Pelvic Pain
Specific reference to Pelvic Pain in Women
The Common Vein Copyright 2008
Barry Giglio MD
Ashley Davidoff MD
Definition
Pelvic pain is an uncomfortable painful sensation felt in the pelvis. Pelvic pain is a common gynecological complaint, and can be broadly classified as cyclic, acute, cyclic, or chronic. There are many causes for pelvic pain, with results that range from spontaneous resolution to some such as ruptured ectopic pregnancy that can be life threatening. The clinical diagnosisis often suspected clinically and imaging with ultrasound is the most commonly used modality in gynecological considerations. Treatment ranges from medical where pain control is the aim, to surgical where mechanical disorders such as obstructions and ruptures are the etiology.
Background
Non traumatic adult female pelvic pain is an extremely common entity, but it is difficult to ascertain an exact prevalence as it is felt that many women who experience pelvic pain do not seek medical care. One estimate of chronic pelvic pain ranged between 4-25% of all women of child rearing ages.
Classification
Female pelvic pain can be divided into acute, chronic, and cyclical depending on the character and timing of the pain. Cyclic pain is associated with menses and occurs either during the menses or the middle of the cycle when ovulation takes place. Acute pelvic pain is intense, characterized by sudden onset, sharpcharacter, and relatively short course. It is often accompanied by nausea, vomiting, diaphoresis, fever or leukocytosis. Chronic pelvic pain persists for greater than 3-4 months, and is typically less intense in severity (although not always).
Structural Principles
The pelvis is a highly vascularized area comprised mostly of the reproductive organs and a multitude of lumbar and sacral nerve plexi. Due to its anatomical proximity to the abdominal viscera, pelvic pain may often reflect an abdominal process.
The reproductive organs, the uterus, fallopian tubes, and ovaries, share the same nerves as lower gastrointestinal organs, including the sigmoid colon and rectum (spinal cord segments T10 through L1). This can sometimes make it difficult to differentiate pain originating from the GI tract versus that from the reproductive tract.
Pelvic Cavity
The pelvic cavity, is the space formed by a diaphragm of pelvic muscle below and an open roof above where the distinction between the pelvic cavity and abdominal cavity is vague but best defined by the region of the bony pelvis, including the iliac crests and lumbosacral joint and sacral promontory and the pubic symphisis. It houses the uterus, ovaries and Fallopian tubes, the bladder and distal ureters, prostate vasa deferentia, sigmoid colon and rectum. Components of the cardiovascular system, nervous system, endocrine system, reticuloendothelial system, and musculoskeletal system are present to enable the pelvic cavity to connect with all the other parts of the body.
Similar to the cranial cavity and the thoracic cavity, there is prominent bony protection by the pelvic bones.
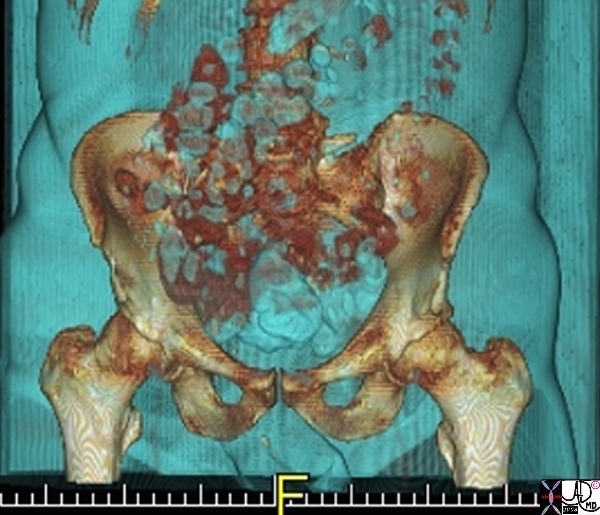
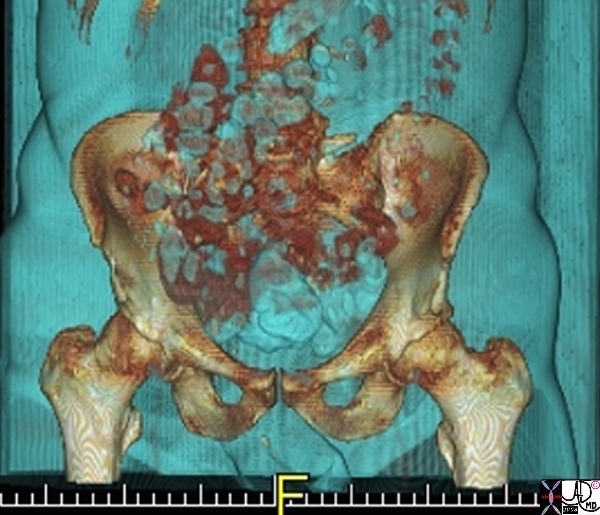
The Normal Pelvis |
| The bony pelvis is shown in the above CT scan reconstruction. While the iliac crests and ischia and pubic symphisis are well shown, the sacral component is hidden by parts of the gastrointestinal tract.
71198b01 pelvis bone iliac crest pubic symphisis hip ischial tuberosity pubic bone normal anatomy CTscan 3D Courtesy Ashley Davidoff MD copyright 2008 |
Spaces in the Pelvis
Most of the pelvic cavity is part of the peritoneal cavity but the retroperitoneum does extend down into the pelvic cavity and there is also a space called the extraperitoneal space.
Space Occupation
Diseases and fluid accumulation can occupy space in the pelvis in the same way as they may in the abdominal cavity. Similarly the space occupation is not usually immediately and emergently life threatening. The cul de sac is a space that in the female lies between the rectum and uterus, and in the male lies between the bladder and the rectum. It is the most posterior space in the abdominal-pelvic cavity, and therefore by default is the the first space to accumulate fluid when the patient is imaged in the supine projection.
Space occupation is sometimes (though rarely) a welcoming event. In the case of the pelvis, the gravid uterus occupies space in the pelvis and although progressively uncomfortable, the final result is not only desirable but also restores the space to its usual owners.
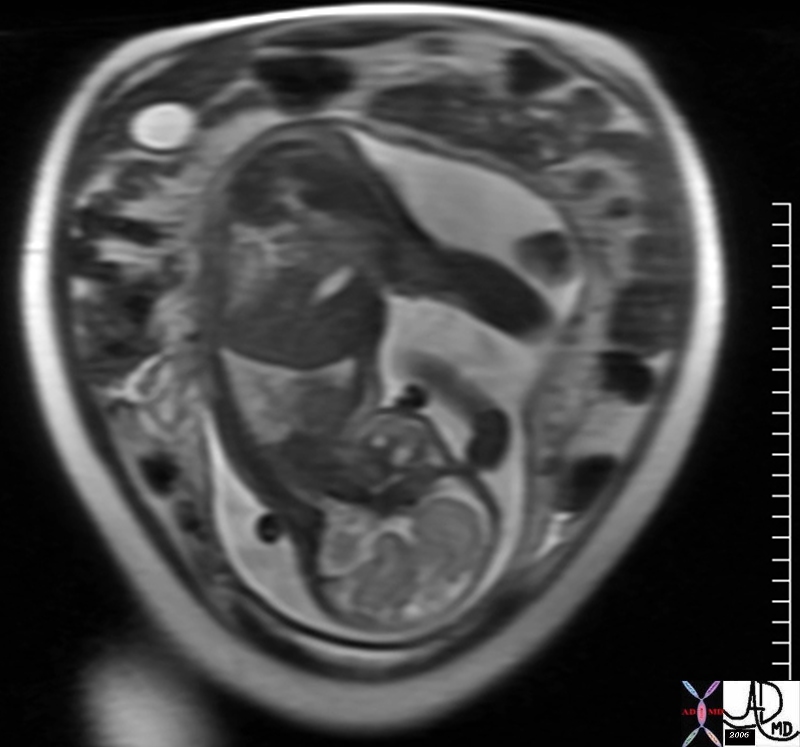
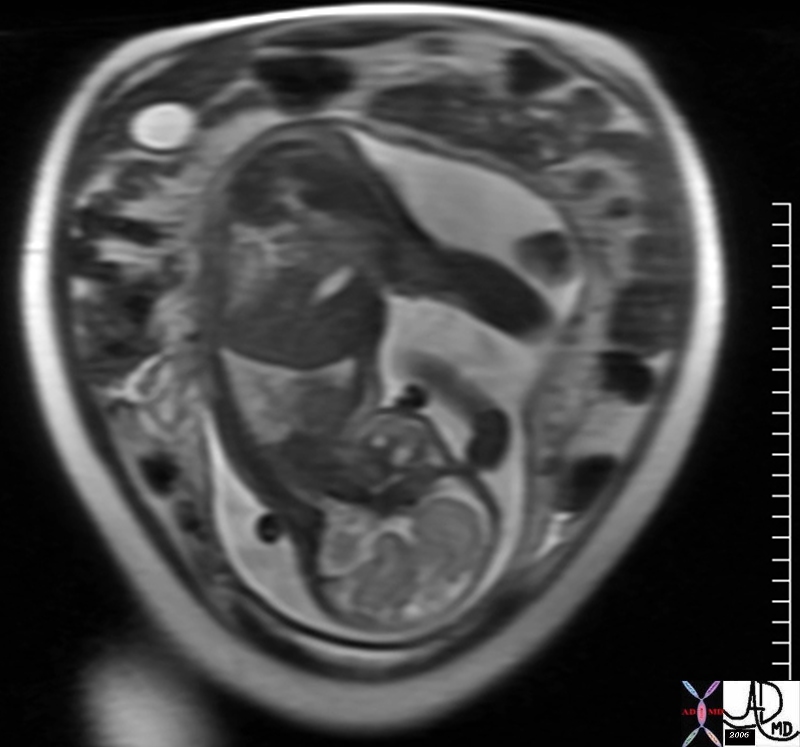
Pregnancy – Physiological and Temporary Space Occupation |
| The MRI shows a fetus with vertex (head) presentation lying within the gestational sac filled with fluid (white), taking up the space of the pelvic cavity and to some extent the abdominal cavity and displacing normal structures into the abdomen.
46704 abdomen pregnancy fetus baby head brain lungs amniotic cavity amniotic fluid normal anatomy physiology MRI T2 weighted Davidoff MD |
When referring to pelvic pain it is usual to assign this condition to females since pelvic pain is so common as a normal physiological event for so many females. We will focus on the female system primarily.
Female Reproductive Organs
The female organs of reproduction include the uterus, Fallopian tubes, ovaries, and vagina. Three of the four organs are hollow. The Fallopian tubes, vagina and uterus follow tubular principles, while the ovaries are considered solid organs. The tubular systems all have an inner mucosal lining a wall containing muscle and an outer capsule.
Uterus
The uterus or womb is part of the female reproductive system and part of the genitourinary tract. It is characterized by its function as a primary reproductive organ that bears the responsibility of carrying the pregnancy through to term. At term it utilizes its muscular abilities to expel the mature baby into the world.
Structurally in the non gravid state, the mature uterus is about the size of a woman’s fist, and measures about 8cms X 6cms X 4cms with a volume of about 75-200ccs, and it weighs 100-200gms. It is pear shaped and is situated between the bladder anteriorly and the rectum posteriorly. It is a muscular organ with a hollow endometrial cavity. It consists of a fundus, body (corpus), and neck (cervix).
Histologically the inner endometrial lining consists of a single layer of columnar cells supported by a thin layer of connective tissue, the middle layer is the thickest and is called the myometrium. It consists of smooth muscle. There is a loose connective tissue layer next which is called the perimetrium and then the outer lining is called the peritoneum.
Functionally it is built to receive the ovum via the Fallopian tubes and the sperm via the cervix, facilitates fertilization and provides subsequent housing for the developing fetus . It enables the implantation of the placenta, soas to facilitate nutritional needs for the fetus, and subsequently functions to expel the mature baby through the vagina into the world.
The cyclical changes of the menstrual cycle present a continual change of events controlled by a series of integrated hormonal events. During the follicular phase (proliferative phase) which occurs in the first half of the cycle, and after the shedding of the endometrial lining, there is a rise in estrogen which causes the endometrial lining to start to thicken. In mid cycle after ovulation, luteinizing hormone is released, which heralds in the luteal phase (aka secretory phase). Progesterone now rises and further proliferation of the endometrium occurs. In the absence of pregnancy progesterone levels and estrogen levels fall, and the endometrium sheds.
The most common structural diseases of the uterus that may cause pain include fibroid disease, polyps, adenomyosis, cervical stenosis, and carcinoma. The more common disorders are the functional disorders that relate to cyclical events including menstrual cramps, endometriosis, dysmenorhea, amenorhea, menorhagia. Pain relating to the placement of and intrauterine device is also relatively common.
The diagnosis is dependent on clinical evaluation, while the most useful imaging modality is ultrasound.
Treatment is dependant on the cause of disease, but includes both medical and surgical techniques.

The Normal Uterus During Follicular (Proliferative) Phase |
| The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The pearshaped structure, wirth fundus to the left of the image and lower uterine segment measures 8.7cms in length. The endometrial stripe is seen in the center as an echogenic line and measures about 5mms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008 |
 The Normal Uterus End of Luteal (Secretory) Phase The Normal Uterus End of Luteal (Secretory) Phase |
| The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008 |

The Normal Uterus End of Luteal (Secretory) Phase
|
| The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008 |
The Ovaries
The pair of ovaries or female gonads, are egg producing organs that are connected loosely to the Fallopian tubes and are partof the female reproductive system and part of the genitourinary tract. They are characterized mostly by their cyclical function and monthly production usually of a single ovum.
