The Common Vein Copyright 2007
Ashley Davidoff MD
Overview
The mucinous tumors of the pancreas consist of mucinous cystadenoma, mucinous cystadenocarcinoma, and intraductal papillary mucin tumor (IPMT). Both cystadenoma and mucinous cystadenocarcinoma arise from the smaller ducts while the intraductal papillary mucinous tumor arises from the larger central ducts.
Mucinous cystadenoma (macrocystic cystadenoma) is a benign and relatively uncommon condition of the pancreas. It is less common than its counterpart, serous cystadenoma by a factor of 2. It is more common in women (80%) and presents in the 6th decade, being slightly younger than the serous tumor. Although there is a range of histopathology from benign through dysplastic to malignant, all mucinous tumors of the pancreas should be considered premalignant.
Imaging
Cystadenoma and Cystadenocarcinoma
The imaging features are by no means pathgnomonic but some features are characteristic. They are large tumors ranging from 2cms to 26cms, usually slightly larger then the serous neoplasms. The larger tumors have a greater likelihood of being malignant. They are most commonly situated in the body and tail of the pancreas. The calcifications are usually in the wall and are of a dystrophic nature. The matrix of the lesion is usually multicystic, but may be unilocular with usually with less cysts than seen in serous cystadenoma. The septae are thickened and usually enhance, and there may be mural excrescences. The cysts are variable in density on the non contrast study because they contain mucin and variable amounts of hemorrhage. MRI is useful in characterizing the hemorrhage that often occurs in the cysts.
Approach
When a cystic lesion is identified in a patient, the first step is to exclude pancreatitis related disease ? a pseudocyst, or a dilated pancreatic duct. When these entities have been excluded, the age, sex, location and morphology of the lesion are prime components for initial consideration. A 50 year old female with a cystic lesion in the tail of the pancreas, that has peripheral curvilinear calcification with a few large cysts, leads to mucinous cystadenoma being the prime suspect. If the features are in question (which is a common occurrence), then biopsy and aspiration is required. The finding of high viscosity mucinous and hemorrhagic fluid, makes the diagnosis more certain. In the absence of a definitive pathological diagnosis, it is prudent surgically remove the lesion since it is premalignant.
Pathology
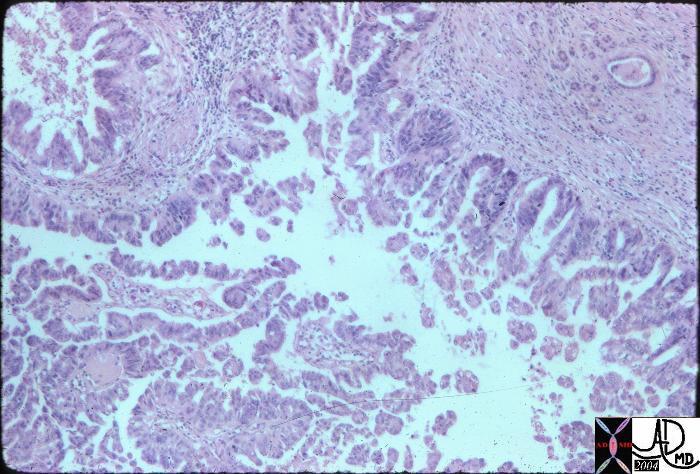 Papillary fronds and a simple columnar mucus epithelium characterizes the histology of the mucinous cystadenoma. The subepithelial layer consists of prominent cellular components and the outer layer consists of hyalinized connective tissue. 15318 Courtesy Barbara Banner MD
