Alok Anand MD
The Common Vein Copyright 2010
Introduction
Ultrasound evaluation of the prostate is performed via the transrectal route, though the prostate may be visualized on transabdominal US. Used alone, ultrasound demonstrates limited sensitivity in evaluating for cancer ? the primary indication is to guide needle biopsy for diagnosis. Standalone ultrasound is of value in evaluating abscess, as well as obstruction of the ejaculatory ducts or the posterior urethra. Ultrasound evaluation is also of value in the workup of infertility, as obstruction that is acquired or due to congenital anomalies within the periprostatic ducts is treatable.
Gray Scale and Doppler |
|
The prostate and seminal vesicles are accessible to the transrectal probe and using gray scale and doppler imaging structural evaluation is optimised.
Courtesy Ashley Davidof MD Copyright 2010 99380b01.4.8sg
|
Principles/Tissue Characterization/Time/Speed Distance and the Image/Impedence
The aim of diagnostic sonography is to characterize lesions, document anatomy and, where appropriate, function of the tissues being imaged whilst keeping the cumulative sound energy delivered ALARA (as low as reasonable achievable). The purpose of ultrasound of the prostate is to define the size shape position and character of the gland, as well as to determine if there are findings of inflammation, hypertrophy, or carcinogenesis.
Indications
Ultrasound is the procedure of choice in patients who present with clinical indications for prostatic evluation for carcinoma i.e. rising PSA, obstructive symptoms. In the setting of infection/abscess without a clear cause, CT imaging may be performed initially, and if prostatic abscess is suspected, ultrasound imaging performed.
Contraindications
There are no absolute medical contraindications to ultrasound. It is generally considered to be a safe procedure without significant side-effects. There is a small theoretical risk of damage to tissues from heating, which has been demonstrated with extreme doses in animal studies. As such, the examination is performed following the ALARA principle (keeping exposure As Low As Reasonably Achieveable).
Advantages
Ultrasound presents numerous advantages. First, it is fast and requires little preparation. It can be performed in real time, and is useful for visualizing the path of the biopsy needle prior to lancing the tissue. The machines used to perform ultrasound are extremely portable, and cheap in comparison to other imaging modalities. It carries few, if any, side-effects, produces no ionizing radiation, and is safe for use in pregnancy, as well as with delicate organs. Lastly imaging can be performed in any plane.
Disadvantages
Ultrasound is not effective in visualizing bone or air-filled structures. In addition, visualizing deep structures is often only possible at the expense of quality and resolution. Finally, the quality of studies produced is highly operator-dependent.
Patient Preparation
Patients are generally placed in the prone position, although some place the patient on his side, in a fetal position. A protective membrane, usually made of latex is placed over the probe, and a watersoluble gell is applied generously for lubrication. The probe is then advanced into the rectum.
The biopsy probe, usually a large cored needle that is spring-loaded, may be passed along a channel on the ultrasound probe, although trans perineal biopsies are not uncommon.
Equipment
Ultrasound equipment consists of a monitor, control panel and transducer (probe). The entire unit is typically wheeled and portable. Ultrasound machines typically have a number of different transducers, which differ in frequency of pulses generated and shape of the probe (and hence the shape of the image ? sector versus rectangle). Machines routinely used for diagnostic exams are relatively large, but much smaller units are available and are sometimes used in emergency rooms, physician offices and intensive care units for non-diagnostic assessment of, for example, bleeding in early pregnancy, musculoskeletal pain or obtaining intravenous access.
Method/Technique
The transducer is passed into the rectal cavity, with the transducer oriented in the coronal plane. Once the prostate is identified and sagittal images are also acquired. Static images are typically saved, though a series of frames may be recorded in certain examinations.
Landmarks
The prostate will appear as a rounded structure at the base of the bladder and is relatively echogenic. On transrectal imaging, the prostate will appear inverted (the transducer, which is closest to the base usually appears on top). The peripheral zone is typically may be relatively echogenic compared to the more heterogeneous central gland, which includes the central and transitional zones.
The prostatic urethra has a characteristic V-shape at the orifice. Adjacent in the coronal orientation is the lobulated appearing seminal vesicles, which lie along the groove between the prostate and urinary bladder.
