the right temperoparietal region . The collection is large and crosses the region of the skull sutures placing it in the subdural space The T1 weighted image (a) shows a hyperintense collection suggesting the presence of methemoglobin. The T2 sequence (b) and FLAIR sequence is also hyperintense suggesting the presence of extracellular methemoglobin. The STIR sequence (c) and to lesser extent the T2 sequence show early rim blackening suggesting the presence of hemosiderin. The effacement of the right lateral ventricle seen on the axila T2 weighted image (b), the coronal FLAIR image (c) and the STIR image (d) suggest mass effect These findings suggest a diagnosis of a large subacute subdural hematoma. With mild mass effect and mild midline shift c
Courtesy Ashley Davidoff MD Copyright 2010 90443c.8S
|
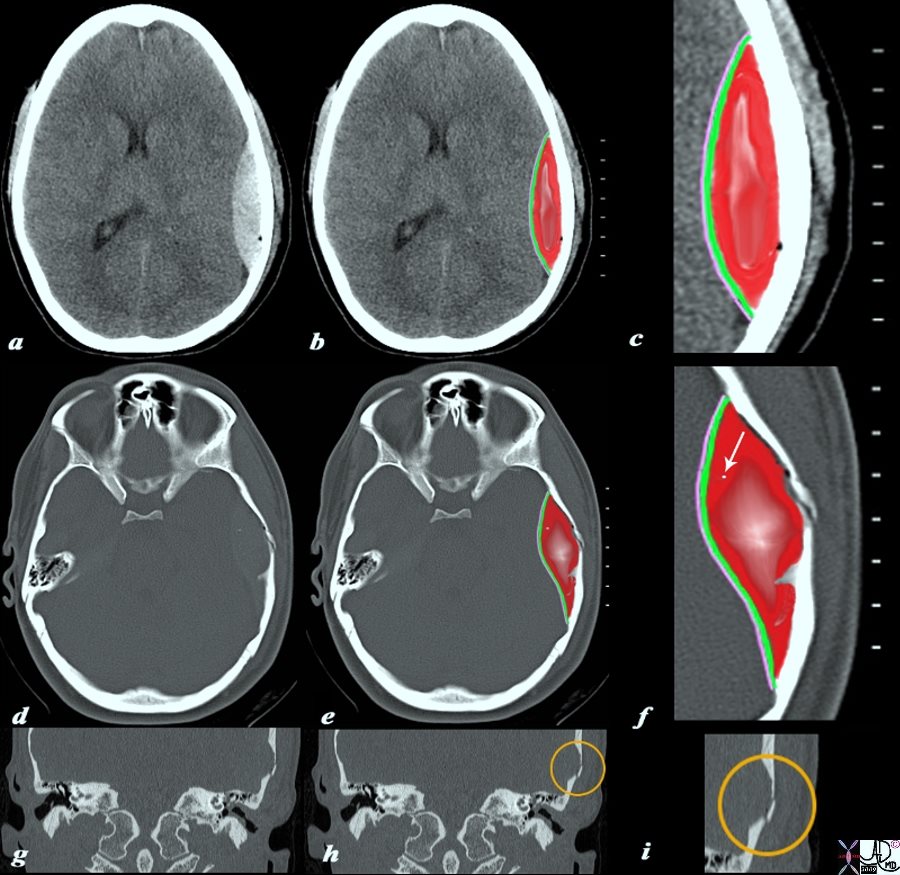
Extradural or Epidural Hemorrhage
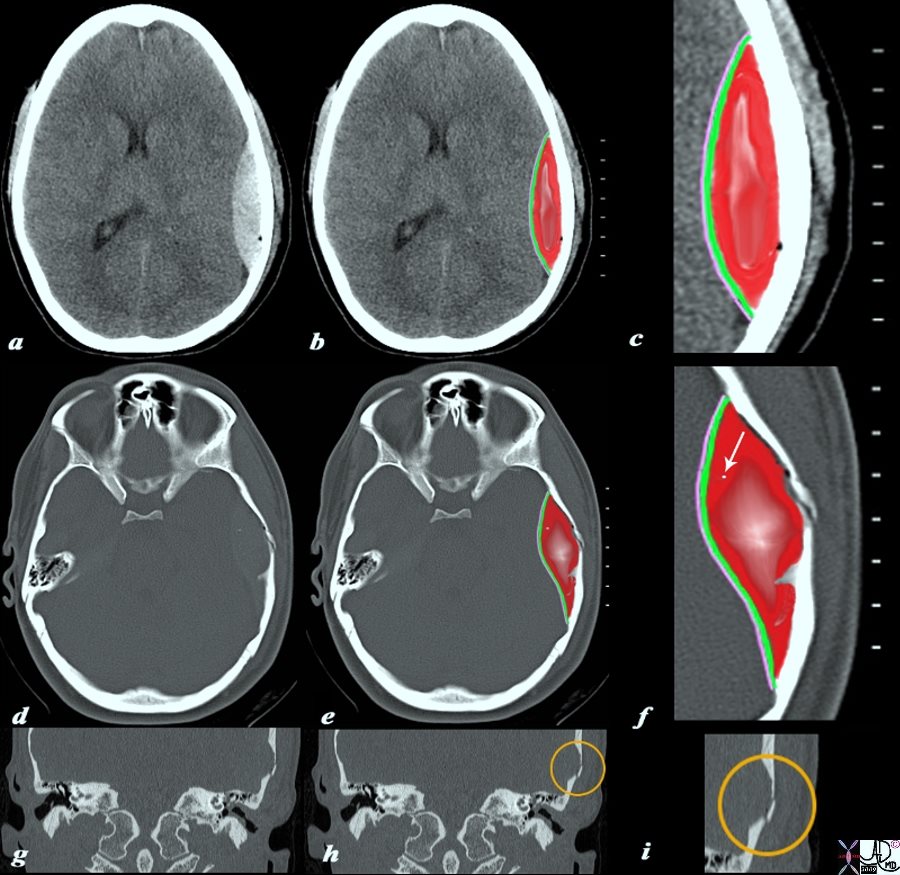
Acute Epidural Hematoma
CTscan |
|
The CTscan without contrast is from a 19 year old male who sustained head trauma and who is complaining of a severe headache. The scan shows a high density lenticular shaped hematoma (a,b,c),. The right parietal collection is an extradural or epidural hematoma, with the outer border conforming to the shape of the skull and lined by the bone) and the inner border lined by two layers of dura (green c,f) and the arachnoid (pink c,f). There are bubbles of air scattered along the inner bone surface (black bubbles best seen on the magnified views (c, f) a tiny fragment of bone (white arrow in f) but seen on images d, and e as a white speck. The fracture of the temporal bone is ringed in orange on the coronal reconstructions of the axial views (h,i)
Courtesy Ashley Davidoff MD Copyright 2010 98056c04.9s
|
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] =>
[nodeName] => table
[nodeValue] =>
Acute Epidural Hematoma
CTscan
The CTscan without contrast is from a 19 year old male who sustained head trauma and who is complaining of a severe headache. The scan shows a high density lenticular shaped hematoma (a,b,c),. The right parietal collection is an extradural or epidural hematoma, with the outer border conforming to the shape of the skull and lined by the bone) and the inner border lined by two layers of dura (green c,f) and the arachnoid (pink c,f). There are bubbles of air scattered along the inner bone surface (black bubbles best seen on the magnified views (c, f) a tiny fragment of bone (white arrow in f) but seen on images d, and e as a white speck. The fracture of the temporal bone is ringed in orange on the coronal reconstructions of the axial views (h,i)
Courtesy Ashley Davidoff MD Copyright 2010 98056c04.9s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Acute Epidural Hematoma
CTscan
The CTscan without contrast is from a 19 year old male who sustained head trauma and who is complaining of a severe headache. The scan shows a high density lenticular shaped hematoma (a,b,c),. The right parietal collection is an extradural or epidural hematoma, with the outer border conforming to the shape of the skull and lined by the bone) and the inner border lined by two layers of dura (green c,f) and the arachnoid (pink c,f). There are bubbles of air scattered along the inner bone surface (black bubbles best seen on the magnified views (c, f) a tiny fragment of bone (white arrow in f) but seen on images d, and e as a white speck. The fracture of the temporal bone is ringed in orange on the coronal reconstructions of the axial views (h,i)