Papillary fronds and a simple columnar mucus epithelium characterizes the histology of the mucinous cystadenoma. The subepithelial layer consists of prominent cellular components and the outer layer consists of hyalinized connective tissue. 15318 Courtesy Barbara Banner MD
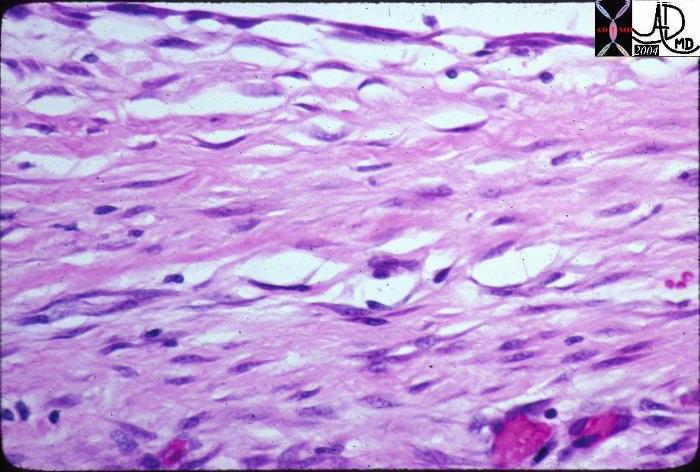 This high powered histological section is from the records of a patient with a pseudocyst. At the top of the image the white space represents the cyst lumen. The lining is made of fibrous tissue rather than an epithelium. A true cyst is lined by epithelial cells. 15306 Courtesy Barbara Banner MD
This high powered histological section is from the records of a patient with a pseudocyst. At the top of the image the white space represents the cyst lumen. The lining is made of fibrous tissue rather than an epithelium. A true cyst is lined by epithelial cells. 15306 Courtesy Barbara Banner MD
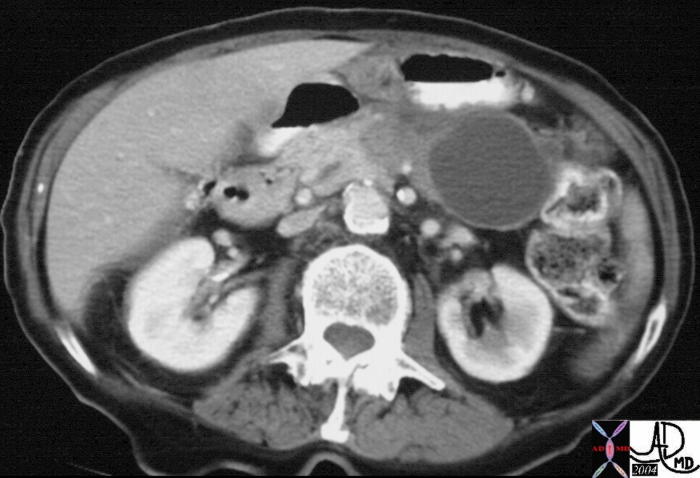
|
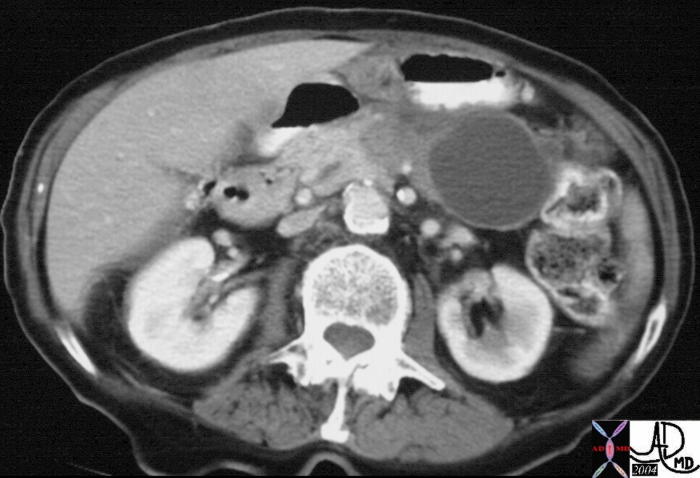
 The CTscan through the body of the pancreas is of a 74 year old female with abdominal discomfort. She has no history of alcohol abuse and a normal US of the gallbladder. The study shows a complex, bilocular, cystic lesion in the tail of the pancreas with an enhancing rind, and two focal peripheral punctate calcifications. A diagnosis of a mucinous cystadenoma is thought to be most likely. The CTscan through the body of the pancreas is of a 74 year old female with abdominal discomfort. She has no history of alcohol abuse and a normal US of the gallbladder. The study shows a complex, bilocular, cystic lesion in the tail of the pancreas with an enhancing rind, and two focal peripheral punctate calcifications. A diagnosis of a mucinous cystadenoma is thought to be most likely.
04811 Courtesy Ashley Davidoff MD
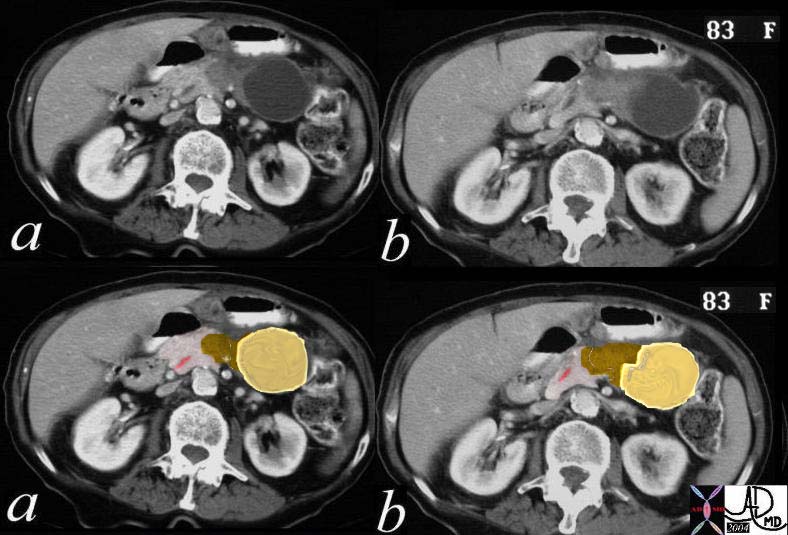
 This CTscan of an 83 year old female is through the body and tail of the pancreas shows a complex cystic mass that has a cystic component with a thickened wall and a solid component medially that has a focal calcification. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19907 Courtesy Ashley Davidoff MD This CTscan of an 83 year old female is through the body and tail of the pancreas shows a complex cystic mass that has a cystic component with a thickened wall and a solid component medially that has a focal calcification. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19907 Courtesy Ashley Davidoff MD
The following series expands the case above with color overlays.
