DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] =>
[nodeName] => table
[nodeValue] =>
Chronic ulcerative colitis
In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Chronic ulcerative colitis
In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Chronic ulcerative colitis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Chronic ulcerative colitis
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Chronic ulcerative colitis
Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Chronic ulcerative colitis
Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Chronic ulcerative colitis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Chronic ulcerative colitis
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/27733.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Ulcerative colitis ? fluid contents
Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Ulcerative colitis ? fluid contents
Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Ulcerative colitis ? fluid contents
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Ulcerative colitis ? fluid contents
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/04198.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Pathology of acute severe ulcerative colitis
The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Pathology of acute severe ulcerative colitis
The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Pathology of acute severe ulcerative colitis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Pathology of acute severe ulcerative colitis
)
https://beta.thecommonvein.net/wp-content/uploads/2023/04/00578.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
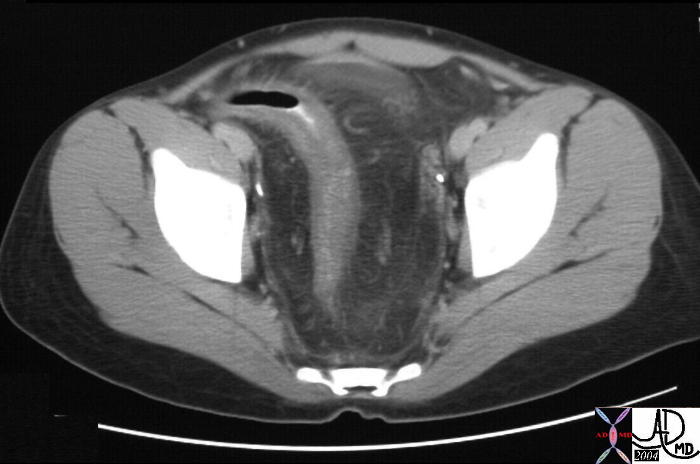
Rectal involvement in pseudomembranous colitis.
Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Rectal involvement in pseudomembranous colitis.
Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Rectal involvement in pseudomembranous colitis.
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Rectal involvement in pseudomembranous colitis.
)
https://beta.thecommonvein.net/wp-content/uploads/2023/06/45352.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
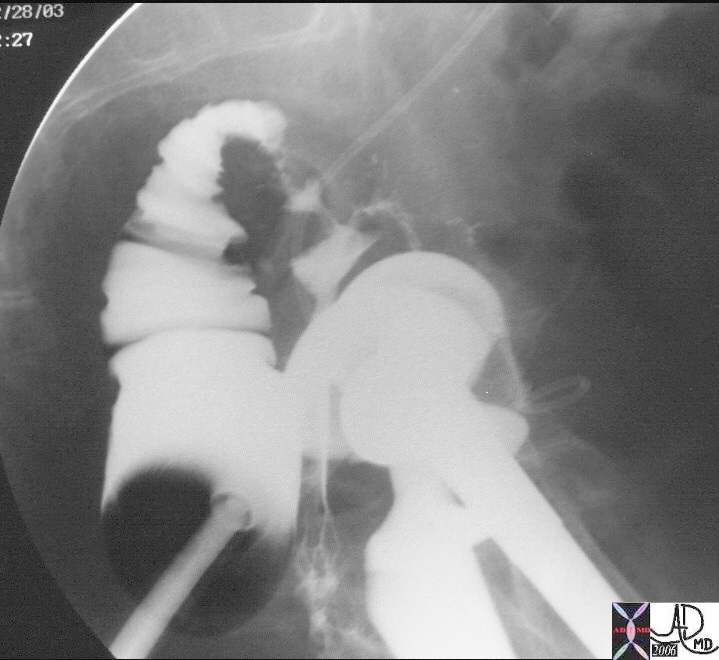
Rectovaginal fistula
This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Rectovaginal fistula
This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Rectovaginal fistula
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Rectovaginal fistula
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/29812b03.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/05/29812.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Lateral rectum anus
The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Lateral rectum anus
The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Lateral rectum anus
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Lateral rectum anus
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/29814b01.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Pectinate line
The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Pectinate line
The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Pectinate line
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Pectinate line
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/29814b01.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/72241p.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
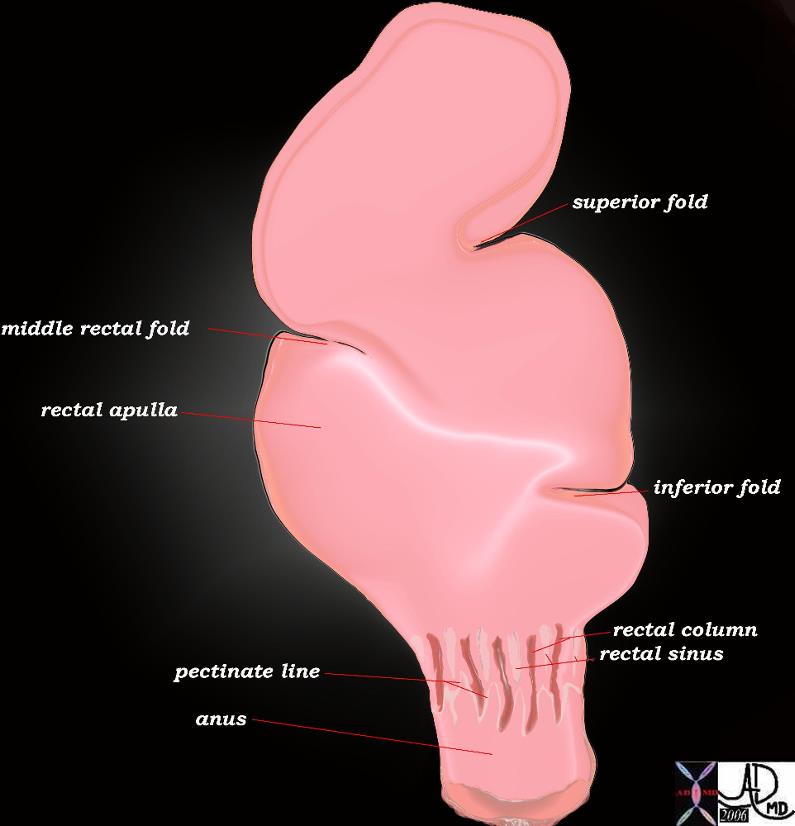
Rectum ? normal anatomy
The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Rectum ? normal anatomy
The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Rectum ? normal anatomy
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Rectum ? normal anatomy
)
https://beta.thecommonvein.net/wp-content/uploads/2023/06/45506b07.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => table
[nodeValue] =>