Courtesy Ashley Davidoff MD Copyright 2010 98056c04.9s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The CTscan without contrast is from a 19 year old male who sustained head trauma and who is complaining of a severe headache. The scan shows a high density lenticular shaped hematoma (a,b,c),. The right parietal collection is an extradural or epidural hematoma, with the outer border conforming to the shape of the skull and lined by the bone) and the inner border lined by two layers of dura (green c,f) and the arachnoid (pink c,f). There are bubbles of air scattered along the inner bone surface (black bubbles best seen on the magnified views (c, f) a tiny fragment of bone (white arrow in f) but seen on images d, and e as a white speck. The fracture of the temporal bone is ringed in orange on the coronal reconstructions of the axial views (h,i)
Courtesy Ashley Davidoff MD Copyright 2010 98056c04.9s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The CTscan without contrast is from a 19 year old male who sustained head trauma and who is complaining of a severe headache. The scan shows a high density lenticular shaped hematoma (a,b,c),. The right parietal collection is an extradural or epidural hematoma, with the outer border conforming to the shape of the skull and lined by the bone) and the inner border lined by two layers of dura (green c,f) and the arachnoid (pink c,f). There are bubbles of air scattered along the inner bone surface (black bubbles best seen on the magnified views (c, f) a tiny fragment of bone (white arrow in f) but seen on images d, and e as a white speck. The fracture of the temporal bone is ringed in orange on the coronal reconstructions of the axial views (h,i)
Courtesy Ashley Davidoff MD Copyright 2010 98056c04.9s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Acute Epidural Hematoma
CTscan
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Acute Epidural Hematoma
CTscan
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Acute Subdural MRI
The MRI scan is of a 75year old male and was performed following trauma and change in level of consciousness. The MRI confirms the presence of a large collection overlying the right temperoparietal region . The collection is large and crosses the region of the skull sutures placing it in the subdural space The T1 weighted image (a) shows a hyperintense collection suggesting the presence of methemoglobin. The T2 sequence (b) and FLAIR sequence is also hyperintense suggesting the presence of extracellular methemoglobin. The STIR sequence (c) and to lesser extent the T2 sequence show early rim blackening suggesting the presence of hemosiderin. The effacement of the right lateral ventricle seen on the axila T2 weighted image (b), the coronal FLAIR image (c) and the STIR image (d) suggest mass effect These findings suggest a diagnosis of a large subacute subdural hematoma. With mild mass effect and mild midline shift c
Courtesy Ashley Davidoff MD Copyright 2010 90443c.8S
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Acute Subdural MRI