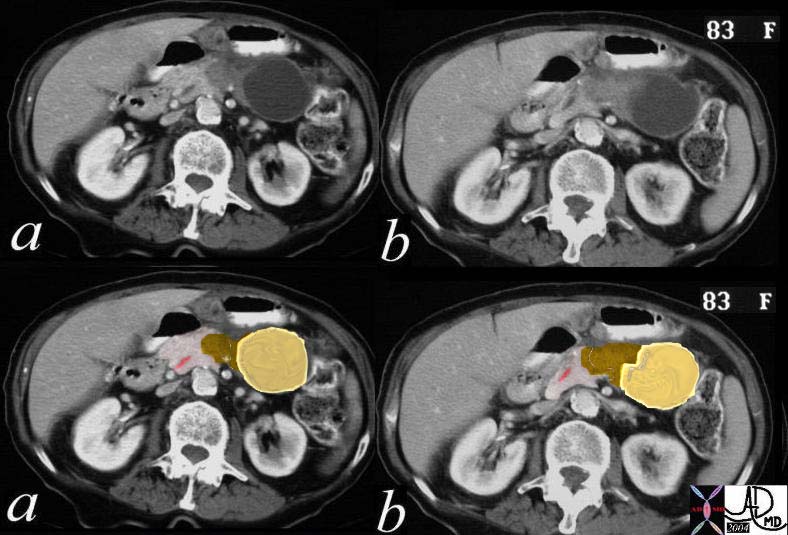 This CTscan of an 83 year old female is through the body and tail of the pancreas shows the complex cystic mass (a, b). In c and d, the cystic component with a thickened wall is shown in yellow, and the solid component medially with a focal calcification is shown in brown. The pancreatic duct which is minimally prominent is shown in pink. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19911c01b03 Courtesy Ashley Davidoff MD This CTscan of an 83 year old female is through the body and tail of the pancreas shows the complex cystic mass (a, b). In c and d, the cystic component with a thickened wall is shown in yellow, and the solid component medially with a focal calcification is shown in brown. The pancreatic duct which is minimally prominent is shown in pink. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19911c01b03 Courtesy Ashley Davidoff MD
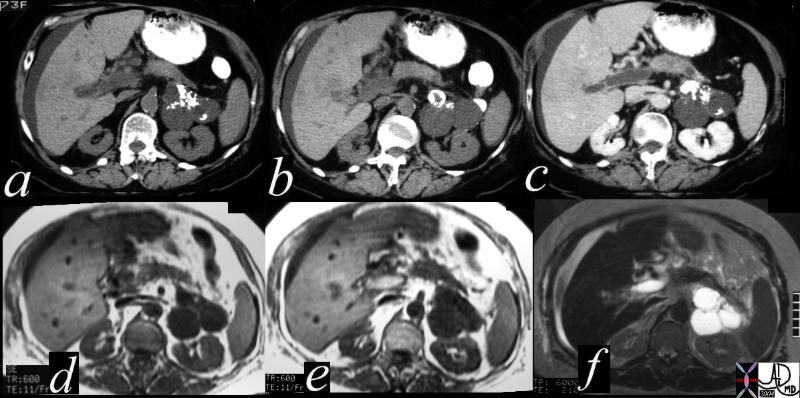
 This CT scan through the pancreas shows a complex bicystic mass with dense peripheral curvilinear and dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. These findings are consistent with a mucinous cystadenoma, and probable malignant transformation. 40712 Courtesy Ashley Davidoff MD. This CT scan through the pancreas shows a complex bicystic mass with dense peripheral curvilinear and dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. These findings are consistent with a mucinous cystadenoma, and probable malignant transformation. 40712 Courtesy Ashley Davidoff MD.
The following series expands the case above with the MRI findings.
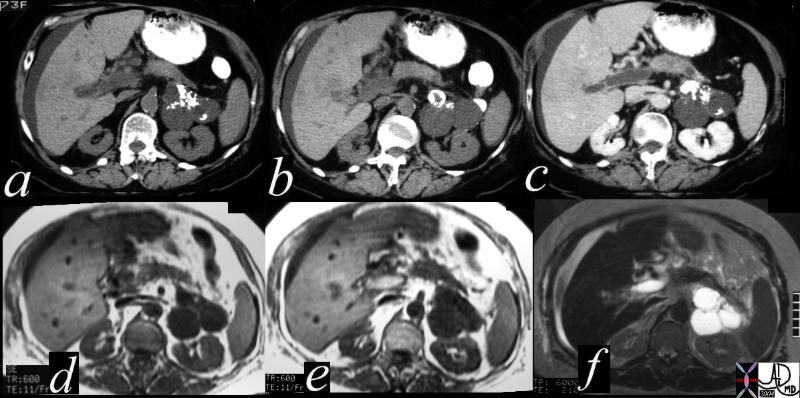 This CT scan through the pancreas (a,b,c) shows a complex cystic mass with dense peripheral dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. The cystic lesions on the T1 weighted image (d) are dark, and are bright on the T2 weighted image consistent with their cystic nature. The portal vein is bright on the T1 image and bright on T2 consistent with acute thrombus. These findings are consistent with a diagnosis of cystadenoma, and a malignant transformation of a mucinous neoplasm has to be considered in view of the PVT. 40717c Courtesy Ashley Davidoff MD This CT scan through the pancreas (a,b,c) shows a complex cystic mass with dense peripheral dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. The cystic lesions on the T1 weighted image (d) are dark, and are bright on the T2 weighted image consistent with their cystic nature. The portal vein is bright on the T1 image and bright on T2 consistent with acute thrombus. These findings are consistent with a diagnosis of cystadenoma, and a malignant transformation of a mucinous neoplasm has to be considered in view of the PVT. 40717c Courtesy Ashley Davidoff MD
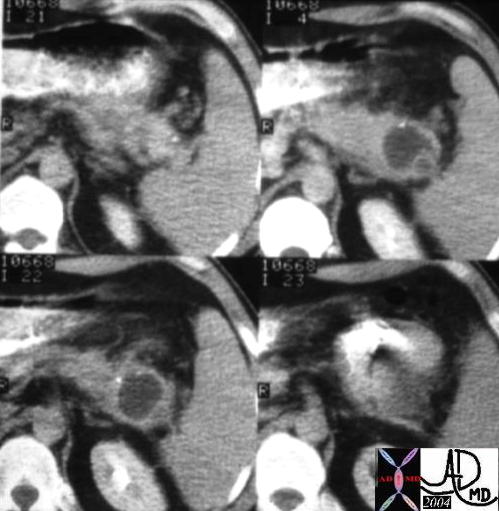
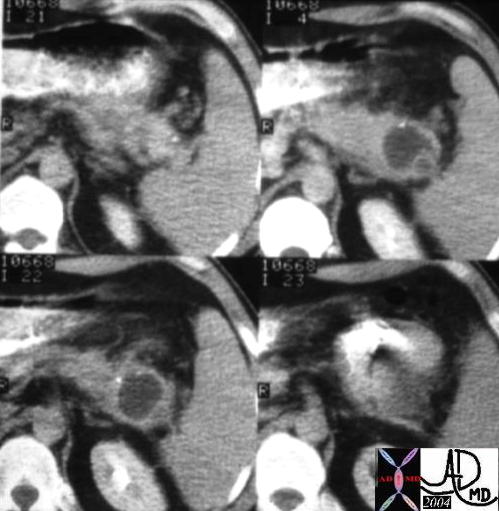
 This CT scan through the head of the pancreas shows a complex cystic mass with dense and thickened components best seen in the bottom right image. The lesion was biopsied and shown to be a cystadenocarcinoma. 40495c Courtesy Ashley Davidoff MD This CT scan through the head of the pancreas shows a complex cystic mass with dense and thickened components best seen in the bottom right image. The lesion was biopsied and shown to be a cystadenocarcinoma. 40495c Courtesy Ashley Davidoff MD
Intraductal Papillary Mucinous Tumor (IPMT) (aka mucinous duct ectasia)
Overview
This tumor is a slow growing papillary tumor that arises from the larger ducts and is characterized by the production of abundant mucus. It is usually a benign lesion but has a premalignant predisposition. They occur more commonly in men in their 7th decade and thus occur in a slightly older group than the mucinous cystadenomas, but the same age group as the serous cystadenomas.