The rectum is a remarkable organ with its ability to detect the nature of its contents enabled by a rich supply of nerves and blood vessels. It can for example distinguish between solid stool, liquid stool, and air. It is far more complex in form, sensitivity, and muscular function than any other part of the colon.
The rectum is formed at about the 3rd sacral segment. As the sigmoid loses its freedom and dives back into the retroperitoneum to form the rectum, the three taenia coli expand to form a complete circumferential layer of longitudinal muscle rather the three distinct bands. The rectum ends at the anorectal junction where it turns at an angle of about ninety degrees posteriorly at the perineal flexure into the anus.
Since there is no taenia coli in the rectum there are no haustra. Its walls are therefore relatively smooth but for three mucosal folds or valves that cross about one third of the diameter of the rectum.? two to the left side and one to its right. They are named according to their position as superior, middle and inferior rectal folds. The crescentic mucosal folds are also called Houston?s valves, and their function may be to partially support the stool so that all feces does not drop in as one mass into the most dependant part of the rectum.
Rectum ? normal anatomy
The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
The middle fold is an important clinical landmark since it is the approximate position of the peritoneal reflection. A perforation above the fold would result in stool contents leaking into the peritoneal space with widespread and potentially devastating clinical consequence, while a perforation below the middle fold results in a more confined leak into the retroperitoneal or extraperitoneal space. It also so happens that the distance from the anus to the middle fold is about 7cms, which is about the length of the examining finger. Thus theoretically if one suspects a perforation and it can be felt by rectal examination then one is able to place it below the middle fold and therefore predict an extraperitoneal or retroperitoneal extension.
The upper part of the rectum above the middle fold may contain feces, but in the healthy normal individuals the rectum should be devoid of stool. The finding of stool in the ampulla suggests a diagnosis of chronic constipation.
The upper portion of the rectum, above the superior fold is about the diameter of the sigmoid colon above. The middle portion, below the superior fold called the ampulla, is more capacious and distensible. At its inferior aspect the rectum again narrows at the level of the rectal columns just above the pectinate line also marking the position of the internal sphincter muscle.
Near the anorectal junction, the mucosa and some smooth muscle becomes heaped up to form the rectal columns between which are the rectal sinuses, and just below the columns is the pectinate line ? the border between the rectum and anus. Pectinate derives from the Latin word for comb since the shape of the line is reminiscent of a comb. It is also known as the dentate line because it also looks like a row of teeth.
The anorectal junction is the most distinct and obvious junction of the entire colon. It has embryological significance since the rectum derives from endoderm (an embryologic tissue responsible for bowel development) and the anus which derives from ectoderm. (an embryologic tissue responsible for skin and brain development) The epithelium changes from the rectal columnar epithelium described above to a squamous epithelium. The lymphatic drainage changes from the internal iliac nodes and mesenteric nodes for the rectum, to the inguinal nodes for the anus, and it also marks the area of blood supply for the middle rectal artery above the line to the inferior rectal artery below the line. The pectinate line which is found about 2-3 cms from the anal opening, also marks the upper portion of the internal sphincter and the level of the internal hemorrhoids.