The MRI scan is of a 75year old male and was performed following trauma and change in level of consciousness. The MRI confirms the presence of a large collection overlying the right temperoparietal region . The collection is large and crosses the region of the skull sutures placing it in the subdural space The T1 weighted image (a) shows a hyperintense collection suggesting the presence of methemoglobin. The T2 sequence (b) and FLAIR sequence is also hyperintense suggesting the presence of extracellular methemoglobin. The STIR sequence (c) and to lesser extent the T2 sequence show early rim blackening suggesting the presence of hemosiderin. The effacement of the right lateral ventricle seen on the axila T2 weighted image (b), the coronal FLAIR image (c) and the STIR image (d) suggest mass effect These findings suggest a diagnosis of a large subacute subdural hematoma. With mild mass effect and mild midline shift c
Courtesy Ashley Davidoff MD Copyright 2010 90443c.8S
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The MRI scan is of a 75year old male and was performed following trauma and change in level of consciousness. The MRI confirms the presence of a large collection overlying the right temperoparietal region . The collection is large and crosses the region of the skull sutures placing it in the subdural space The T1 weighted image (a) shows a hyperintense collection suggesting the presence of methemoglobin. The T2 sequence (b) and FLAIR sequence is also hyperintense suggesting the presence of extracellular methemoglobin. The STIR sequence (c) and to lesser extent the T2 sequence show early rim blackening suggesting the presence of hemosiderin. The effacement of the right lateral ventricle seen on the axila T2 weighted image (b), the coronal FLAIR image (c) and the STIR image (d) suggest mass effect These findings suggest a diagnosis of a large subacute subdural hematoma. With mild mass effect and mild midline shift c
Courtesy Ashley Davidoff MD Copyright 2010 90443c.8S
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The MRI scan is of a 75year old male and was performed following trauma and change in level of consciousness. The MRI confirms the presence of a large collection overlying the right temperoparietal region . The collection is large and crosses the region of the skull sutures placing it in the subdural space The T1 weighted image (a) shows a hyperintense collection suggesting the presence of methemoglobin. The T2 sequence (b) and FLAIR sequence is also hyperintense suggesting the presence of extracellular methemoglobin. The STIR sequence (c) and to lesser extent the T2 sequence show early rim blackening suggesting the presence of hemosiderin. The effacement of the right lateral ventricle seen on the axila T2 weighted image (b), the coronal FLAIR image (c) and the STIR image (d) suggest mass effect These findings suggest a diagnosis of a large subacute subdural hematoma. With mild mass effect and mild midline shift c
Courtesy Ashley Davidoff MD Copyright 2010 90443c.8S
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Acute Subdural MRI
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Acute Subdural MRI
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Acute on Chronic Subdural Hemorrhage
CTscan