Imaging
The lesion usually occurs in the head of the pancreas, and is associated with a dilated duct. It is suspected when the profuse mucus secretion is noted by the endoscopist.
 This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla.18143 Courtesy Ashley Davidoff MD This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla.18143 Courtesy Ashley Davidoff MD
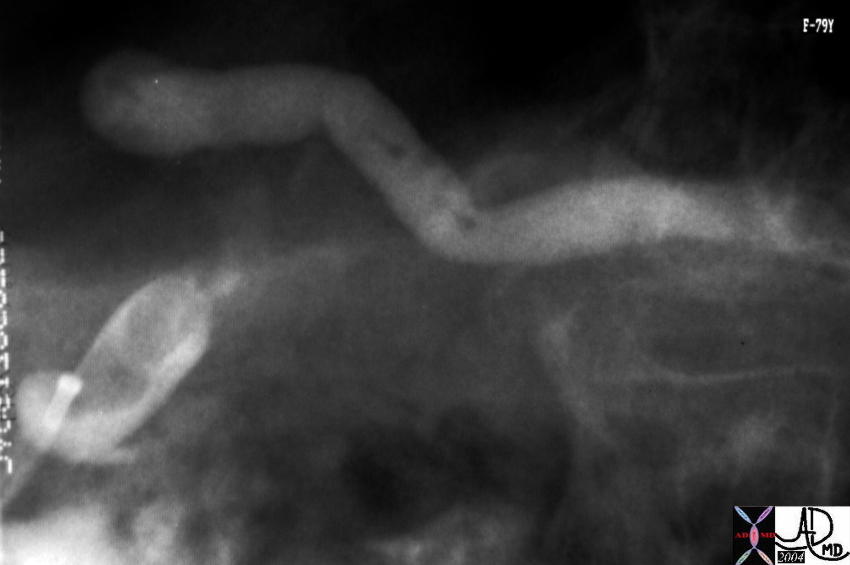
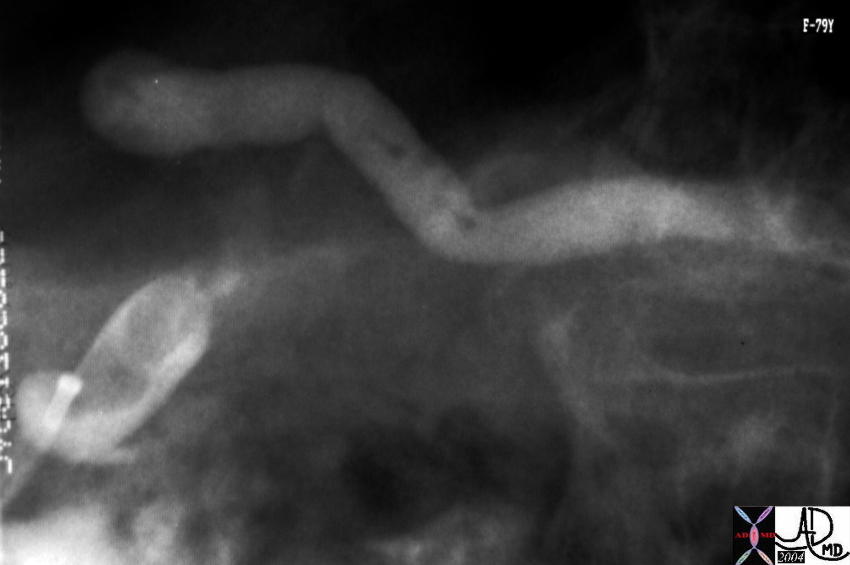 This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD
References
Suzuki Y, Atomi Y, Sugiyama M, Isaji S, Inui K, Kimura W, Sunamura M, Furukawa T, Yanagisawa A, Ariyama J, Takada T, Watanabe H, Suda K: Cystic neoplasm of the pancreas: a Japanese multiinstitutional study of intraductal papillary mucinous tumor and mucinous cystic tumor.
Pancreas 2004, 28(3):241-246. [PubMed Abstract][Publisher Full Text]
Thompson LD, Becker RC, Przygodzki RM, Adair CF, Heffess CS: Mucinous cystic neoplasm (mucinous cystadenocarcinoma of low-grade malignant potential) of the pancreas: a clinicopathologic study of 130 cases.