Pectinate line
The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
Although the word rectum means straight when viewed from the lateral projection it is far from straight. The rectum conforms to the arch of the sacrum and coccyx, and when looked at from the lateral projection is seen to fit snugly into the gentle curve of the sacrum. At the anorectal junction the anus turns backward so that the anal axis from anal opening t anorectal junction is from posterior to anterior directed toward the umbilicus. This anatomic point is very important for all professionals who insert tubes, drains or scopes into the rectum. From the anal verge the catheter must be directed to an imaginary point that coincides with the umbilicus.
Lateral rectum anus
The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
The rectum is about 12cms in length, and should be about 4cms in diameter. A rectum that is larger than 6.5cms is abnormal and considered a megarectum.
As stated above, the rectum is a retroperitoneal organ. The sigmoid on its long mesentery is intraperitoneal. When the transition to rectum occurs the peritoneum initially covers the anterior and lateral walls of the rectum, then more distally only the anterior wall is covered while the lower third has no peritoneal covering.
The rectum has a dual blood supply. It receives supply from the IMA and the internal iliac arteries. The superior rectal arises from the IMA while the middle rectal and inferior rectal arise from the internal iliacs. The internal submucosal venous plexus situated in the upper portion of the rectum drains into the inferior mesenteric vein while the lower portion of the rectum and external hemorrhoidal plexus drains into the iliac veins. Carcinomas of the upper and middle rectal region will metastasize to the liver via the portal vein, while a tumor in the lower rectum will spread to the systemic venous system and will travel via the IVC and heart ending up as a metastasis in the lung.
Applied Anatomy
In the female one of the anterior relations of the rectum is the vagina and hence disease from the one can spread to the second. The result is a fistula between the two ? rectovaginal fistula.
Rectovaginal fistula
This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
Rectal involvement in pseudomembranous colitis.
Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
Ulcerative colitis (UC)
Ulcerative colitis is an inflammatory condition of the mucosa of the large bowel which characteristically starts distally in the colon involving the rectum progressing in a retrograde manner to the right side of the colon via the left side. As a rule the rectum is almost always involved. Backwash ileitis can occur when the cecum is involved. In severe cases the disease can spread to the deeper layers, and in long standing cases carcinoma can develop. The involvement of the deeper layers and the ileum creates difficulty for the radiologist and pathologist sometimes to distinguish Crohn?s disease and UC. The finding of granulomas as noted above in the Crohn?s paragraph, distinguishes the two entities pathologically.
(eMedicine)
Pathology of acute severe ulcerative colitis
The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
The radiology of acute ulcerative colitis was discussed in the section on diarrhea and is represented below again to correlate with the pathology image above.
Ulcerative colitis ? fluid contents
Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
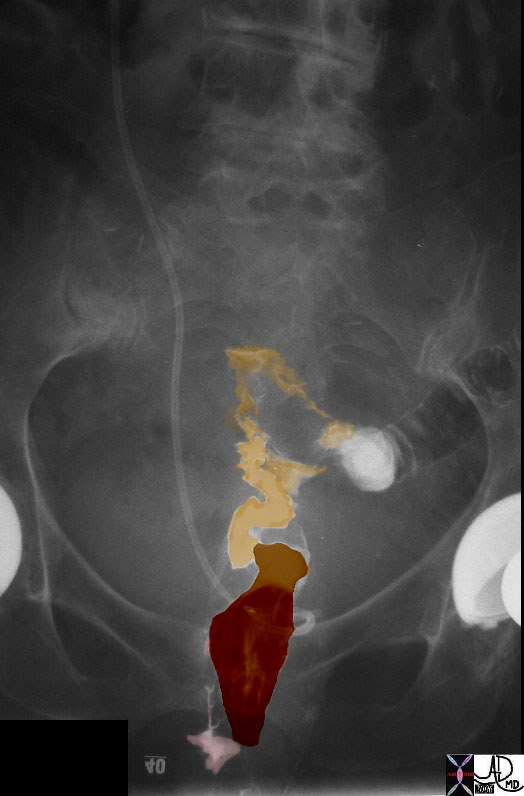
Chronic ulcerative colitis shows thickening, shortening rigidity sometimes becoming stiff and straight like a lead pipe. There is also accumulation of fat in the submucosa as well as in the pericolonic region.