The CTscan without contrast is from a 88 year old male who has a history of falling who recently sustained head trauma and was complaining of a severe headache. The scan shows a collection in the left fronto-parietal collection with both high density and low density components. The left frontoparietal collection is subdural hematoma since it crosses suture lines, with the outer border conforming to the shape of the skull . Associated findings include flattening of the right sided frontal sulci and parietal sulci (a,b,c) as well as shift of the midline structures typified by the displacement of the septum pellucidum (b) and effacement of the left lateral ventricle(a,b,c). In image d, the hemorrhage has extended into the leaves of the posterior falx and inferior sagittal sinus (white arrow). The combination of low density and high density fluid in the subdural collection is consistent with an acute on chronic accumulation
Courtesy Ashley Davidoff MD Copyright 2010 97737c.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Acute on Chronic Subdural Hemorrhage
CTscan
The CTscan without contrast is from a 88 year old male who has a history of falling who recently sustained head trauma and was complaining of a severe headache. The scan shows a collection in the left fronto-parietal collection with both high density and low density components. The left frontoparietal collection is subdural hematoma since it crosses suture lines, with the outer border conforming to the shape of the skull . Associated findings include flattening of the right sided frontal sulci and parietal sulci (a,b,c) as well as shift of the midline structures typified by the displacement of the septum pellucidum (b) and effacement of the left lateral ventricle(a,b,c). In image d, the hemorrhage has extended into the leaves of the posterior falx and inferior sagittal sinus (white arrow). The combination of low density and high density fluid in the subdural collection is consistent with an acute on chronic accumulation
Courtesy Ashley Davidoff MD Copyright 2010 97737c.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The CTscan without contrast is from a 88 year old male who has a history of falling who recently sustained head trauma and was complaining of a severe headache. The scan shows a collection in the left fronto-parietal collection with both high density and low density components. The left frontoparietal collection is subdural hematoma since it crosses suture lines, with the outer border conforming to the shape of the skull . Associated findings include flattening of the right sided frontal sulci and parietal sulci (a,b,c) as well as shift of the midline structures typified by the displacement of the septum pellucidum (b) and effacement of the left lateral ventricle(a,b,c). In image d, the hemorrhage has extended into the leaves of the posterior falx and inferior sagittal sinus (white arrow). The combination of low density and high density fluid in the subdural collection is consistent with an acute on chronic accumulation