Am J Surg Pathol 1999, 23(1):1-16. [PubMed Abstract][Publisher Full Text]
Wilentz RE, Albores-Saavedra J, Hruban RH: Mucinous cystic neoplasms of the pancreas.
Semin Diagn Pathol 2000, 17(1):31-42. [PubMed Abstract]
Zamboni G, Scarpa A, Bogina G, Iacono C, Bassi C, Talamini G, Sessa F, Capella C, Solcia E, Rickaert F, Mariuzzi GM, Kloppel G: Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors.
Am J Surg Pathol 1999, 23(4):410-422. [PubMed Abstract][Publisher Full Text]
Kloppel G, Luttges J: WHO-classification 2000: exocrine pancreatic tumors.
Verh Dtsch Ges Pathol 2001, 85:219-228. [PubMed Abstract]
van den Berg W, Tascilar M, Offerhaus GJ, Albores-Saavedra J, Wenig BM, Hruban RH, Gabrielson E: Pancreatic mucinous cystic neoplasms with sarcomatous stroma: molecular evidence for monoclonal origin with subsequent divergence of the epithelial and sarcomatous components.
Mod Pathol 2000, 13(1):86-91. [PubMed Abstract][Publisher Full Text]
Web references
Khan AN MD e Medicine |
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] =>
[nodeName] => table
[nodeValue] =>
The CTscan through the body of the pancreas is of a 74 year old female with abdominal discomfort. She has no history of alcohol abuse and a normal US of the gallbladder. The study shows a complex, bilocular, cystic lesion in the tail of the pancreas with an enhancing rind, and two focal peripheral punctate calcifications. A diagnosis of a mucinous cystadenoma is thought to be most likely.
04811 Courtesy Ashley Davidoff MD
This CTscan of an 83 year old female is through the body and tail of the pancreas shows a complex cystic mass that has a cystic component with a thickened wall and a solid component medially that has a focal calcification. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19907 Courtesy Ashley Davidoff MD
The following series expands the case above with color overlays.
This CTscan of an 83 year old female is through the body and tail of the pancreas shows the complex cystic mass (a, b). In c and d, the cystic component with a thickened wall is shown in yellow, and the solid component medially with a focal calcification is shown in brown. The pancreatic duct which is minimally prominent is shown in pink. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19911c01b03 Courtesy Ashley Davidoff MD
This CT scan through the pancreas shows a complex bicystic mass with dense peripheral curvilinear and dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. These findings are consistent with a mucinous cystadenoma, and probable malignant transformation. 40712 Courtesy Ashley Davidoff MD.
The following series expands the case above with the MRI findings.
This CT scan through the pancreas (a,b,c) shows a complex cystic mass with dense peripheral dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. The cystic lesions on the T1 weighted image (d) are dark, and are bright on the T2 weighted image consistent with their cystic nature. The portal vein is bright on the T1 image and bright on T2 consistent with acute thrombus. These findings are consistent with a diagnosis of cystadenoma, and a malignant transformation of a mucinous neoplasm has to be considered in view of the PVT. 40717c Courtesy Ashley Davidoff MD
This CT scan through the head of the pancreas shows a complex cystic mass with dense and thickened components best seen in the bottom right image. The lesion was biopsied and shown to be a cystadenocarcinoma. 40495c Courtesy Ashley Davidoff MD
Intraductal Papillary Mucinous Tumor (IPMT) (aka mucinous duct ectasia)
Overview
This tumor is a slow growing papillary tumor that arises from the larger ducts and is characterized by the production of abundant mucus. It is usually a benign lesion but has a premalignant predisposition. They occur more commonly in men in their 7th decade and thus occur in a slightly older group than the mucinous cystadenomas, but the same age group as the serous cystadenomas.
Imaging
The lesion usually occurs in the head of the pancreas, and is associated with a dilated duct. It is suspected when the profuse mucus secretion is noted by the endoscopist.
This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla.18143 Courtesy Ashley Davidoff MD
This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD
References
Suzuki Y, Atomi Y, Sugiyama M, Isaji S, Inui K, Kimura W, Sunamura M, Furukawa T, Yanagisawa A, Ariyama J, Takada T, Watanabe H, Suda K: Cystic neoplasm of the pancreas: a Japanese multiinstitutional study of intraductal papillary mucinous tumor and mucinous cystic tumor.
Pancreas 2004, 28(3):241-246. [PubMed Abstract][Publisher Full Text]
Thompson LD, Becker RC, Przygodzki RM, Adair CF, Heffess CS: Mucinous cystic neoplasm (mucinous cystadenocarcinoma of low-grade malignant potential) of the pancreas: a clinicopathologic study of 130 cases.
Am J Surg Pathol 1999, 23(1):1-16. [PubMed Abstract][Publisher Full Text]
Wilentz RE, Albores-Saavedra J, Hruban RH: Mucinous cystic neoplasms of the pancreas.
Semin Diagn Pathol 2000, 17(1):31-42. [PubMed Abstract]
Zamboni G, Scarpa A, Bogina G, Iacono C, Bassi C, Talamini G, Sessa F, Capella C, Solcia E, Rickaert F, Mariuzzi GM, Kloppel G: Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors.
Am J Surg Pathol 1999, 23(4):410-422. [PubMed Abstract][Publisher Full Text]
Kloppel G, Luttges J: WHO-classification 2000: exocrine pancreatic tumors.
Verh Dtsch Ges Pathol 2001, 85:219-228. [PubMed Abstract]
van den Berg W, Tascilar M, Offerhaus GJ, Albores-Saavedra J, Wenig BM, Hruban RH, Gabrielson E: Pancreatic mucinous cystic neoplasms with sarcomatous stroma: molecular evidence for monoclonal origin with subsequent divergence of the epithelial and sarcomatous components.