Chronic ulcerative colitis
Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
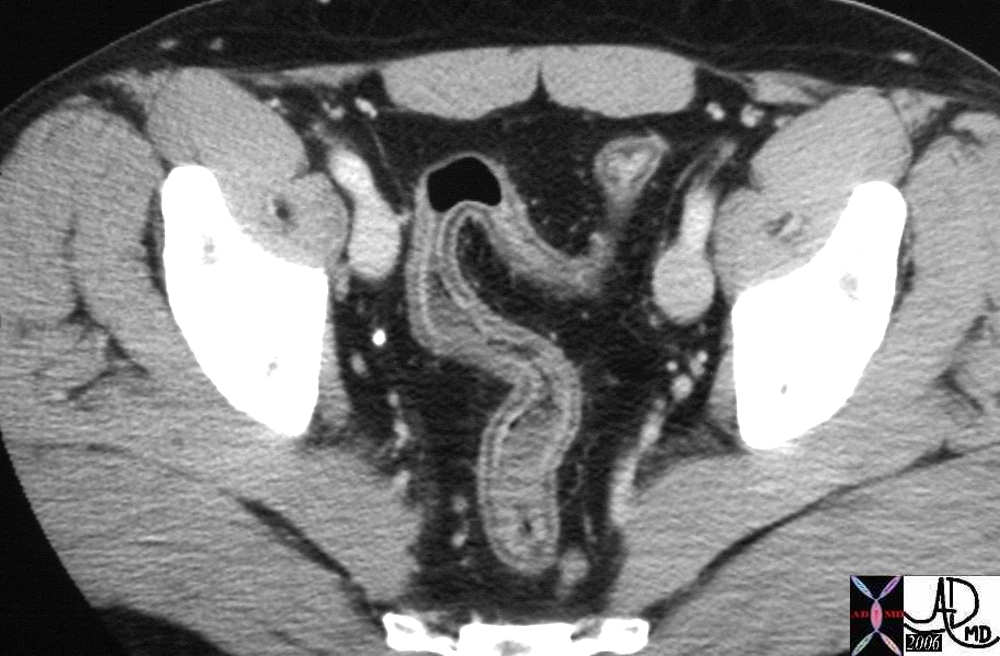
Chronic ulcerative colitis
In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] =>
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
The rectum is a remarkable organ with its ability to detect the nature of its contents enabled by a rich supply of nerves and blood vessels. It can for example distinguish between solid stool, liquid stool, and air. It is far more complex in form, sensitivity, and muscular function than any other part of the colon.
The rectum is formed at about the 3rd sacral segment. As the sigmoid loses its freedom and dives back into the retroperitoneum to form the rectum, the three taenia coli expand to form a complete circumferential layer of longitudinal muscle rather the three distinct bands. The rectum ends at the anorectal junction where it turns at an angle of about ninety degrees posteriorly at the perineal flexure into the anus.
Since there is no taenia coli in the rectum there are no haustra. Its walls are therefore relatively smooth but for three mucosal folds or valves that cross about one third of the diameter of the rectum.? two to the left side and one to its right. They are named according to their position as superior, middle and inferior rectal folds. The crescentic mucosal folds are also called Houston?s valves, and their function may be to partially support the stool so that all feces does not drop in as one mass into the most dependant part of the rectum.
Rectum ? normal anatomy
The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
The middle fold is an important clinical landmark since it is the approximate position of the peritoneal reflection. A perforation above the fold would result in stool contents leaking into the peritoneal space with widespread and potentially devastating clinical consequence, while a perforation below the middle fold results in a more confined leak into the retroperitoneal or extraperitoneal space. It also so happens that the distance from the anus to the middle fold is about 7cms, which is about the length of the examining finger. Thus theoretically if one suspects a perforation and it can be felt by rectal examination then one is able to place it below the middle fold and therefore predict an extraperitoneal or retroperitoneal extension.
The upper part of the rectum above the middle fold may contain feces, but in the healthy normal individuals the rectum should be devoid of stool. The finding of stool in the ampulla suggests a diagnosis of chronic constipation.
The upper portion of the rectum, above the superior fold is about the diameter of the sigmoid colon above. The middle portion, below the superior fold called the ampulla, is more capacious and distensible. At its inferior aspect the rectum again narrows at the level of the rectal columns just above the pectinate line also marking the position of the internal sphincter muscle.
Near the anorectal junction, the mucosa and some smooth muscle becomes heaped up to form the rectal columns between which are the rectal sinuses, and just below the columns is the pectinate line ? the border between the rectum and anus. Pectinate derives from the Latin word for comb since the shape of the line is reminiscent of a comb. It is also known as the dentate line because it also looks like a row of teeth.
The anorectal junction is the most distinct and obvious junction of the entire colon. It has embryological significance since the rectum derives from endoderm (an embryologic tissue responsible for bowel development) and the anus which derives from ectoderm. (an embryologic tissue responsible for skin and brain development) The epithelium changes from the rectal columnar epithelium described above to a squamous epithelium. The lymphatic drainage changes from the internal iliac nodes and mesenteric nodes for the rectum, to the inguinal nodes for the anus, and it also marks the area of blood supply for the middle rectal artery above the line to the inferior rectal artery below the line. The pectinate line which is found about 2-3 cms from the anal opening, also marks the upper portion of the internal sphincter and the level of the internal hemorrhoids.