Structurally they are characterized by their almond shape, and measure approximately 3 X 1.5 X 1.5 cms. They are positioned on either side of the uterus as part of the adnexa in the peritoneal cavity, and are found close the lateral wall of the pelvis, though they are mobile and their position changes. They are covered and supported by the mesovarium. Unlike most organs their epithelium is on the outside and is called the germinal epithelium The deeper layers are called the ovarian cortex and medulla. The cortex contains follicles, aging corpus lutea, corpora albuginea, and a fibrous stroma. The medulla only has a stroma.
Functionally the ovaries are the source of the ova and each ovary usually produces one ovum every second month. They are subjected to the same hormonal influences as the uterus. During the proliferative phase (follicular phase), the follicles develop, and one of the follicles usually becomes dominant under the influence of estrogen. At mid cycle, there is an LH surge causing the dominant follicle to rupture and release its egg. Thereafter progesterone rises in the luteal phase (secretory phase) and the ruptured follicle becomes a corpus luteum. If pregnancy ensues the corpus luteum functions as an early endocrine organ to support the early pregnancy until the placenta takes over. If there is no pregnancy then the corpus luteum degenerates.
The common diseases that affect the ovary include cysts, hemorrhagic cysts, endometriosis, and carcinoma. Less common are torsion and metastases. Ectopic pregnancy more commonly involves the adnexa and and Fallopian tubes. Pain with ovulation is quite common and has been given the name mittelschmerz – the German word for “middle pain” that affects about 20% of women – which for some women is every cycle and for others an intermittent symptom.
The diagnosis of ovarian disease requires the combination of meticulous clinical evaluation and ultrasound .
Treatment of disease depends on the cause and includes both medical and surgical techniques.

The Almond
|
| The almond not only has the same shape as the ovary, but also has almost the same size.
82470.81s fruit nut food food in the body shape almond ovary amygdala Davidoff photography copyright 2008 |

Normal Ovary with Follicles
|
| The transvaginal ultrasound shows a normal right ovary in longitudinal view containing black cystic follicles that are all about the same size and are all less than 1cms in diameter.
71689 ovary follicles normal anatomy function physiology TCV Applied Biology Cycle time USscan Davidoff MD |
Fallopian Tubes
The Fallopian tubes (aka salpinges, oviducts) are a pair of tubular structures that are part of the female reproductive system and also part of the genitourinary system. They are characterized by their delicate and gracile nature and functional importance in fertilization.
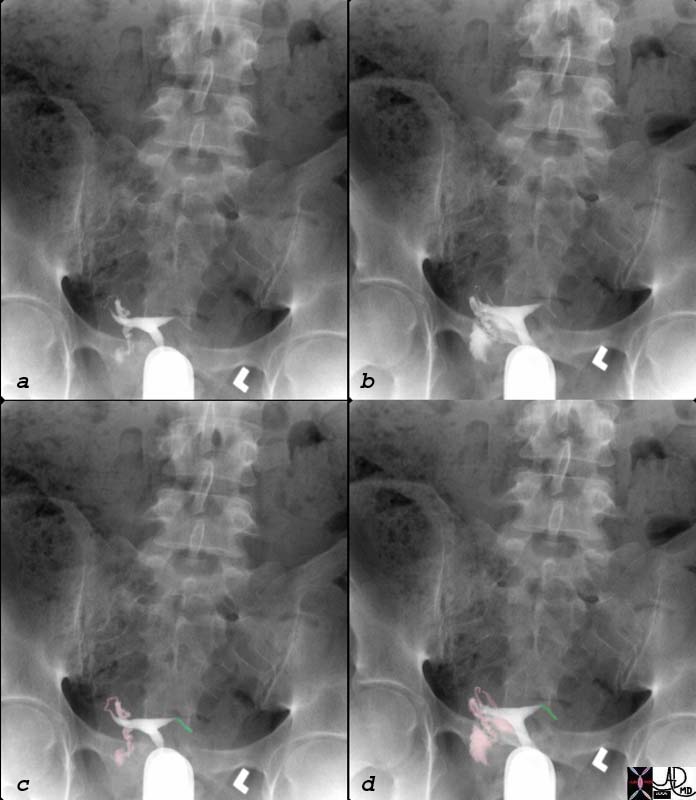
 Hysterosalpingogram Fallopian Tubes Hysterosalpingogram Fallopian Tubes |
| 46376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MDpelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MD |
Functional Principles relating to Pain Syndrome
The cyclical changes of the female reproductive system involves dramatic monthly events. Each month the entire endometrium sheds into the endometrial cavity creating strong expulsion waves that can be the source of pain.
In addition in the middle of the month a rupture of a follicle with its contents extrudes both the ovum and its contents into the peritoneal cavity. Even although the cyst is in the 2cms range and the volume of fluid is small, if there is hemorrhage then this can cause significant pain either by enlarging the cyst which in fact may not rupture and pain is caused by distension, (mechanoreceptors), or by rupture and hemorrhage causing sudden distension in a space (mechanoreceptors) or by irritation on the omentum (chemoreceptors).
Blood flow increases to the pelvis and pelvic organs during the cycle and congestive changes can also create aberrant and uncomfortable feeling including pain (mechanoreceptors).
The cyclical changes of hormones and particulalrly estrogen have been incriminated in the softening on pelvic ligaments that can create lower back pain and pelvic pain.
Most of the pain arises from visceral mechanoreceptors where distension of the hollow organs causes the pain and discomfort. In the inflammatory diseases, inflammatory mediators lower the threshold for the pain as well as induce pain by causing swelling, and congestion. Visceral pain in general is a dull deep ache that is poorly localized and often referred. When the process spreads to somatic structures like the peritoneum, then the pain can become more somatic, and thus acute, sharp, and well localized.
The visceral pain sensations travel along sympathetic afferents in first order neurons and the somatic afferents travel in the peripheral nerves in first order neurons. They both synapse in the dorsal horn of the spinal cord, cross into the contralateral spinothalamic tract, and become second order neurons which travel to the thalamus. The third order neurons leave the thalamus and connect with the somatosensory cortex, limbic and autonomic nervous systems enabling the perception of the pain sensation, and also enabling reactions to the pain to take place on a visceral and emotional level.
Functional Disorders and Diseases
 Acute Debilitating Pelvic Pain – Artistic Rendition Acute Debilitating Pelvic Pain – Artistic Rendition |
| 89081pd04b09.8s pain abdomen sleep woken awakened from sleep somatic peritoneal peritonitis Davidoff art copyright 2008 |
The female pelvis contains many important organs and structures. Portions of the gastrointestinal tract, urinary tract, as well as reproductive tract are located within the Pelvis. Several of the causes of female pelvic pain involve the derangement in the arrangement of these structures. The diseases that can cause pelvic pain are innumerable. We will introduce this section with a classification of the entities that can cause the pain and then will provide some detail on the specifics of each entity.
Cyclical Pain
Cyclical pelvic pain can be caused by;
menstrual cramps
endometriosis,
mittelschmerz
dysmenorrhea
premenstrual disorders.
Acute Pelvic Pain
There are both gynecological causes of acute pelvic pain and non gynecological of acute pelvic pain
Gynecologic Causes
Common gynecologic causes of acute pelvic pain include
hemorrhagic ovarian cyst
endometriosis
pelvic inflammatory disease
endometritis
ectopic pregnancy
spontaneous abortion
adnexal torsion
degeneration or hemorrhage into a uterine fibroid
Non Gynecological Causes
Non gynecologic causes of acute pelvic pain include;
GI issues
appendicitis
diverticulitis
constipation
Musculoskeletal issues
muscle strain
diastasis of the symphysis pubis
Urinary issues
acute cystitis
kidney stones and ureterolithiasis
Chronic Pain
gynecological
endometriosis
adhesions
fibroids
urinary tract issues
interstitial cystitis
gastrointestinal issues
irritable bowel syndrome
constipation
musculoskeletal and neurological issues
mental health issues.
We will now explain in more detail the causes and manifestations of each of the pain syndromes and will start off with t cyclical pains
Menstrual Cramps – Dysmenorrhea
Menstrual cramps or dysmenorrhea are cramps that occur during the menses or more simply painful menstruation. They are caused by uterine muscle contractions which serve to evacuate the denuded mucosa and blood clots from the endometrial cavity. Primary dysmenorrhea is more common but dysmenorrhea may be associated with other pelvic disorders such as endometriosis, adenomyosis, PID, and adhesions, in which case the dysmenorrhea may be more severe or prolonged.
Many women experience tolerable discomfort or pain but when the pain can become incapacitating. Dysmenorrhea may be associated with excessive blood loss and this is known as menorrhagia.
From a structural standpoint the pain is caused by pressure receptors that sense the increased pressure during muscle contractions, or by chemical receptors that may be incited by ischemia when contractions are excessive and temporary ischemia results.
Functionally muscle contractions of the uterus are normal and are usually not felt. If the contractions are sufficiently strong, pressure receptors are activated or ischemia is induced by obstruction of the intramural arteries, causing the pain.
Clinically the pain presents as cramps dusing the menses in the lower abdomen, usually in the suprapubic region but may be periumbilical, left or right abdomen, or may radiate down the thighs or occur in the back. Associate symptoms include nausea vomiting, headache, weakness or even fainting. If the pain pattern changes or becomes more severe, or the pelvic examination is abnormal then secondary causes should be sought and is best done by starting with an ultrasound of the pelvis.
Treatment is commonly with NSAIDS (Non steroidal anti inflammatory agents) or a COX-2 inhibitor. For some patients hormonal contraceptives prove effective. Secondary causes of dysmenorrhea may require surgery.
 Denuded Endometrium Denuded Endometrium |
| The longitudinal view of the uterus is shown in the ultrasound of this young patient who was having severe pain during her menses. The images show part of the endometrial lining within the lumen (maroon), with a small amount of blood (bright red), and the remaining endometrium lining (pink). The denuded endometrium and associated clots cause prostaglandins to be released which induce muscle contraction, and these are the primary cause of the pain.
83218c02.8s 42F pain during menses menstrual cycle cyclical pain uterus endometrium shedding of the endometrium contraction expulsion menstrual cramps US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008 |
Endometriosis
Endometriosis is a disease of the endometrial lining caused by misplaced or ectopic endometrial tissues that are located beyond the uterus and usually results in pelvic pain.
It occurs in 5-10% of women. When endometrial tissue is located outside of the uterus, it can cause pelvic and back pain as well as dyspareunia. The potential of endometrial tissue to be deneuded into the peritoneal cavity is based on the connection of the cavity with the peritoneal space via the fallopian tubes.
From a structural standpoint, endometriosis commonly affects the ovaries but also can affect the broad ligaments, fallopian tubes, uterosacral ligaments, cul de sac, or other locations in the pelvis or abdomen, including the ureters and the bowel serosa. Endometriosis is rarely more far reaching including the kidneys, brain, diaphragm, and pleura. When it involves the iaphragm or pleura, shoulder pain may be associated with the entity. Catamenial pneumothorax is pneumothorax induced by the menstrual cycle and implies endometriosis of the pleura.
The nodules can be red-blue to yellow-brown in color, (chocolate cysts) occur just below the serosa of the organ to which they are attached. As the lesions undergo recurrent hemorrhage, they can become associated with fibrosis.
Clinically the entity more commonly occurs in nulliparous women and the degree of pain is variable. As endometrial tissue it is responsive to the cyclical hormonal fluxes and thus may bleed in response to hormonal changes and so pain commonly occurs at the time of the menses. The volume of ectopic endometrial tissue does not correlate with the severity of the pain. The pain is usually recurring and commonly but not necessarily occurs during the menses. With induction of fibrosis, pain may be caused by other structural changes that are unrelated to the menses.
Diagnosis is suspected clinically and confirmed by ultrasound or MRI. Endometriomas have a characteristic appearance. Microscopic deposits which may cause symptoms may not be identified by imaging techniques and may only be seen laparoscopically.
Treatment options depend on patient preference, including whether fertility is desired, but include both medical and surgical options. Medical management frequently involves suppression of regular menses/hormones and surgical options typically attempt to remove endometrial tissue or surgical menopause (i.e. oophorectomy and hysterectomy).