Mod Pathol 2000, 13(1):86-91. [PubMed Abstract][Publisher Full Text]
Web references
Khan AN MD e Medicine
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
The CTscan through the body of the pancreas is of a 74 year old female with abdominal discomfort. She has no history of alcohol abuse and a normal US of the gallbladder. The study shows a complex, bilocular, cystic lesion in the tail of the pancreas with an enhancing rind, and two focal peripheral punctate calcifications. A diagnosis of a mucinous cystadenoma is thought to be most likely.
04811 Courtesy Ashley Davidoff MD
This CTscan of an 83 year old female is through the body and tail of the pancreas shows a complex cystic mass that has a cystic component with a thickened wall and a solid component medially that has a focal calcification. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19907 Courtesy Ashley Davidoff MD
The following series expands the case above with color overlays.
This CTscan of an 83 year old female is through the body and tail of the pancreas shows the complex cystic mass (a, b). In c and d, the cystic component with a thickened wall is shown in yellow, and the solid component medially with a focal calcification is shown in brown. The pancreatic duct which is minimally prominent is shown in pink. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19911c01b03 Courtesy Ashley Davidoff MD
This CT scan through the pancreas shows a complex bicystic mass with dense peripheral curvilinear and dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. These findings are consistent with a mucinous cystadenoma, and probable malignant transformation. 40712 Courtesy Ashley Davidoff MD.
The following series expands the case above with the MRI findings.
This CT scan through the pancreas (a,b,c) shows a complex cystic mass with dense peripheral dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. The cystic lesions on the T1 weighted image (d) are dark, and are bright on the T2 weighted image consistent with their cystic nature. The portal vein is bright on the T1 image and bright on T2 consistent with acute thrombus. These findings are consistent with a diagnosis of cystadenoma, and a malignant transformation of a mucinous neoplasm has to be considered in view of the PVT. 40717c Courtesy Ashley Davidoff MD
This CT scan through the head of the pancreas shows a complex cystic mass with dense and thickened components best seen in the bottom right image. The lesion was biopsied and shown to be a cystadenocarcinoma. 40495c Courtesy Ashley Davidoff MD
Intraductal Papillary Mucinous Tumor (IPMT) (aka mucinous duct ectasia)
Overview
This tumor is a slow growing papillary tumor that arises from the larger ducts and is characterized by the production of abundant mucus. It is usually a benign lesion but has a premalignant predisposition. They occur more commonly in men in their 7th decade and thus occur in a slightly older group than the mucinous cystadenomas, but the same age group as the serous cystadenomas.
Imaging
The lesion usually occurs in the head of the pancreas, and is associated with a dilated duct. It is suspected when the profuse mucus secretion is noted by the endoscopist.
This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla.18143 Courtesy Ashley Davidoff MD
This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD
References
Suzuki Y, Atomi Y, Sugiyama M, Isaji S, Inui K, Kimura W, Sunamura M, Furukawa T, Yanagisawa A, Ariyama J, Takada T, Watanabe H, Suda K: Cystic neoplasm of the pancreas: a Japanese multiinstitutional study of intraductal papillary mucinous tumor and mucinous cystic tumor.
Pancreas 2004, 28(3):241-246. [PubMed Abstract][Publisher Full Text]
Thompson LD, Becker RC, Przygodzki RM, Adair CF, Heffess CS: Mucinous cystic neoplasm (mucinous cystadenocarcinoma of low-grade malignant potential) of the pancreas: a clinicopathologic study of 130 cases.
Am J Surg Pathol 1999, 23(1):1-16. [PubMed Abstract][Publisher Full Text]
Wilentz RE, Albores-Saavedra J, Hruban RH: Mucinous cystic neoplasms of the pancreas.
Semin Diagn Pathol 2000, 17(1):31-42. [PubMed Abstract]
Zamboni G, Scarpa A, Bogina G, Iacono C, Bassi C, Talamini G, Sessa F, Capella C, Solcia E, Rickaert F, Mariuzzi GM, Kloppel G: Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors.
Am J Surg Pathol 1999, 23(4):410-422. [PubMed Abstract][Publisher Full Text]
Kloppel G, Luttges J: WHO-classification 2000: exocrine pancreatic tumors.
Verh Dtsch Ges Pathol 2001, 85:219-228. [PubMed Abstract]
van den Berg W, Tascilar M, Offerhaus GJ, Albores-Saavedra J, Wenig BM, Hruban RH, Gabrielson E: Pancreatic mucinous cystic neoplasms with sarcomatous stroma: molecular evidence for monoclonal origin with subsequent divergence of the epithelial and sarcomatous components.
Mod Pathol 2000, 13(1):86-91. [PubMed Abstract][Publisher Full Text]
Web references
Khan AN MD e Medicine
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 48
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The CTscan through the body of the pancreas is of a 74 year old female with abdominal discomfort. She has no history of alcohol abuse and a normal US of the gallbladder. The study shows a complex, bilocular, cystic lesion in the tail of the pancreas with an enhancing rind, and two focal peripheral punctate calcifications. A diagnosis of a mucinous cystadenoma is thought to be most likely.
04811 Courtesy Ashley Davidoff MD
This CTscan of an 83 year old female is through the body and tail of the pancreas shows a complex cystic mass that has a cystic component with a thickened wall and a solid component medially that has a focal calcification. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19907 Courtesy Ashley Davidoff MD
The following series expands the case above with color overlays.
This CTscan of an 83 year old female is through the body and tail of the pancreas shows the complex cystic mass (a, b). In c and d, the cystic component with a thickened wall is shown in yellow, and the solid component medially with a focal calcification is shown in brown. The pancreatic duct which is minimally prominent is shown in pink. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19911c01b03 Courtesy Ashley Davidoff MD
This CT scan through the pancreas shows a complex bicystic mass with dense peripheral curvilinear and dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. These findings are consistent with a mucinous cystadenoma, and probable malignant transformation. 40712 Courtesy Ashley Davidoff MD.