Pectinate line
The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
Although the word rectum means straight when viewed from the lateral projection it is far from straight. The rectum conforms to the arch of the sacrum and coccyx, and when looked at from the lateral projection is seen to fit snugly into the gentle curve of the sacrum. At the anorectal junction the anus turns backward so that the anal axis from anal opening t anorectal junction is from posterior to anterior directed toward the umbilicus. This anatomic point is very important for all professionals who insert tubes, drains or scopes into the rectum. From the anal verge the catheter must be directed to an imaginary point that coincides with the umbilicus.
Lateral rectum anus
The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
The rectum is about 12cms in length, and should be about 4cms in diameter. A rectum that is larger than 6.5cms is abnormal and considered a megarectum.
As stated above, the rectum is a retroperitoneal organ. The sigmoid on its long mesentery is intraperitoneal. When the transition to rectum occurs the peritoneum initially covers the anterior and lateral walls of the rectum, then more distally only the anterior wall is covered while the lower third has no peritoneal covering.
The rectum has a dual blood supply. It receives supply from the IMA and the internal iliac arteries. The superior rectal arises from the IMA while the middle rectal and inferior rectal arise from the internal iliacs. The internal submucosal venous plexus situated in the upper portion of the rectum drains into the inferior mesenteric vein while the lower portion of the rectum and external hemorrhoidal plexus drains into the iliac veins. Carcinomas of the upper and middle rectal region will metastasize to the liver via the portal vein, while a tumor in the lower rectum will spread to the systemic venous system and will travel via the IVC and heart ending up as a metastasis in the lung.
Applied Anatomy
In the female one of the anterior relations of the rectum is the vagina and hence disease from the one can spread to the second. The result is a fistula between the two ? rectovaginal fistula.
Rectovaginal fistula
This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
Rectal involvement in pseudomembranous colitis.
Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
Ulcerative colitis (UC)
Ulcerative colitis is an inflammatory condition of the mucosa of the large bowel which characteristically starts distally in the colon involving the rectum progressing in a retrograde manner to the right side of the colon via the left side. As a rule the rectum is almost always involved. Backwash ileitis can occur when the cecum is involved. In severe cases the disease can spread to the deeper layers, and in long standing cases carcinoma can develop. The involvement of the deeper layers and the ileum creates difficulty for the radiologist and pathologist sometimes to distinguish Crohn?s disease and UC. The finding of granulomas as noted above in the Crohn?s paragraph, distinguishes the two entities pathologically.
(eMedicine)
Pathology of acute severe ulcerative colitis
The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
The radiology of acute ulcerative colitis was discussed in the section on diarrhea and is represented below again to correlate with the pathology image above.
Ulcerative colitis ? fluid contents
Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
Chronic ulcerative colitis shows thickening, shortening rigidity sometimes becoming stiff and straight like a lead pipe. There is also accumulation of fat in the submucosa as well as in the pericolonic region.
Chronic ulcerative colitis
Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
Chronic ulcerative colitis
In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Chronic ulcerative colitis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Chronic ulcerative colitis
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Chronic ulcerative colitis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Chronic ulcerative colitis
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
https://beta.thecommonvein.net/wp-content/uploads/2023/05/27733.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Ulcerative colitis ? fluid contents
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Ulcerative colitis ? fluid contents
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
https://beta.thecommonvein.net/wp-content/uploads/2023/05/04198.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Pathology of acute severe ulcerative colitis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Pathology of acute severe ulcerative colitis
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
https://beta.thecommonvein.net/wp-content/uploads/2023/04/00578.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Rectal involvement in pseudomembranous colitis.
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Rectal involvement in pseudomembranous colitis.
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
https://beta.thecommonvein.net/wp-content/uploads/2023/06/45352.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Rectovaginal fistula
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Rectovaginal fistula
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
https://beta.thecommonvein.net/wp-content/uploads/2023/05/29812.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/05/29812b03.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Lateral rectum anus
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Lateral rectum anus
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
https://beta.thecommonvein.net/wp-content/uploads/2023/05/29814b01.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Pectinate line
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Pectinate line
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
https://beta.thecommonvein.net/wp-content/uploads/2023/06/72241p.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/05/29814b01.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Rectum ? normal anatomy
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Rectum ? normal anatomy
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/20083.jpg
https://beta.thecommonvein.net/wp-content/uploads/2023/06/45506b07.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 48
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The rectum is a remarkable organ with its ability to detect the nature of its contents enabled by a rich supply of nerves and blood vessels. It can for example distinguish between solid stool, liquid stool, and air. It is far more complex in form, sensitivity, and muscular function than any other part of the colon.
The rectum is formed at about the 3rd sacral segment. As the sigmoid loses its freedom and dives back into the retroperitoneum to form the rectum, the three taenia coli expand to form a complete circumferential layer of longitudinal muscle rather the three distinct bands. The rectum ends at the anorectal junction where it turns at an angle of about ninety degrees posteriorly at the perineal flexure into the anus.