The fibromuscular stroma can be identified anterior to the prostate, and appears hypoechoic in the superior aspect of the gland.
TRUS is useful in performing prostatic biopsies, evaluating for abscesses, and providing some useful information of local staging if cancer is detected. TRUS also enables measurement of prostatic volume
|
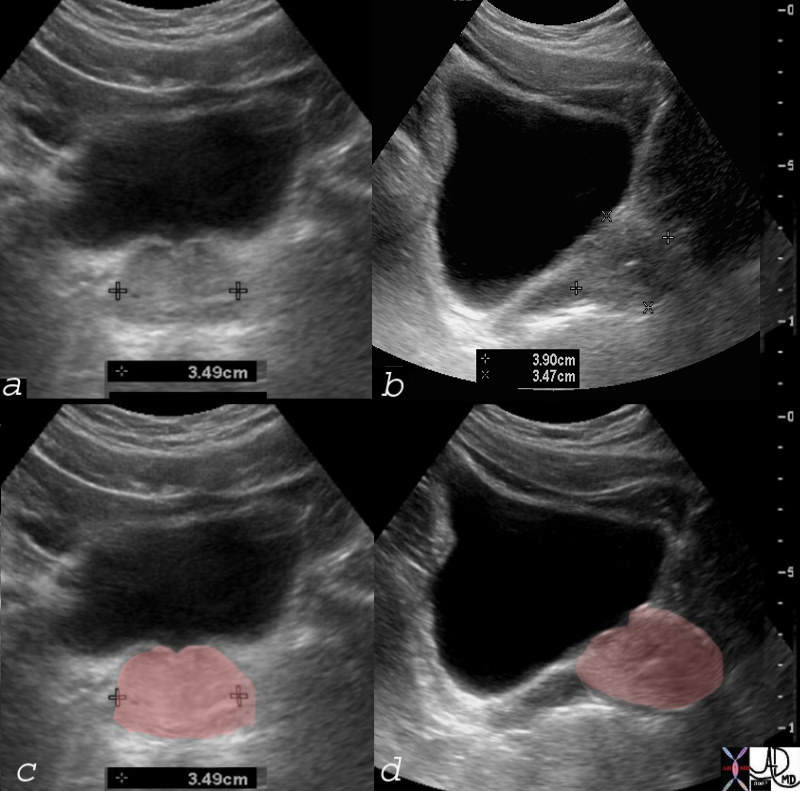
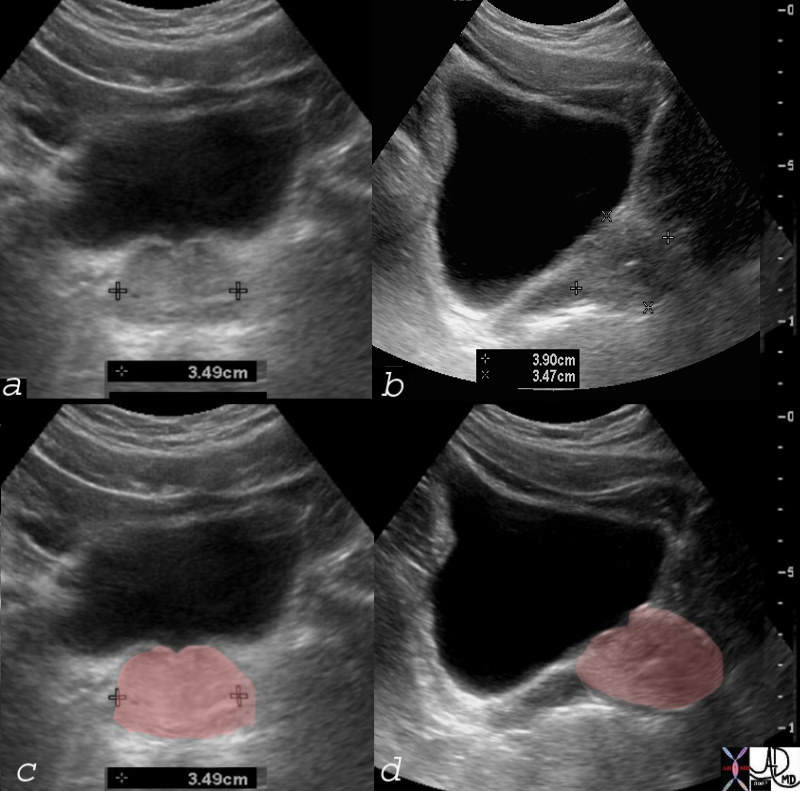
Normal Prostate by Ultrasound |
|
The volume of this gland is calculated by the formula using a simple prorated ellipsoid formula. Thus transverse diameter of 3.5cms is multipled by A-P dimension of 3.5cms by the craniocaudad dimension of 3.9cms and then by a correction factor of .52 . This calculation reveals a a volume of 25ccs which is normal.