The following series expands the case above with the MRI findings.
This CT scan through the pancreas (a,b,c) shows a complex cystic mass with dense peripheral dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. The cystic lesions on the T1 weighted image (d) are dark, and are bright on the T2 weighted image consistent with their cystic nature. The portal vein is bright on the T1 image and bright on T2 consistent with acute thrombus. These findings are consistent with a diagnosis of cystadenoma, and a malignant transformation of a mucinous neoplasm has to be considered in view of the PVT. 40717c Courtesy Ashley Davidoff MD
This CT scan through the head of the pancreas shows a complex cystic mass with dense and thickened components best seen in the bottom right image. The lesion was biopsied and shown to be a cystadenocarcinoma. 40495c Courtesy Ashley Davidoff MD
Intraductal Papillary Mucinous Tumor (IPMT) (aka mucinous duct ectasia)
Overview
This tumor is a slow growing papillary tumor that arises from the larger ducts and is characterized by the production of abundant mucus. It is usually a benign lesion but has a premalignant predisposition. They occur more commonly in men in their 7th decade and thus occur in a slightly older group than the mucinous cystadenomas, but the same age group as the serous cystadenomas.
Imaging
The lesion usually occurs in the head of the pancreas, and is associated with a dilated duct. It is suspected when the profuse mucus secretion is noted by the endoscopist.
This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla.18143 Courtesy Ashley Davidoff MD
This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD
References
Suzuki Y, Atomi Y, Sugiyama M, Isaji S, Inui K, Kimura W, Sunamura M, Furukawa T, Yanagisawa A, Ariyama J, Takada T, Watanabe H, Suda K: Cystic neoplasm of the pancreas: a Japanese multiinstitutional study of intraductal papillary mucinous tumor and mucinous cystic tumor.
Pancreas 2004, 28(3):241-246. [PubMed Abstract][Publisher Full Text]
Thompson LD, Becker RC, Przygodzki RM, Adair CF, Heffess CS: Mucinous cystic neoplasm (mucinous cystadenocarcinoma of low-grade malignant potential) of the pancreas: a clinicopathologic study of 130 cases.
Am J Surg Pathol 1999, 23(1):1-16. [PubMed Abstract][Publisher Full Text]
Wilentz RE, Albores-Saavedra J, Hruban RH: Mucinous cystic neoplasms of the pancreas.
Semin Diagn Pathol 2000, 17(1):31-42. [PubMed Abstract]
Zamboni G, Scarpa A, Bogina G, Iacono C, Bassi C, Talamini G, Sessa F, Capella C, Solcia E, Rickaert F, Mariuzzi GM, Kloppel G: Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors.
Am J Surg Pathol 1999, 23(4):410-422. [PubMed Abstract][Publisher Full Text]
Kloppel G, Luttges J: WHO-classification 2000: exocrine pancreatic tumors.
Verh Dtsch Ges Pathol 2001, 85:219-228. [PubMed Abstract]
van den Berg W, Tascilar M, Offerhaus GJ, Albores-Saavedra J, Wenig BM, Hruban RH, Gabrielson E: Pancreatic mucinous cystic neoplasms with sarcomatous stroma: molecular evidence for monoclonal origin with subsequent divergence of the epithelial and sarcomatous components.
Mod Pathol 2000, 13(1):86-91. [PubMed Abstract][Publisher Full Text]
Web references
Khan AN MD e Medicine
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The CTscan through the body of the pancreas is of a 74 year old female with abdominal discomfort. She has no history of alcohol abuse and a normal US of the gallbladder. The study shows a complex, bilocular, cystic lesion in the tail of the pancreas with an enhancing rind, and two focal peripheral punctate calcifications. A diagnosis of a mucinous cystadenoma is thought to be most likely.
04811 Courtesy Ashley Davidoff MD
This CTscan of an 83 year old female is through the body and tail of the pancreas shows a complex cystic mass that has a cystic component with a thickened wall and a solid component medially that has a focal calcification. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19907 Courtesy Ashley Davidoff MD
The following series expands the case above with color overlays.
This CTscan of an 83 year old female is through the body and tail of the pancreas shows the complex cystic mass (a, b). In c and d, the cystic component with a thickened wall is shown in yellow, and the solid component medially with a focal calcification is shown in brown. The pancreatic duct which is minimally prominent is shown in pink. These findings are consistent with a mucinous cystadenocarcinoma which was pathologically proven. 19911c01b03 Courtesy Ashley Davidoff MD
This CT scan through the pancreas shows a complex bicystic mass with dense peripheral curvilinear and dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. These findings are consistent with a mucinous cystadenoma, and probable malignant transformation. 40712 Courtesy Ashley Davidoff MD.
The following series expands the case above with the MRI findings.
This CT scan through the pancreas (a,b,c) shows a complex cystic mass with dense peripheral dystrophic calcification in the tail of the pancreas. Associated findings include portal vein thrombosis (PVT) and ascites. The cystic lesions on the T1 weighted image (d) are dark, and are bright on the T2 weighted image consistent with their cystic nature. The portal vein is bright on the T1 image and bright on T2 consistent with acute thrombus. These findings are consistent with a diagnosis of cystadenoma, and a malignant transformation of a mucinous neoplasm has to be considered in view of the PVT. 40717c Courtesy Ashley Davidoff MD
This CT scan through the head of the pancreas shows a complex cystic mass with dense and thickened components best seen in the bottom right image. The lesion was biopsied and shown to be a cystadenocarcinoma. 40495c Courtesy Ashley Davidoff MD
Intraductal Papillary Mucinous Tumor (IPMT) (aka mucinous duct ectasia)
Overview
This tumor is a slow growing papillary tumor that arises from the larger ducts and is characterized by the production of abundant mucus. It is usually a benign lesion but has a premalignant predisposition. They occur more commonly in men in their 7th decade and thus occur in a slightly older group than the mucinous cystadenomas, but the same age group as the serous cystadenomas.