Since there is no taenia coli in the rectum there are no haustra. Its walls are therefore relatively smooth but for three mucosal folds or valves that cross about one third of the diameter of the rectum.? two to the left side and one to its right. They are named according to their position as superior, middle and inferior rectal folds. The crescentic mucosal folds are also called Houston?s valves, and their function may be to partially support the stool so that all feces does not drop in as one mass into the most dependant part of the rectum.
Rectum ? normal anatomy
The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
The middle fold is an important clinical landmark since it is the approximate position of the peritoneal reflection. A perforation above the fold would result in stool contents leaking into the peritoneal space with widespread and potentially devastating clinical consequence, while a perforation below the middle fold results in a more confined leak into the retroperitoneal or extraperitoneal space. It also so happens that the distance from the anus to the middle fold is about 7cms, which is about the length of the examining finger. Thus theoretically if one suspects a perforation and it can be felt by rectal examination then one is able to place it below the middle fold and therefore predict an extraperitoneal or retroperitoneal extension.
The upper part of the rectum above the middle fold may contain feces, but in the healthy normal individuals the rectum should be devoid of stool. The finding of stool in the ampulla suggests a diagnosis of chronic constipation.
The upper portion of the rectum, above the superior fold is about the diameter of the sigmoid colon above. The middle portion, below the superior fold called the ampulla, is more capacious and distensible. At its inferior aspect the rectum again narrows at the level of the rectal columns just above the pectinate line also marking the position of the internal sphincter muscle.
Near the anorectal junction, the mucosa and some smooth muscle becomes heaped up to form the rectal columns between which are the rectal sinuses, and just below the columns is the pectinate line ? the border between the rectum and anus. Pectinate derives from the Latin word for comb since the shape of the line is reminiscent of a comb. It is also known as the dentate line because it also looks like a row of teeth.
The anorectal junction is the most distinct and obvious junction of the entire colon. It has embryological significance since the rectum derives from endoderm (an embryologic tissue responsible for bowel development) and the anus which derives from ectoderm. (an embryologic tissue responsible for skin and brain development) The epithelium changes from the rectal columnar epithelium described above to a squamous epithelium. The lymphatic drainage changes from the internal iliac nodes and mesenteric nodes for the rectum, to the inguinal nodes for the anus, and it also marks the area of blood supply for the middle rectal artery above the line to the inferior rectal artery below the line. The pectinate line which is found about 2-3 cms from the anal opening, also marks the upper portion of the internal sphincter and the level of the internal hemorrhoids.
Pectinate line
The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
Although the word rectum means straight when viewed from the lateral projection it is far from straight. The rectum conforms to the arch of the sacrum and coccyx, and when looked at from the lateral projection is seen to fit snugly into the gentle curve of the sacrum. At the anorectal junction the anus turns backward so that the anal axis from anal opening t anorectal junction is from posterior to anterior directed toward the umbilicus. This anatomic point is very important for all professionals who insert tubes, drains or scopes into the rectum. From the anal verge the catheter must be directed to an imaginary point that coincides with the umbilicus.
Lateral rectum anus
The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
The rectum is about 12cms in length, and should be about 4cms in diameter. A rectum that is larger than 6.5cms is abnormal and considered a megarectum.
As stated above, the rectum is a retroperitoneal organ. The sigmoid on its long mesentery is intraperitoneal. When the transition to rectum occurs the peritoneum initially covers the anterior and lateral walls of the rectum, then more distally only the anterior wall is covered while the lower third has no peritoneal covering.
The rectum has a dual blood supply. It receives supply from the IMA and the internal iliac arteries. The superior rectal arises from the IMA while the middle rectal and inferior rectal arise from the internal iliacs. The internal submucosal venous plexus situated in the upper portion of the rectum drains into the inferior mesenteric vein while the lower portion of the rectum and external hemorrhoidal plexus drains into the iliac veins. Carcinomas of the upper and middle rectal region will metastasize to the liver via the portal vein, while a tumor in the lower rectum will spread to the systemic venous system and will travel via the IVC and heart ending up as a metastasis in the lung.
Applied Anatomy
In the female one of the anterior relations of the rectum is the vagina and hence disease from the one can spread to the second. The result is a fistula between the two ? rectovaginal fistula.
Rectovaginal fistula
This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
Rectal involvement in pseudomembranous colitis.
Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
Ulcerative colitis (UC)
Ulcerative colitis is an inflammatory condition of the mucosa of the large bowel which characteristically starts distally in the colon involving the rectum progressing in a retrograde manner to the right side of the colon via the left side. As a rule the rectum is almost always involved. Backwash ileitis can occur when the cecum is involved. In severe cases the disease can spread to the deeper layers, and in long standing cases carcinoma can develop. The involvement of the deeper layers and the ileum creates difficulty for the radiologist and pathologist sometimes to distinguish Crohn?s disease and UC. The finding of granulomas as noted above in the Crohn?s paragraph, distinguishes the two entities pathologically.