Courtesy Ashley Davidoff MD Copyright 2010 97737c.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The CTscan without contrast is from a 88 year old male who has a history of falling who recently sustained head trauma and was complaining of a severe headache. The scan shows a collection in the left fronto-parietal collection with both high density and low density components. The left frontoparietal collection is subdural hematoma since it crosses suture lines, with the outer border conforming to the shape of the skull . Associated findings include flattening of the right sided frontal sulci and parietal sulci (a,b,c) as well as shift of the midline structures typified by the displacement of the septum pellucidum (b) and effacement of the left lateral ventricle(a,b,c). In image d, the hemorrhage has extended into the leaves of the posterior falx and inferior sagittal sinus (white arrow). The combination of low density and high density fluid in the subdural collection is consistent with an acute on chronic accumulation
Courtesy Ashley Davidoff MD Copyright 2010 97737c.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Acute on Chronic Subdural Hemorrhage
CTscan
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Acute on Chronic Subdural Hemorrhage
CTscan
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Bilateral Acute Subdural Hematomas
In this patient the non contrast CTscan reveals small bilateral subdural hematomas . In the left frontal region there is a subgaleal hematoma and underlying the hematoma there is a small hyperdense subdural hematoma in the region of the Sylvian fissure. A contracoup injury manifesting also as a subdural hematoma is seen in the right posterior parietal region. There are linear hyperdensities overlying the frontal lobes bilaterally that may represent small acute hemorrhages as well.
Image Courtesy Davidoff MD 70000.800
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Bilateral Acute Subdural Hematomas
In this patient the non contrast CTscan reveals small bilateral subdural hematomas . In the left frontal region there is a subgaleal hematoma and underlying the hematoma there is a small hyperdense subdural hematoma in the region of the Sylvian fissure. A contracoup injury manifesting also as a subdural hematoma is seen in the right posterior parietal region. There are linear hyperdensities overlying the frontal lobes bilaterally that may represent small acute hemorrhages as well.
Image Courtesy Davidoff MD 70000.800
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
In this patient the non contrast CTscan reveals small bilateral subdural hematomas . In the left frontal region there is a subgaleal hematoma and underlying the hematoma there is a small hyperdense subdural hematoma in the region of the Sylvian fissure. A contracoup injury manifesting also as a subdural hematoma is seen in the right posterior parietal region. There are linear hyperdensities overlying the frontal lobes bilaterally that may represent small acute hemorrhages as well.
Image Courtesy Davidoff MD 70000.800
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
In this patient the non contrast CTscan reveals small bilateral subdural hematomas . In the left frontal region there is a subgaleal hematoma and underlying the hematoma there is a small hyperdense subdural hematoma in the region of the Sylvian fissure. A contracoup injury manifesting also as a subdural hematoma is seen in the right posterior parietal region. There are linear hyperdensities overlying the frontal lobes bilaterally that may represent small acute hemorrhages as well.