Courtesy Ashley Davidoff MD 74897c03
|
Disease Findings
BPH
In the setting of an enlarged (> 30mL) prostate, the base of the bladder will be elevated. In the setting of BPH the transitional zone (part of the central gland) becomes larged and more heterogeneous. Discrete nodules and cysts may be noted. In addition, an echogenic pseudocapsule may form around the hypertrophic locus. Secondary to obstruction, bladder calculi may also be visualized, along with bladderwall thickedning and irregularity.
Prostatitis
In the acute setting, the gland may appear swollen and edematous. If the infection progresses, collections of echogenic fluid (from cellular debris) may be noted. In abscess, septations may also be present. If inflammation continues into the chronic setting, large calculi can also be identified. These become a nidus of persistent, relapsing infection.
Cysts
Cysts are commonly seen and are nonspecific. Depending on the location of cysts, they may be attributed to embryologic development, or obstruction. Midline cysts are usually Müllerian or Utricle cysts. Müllerian cysts often extend outside the confines of the gland. Utricular cysts are often associated with other congenital anomalies, such as hypospadias, cryptorchidism, or renal agenesis. The lateral locations are associated with functional obstruction for the seminal vesicle and ejaculatory ducts, most often in the setting of urinary tract infection. These two are of particular importance as they are treatable causes of infertility. Retention cysts are associated with BPH.
Carcinoma
Carcinoma can not be diagnosed on ultrasonography, however, several signs may be found in the setting of this disease. One finding is the presence of a distinct hypoechoic nodule, particularly a poorly marginated hypoechoic area in the peripheral zone. Mass effect on surrounding tissue. Asymmetric enlargement of the prostate may be seen, as well as deformation irregularities of the prostatic countour. Heterogeneities within the gland often arise as a result of tumor growth and necrosis, as the proliferatio outstrips the available blood supply. Consequently, there may also be focally increased areas vascularity of the gland on doppler color flow. These findings alone are nonspecific, and should lead the experienced clinician to perform biopsy for confirmation of suspicion.
Calculi
Calculi are common findings, particularly in the aging prostate. Thy may form spontaneously or in response to inflammation. Most are periurethral, caused by proteinaceous deposits within the gland called corpora amylacea. On ultrasound they appear bright (echogenic) and cause acoustic shadows, as they prevent sound waves from passing. They are NOT an indication of cancer, though they are often found in cancerous areas.