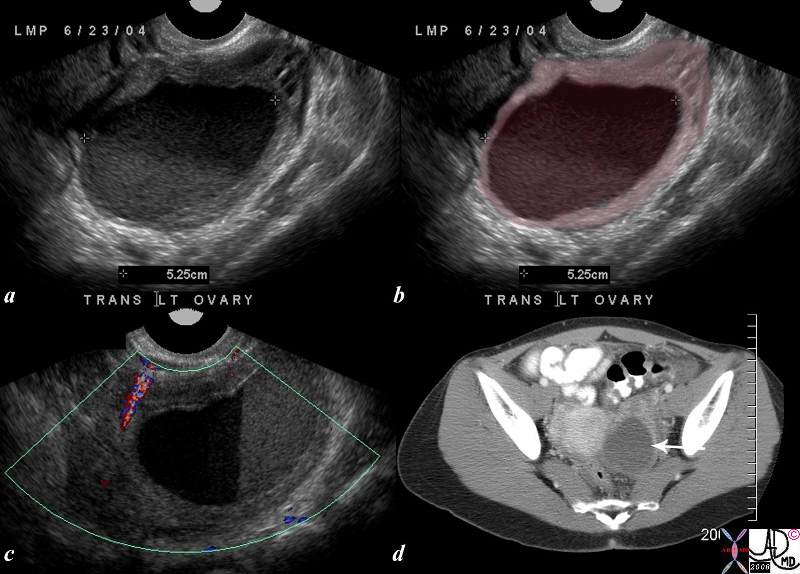
Endometrioma Left Ovary |
| 25 year old female presents with painful menses. The ultrasound shows a cystic mass in the pelvis with a large amount of debris in the cystic cavity consistent with a chocolate cyst. Although the appearance is consistent with endometriosis, a hemorrhagic cycts is possible and the distiction may only be made pathologicallly
uterus pain ovary hemorrhagic cyst endometrioma 83261c01.8s |
Adenomyosis
Adenomyosis is a disease of the endometrial lining caused by misplaced or ectopic endometrial tissues that are located within the uterus and results in pelvic pain and uterine enlargement. The exact cause of the displacement is not known but it is presumed that a breach in the endometrial myometrial barrier enable a small amount of endometrium to translocate and remain viable.
Clinically the patient presents with dysmenorrhea and menorrhagia and on exam the uterus is enlarged.
The diagnosis is best made by MRI which shows a thickened junctional zone (>10-12mms) of the uterus The deposition of acute blood, blood degradation products such as iron, or the the presence of fluid filled microglandular deposits in the junctional zone make the MRI findings highly specific for the diagnosis.
Treatment options include pain management with NSAIDS, hormonal manipulation. Surgery and hysterectomy is the only current option for cure.
Mittelschmerz
Mittelschmerz is the Gernam word for “middle pain” and refers to the lower abdominal and pelvic discomfort associated with ovulation, which occurs in the middle of the menstrual cycle. The cause of the pain may be due to the actual follicle rupturing, follicular distension, the contraction of the fallopian tube, or the release of blood/fluid from the ruptured follicle into the abdominal or pelvic cavity.
From a structural point of view it usually is considered a visceral pain caused by stimulation of pressure receptors in the ovary, but the proximity and intimate relationship of the ovary to the peritoneum and release of fluid and blood into the peritoneal cavity may cause irritation of chemical receptors in the peritoneum, inciting somatic like pain.
Functionally it is a cruel mechanism that allows awomen ao mark the time for potential fertilization, or on the other hand to abstain from intercourse if fertilization is not desirable.
Clinically the pain classically occurs in the middle of the month, lasts between 6-8 hours but may last up to 2-3 days, occurs suddenly, is situated on one or other side of the pelvis, in the midline or sometimes in the back, usually is ill defined and is either cramp like or a deep discomfort. It is not considered a disease state but can sometimes be quite uncomfortable.
The diagnosis rests on the timing of the pain, and the usual pattern of an individual woman, though each cyle can be uniquely different. One may be suspicious of other disorders if the pain is more severe or lasts longer than usual, or if a mass is palpated on pelvic examination.
Ultrasound is recommended if the pain is not classical or if a mass is felt, in order to exclude other causes such as a large unruptured cyst, hemorhagic cyst, blood in the peritoneum, endometriosis, ectopic pregnancy, or torsion.
Management generally is supportive and reassurance. If necessary, pain can be managed with NSAIDs (non steroidal anti-inflammatories) such as ibuprofen.
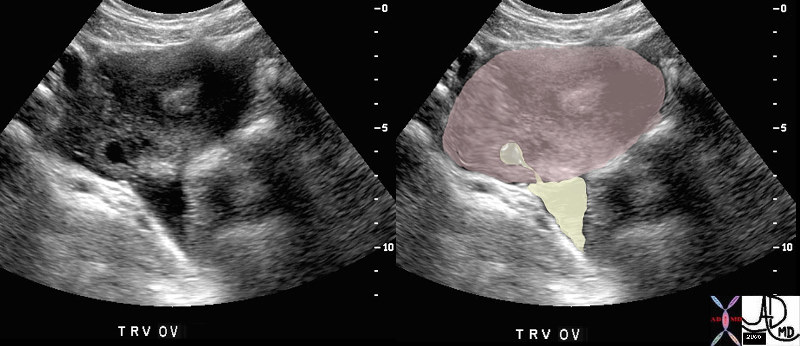
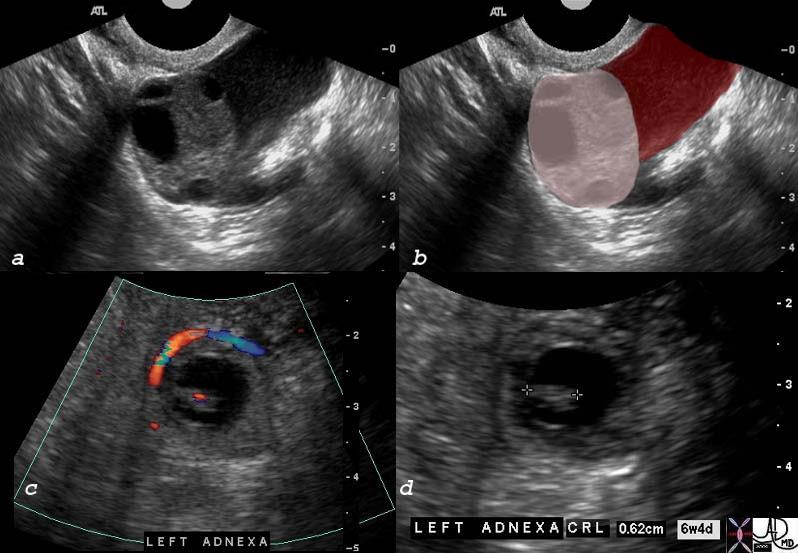
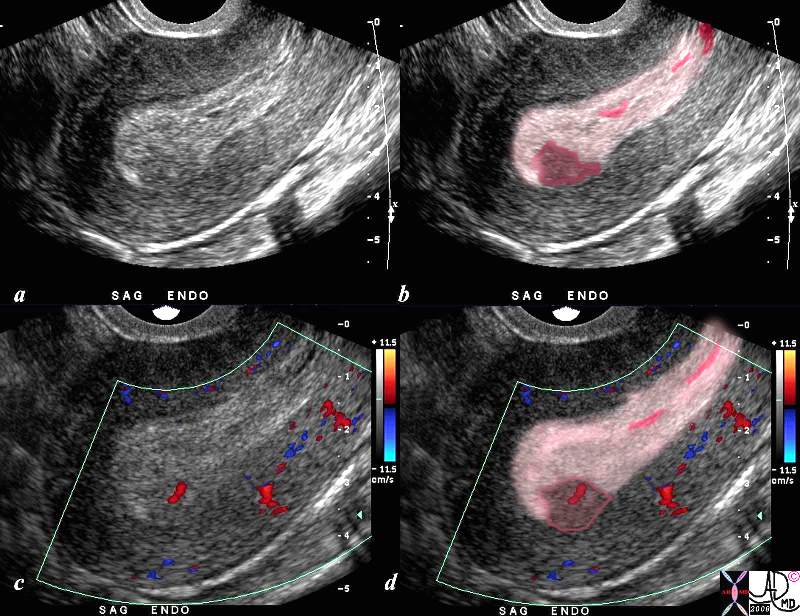
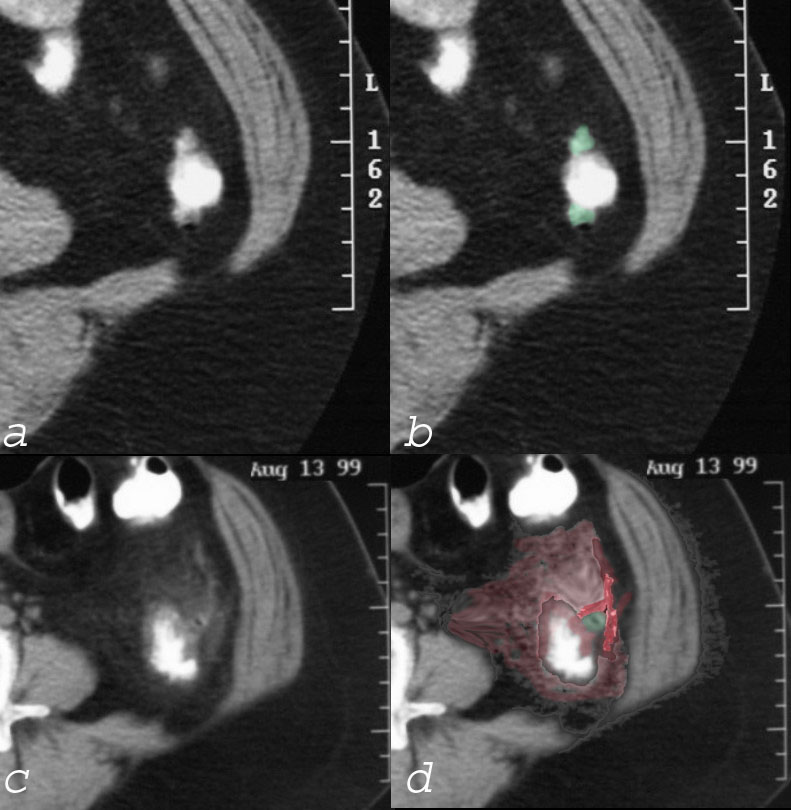
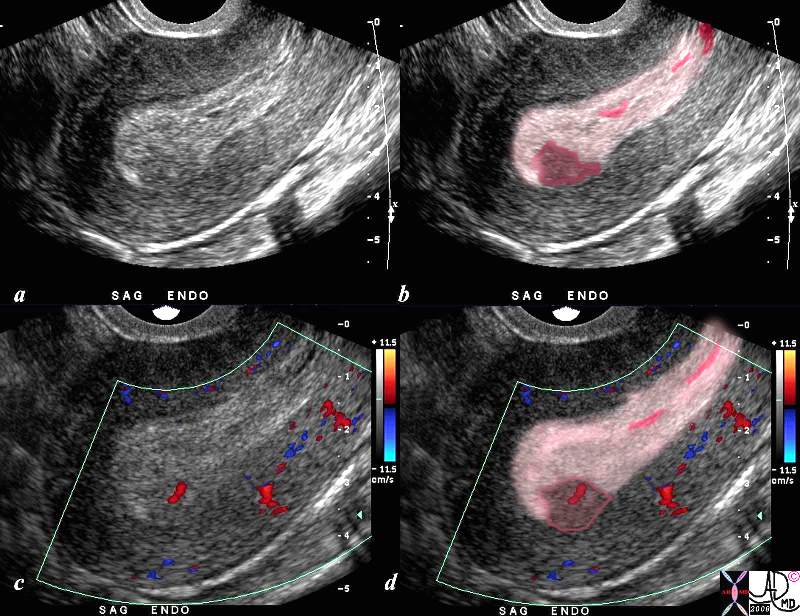
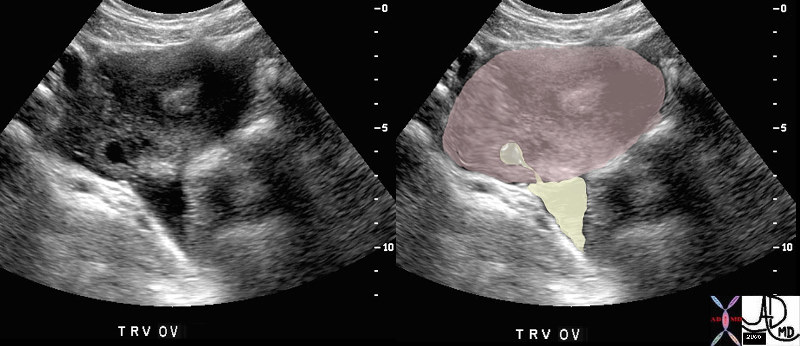 Ovulation and Mittelschmerz Ovulation and Mittelschmerz |
| The transvaginal ultrasound focuses on the ovary (pink oval structure) of a young woman who was complaining of midcycle pain. A decompressed Graaffian follicle (inverted teardrop shaped yellow structure in the ovary) is seen emptying its contents into the peritoneal cavity, causing a triangular shaped accumulation of fluid in the peritoneal cavity (yellow triangle). It is the shape of the follicle and its proximity to the fluid in the peritoneum together with the concordant site of the pain that allowed the diagnosis of mittelschmerz to be made.
47025c01 young patient with known ovulation one day earlier ovary Graafian follicle rupture tear drop shape pear shaped ovulation physiology normal anatomy USscan Davidoff MD |
Premenstrual Disorder
Premenstrual Disorder or Syndrome (PMS) is a group of systemic and local manifestations of the late phase (luteal or proliferative) part of the cycle thought to be caused by abnormal sensitivity to the fluctuation of estrogen and progesterone levels, serotonin deficiency, magnesium or calcium deficiency resulting in by physical psychological and behavioral changes.
Clinically symptoms occur a few days prior to menstruation and can involve abdominal and pelvic pain as well as mood changes. Mood changes include irritability, anxiety and depression. Physical symptoms can include bloating/fluid retention, breast tenderness, headaches, and muscle or joint pain.