Image Courtesy Davidoff MD 70000.800
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Bilateral Acute Subdural Hematomas
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Bilateral Acute Subdural Hematomas
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Subacute Hemorrhagic Infarct of the Parietal Lobe MRI
The series of MRI images from a 70 year old male who by history suffered a stroke 1 month ago and has new onset symptoms. the series of images reveal complex changes of a subacute hemorrhagic infarct. Image a is from a DWI sequence and it shows a heterogenous increase in signal some of which represents T2 shine throughand sopme of which is bright raising the question on an acute on subacute entity. Image b is a sagittal T1 weighted image which shows areas of vague increase in density suggesting hemorrhage. Image c is a T2weighted sequence and shows some increase in water but the granular low intensity suggests hemosiderin deposit. Image d is FLAIR sequence showing increase brightness to the lesion in the left parietal lobe and image e is an axial FLAIR sequence The findings suggest extensive infarct in the left MCA territory which has mild mass effect on ventricles with petechial hemorrhage as seen on T2 and FLAIR and hyperintense T2 shine through on diffusion weighted images The punctate areas in left parietal lobe with restricted area of diffusion raises the question of a recent small infarct less bright regions on DWI suggests a subacute hemorrhagic infarct.
Courtesy Ashley Davidoff MD copyright 2010 71000c03
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Subacute Hemorrhagic Infarct of the Parietal Lobe MRI
The series of MRI images from a 70 year old male who by history suffered a stroke 1 month ago and has new onset symptoms. the series of images reveal complex changes of a subacute hemorrhagic infarct. Image a is from a DWI sequence and it shows a heterogenous increase in signal some of which represents T2 shine throughand sopme of which is bright raising the question on an acute on subacute entity. Image b is a sagittal T1 weighted image which shows areas of vague increase in density suggesting hemorrhage. Image c is a T2weighted sequence and shows some increase in water but the granular low intensity suggests hemosiderin deposit. Image d is FLAIR sequence showing increase brightness to the lesion in the left parietal lobe and image e is an axial FLAIR sequence The findings suggest extensive infarct in the left MCA territory which has mild mass effect on ventricles with petechial hemorrhage as seen on T2 and FLAIR and hyperintense T2 shine through on diffusion weighted images The punctate areas in left parietal lobe with restricted area of diffusion raises the question of a recent small infarct less bright regions on DWI suggests a subacute hemorrhagic infarct.
Courtesy Ashley Davidoff MD copyright 2010 71000c03
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The series of MRI images from a 70 year old male who by history suffered a stroke 1 month ago and has new onset symptoms. the series of images reveal complex changes of a subacute hemorrhagic infarct. Image a is from a DWI sequence and it shows a heterogenous increase in signal some of which represents T2 shine throughand sopme of which is bright raising the question on an acute on subacute entity. Image b is a sagittal T1 weighted image which shows areas of vague increase in density suggesting hemorrhage. Image c is a T2weighted sequence and shows some increase in water but the granular low intensity suggests hemosiderin deposit. Image d is FLAIR sequence showing increase brightness to the lesion in the left parietal lobe and image e is an axial FLAIR sequence The findings suggest extensive infarct in the left MCA territory which has mild mass effect on ventricles with petechial hemorrhage as seen on T2 and FLAIR and hyperintense T2 shine through on diffusion weighted images The punctate areas in left parietal lobe with restricted area of diffusion raises the question of a recent small infarct less bright regions on DWI suggests a subacute hemorrhagic infarct.
Courtesy Ashley Davidoff MD copyright 2010 71000c03
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The series of MRI images from a 70 year old male who by history suffered a stroke 1 month ago and has new onset symptoms. the series of images reveal complex changes of a subacute hemorrhagic infarct. Image a is from a DWI sequence and it shows a heterogenous increase in signal some of which represents T2 shine throughand sopme of which is bright raising the question on an acute on subacute entity. Image b is a sagittal T1 weighted image which shows areas of vague increase in density suggesting hemorrhage. Image c is a T2weighted sequence and shows some increase in water but the granular low intensity suggests hemosiderin deposit. Image d is FLAIR sequence showing increase brightness to the lesion in the left parietal lobe and image e is an axial FLAIR sequence The findings suggest extensive infarct in the left MCA territory which has mild mass effect on ventricles with petechial hemorrhage as seen on T2 and FLAIR and hyperintense T2 shine through on diffusion weighted images The punctate areas in left parietal lobe with restricted area of diffusion raises the question of a recent small infarct less bright regions on DWI suggests a subacute hemorrhagic infarct.