|
Strength and Weakness of Ultrasound |
|
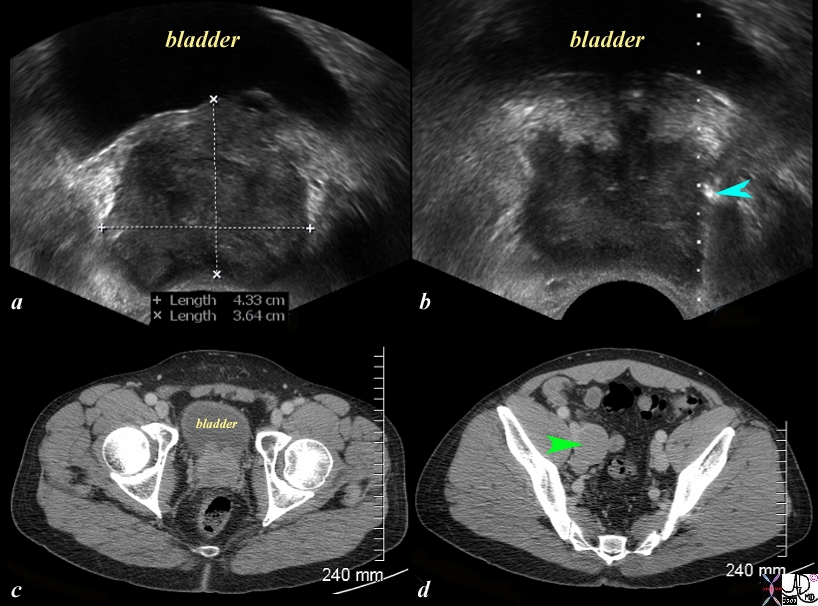
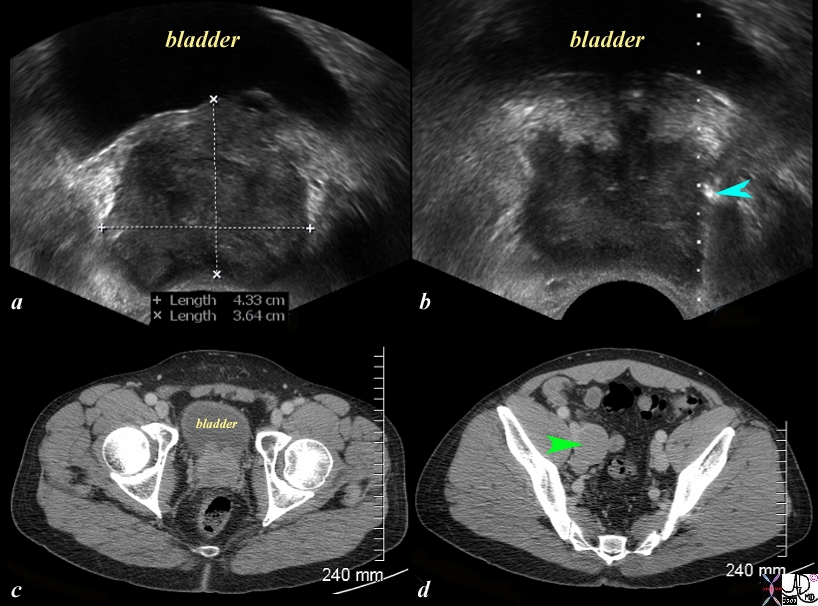
The series of US and CTscans are from a 50 year old man with an elevated PSA Image a is a transverse ultrasound showing a minimally prominent nodular prostate. Image b shows the needle tip (teal blue arrow) in the left peripheral zone. Image c is a transverse image of the prostate showing a nodular anterior surface while image d shows an almost 3cms external iliac node. The biopsy was positive for prostate carcinoma.
Whereas ultrasound is able to characterize the lesion and provide guidance for biopsy, it is unable to consistently visualise lymph nodes and hence CT is necessary for staging. The combination of the two modalities is required. PET CT is even more helpful.
Image Courtesy Ashley Davidoff MD Copyright 2010 97374c.81s
|
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] =>
[nodeName] => table
[nodeValue] =>
Strength and Weakness of Ultrasound
The series of US and CTscans are from a 50 year old man with an elevated PSA Image a is a transverse ultrasound showing a minimally prominent nodular prostate. Image b shows the needle tip (teal blue arrow) in the left peripheral zone. Image c is a transverse image of the prostate showing a nodular anterior surface while image d shows an almost 3cms external iliac node. The biopsy was positive for prostate carcinoma.
Whereas ultrasound is able to characterize the lesion and provide guidance for biopsy, it is unable to consistently visualise lymph nodes and hence CT is necessary for staging. The combination of the two modalities is required. PET CT is even more helpful.
Image Courtesy Ashley Davidoff MD Copyright 2010 97374c.81s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Strength and Weakness of Ultrasound
The series of US and CTscans are from a 50 year old man with an elevated PSA Image a is a transverse ultrasound showing a minimally prominent nodular prostate. Image b shows the needle tip (teal blue arrow) in the left peripheral zone. Image c is a transverse image of the prostate showing a nodular anterior surface while image d shows an almost 3cms external iliac node. The biopsy was positive for prostate carcinoma.