The treatment of PMS frequently requires a multidisciplinary approach including medical and non medical treatments. Non medical approaches include emphasizing regular exercise and adequate nutrition and sleep. Medical management includes SSRI (selective serotonin re-uptake inhibitor) and antidepressants.
Gynecological Causes
Ovarian Cysts
Ovarian cysts (follicles) are normal evolutions of the menstrual cycle but in certain instances the cyst physiology is altered for unknown reasons, causing the cyst to enlarge unusually, rupture in a different manner, or become hemorrhagic, resulting in a pain syndrome.
A variety of situations manifest structurally including;
Follicular rupture – mittelschmerz
Enlargement of the follicle without rupture
Hemorrhage into the follicle/cyst without rupture
Hemorrhage into the follicle/cyst with rupture
Hemorrhage into an endometrioma simulating hemorrhage into a follicle usually without rupture
The common result is a pain syndrome that commonly occurs in midcycle.
Physiologically, during each menstrual cycle, a normally functioning ovary produces multiple cysts called graafian follicles. During the middle of the cycle, one cyst dominates and releases an egg. The follicle then becomes the corpus luteum, which can mature to measure up to 2 cm. If fertilization does not occur, the corpus luteum fibroses and is resorbed. If fertilization does occur, the corpus luteum matures and enlarges initially, but later shrinks during pregnancy. Ovarian cysts can be either follicular or luteal, and may respond to gonadotropins (including FSH).
Clinically the pain is different from mittelschmerz in that it may be more severe, prolonged, or with a different character. Sometimes the pain can simulate peritonitis. Most importantly from a diagnostic standpoint, is that a mass is usually felt on clinical examination.
The diagnosis is confirmed by ultrasound which usually shows a cystic mass in the adnexa. The cyst is either larger than the usual follicle, contains hemorrhage, or hemorrhage and large amounts of fluid are noted free in the pelvic cavity. When the patient presents with peritonism, a CTscan is usually indicated and in the case of a ruptured cyst, induration of the greater omentum or proximity of the bleed to the anterior peritoneum is recognized together with the hemorrhagic cyst. When an ovarian cyst ruptures, there is usually minimal blood loss.
Treatment depends on several factors. In most patients, the treatment is conservative with pain management being central to the care. Surgery may be indicated if the cyst does not go away after several periods or is enlarging. In a post menopausal woman, when complex cysts are identified cyclical disease is not a consideration and malignant disease must be suspected.
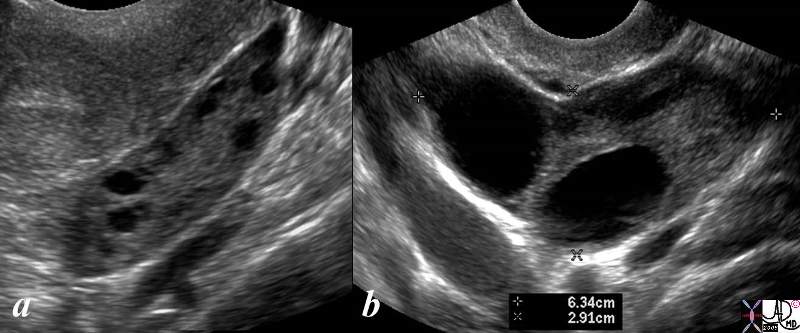
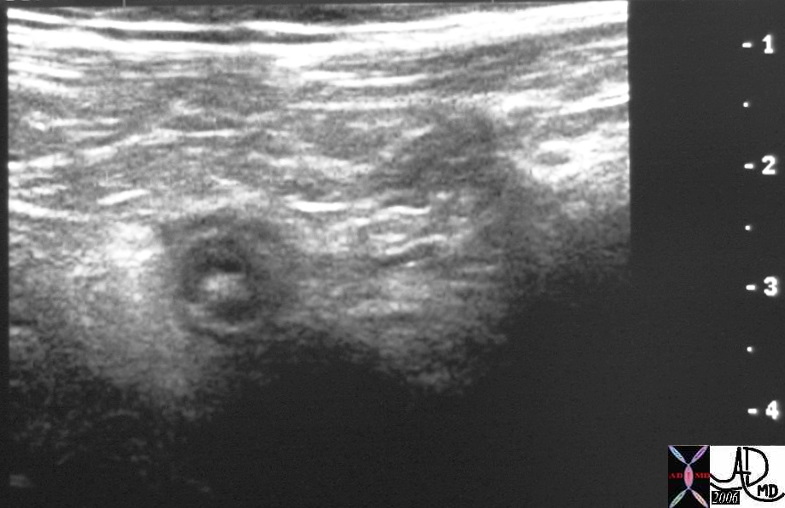
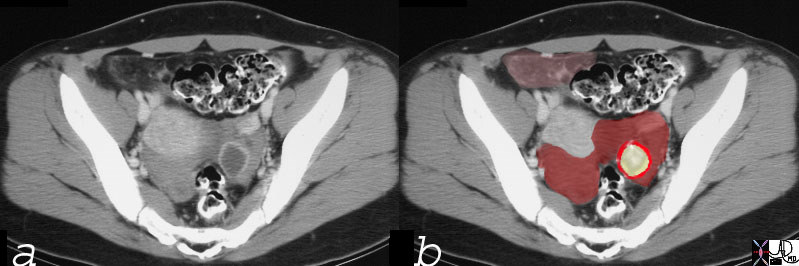
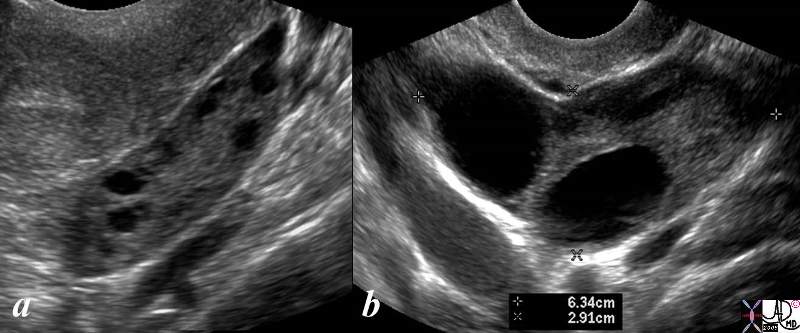 Normal (a) and Large Unruptured Follicles (b) Normal (a) and Large Unruptured Follicles (b) |
| The ultrasound shows a normal left ovary with small Graaffian follicles (a) and an enlarged ovary with two unruptured simple cysts (b) The latter study is from is from a 46 year female who presents with pelvic discomfort. The transvaginal ultrasound (b) shows a large 6cms ovary that contains two cysts each about 2cms in size.. The ovary is about twice to 3 times normal in size and the distension presumably causes the discomfort. The cysts are simple in nature without hemorrhage.