Imaging
The lesion usually occurs in the head of the pancreas, and is associated with a dilated duct. It is suspected when the profuse mucus secretion is noted by the endoscopist.
This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla.18143 Courtesy Ashley Davidoff MD
This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD
References
Suzuki Y, Atomi Y, Sugiyama M, Isaji S, Inui K, Kimura W, Sunamura M, Furukawa T, Yanagisawa A, Ariyama J, Takada T, Watanabe H, Suda K: Cystic neoplasm of the pancreas: a Japanese multiinstitutional study of intraductal papillary mucinous tumor and mucinous cystic tumor.
Pancreas 2004, 28(3):241-246. [PubMed Abstract][Publisher Full Text]
Thompson LD, Becker RC, Przygodzki RM, Adair CF, Heffess CS: Mucinous cystic neoplasm (mucinous cystadenocarcinoma of low-grade malignant potential) of the pancreas: a clinicopathologic study of 130 cases.
Am J Surg Pathol 1999, 23(1):1-16. [PubMed Abstract][Publisher Full Text]
Wilentz RE, Albores-Saavedra J, Hruban RH: Mucinous cystic neoplasms of the pancreas.
Semin Diagn Pathol 2000, 17(1):31-42. [PubMed Abstract]
Zamboni G, Scarpa A, Bogina G, Iacono C, Bassi C, Talamini G, Sessa F, Capella C, Solcia E, Rickaert F, Mariuzzi GM, Kloppel G: Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors.
Am J Surg Pathol 1999, 23(4):410-422. [PubMed Abstract][Publisher Full Text]
Kloppel G, Luttges J: WHO-classification 2000: exocrine pancreatic tumors.
Verh Dtsch Ges Pathol 2001, 85:219-228. [PubMed Abstract]
van den Berg W, Tascilar M, Offerhaus GJ, Albores-Saavedra J, Wenig BM, Hruban RH, Gabrielson E: Pancreatic mucinous cystic neoplasms with sarcomatous stroma: molecular evidence for monoclonal origin with subsequent divergence of the epithelial and sarcomatous components.
Mod Pathol 2000, 13(1):86-91. [PubMed Abstract][Publisher Full Text]
Web references
Khan AN MD e Medicine
)
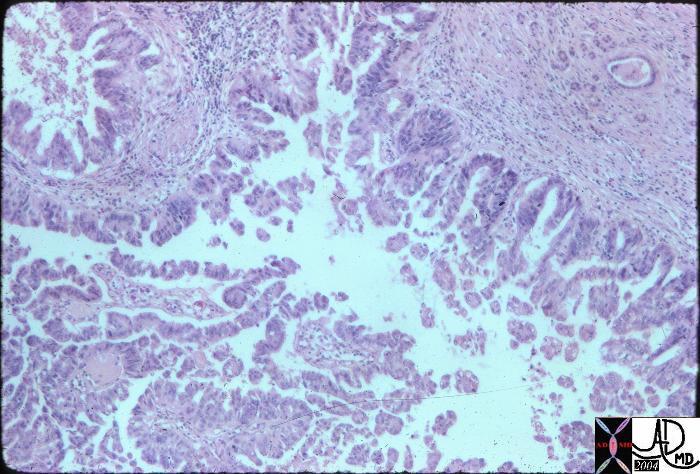 Papillary fronds and a simple columnar mucus epithelium characterizes the histology of the mucinous cystadenoma. The subepithelial layer consists of prominent cellular components and the outer layer consists of hyalinized connective tissue. 15318 Courtesy Barbara Banner MD
Papillary fronds and a simple columnar mucus epithelium characterizes the histology of the mucinous cystadenoma. The subepithelial layer consists of prominent cellular components and the outer layer consists of hyalinized connective tissue. 15318 Courtesy Barbara Banner MD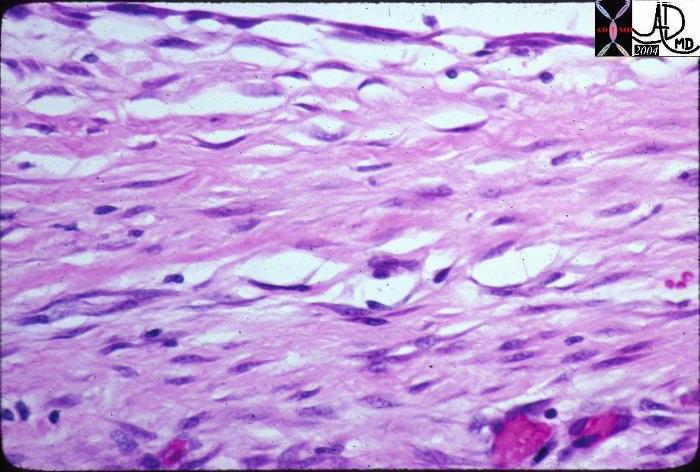 This high powered histological section is from the records of a patient with a pseudocyst. At the top of the image the white space represents the cyst lumen. The lining is made of fibrous tissue rather than an epithelium. A true cyst is lined by epithelial cells. 15306 Courtesy Barbara Banner MD
This high powered histological section is from the records of a patient with a pseudocyst. At the top of the image the white space represents the cyst lumen. The lining is made of fibrous tissue rather than an epithelium. A true cyst is lined by epithelial cells. 15306 Courtesy Barbara Banner MD