Courtesy Ashley Davidoff MD copyright 2010 71000c03
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Subacute Hemorrhagic Infarct of the Parietal Lobe MRI
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Subacute Hemorrhagic Infarct of the Parietal Lobe MRI
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Acute Embolic Infarct High Parietal Region
CT and MRI
The axial images are from a patient with atrial fibrillation and neurological deficits.
Image a is a CT scan which shows a high density lesion i the vertex of the right pariettal lobe suggesting hemorhagic change.
Image b is a diffusion weighted MRI image at the level of the ventricles which shows a high intensity region in the parieto-occipital region suggesting acute infarction.
Image c is a axial T2 weighted image showing edema in the white matter of the right parietal lobe.
Image is aGRE image showing mixed heterogeneity with probable iron deposition suggesting subacute or chronic hemorhage.
Findings are consistent with old and new multicentric infarcts of the brain likely from the heart caused by atrial fibrillation
Courtesy Ashley Davidoff MD copyright 2010 71239c01
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Acute Embolic Infarct High Parietal Region
CT and MRI
The axial images are from a patient with atrial fibrillation and neurological deficits.
Image a is a CT scan which shows a high density lesion i the vertex of the right pariettal lobe suggesting hemorhagic change.
Image b is a diffusion weighted MRI image at the level of the ventricles which shows a high intensity region in the parieto-occipital region suggesting acute infarction.
Image c is a axial T2 weighted image showing edema in the white matter of the right parietal lobe.
Image is aGRE image showing mixed heterogeneity with probable iron deposition suggesting subacute or chronic hemorhage.
Findings are consistent with old and new multicentric infarcts of the brain likely from the heart caused by atrial fibrillation
Courtesy Ashley Davidoff MD copyright 2010 71239c01
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 7
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The axial images are from a patient with atrial fibrillation and neurological deficits.
Image a is a CT scan which shows a high density lesion i the vertex of the right pariettal lobe suggesting hemorhagic change.
Image b is a diffusion weighted MRI image at the level of the ventricles which shows a high intensity region in the parieto-occipital region suggesting acute infarction.
Image c is a axial T2 weighted image showing edema in the white matter of the right parietal lobe.
Image is aGRE image showing mixed heterogeneity with probable iron deposition suggesting subacute or chronic hemorhage.
Findings are consistent with old and new multicentric infarcts of the brain likely from the heart caused by atrial fibrillation
Courtesy Ashley Davidoff MD copyright 2010 71239c01
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The axial images are from a patient with atrial fibrillation and neurological deficits.
Image a is a CT scan which shows a high density lesion i the vertex of the right pariettal lobe suggesting hemorhagic change.
Image b is a diffusion weighted MRI image at the level of the ventricles which shows a high intensity region in the parieto-occipital region suggesting acute infarction.
Image c is a axial T2 weighted image showing edema in the white matter of the right parietal lobe.
Image is aGRE image showing mixed heterogeneity with probable iron deposition suggesting subacute or chronic hemorhage.