ovary pain cysts discomfort nrmal variant enlarged normal follicles USscan ultrasound copyright 2008 Courtesy Ashley Davidoff MD 83269c.8s |
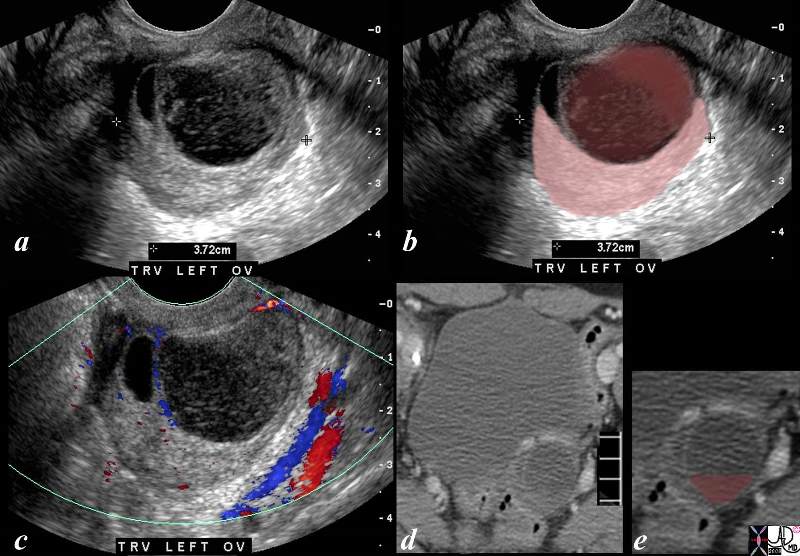
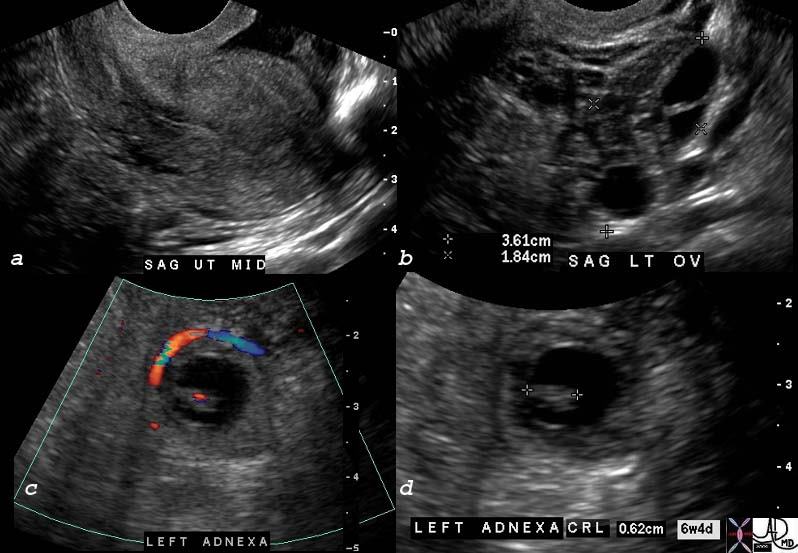
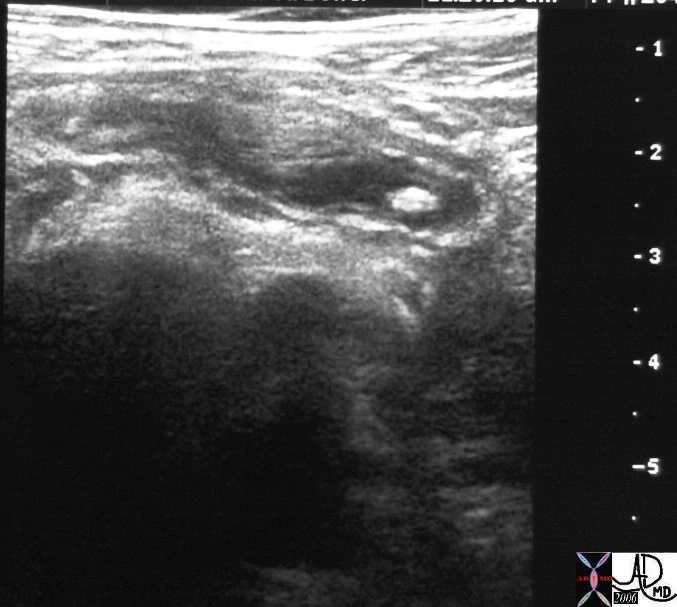
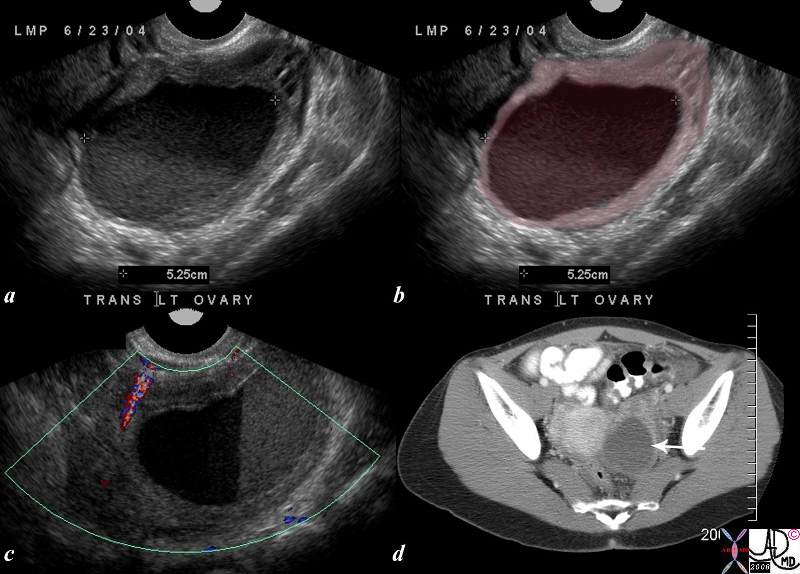
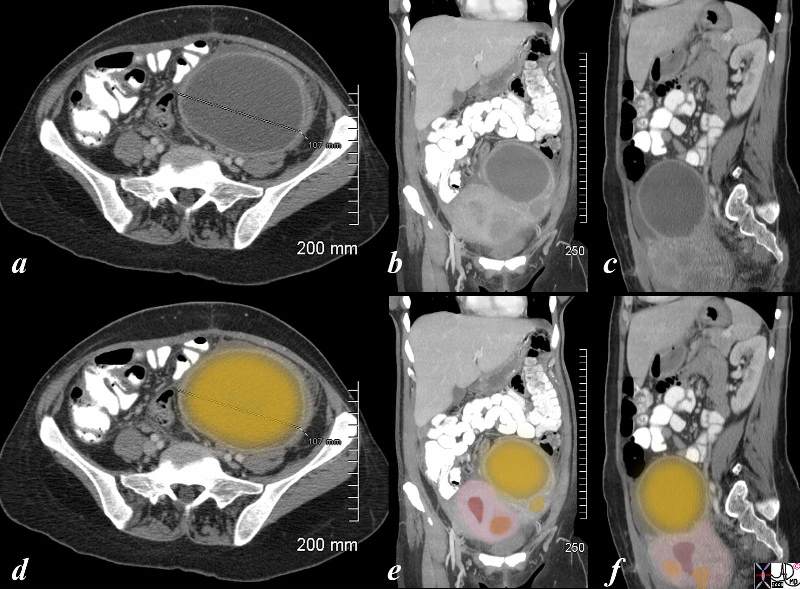
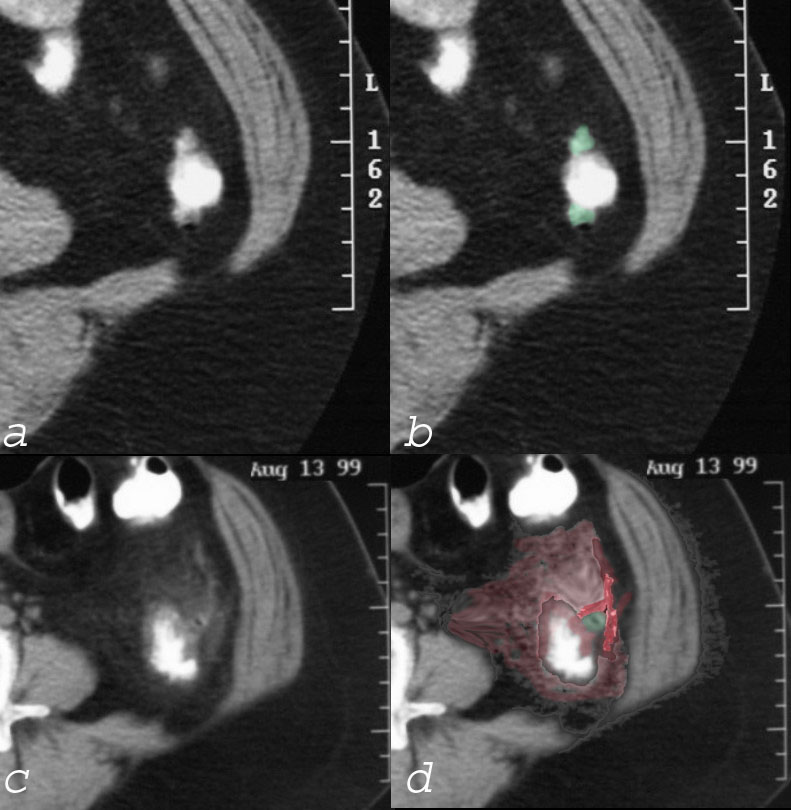
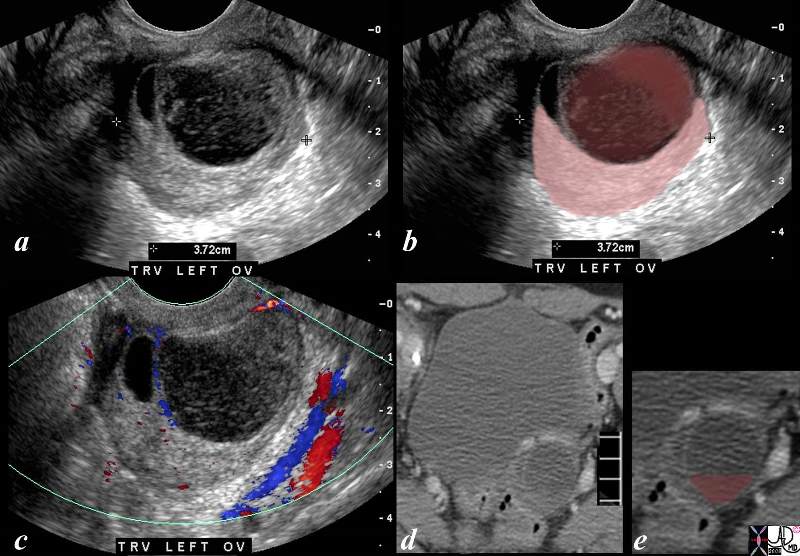 Hemorrhage into a Cyst with Clot Formation Hemorrhage into a Cyst with Clot Formation |
| The ultrasound (a,b,c) and CTscan (d,e) are from a 39year old female with midcycle pain and show linear stranding and soft tissue changes into a large cyst in the left adnexa (a and b), with the hemorrhage outlined in maroon in b and displaced crescentic ovary in pink. The hemorrhage consists of soft tissue components (dark maroon in b) and the lighter maroon overlies the fibrinous and linear component of the clot that is better visualized in a. The doppler study in c, shows no color in the cyst implying that it is a non vascular structure. These findings are most characteristic of a cyst that has hemorrhaged into the cyst but without rupture of the cyst. The sudden distension of the cyst incites the pressure receptors and accounts for the pain.
The CTscan limoited to the bladder and left adnexa in d, shows a rounded complex lesion in the left adnexa with a fluid fluid level overlaid in maroon in e. This reflects sedimented red cells that were free to fall to the dependant portion of the hemorrhagic cyst.
ovary cyst hemorrhage clot fibrin pain midcycle USscan ultrasound Courtesy Ashley Davidoff MD copyright 2008 83279c02.8s |
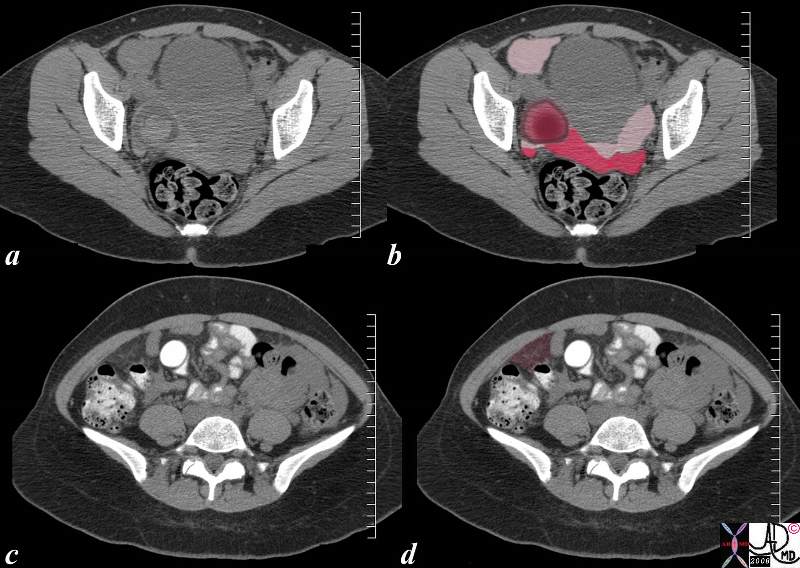
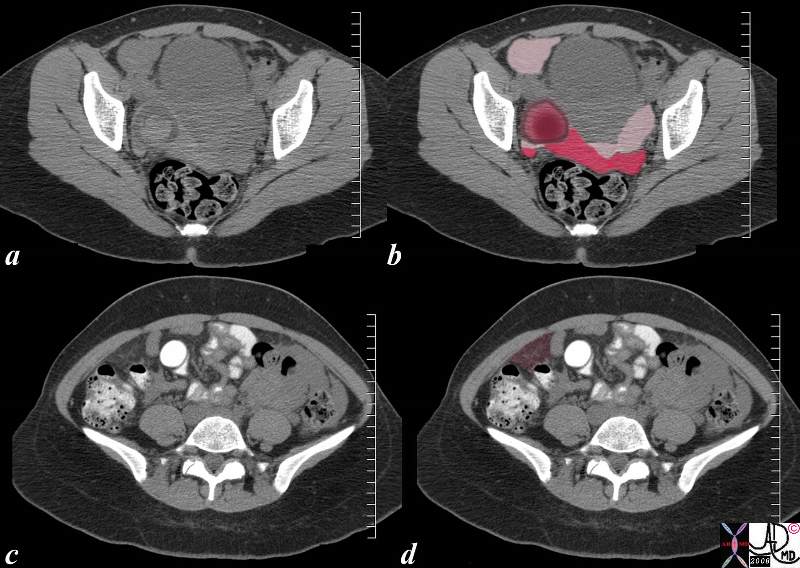 83268c02.8c 83268c02.8c |
| 26 year old female presents with acute midcycle right lower quadrant pain without a fever, associated with peritonism in the right lower quadrant. Differential diagnosis included appendicitis, ruptured cyst, torsion, endometrioma and ectopic pregnancy, but her HCG was normal.
The CTscan shows acute hemorrhage in a cyst int the right adnexa consistent with a hemorrhagic and ruptured follicle, (maroon nodule with a pink circle in b), but also shows a large amount of blood and fluid, some accumulating in the right lower quadrant, (light pink anteriorly on right in b) some in the cul de sac (bright red sediment, and light pink supernatant in b) and some in the greater omentum on the right side (maroon in d). It is the latter component that incites the somatic nocicptors of the peritoneum to simulate peritonitis.
The patient was treated conservatively and improved over the next 24-48 hours.
pain ovary mittelschmerz hemorrhage rupture right lower quadrant pain RLQ peritonism peritonitis CTscan Courtesy Ashley Davidoff MD copyright 2008 83268c02.8c |
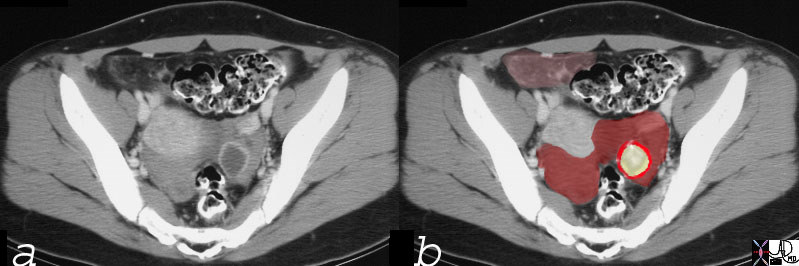
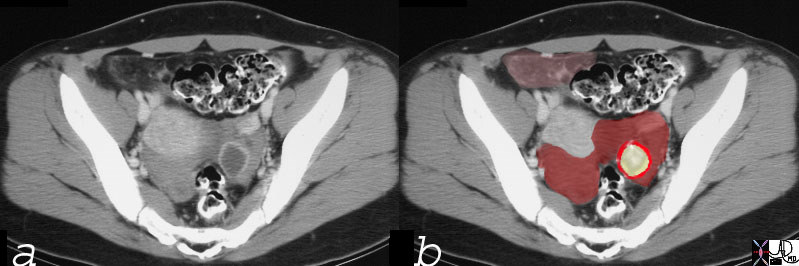
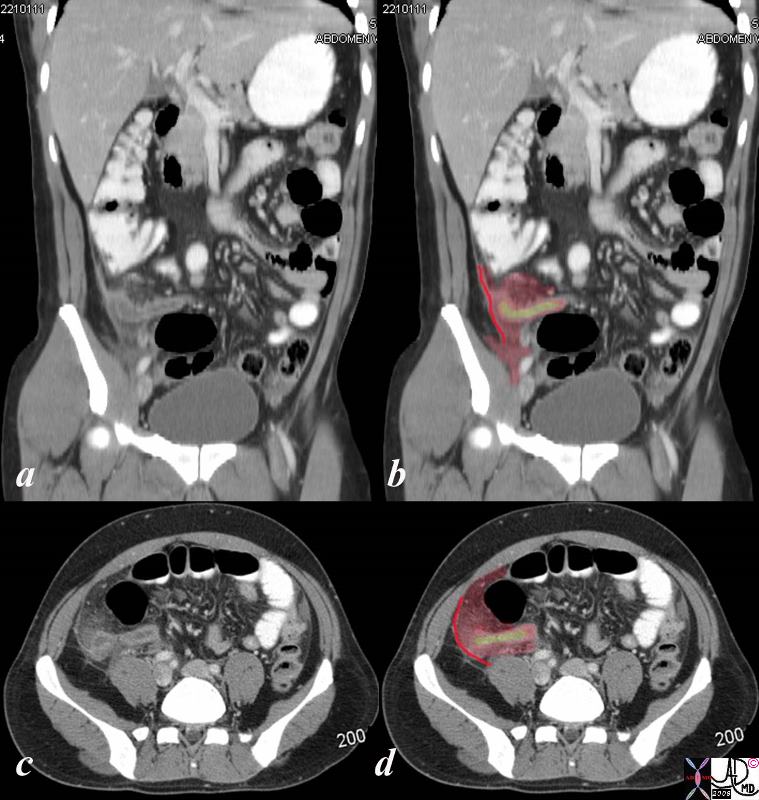
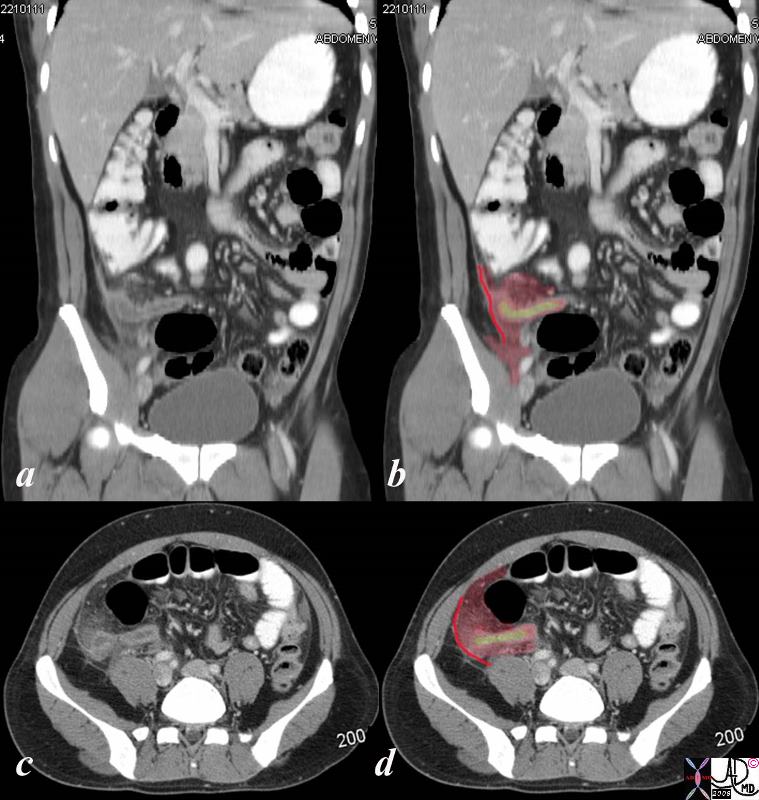
 Left Sided Ruptured Hemorrhagic Cyst with Free Blood in the Pelvis and Bleeding onto the Greater Omentum RLQ (pink) Left Sided Ruptured Hemorrhagic Cyst with Free Blood in the Pelvis and Bleeding onto the Greater Omentum RLQ (pink) |
| This CT scan is that of a 27 year old female who presented with acute lower pelvic pain in mid cycle. The findings of free blood in the pelvis (maroon) the cyst (yellow) with an enhancing rim (bright red) and spillage of blood onto the greater omentum (pink let anterior) are consistent with a ruptured hemorrhagic cyst . The intense ring around the cyst suggests that a corpus luteum cyst has formed already.