(eMedicine)
Pathology of acute severe ulcerative colitis
The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
The radiology of acute ulcerative colitis was discussed in the section on diarrhea and is represented below again to correlate with the pathology image above.
Ulcerative colitis ? fluid contents
Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
Chronic ulcerative colitis shows thickening, shortening rigidity sometimes becoming stiff and straight like a lead pipe. There is also accumulation of fat in the submucosa as well as in the pericolonic region.
Chronic ulcerative colitis
Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
Chronic ulcerative colitis
In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The rectum is a remarkable organ with its ability to detect the nature of its contents enabled by a rich supply of nerves and blood vessels. It can for example distinguish between solid stool, liquid stool, and air. It is far more complex in form, sensitivity, and muscular function than any other part of the colon.
The rectum is formed at about the 3rd sacral segment. As the sigmoid loses its freedom and dives back into the retroperitoneum to form the rectum, the three taenia coli expand to form a complete circumferential layer of longitudinal muscle rather the three distinct bands. The rectum ends at the anorectal junction where it turns at an angle of about ninety degrees posteriorly at the perineal flexure into the anus.
Since there is no taenia coli in the rectum there are no haustra. Its walls are therefore relatively smooth but for three mucosal folds or valves that cross about one third of the diameter of the rectum.? two to the left side and one to its right. They are named according to their position as superior, middle and inferior rectal folds. The crescentic mucosal folds are also called Houston?s valves, and their function may be to partially support the stool so that all feces does not drop in as one mass into the most dependant part of the rectum.
Rectum ? normal anatomy
The rectum has 3 crescentic folds with the superior and inferior on the left and the middle rectal fold on the right. The superior fold marks the border between the first inlet part of the rectum above and the ampulla below. The inlet portion is narrow, widening at the ampulla and then narrowing again at the anorectal junction. The outlet portion contains the rectal columns and the pectinate line which is the anorectal junction.
Courtesy Ashley Davidoff MD
45506b07
The middle fold is an important clinical landmark since it is the approximate position of the peritoneal reflection. A perforation above the fold would result in stool contents leaking into the peritoneal space with widespread and potentially devastating clinical consequence, while a perforation below the middle fold results in a more confined leak into the retroperitoneal or extraperitoneal space. It also so happens that the distance from the anus to the middle fold is about 7cms, which is about the length of the examining finger. Thus theoretically if one suspects a perforation and it can be felt by rectal examination then one is able to place it below the middle fold and therefore predict an extraperitoneal or retroperitoneal extension.
The upper part of the rectum above the middle fold may contain feces, but in the healthy normal individuals the rectum should be devoid of stool. The finding of stool in the ampulla suggests a diagnosis of chronic constipation.
The upper portion of the rectum, above the superior fold is about the diameter of the sigmoid colon above. The middle portion, below the superior fold called the ampulla, is more capacious and distensible. At its inferior aspect the rectum again narrows at the level of the rectal columns just above the pectinate line also marking the position of the internal sphincter muscle.
Near the anorectal junction, the mucosa and some smooth muscle becomes heaped up to form the rectal columns between which are the rectal sinuses, and just below the columns is the pectinate line ? the border between the rectum and anus. Pectinate derives from the Latin word for comb since the shape of the line is reminiscent of a comb. It is also known as the dentate line because it also looks like a row of teeth.
The anorectal junction is the most distinct and obvious junction of the entire colon. It has embryological significance since the rectum derives from endoderm (an embryologic tissue responsible for bowel development) and the anus which derives from ectoderm. (an embryologic tissue responsible for skin and brain development) The epithelium changes from the rectal columnar epithelium described above to a squamous epithelium. The lymphatic drainage changes from the internal iliac nodes and mesenteric nodes for the rectum, to the inguinal nodes for the anus, and it also marks the area of blood supply for the middle rectal artery above the line to the inferior rectal artery below the line. The pectinate line which is found about 2-3 cms from the anal opening, also marks the upper portion of the internal sphincter and the level of the internal hemorrhoids.
Pectinate line
The pectinate line has the shape of a cocks comb. Pectinate comes from the Latin word that means comb. It is also called the dentate line because it also looks like a row of teeth.. This line marks the junction between the rectum and the anus and is a very important as it marks an embryological border as well as an anatomic border. This picture of a cock was taken at a family theme park in New Hampshire.
Courtesy Ashley Davidoff MD
29814b012 72241p
Although the word rectum means straight when viewed from the lateral projection it is far from straight. The rectum conforms to the arch of the sacrum and coccyx, and when looked at from the lateral projection is seen to fit snugly into the gentle curve of the sacrum. At the anorectal junction the anus turns backward so that the anal axis from anal opening t anorectal junction is from posterior to anterior directed toward the umbilicus. This anatomic point is very important for all professionals who insert tubes, drains or scopes into the rectum. From the anal verge the catheter must be directed to an imaginary point that coincides with the umbilicus.