Findings are consistent with old and new multicentric infarcts of the brain likely from the heart caused by atrial fibrillation
Courtesy Ashley Davidoff MD copyright 2010 71239c01
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Acute Embolic Infarct High Parietal Region
CT and MRI
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Acute Embolic Infarct High Parietal Region
CT and MRI
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Acute Intracerebral Hemorrhage with Mass Effect and Rupture into the Ventricles –
CT
This CT shows an acute hemorrhagic event originating in the frontoparietal region of the left cerebral hemisphere causing significant mass effect by compressing and displacing the ipsilateral lateral ventricle with significant midline shift. The hemorrhage has ruptured into the ipsilateral lateral ventricle and blood can be seen within the choroid plexus (b) in the posterior horn (c) as well as the 4th ventricle (d). The ipsilateral edema has caused loss of the gray white matter interface in the left parietal lobe
Courtesy Ashley Davidoff MD copyright 2010 72143c01
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Acute Intracerebral Hemorrhage with Mass Effect and Rupture into the Ventricles –
CT
This CT shows an acute hemorrhagic event originating in the frontoparietal region of the left cerebral hemisphere causing significant mass effect by compressing and displacing the ipsilateral lateral ventricle with significant midline shift. The hemorrhage has ruptured into the ipsilateral lateral ventricle and blood can be seen within the choroid plexus (b) in the posterior horn (c) as well as the 4th ventricle (d). The ipsilateral edema has caused loss of the gray white matter interface in the left parietal lobe
Courtesy Ashley Davidoff MD copyright 2010 72143c01
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
This CT shows an acute hemorrhagic event originating in the frontoparietal region of the left cerebral hemisphere causing significant mass effect by compressing and displacing the ipsilateral lateral ventricle with significant midline shift. The hemorrhage has ruptured into the ipsilateral lateral ventricle and blood can be seen within the choroid plexus (b) in the posterior horn (c) as well as the 4th ventricle (d). The ipsilateral edema has caused loss of the gray white matter interface in the left parietal lobe
Courtesy Ashley Davidoff MD copyright 2010 72143c01
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
This CT shows an acute hemorrhagic event originating in the frontoparietal region of the left cerebral hemisphere causing significant mass effect by compressing and displacing the ipsilateral lateral ventricle with significant midline shift. The hemorrhage has ruptured into the ipsilateral lateral ventricle and blood can be seen within the choroid plexus (b) in the posterior horn (c) as well as the 4th ventricle (d). The ipsilateral edema has caused loss of the gray white matter interface in the left parietal lobe
Courtesy Ashley Davidoff MD copyright 2010 72143c01
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Acute Intracerebral Hemorrhage with Mass Effect and Rupture into the Ventricles –
CT
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Acute Intracerebral Hemorrhage with Mass Effect and Rupture into the Ventricles –
CT
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Acute Intracerebral Hemorrhage
The CT is from a 77year old male with acute neurological deficit The epicenter of the disease is an acute hemorrhage in the right thalamus, bright red in (b,d) with extension of the clot into the ventricle (maroon). There is non clotted blood lying dependently in the occipital horns (dense on c) presenting as a CSF-blood level (light pink on black CSF) in (d). The hemorrhage is surrounded by a rim of edema (light yellow) as seen in b and d.
Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 90461c03.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Acute Intracerebral Hemorrhage
The CT is from a 77year old male with acute neurological deficit The epicenter of the disease is an acute hemorrhage in the right thalamus, bright red in (b,d) with extension of the clot into the ventricle (maroon). There is non clotted blood lying dependently in the occipital horns (dense on c) presenting as a CSF-blood level (light pink on black CSF) in (d). The hemorrhage is surrounded by a rim of edema (light yellow) as seen in b and d.
Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 90461c03.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The CT is from a 77year old male with acute neurological deficit The epicenter of the disease is an acute hemorrhage in the right thalamus, bright red in (b,d) with extension of the clot into the ventricle (maroon). There is non clotted blood lying dependently in the occipital horns (dense on c) presenting as a CSF-blood level (light pink on black CSF) in (d). The hemorrhage is surrounded by a rim of edema (light yellow) as seen in b and d.
Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 90461c03.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The CT is from a 77year old male with acute neurological deficit The epicenter of the disease is an acute hemorrhage in the right thalamus, bright red in (b,d) with extension of the clot into the ventricle (maroon). There is non clotted blood lying dependently in the occipital horns (dense on c) presenting as a CSF-blood level (light pink on black CSF) in (d). The hemorrhage is surrounded by a rim of edema (light yellow) as seen in b and d.
Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 90461c03.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Acute Intracerebral Hemorrhage
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Acute Intracerebral Hemorrhage
)