24480c01 27 year old female presented with lower abdominal pain pelvic pain ovary fx cyst cul de sac blood free blood hyperdense corpus luteum cyst greater ometum congested fx enhancing dx hemorhagic ovarian cyst CT scan C- CTscan Courtesy Ashley DAvidoff MD |
Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease (PID) is a sexually transmitted infection of the upper female genital tract which is usually caused by polymicrobial group that includes Chlamydia and/or Neisseria gonorrhea (GC) and results in salpingitis, endometritis, and may be complicated by tubo-ovarian abscess. The infection often starts at the cervix and travels upward. Possible complications include infertility and ectopic pregnancy.
The diagnosis usually rests on the clinical presentation includes fever, vaginal discharge, and pelvic pain and may be complicated by shock. Cervical tenderness is characteristic on examination. Imaging is not usually warranted unless a mass is felt on examination or the patient fails to improve on medical therapy.
Depending on the severity at presentation, treatment is with either oral or IV antibiotics. Management ideally is initiated even prior to results of cultures, which otherwise would delay treatment. A high index of suspicion is required and there are guidelines for empiric antibiotic coverage, typically to cover gonorrhea and Chlamydia along with other common pathogens. http://www.cdc.gov/std/treatment/2006/updated-regimens.htm. Those with mild to moderate symptoms may be treated with oral antibiotics unless there is concern they will be unable to complete this therapy, then they should be hospitalized. Patients with more severe infection, or abscess should be hospitalized for parenteral antibiotics. Likewise, if another serious etiology such as appendicitis can?t be excluded, the patient should be hospitalized.
Prevention includes routine screening for GC and Chlamydia for at risk groups.
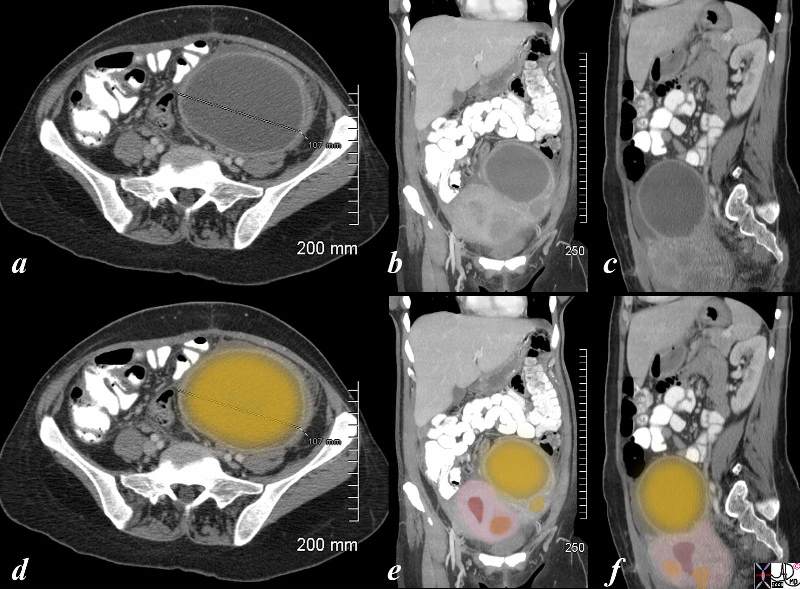
Left Ovarian Abscess |
| The CT is from a 36 year old female recently post cesarian section who developed pain the left lower quadrant, fever and rigors. She has a known fibroid uterus but a new tender mass was found in her left adnexa. The CTscan shows a large cystic collection in the left adnexa(dark yellow) with an enhancing rind. Pus was aspirated under ultrasound guidance , and a diagnosis of an ovarian abscess was made. She was treated on antibiotics and she subsequently her pain and fever resolved . The axial view (a,d) shows a 10.7 cms abscess. The coronal view (b,e) shows the large abscess in the left adnexa with a smaller abscess just below it (yellow) adnexa with the uterus and its endometrial cavity(maroon) and a fibroid in orange. The sagittal view (c,f) shows an irregular uterus (pink) with endometrial cavity (maroon) and a few fibroids (orange)
pain ovary PID pelvic inflammatory disease infection abscess CTscan Ashley DAvidoff MD copyright 2008 83287c03.8s |
Endometritis
Endometritis is an inflammatory condition of the endometrium and can be acute or chronic. The most common cause is infection, staphylococcus aureus, streptococcus, and Gardnerella vaginalis. Acute infection is most commonly seen in post partum period, after a prolonged labor, following cesarian section, and premature rupture of membranes. The most common causes of chronic endometritis is PID, but may be caused by retained products of conception and IUD. Pyometrium is a form of chronic endometriti
Clinically the patienrt with acute endometritis presents with pain, fever, vaginal discharge and bleeding The patient with chronic endometritis presents with vague discomfort or chronic pain, sometimes with a blood stained discharge.
The clinical symptoms are characteristisc and ususally the diagnosis is made clinically particularly in the obstetric population where clinical suspicion is high. If the patient does not respond to antibiotics within 48-72 hours, then imaging to exclude an abscess, or retained products is warranted. Ultrasound is the procedure of choice, and it is able to identify abscesses and retained products but cannot confirm endometritis. If thrombophlebitis is considered then CT or MRI would be helpful.
Treatment is initially with antibiotics but if an abscess is identified it requires drainage, and if retained products are identified then dilatation and curettage is necessary.
  Normal (above) and Endometritis (below) Normal (above) and Endometritis (below) |
| The CTscan through the pelvis in the top image shows a heart shaped fluid filled endometrium with no enhancement of the mucosa and this patient was normal except for a focal probable physiologic process in the left adnexa and a small amount of free fluid in the right pararectal space. The second image is from a 20 year old female with severe colitis who demonstrates an enhancing endometrium that is suggestive of acute endomtritis. In addition she has a large amount of ascites allowing us to visualize both ovaries and broad ligaments.
46355
45318 hx 20 F with acute diarrhea and abdominal pain uterus endometrium fx fluid filled adnexa ovary ovaries normal fx ascites fx fluid in the rectum dx infectious colitis CTscan Courtesy Ashley Davidoff MD |
Ectopic Pregnancy
Ectopic Pregnancy is a disorder where a gestation is located in a location other than the uterus, most commonly in a fallopian tube, but can occur on an ovary or intra-abdominally. It is characterized by pelvic pain associated with vaginal bleeding and a positive pregnancy test. Predisposing factors include previous ectopic pregnancy, pelvic infections (such as Pelvic Inflammatory Disease (PID)). Ectopic Pregnancy can result in serious complications including hemodynamic instability and death.
The diagnosis is suspected clinically by a positive pregnancy test, pelvic pain, and/or vaginal bleeding. It is confirmed by characteristic changes in the velocity of Beta-HCG and ultrasound findings.
Treatment options depend on whether the patient is hemodynamically stable, but include expectant management, medical and surgical management.
Principles
The principles revolve around the malpositioning of the fertilized ovum. The fertilized ovum has to be in the correct space to develop to full term. Once fertilization takes place, division starts immediately and in the early stages the process can continue anywhere in the pelvic cavity requiring any space with minimal blood supply for this to occur. As the developing fetus evolves it requires additional nutrition and the evolving placenta requires the fertile and vascular endometrium to allow growth to continue to full development. In the ectopic situation this is not available and the developing embryo will continue to seek new blood supply. In the rare situation where the pregnancy is intraabdominal, it will parasitize the mesenteries of the abdomen and will implant there until the catrastrophic situation occurs. If undetected an advanced abdominal pregnacy may precitate a catastrophic and fatal bleed. The more usual situation of a tubal ectopic pregnancy can be dramatic but will present earlier. Thus the most basic principle relates to the position and space that is essential to full development. The fertilized ovum can only develop to full term in the endometrial cavity.
Structural Principles
The uterus is uniquely structured to accommodate, nourish, and protect a growing pregnancy. Other structures in the pelvis and abdomen are unable to accommodate or support a pregnancy and an ectopic can lead to serious life threatening consequences. The developing placenta “invades” the endometrial lining which becomes primed for the invasion, to set up a transport and filtering mechanism so that maternal blood, rich in nutrients can transfer this blood to the fetus, and can also receive the fetal blood to export waste for the fetus
  The Normal Fallopian Tubes The Normal Fallopian Tubes |
| 46376 4376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity |
Cause and Predisposing Factors
There are multiple predisposing factors, including those which alter the structure and function of the fallopian tubes. These include previous ectopic pregnancy or fallopian tubal surgery, PID. Other factors include cigarette smoking, use of fertility drugs and previous use of some intrauterine devices, and of course being a female of child bearing age. For unclear reasons, females over the age of 35 are also at higher risk for ectopic pregnancy.
Pathophysiology and Pathogenesis
Pathophysiology and Pathogenesis: The most common location of an ectopic pregnancy is in a Fallopian Tube, most commonly in the ampullary portion. The abnormally implanted gestation draws its blood supply from the organ within which it is implanted. Symptoms of an ectopic pregnancy typically start at approximate week number seven of a pregnancy, when the gestation is becomes too large for the organ within which it is implanted to accommodate. This can lead to rupture of the organ, uncontrolled bleeding and even death.
Diagnosis
The diagnosis of ectopic pregnancy involves a complex but standardized approach. This involves a careful history and physical examination and a high index of suspicion along with appropriate laboratory studies and imaging.
Clinical
The classic presentation of ectopic pregnancy includes amenorrhea (no periods for more than 6-7 weeks), pelvic pain, and vaginal bleeding. Many patients do not have this classic presentation, however. Anytime a woman presents with pelvic or abdominal pain associated with amenorrhea, one must consider ectopic pregnancy. A positive pregnancy test along with a normal or slightly enlarged, often tender uterus or adnexal mass is highly suggestive of ectopic pregnancy. However, no combination of physical findings can definitively diagnose an ectopic pregnancy.
Differential Diagnosis
Includes multiple conditions which can cause acute pelvic pain including Pelvic Inflammatory Disease (PID), spontaneous abortion (SAB), appendicitis, and kidney stones. In pelvic inflammatory disease, kidney stones, and appendicitis, pregnancy testing is typically negative and vaginal bleeding is less likely. Perhaps most difficult to differentiate are spontaneous abortions from ectopics. On physical exam, there may be pregnancy tissue present in the os in a spontaneous abortion which is typically not the case with an ectopic pregnancy. Also, the ultrasound findings may be different and the serum HCG level typically falls more quickly with an SAB.
Lab Tests
A laboratory evaluation should include a quantitative serum human chorionic gonadotropin (HCG) level, complete blood count, along with kidney and liver function. In a normal pregnancy, the HCG level typically will double every 48 hours in early pregnancy but will not in ectopic pregnancy. Typically, the HCG will go do down in SAB. Sometimes, a serum progesterone level can also be helpful in determining the viability of a pregnancy but generally is not considered as reliable a marker as an HCG.
Imaging
An ultrasound correlated with a quantitative HCG can be diagnostic of ectopic pregnancy. An ectopic is suspected if the HCG is greater than 1500 and there is no evidence of an intrauterine gestational sac on transvaginal ultrasonography. On, intravaginal ultrasonography, an ectopic is suspected if an intrauterine pregnancy is not detected with a HCG level of greater than 6500.