Whereas ultrasound is able to characterize the lesion and provide guidance for biopsy, it is unable to consistently visualise lymph nodes and hence CT is necessary for staging. The combination of the two modalities is required. PET CT is even more helpful.
Image Courtesy Ashley Davidoff MD Copyright 2010 97374c.81s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The series of US and CTscans are from a 50 year old man with an elevated PSA Image a is a transverse ultrasound showing a minimally prominent nodular prostate. Image b shows the needle tip (teal blue arrow) in the left peripheral zone. Image c is a transverse image of the prostate showing a nodular anterior surface while image d shows an almost 3cms external iliac node. The biopsy was positive for prostate carcinoma.
Whereas ultrasound is able to characterize the lesion and provide guidance for biopsy, it is unable to consistently visualise lymph nodes and hence CT is necessary for staging. The combination of the two modalities is required. PET CT is even more helpful.
Image Courtesy Ashley Davidoff MD Copyright 2010 97374c.81s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The series of US and CTscans are from a 50 year old man with an elevated PSA Image a is a transverse ultrasound showing a minimally prominent nodular prostate. Image b shows the needle tip (teal blue arrow) in the left peripheral zone. Image c is a transverse image of the prostate showing a nodular anterior surface while image d shows an almost 3cms external iliac node. The biopsy was positive for prostate carcinoma.
Whereas ultrasound is able to characterize the lesion and provide guidance for biopsy, it is unable to consistently visualise lymph nodes and hence CT is necessary for staging. The combination of the two modalities is required. PET CT is even more helpful.
Image Courtesy Ashley Davidoff MD Copyright 2010 97374c.81s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Strength and Weakness of Ultrasound
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Strength and Weakness of Ultrasound
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Normal Prostate by Ultrasound
The volume of this gland is calculated by the formula using a simple prorated ellipsoid formula. Thus transverse diameter of 3.5cms is multipled by A-P dimension of 3.5cms by the craniocaudad dimension of 3.9cms and then by a correction factor of .52 . This calculation reveals a a volume of 25ccs which is normal.
Courtesy Ashley Davidoff MD 74897c03
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Normal Prostate by Ultrasound
The volume of this gland is calculated by the formula using a simple prorated ellipsoid formula. Thus transverse diameter of 3.5cms is multipled by A-P dimension of 3.5cms by the craniocaudad dimension of 3.9cms and then by a correction factor of .52 . This calculation reveals a a volume of 25ccs which is normal.
Courtesy Ashley Davidoff MD 74897c03
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The volume of this gland is calculated by the formula using a simple prorated ellipsoid formula. Thus transverse diameter of 3.5cms is multipled by A-P dimension of 3.5cms by the craniocaudad dimension of 3.9cms and then by a correction factor of .52 . This calculation reveals a a volume of 25ccs which is normal.
Courtesy Ashley Davidoff MD 74897c03
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The volume of this gland is calculated by the formula using a simple prorated ellipsoid formula. Thus transverse diameter of 3.5cms is multipled by A-P dimension of 3.5cms by the craniocaudad dimension of 3.9cms and then by a correction factor of .52 . This calculation reveals a a volume of 25ccs which is normal.
Courtesy Ashley Davidoff MD 74897c03
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Normal Prostate by Ultrasound
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Normal Prostate by Ultrasound
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Gray Scale and Doppler
The prostate and seminal vesicles are accessible to the transrectal probe and using gray scale and doppler imaging structural evaluation is optimised.
Courtesy Ashley Davidof MD Copyright 2010 99380b01.4.8sg
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Gray Scale and Doppler
The prostate and seminal vesicles are accessible to the transrectal probe and using gray scale and doppler imaging structural evaluation is optimised.
Courtesy Ashley Davidof MD Copyright 2010 99380b01.4.8sg
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The prostate and seminal vesicles are accessible to the transrectal probe and using gray scale and doppler imaging structural evaluation is optimised.
Courtesy Ashley Davidof MD Copyright 2010 99380b01.4.8sg
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The prostate and seminal vesicles are accessible to the transrectal probe and using gray scale and doppler imaging structural evaluation is optimised.
Courtesy Ashley Davidof MD Copyright 2010 99380b01.4.8sg
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Gray Scale and Doppler
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Gray Scale and Doppler
)