Lateral rectum anus
The rectum in the lateral projection is far from straight. It conforms to the shape of the sacrum making a gentle ?C? shaped curve. At the anorectal junction it makes a backward turn, and at the point of turning it is called the anorectal flexure.
Courtesy Ashley Davidoff MD
29814b013
The rectum is about 12cms in length, and should be about 4cms in diameter. A rectum that is larger than 6.5cms is abnormal and considered a megarectum.
As stated above, the rectum is a retroperitoneal organ. The sigmoid on its long mesentery is intraperitoneal. When the transition to rectum occurs the peritoneum initially covers the anterior and lateral walls of the rectum, then more distally only the anterior wall is covered while the lower third has no peritoneal covering.
The rectum has a dual blood supply. It receives supply from the IMA and the internal iliac arteries. The superior rectal arises from the IMA while the middle rectal and inferior rectal arise from the internal iliacs. The internal submucosal venous plexus situated in the upper portion of the rectum drains into the inferior mesenteric vein while the lower portion of the rectum and external hemorrhoidal plexus drains into the iliac veins. Carcinomas of the upper and middle rectal region will metastasize to the liver via the portal vein, while a tumor in the lower rectum will spread to the systemic venous system and will travel via the IVC and heart ending up as a metastasis in the lung.
Applied Anatomy
In the female one of the anterior relations of the rectum is the vagina and hence disease from the one can spread to the second. The result is a fistula between the two ? rectovaginal fistula.
Rectovaginal fistula
This 73 year old patient has a vaginal discharge. The post evacuation film shows a decompressed rectum with upper portion of the more tubular rectum shown in mustard contains barium while the lower ampulla in burgundy is more sac-like and contains mostly air. The rectal folds are not seen. Can you see the contrast within the vagina? It is overlaid in pink to the right of the air filled rectum. The presence of contrast in the vagina implies a rectovaginal fistula.
Courtesy Ashley Davidoff MD
29812 29812b03
Rectal involvement in pseudomembranous colitis.
Clostridium difficile was identified in this elderly patient. The CT scan reveals transmural changes with thickened wall and perirectal fat involvement. The rectum is not usually involved in ischemic bowel since it has such a rich blood supply, while Crohn?s disease also usually spares the rectum as well. Ulcerative colitis is a mucosal disease, and hence the radiological image of transmural disease in the rectum is not consistent with UC, and therefore the most likely diagnosis is pseudomembranous colitis. Pseudomembranous colitis is caused by clostridium difficile.
Courtesy Ashley Davidoff MD
45352
Ulcerative colitis (UC)
Ulcerative colitis is an inflammatory condition of the mucosa of the large bowel which characteristically starts distally in the colon involving the rectum progressing in a retrograde manner to the right side of the colon via the left side. As a rule the rectum is almost always involved. Backwash ileitis can occur when the cecum is involved. In severe cases the disease can spread to the deeper layers, and in long standing cases carcinoma can develop. The involvement of the deeper layers and the ileum creates difficulty for the radiologist and pathologist sometimes to distinguish Crohn?s disease and UC. The finding of granulomas as noted above in the Crohn?s paragraph, distinguishes the two entities pathologically.
(eMedicine)
Pathology of acute severe ulcerative colitis
The pathology specimen reveals a hyperemic (swollen with blood) mucosa from a patient with severe acute hemorrhagic ulcerative colitis. The appearance is reminiscent of raw meat.
00578
The radiology of acute ulcerative colitis was discussed in the section on diarrhea and is represented below again to correlate with the pathology image above.
Ulcerative colitis ? fluid contents
Note that in this patient the colon is mildly distended and the contents are fluid in nature.. This 71year old male patient has diarrhea caused by ulcerative colitis which is a disease of the mucosa.
Courtesy Ashley Davidoff MD
04198
Chronic ulcerative colitis shows thickening, shortening rigidity sometimes becoming stiff and straight like a lead pipe. There is also accumulation of fat in the submucosa as well as in the pericolonic region.
Chronic ulcerative colitis
Three distinct lines are noted in the wall of the rectosigmoid colon. There is the inner bright line that represents the mucosa and submucosa, the black line that represents fat infiltration in the submucosa and the outer white line that represents the muscularis and the serosa. The fatty infiltration reflects chronicty and is not specific for UC and can be seen in Crohn?s disease.
Courtesy Ashley Davidoff MD
27733
Chronic ulcerative colitis
In this patient with chronic UC, the sigmoid wall is thickened and there is an increase in the pericolonic fat. This increase in pericolic fat is characteristic but is also seen in Crohn?s disease. It is called creeping fat.
Courtesy Ashley Davidoff MD
20083
)