Treatment and Management
There are several treatment options, and the appropriate selection depends on the clinical conditions. The options include expectant management, medical management, and surgical management. Expectant management: sometimes, if the pregnancy is early (with a serum HCG of < 1000 and declining) and the gestation is small (less than 3 cm), and absent fetal heartbeat, expectant management with close follow-up may be considered. If the patient is hemodynamically stable, it may be possible to treat the ectopic medically. Medical management typically involves methotrexate. Methotrexate is a chemotherapeutic agent which inhibits folate metabolism, therefore inhibiting the growth of rapidly dividing cells such as a new gestation. Surgical intervention typically involves laparoscopic surgery and most recently tubal incision to remove the gestation. Surgery is chosen for the unstable patient, larger, more advanced pregnancies, and for medical treatment failures.
Prognosis
Generally the prognosis of ectopic pregnancy is good if it is diagnosed in a timely fashion. However, this serious condition is also one of the most common causes of maternal death and infertility.
Conclusion
Ectopic pregnancy involves the abnormal location of a pregnancy, most commonly in a fallopian tube. Risk factors include those conditions which affect the structure and function of the fallopian tube including pelvic inflammatory disease, previous fallopian tube surgery, or previous ectopic pregnancy. Any woman with amenorrhea with a positive pregnancy test, pelvic or abdominal pain, and/or vaginal bleeding, needs to be evaluated for possible ectopic pregnancy. The gestation will not survive outside of the uterus. This potentially life threatening condition is treatable if diagnosed in a timely fashion. Potential complications of ectopic pregnancy include recurrent ectopic pregnancy, infertility, and death.
Spontaneous Abortion – Miscarriage
Spontaneous abortion is the expulsion of a non viable embryo or fetus usually caused by to chromosomal aberrations or environmental factors, occurring before the 20the week, though most occur before 12 weeks.
There are 4 clinical entities including threatened, inevitable, incomplete and complete spontaneous abortion.
Clinically threatened abortion is diagnosed and characterized by some bleeding and sometimes accompanied by pain in the first trimester. About half of these patients will recover and proceed to full term pregnancies. When the symptoms are accompanied by a dilated cervix then abortion becomes “inevitable”. Bleeding and cramps are usually more prominent with inevitable abortion. The presence of products of conception in the discharged blood warrants examination by ultrasound. If products of conception are identified in the endometrial cavity the diagnosis is is compatible with incomplete abortion and their absence confirms the diagnosis of a complete spontaneous abortion. Pain and bleeding subside when the abortion is complete.
Treatment depends on the stage of the the spontaneous abortion. A complete abortion requires no further treatment. nA incomplete or inevitable abortion before 13 weeks is treated with suction dilatation and curettage though medical therapy (misorostol) can be used.
 Retained Products of Conception Retained Products of Conception |
| The ultrasound is from a 46 patient who presents with bleeding and pain 9 weeks into her pregnancy. Doppler study shows no fetal pole nor fetal heart beat. Findings include a thickened endometrium (light pink) with a focal area in the posterior and fundal portion of the endometrium (dark pink with red blood vessel inside) that enhances, consistent with retained products of conception and spontaneous abortion.
SAB US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008 83222c02.8s |
Ovarian Torsion
Adnexal torsion is a twisting of the ovary around its pedicle including its neurovascular bundle, usually caused by an associated benign tumor, resulting in an acute pain syndrome. There may be spontaneous untwisting with symptomatic resolution or progressive venous congestion, followed by arterial compromise. Torsion may be complicated by hemorrhagic infarction.
The diagnosis is based on the clinical presentation of acute severe lower abdominal pain and tenderness often associated with nausea and vomitting..usually in a young female or in post menopausal woman. Torsion is also seen with increased frequency during pregnancy.and the diagnosis is confirmed using ultrasound which shows a twisted vascular pedicle (“whirlpool” sign) and lack of flow to the ovary. The ovary is swollen.
Treatment includes urgent laparoscopic evaluation to determine viability. if the ovary looks viable then the pedicle is untwisted and pexied to prevent recurrence. If infarction has occurred then the ovary needs to be removed
Fibroid Disease and Degeneration
Uterine fibroids (leiomyomas) are benign tumors of the myometrium and are the most common female reproductive tract tumor. They are thought to arise from a single cell (? chromosomal aberration) and growth is affected by estrogen and progesterone. They typically regress with menopause.
They occupy space and in so doing may displace or obstruct other structures. They may cause pain during the menses and if they degenerate with disruption of their blood supply, sudden severe pelvic pain can occur. If a pedunculated fibroid becomes twisted on itself (torsion), this can cause acute pain.
Symptoms associated with these space occupying lesions can include irregular or prolonged menstrual bleeding, painful intercourse, and pressure on other structures located nearby including the bladder (urinary frequency) or bowels (constipation.)
Treatment depends on the clinical scenario, but usually for the pain syndromes it is symptomatic. Frequently, fibroids are incidental findings which can be managed expectantly. If there is significant pain suggestive of necrosis, bleeding, or infertility surgery may be considered. Options include myomectomy (removal of the tumor only) or complete hysterectomy. Sometimes, selective emboliziation is used, particulalrly when the fibroids are large. this is a percutaneous technique that involves selective catheterization of the feeding arteries and causing ischemia and infarction of the tumor.
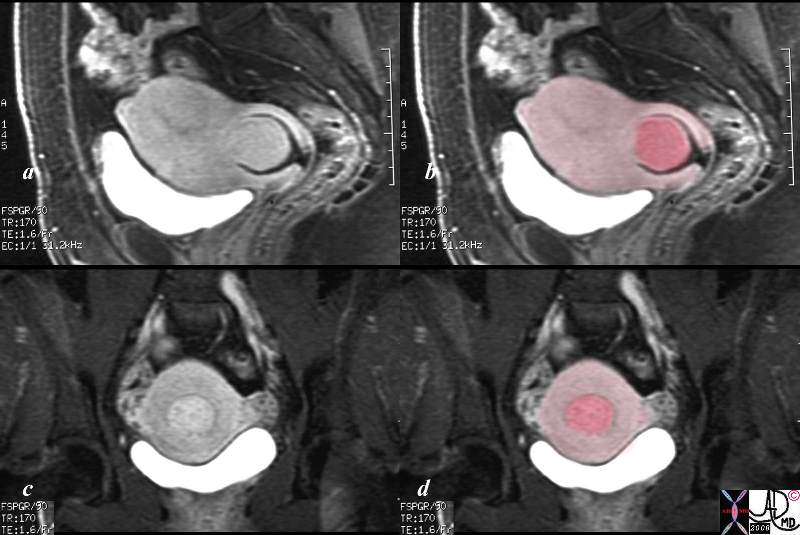
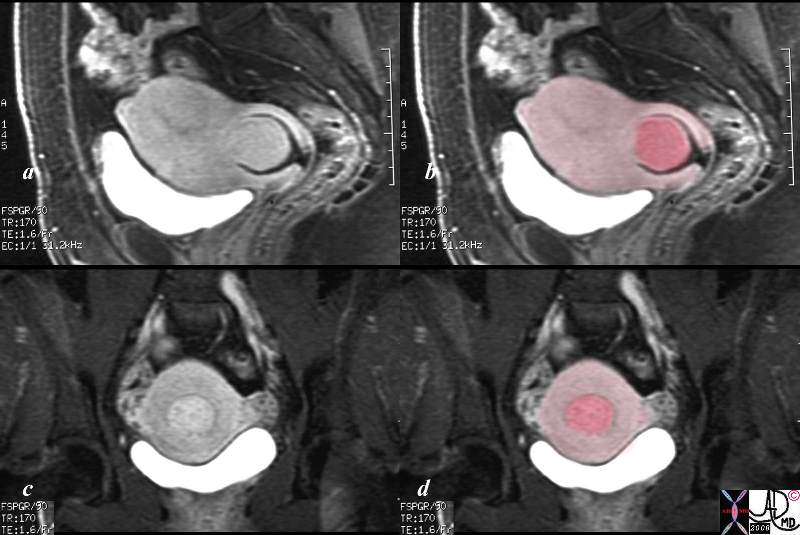 Prolapsing Submucosal Fibroid Prolapsing Submucosal Fibroid |
| This patient presented to the emergency room with severe crampy abdominal pain and a known history of a submucosal fibroid. The MRI shows the fibroid (dark pink) orotruding and expanding the cervix in the sagital view, and in the coronal view it is seen as a hyperemic structure (c) surrounded by lighter pink myometrium.
pain uterus submucosal fibroid prolapse MRI Courtesy Ashley DAvidoff MD copyright 2008 16265c01.8s |
Non Gynecological Causes of Acute Pain
Acute Pelvic Pain Generated by Gastrointestinal Disorders
Appendicitis
Appendicitis is an inflammatory condition of the appendix caused primarily by an initial obstruction with secondary infection, distension, and subsequent infarction and rupture.: The appendix is a long tube-like structure (diverticulum) which extends from the cecum. The obstruction may be caused by lymphoid hyperplasia (often related to a viral illness), foreign bodies and fecoliths, or related to Crohn?s disease. Acute appendicitis is the most common surgical emergency in the Western World. It typically affects teenagers and young adults, though may occur in younger children and infants. There is a smaller secondary peak in the elderly.
Structural considerations
The appendix is situated in the right lower quadrant but its origin off the cecum is quite variable so that it may be anterior, medial or posterior to the cecum. its length also varies, so for example a very long retrocecal appendix may reach to the right upper quadrant. Depending on the anatomic location of the appendix, it may be initially difficult to differentiate from other causes of acute pelvic pain
Clinically, appendicitis classically presents with abdominal pain that starts at the umbilicus and and migrates to the right lower quadrant . It is usually associated with systemic symptoms and signs such as nausea, vomiting, fever. The pain almost always precedes the vomiting. On examination there is usually tenderness with guarding and rebound in the right lower quadrant at Mc Burney’s point, and rectal examination usually reveals right sided pelvic tenderness. Systemically mild dehydration, fever and an elevated wcc are associated signs. (Family Practice Notebook). The classical pain only occurs in about 50% of patients. When the patients presents with these classical features there is no reason to go any further with imaging to confirm the diagnosis. However appendicitis is notoriously a masquerader from being relatively asymptomatic to having severe visceral and somatic pain.
When clinical findings are equivocal diagnostic imaging choices include ultrasound and CTscan are considered. In children, and young thin females, ultrasound is the study of choice. Ultrasound is extremely dependant on the opearator, and also is made difficult if bowel gas is present. In the older population, CT is preferred. The overall accuracy of US for appendicitis is reported at 70-95% and for CT accuracy is 93-98%. CT is indicated when perforation or peritonitis is clinically suspected.
Treatment is surgical. Laparoscopic removal is frequently utilized. Sometimes, open laparotomy is required, such as when an associated abscess is suspected.


 Normal and Necrotic Normal and Necrotic
|
| These two pathological specimens of the gallbladder show a normal lily white appendix on the left and a severely inflammed, blackened and necrotic appendix on the right.
02559 colon large bowel appendix grosspathology Courtesy Ted Gulkin MD
courtesy Barbara Banner MD 02435 colon appendix dx black fx distended fx enlarged fx discoloration discolored dx acute gangrenous appendicitis dx ischemic necrosis dx acute appendicitis necrotic grosspathology Courtesy Dr Gutkin |
 Appendicitis with Significant Perappendiceal Induration Appendicitis with Significant Perappendiceal Induration |
| This is a CTscan of a young man who presented with severe somatic pain, well localized to the right lower quadrant. He did not have a fever but had a mildly elevated white cell count. The CT shows an appendix that has a diameter of 8mms., is distended with fluid (yellow in b and d) is surrounded by an hyperemic rim (white rind in a and c – pink around the yellow in b and d) significant induration of the pericolic fat, (maroon) and thickened peritoneum (bright red). It is the latter involvement of the peritoneum that causes the severe well localized somatic pain.
appendix distended colon peritoneal thickening peritonitis CTsca Courteysy Ashley Davidoff MD copyright 2008 44780c01.8s |
Diverticulitis
Diverticulitis is an inflammation of a diverticulum caused by an initial obstruction and then infection of the diverticulum. This results in spread of the inflammation to the surrounding fat and other tissues or organs surrounding the bowel. Diverticulitis can be complicated by abscess formation, bowel perforation, peritonitis or less commonly by fistulous formation to the bladder
Structural considerations
Diverticula occur at sites of the colon wall that are relative weak, typically at sites of the insertions of blood vessels through the muscle wall. Its lumen communicates with the lumen of the colon. Although not completely understood, these outpouchings are much more common with a Western, low fiber diet and appear to be related to increased intraluminal pressure. Diverticulitis is a condition that most commonly involves the sigmoid colon and therefore presents with left lower quadrant pain which can occasionally be confused with other pelvic pathology. Most colonic diverticula are 0.5 to 1 cm in diameter, typically located in the sigmoid colon.
Clinically the patient classically presents with left lower quadrant pain because the sigmoid colon is the most common site of involvement. The descending colon is sometimes affected in which case the patient will present with left upper quadrant or left mid or lateral pain. Diverticulitis is a condition that most commonly involves the sigmoid colon and therefore presents with left lower quadrant pain which can occasionally be confused with other pelvic pathology. Pain is often present for several days, and there may be a history of prior similar episodes. Fever and elevated white count are common accompaniments. It is sometimes associated with changes in bowel movements.
The diagnosis is confirmed by CT scan which is the study of choice. Oral and intravenous contrast are preferred, but not essential if there is a contraindication. Administration of rectal contrast may be considered in such cases and may slightly improve sensitivity by dilating the colon. The reported sensitivity of CT for diagnosing acute diverticulitis is 79-99%. CT is excellent for detection of complications of diverticulitis including abscess and fistula formation; furthermore, it may detect other non-colonic causes of abdominal pain. CT is able to direct management since uncomplicated diverticulitis would be managed conservatively and when complications such as abscess formation or perforation are identified they would be managed surgically.
Diverticulitis is commonly treated with antibiotics, but sometimes surgery is required. Depending on the severity, the condition is medically managed with oral or parenteral antibiotics which provide broad coverage. This coverage needs to include anaerobes. Sometimes this can be done as an outpatient with oral medications. But for more severe cases, including those associated with vomiting, intractable pain, or associated abscess, are managed in hospital with IV antibiotics. Large abscesses can be drained percutaneously while surgery is sometimes required for abscesses associated with perforation and free air. For frequent recurrences, sometimes the portion of affected bowel is removed electively, after the acute inflammatory process settles down.
 Non inflammed diverticulum (a, b -green), Diverticulitis (c,d), and Pericolic inflammation (red) Non inflammed diverticulum (a, b -green), Diverticulitis (c,d), and Pericolic inflammation (red) |
| The CT scan shows evidence of both diverticulosis and diverticulitis. In images a and b, two small non inflammed outpouchings are seen. The diverticula are outlined in green in b. In the same patient another diverticulum has become inflammed, and diverticulitis is present. This is characterized by induration of the fat around the diverticulum and the colon (maroon) and extension of the inflammatory process to the peritoneal lining (bright red in d). Inflammation of the colon and colonic wall induces visceral pain which is an ache and poorly localized, and inflammation of the peritoneal lining causes a sharp well localised somatic pain that is sensitive to deep palpation.
28582c02 colon descending colon diverticulum diverticulitis pericolic induration acute inflammation acute diverticulitis diverticulosis CTscan Courtesy Ashley Davidoff MD |
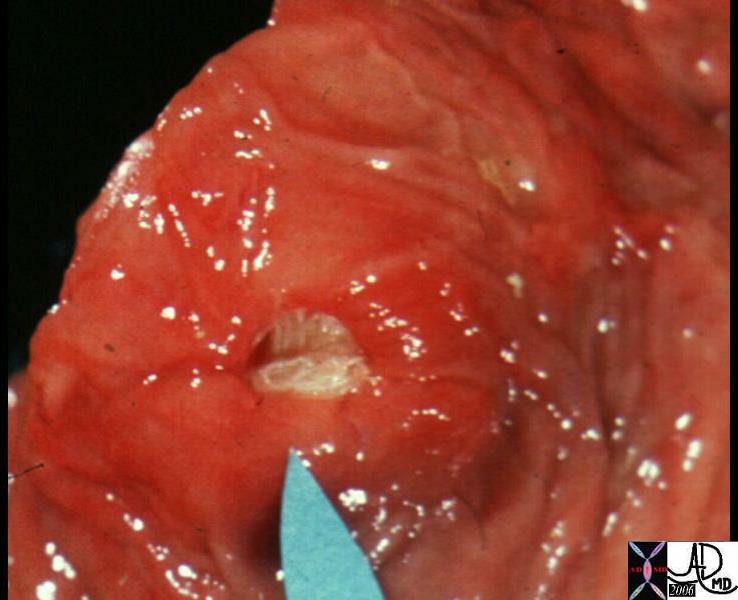
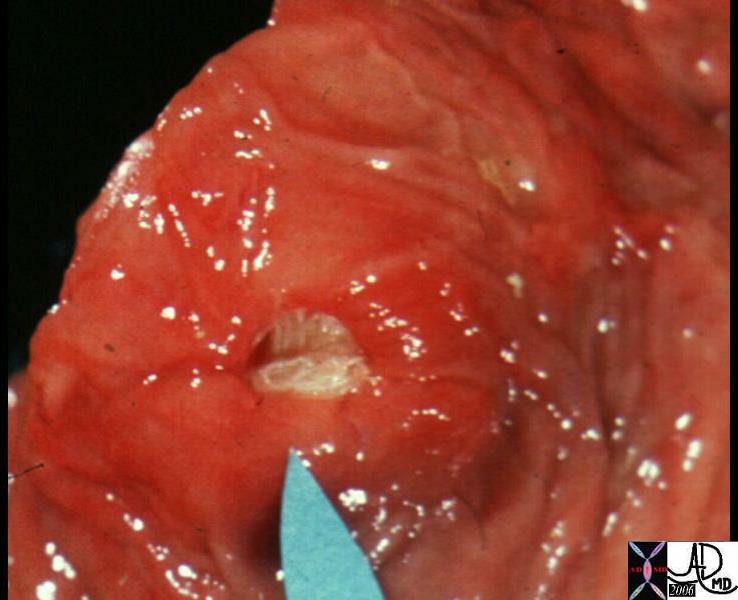
Acute Diverticulitis – Mouth of Diverticulum is Filled with Pus |
| This pathological specimen shows the mouth of a diverticulum filled with yellow pus in this patient who had complicated diverticulitis. The tissues surrounding the diverticulum are swollen and red.
12077 colon large bowel fx pus filled purulent diverticulum fx mucosal hyperemia reddening dx acute diverticulitis grosspathology Courtesy Barbara Banner MD |
Acute Pelvic Pain Generated by the Musculoskeletal Disorders
Acute muscle strain includes injuries such as acute groin strain that is caused by running, jumping or twisting that resulting in external rotation or sudden contraction and puts strain by overstretching the adductor longus muscle. The event is marked by a sudden twinge or tearing sensation during the stress and is easily recognized by the patient and relatively easily diagnosed. Treatment is with NSAIDS and rest.
There are musculoskeletal causes of acute hip injury that include sprains of the hip joint caused by exceeding the range of motion of the hip joint. Injuries that may do this include a force from an opponent in a physical contact sports game or by trunk force that is in the opposite direction of a planted foot. Clinical exam shows pain which increases with hip rotation, inability to circumduct the hip. Treatment is with NSAIDS and rest.
Stress fractures of the inferior pubic ramus, femoral neck or subtrochanteric area of the femur caused by repetitive stress (running) manifesting as groin pain or an aching sensation in the upper thigh that increases with activity and improves with rest. Clinically the patient cannot stand on one leg, and deep palpation results in point tenderness. X-ray, bone scan and MRI are required to confirm the diagnosis. Treatment requires rest for 2-5 months and usually requires a crutch and snapping hip phenomenon commonly seen in dancers gymnasts and hurdlers, where repetitive movements lead to muscle imbalance.
Direct blows to the hips may result in contusion of the iliac crest or abdominal musculature and these may result in pain caused by hematoma, or muscle spasm. This can last from 1-3 weeks. Treatment is with NSAIDS, ice pads, and rest.
Diastases of the pubic symphisis is a common association with pregnancy where the combination of ligamentous laxity, and stresses induced by labor cause permanent diastasis and acute pain. Addditionally diastasis may be caused by high energy trauma, as is seen in horesriders who by virtue of stretching of the pubic symphis, insult to injury is caused by repetitve forces created by up and down motion of horse riding.
Acute Pelvic Pain Generated by the Urinary System
Acute Cystitis
Acute cystitis is an inflammatory condition of the bladder usually caused by coliform bacteria, usually E Coli, transferred from the bowel to the bladder via the urethra. Non infectious causes are also present such as interstitial cystitis and esinophillic cystitis. It is common in females who are sexually active, (honeymoon cytitis) but sometimes seen in young females with a second peak in the older women. It is rare in males.
Structural Considerations. The proximity of the rectum to the urethra together with the short urethra of women, enable coliform bacteria to enter and infect the bladder. In the young and old uncoordinated and inappropriate cleansing of the area may cause the infection and the mechanical consequences of sexual intercourse may be the cause in honeymoon cystitis. Normal bladder function and excretion of urine enable bacteria to be removed by the evacuation, but if patient have bladder stagnation and there is difficulty with urinary evacuation then infection becomes more likely.
Clinically cystitis commonly results in with dysuria (painful urination), urinary frequency, cloudy urine, and possibly hematuria (blood in the urine).
Urine testing in the lab enables the diagnosis by identifying white blood cells, red blood cells, and may be able to culture the bacteria with a clean catch specimen.
Treatment with antibiotics is instituted if bacteria are identified. Pyridium is used to reduce the burning and pain, and fluids are encouraged to increase flushing of the bladder.
Kidney Stones
Renal colic is a acute pain caused by acute obstruction of the urinary collecting system, by a stone that has become dislodged from the kidney and become lodged in the ureter. Ureterolithiasis is most commonly asponataneous event but is sometimes associated with decreased fluid intake, dehydration and subsequent urinary concentration. It is also associated with increased intake of oxalates. Clinically the pain syndrome that results is classically associated with flank pain, or “loin to groin pain”, though isolated groin pain is possible. The pain is usually excruciating and possibly the most severe pain the patient has experienced. Hematuria is very common.
CTscan without contrast is the study of choice.
When the stone is small (<5mms) conservative treatment is usual which includes analgesia and hydration. Retrograde retrieval and or stenting of the system is reserved for larger stones or stones that do not respond to conservative therapy.
Chronic Pelvic Pain
Chronic pelvic pain that has been present for longer than three months. It is a poorly understood debilitating disorder with multiple causes. Many of the disease discussed above can progress to a chronic condition, and the classification into gynecological , gastrointestinal, urinary, and musculoskeletal causes is similar
Clinically, a careful history directed at the prior medical and surgical history is essential. Direct questioning related specifically to the genitourinary system, gastrointestinal system and musculoskeltal system is necessary, and probably the most important component of the diagnostic work up. A prior history of fibroids, endometriosis, PID, ectopic pregnancy, are all diseases that may progress to a chronipelvic c pain syndrome.
If the clinical examination revels unexpected findings such as a mass, then diagnostic imaging by ultraound may be helpful in the workup.
Treatment depends on the known cause but if a structural abnormality is not identified or is not amenable to surgical or specific medical intervention, then recommendations include prudent use of alpha blockers, phytotherapy, directives allowing release of myofascial triggerpoints, and anxiety control.
We will outline a few of the more of the common disorders associated with chronic pelvic pain that have not been outlined above.
Pelvic Adhesions
Pelvic adhesion is the fibrotic consequence of inflammation in the pelvis that may have been caused by previous surgery, pelvic inflammatory disease, complications of diverticulitis or recurrent intraperitoneal bleeds caused by cyclical events or endometriosis. The result is that the fibrous tissues cause structural distortion and enttrapment of the pelvic organs causing pain and dysfunction.
Clinically the patient presents with visceral type pain that is characteristically poorly localised in the lower abdomen, with an aching or cramping character. The diagnosis is based on the clinical history, and unless frank obstruction of the gastrointestinal or genitourinary system is observed radiologically or laparoscopically, it is a diagnosis of exclusion.
Treatment is somewhat controversial, but sometimes surgery for lysis of adhesions is helpful.
Irritable Bowel Syndrome IBS
Irritable Bowel Syndrome is a debilitating functional gastrointestinal disorder characterized by abdominal (and pelvic) cramping, increased bowel gas, and bowel movement changes including diarrhea and/or constipation. The cause is mostly unknown, but the syndrome may be initiated by an infection, and sometimes has psychological origins.
Clinically the presenting symptoms are non specific. The pain ranges from mild to severe, the bowel habit may manifest with constipation or diarrhea, there maty be a sense of incomplete evacuation, bloating and abdominal distension. These symptoms simulate many other disorders including inflammatory bowel disease celiac disease, giardiasis, yersinia enterocoltica and these need to be excluded before the diagnosis is considered. It is thus a diagnosis of exclusion.
Treatment includes symptomatic relief, dietary intervention, and when indicated psychological evaluation and assistance.
Constipation
Constipation is the presence of hard feces that is difficult and painful to evacuate. This usually occurs when the patient evacuates less than three times per week. In general constipation is caused by dry stool . When the transit time of the stool through the colon is slowed, there is excessive absorbtion of water from the stool making it hard and dry and difficult to evacuate. There are many causes for this slowing, including age, mental status, dietary factors, hormonal factors, and side effect of medications (morphine and other opiates). The gradual accumualation of feces can be complicated by abdominal distension and finally impaction and obstruction which becomes a surgical emergency.
Functional considerations; Because the pelvis contains a portion of the colon, the cramping and pressure associated with constipation can cause pelvic pain both by pressure on neighboring structures as well as referred pain.
Clinically the patient complains of difficult, painful, infrequent and ineffective vacuation. Small fecal pellets may be passed but this is overall an ineffective evacuation.
The diagnosis is made clinically but the presence of large amounts of stool distending the colon is easily diagnosed by a plain film of the abdomen, while complications are best diagnosed by CTscanning.
There are multiple therapies for constipation. Frequently, if the constipation is severe enough to present for medical attention, more aggressive approaches such as enemas are employed. Multiple over the counter laxatives are available for less severe cases. High fiber diet and adequate hydration should also be emphasized.
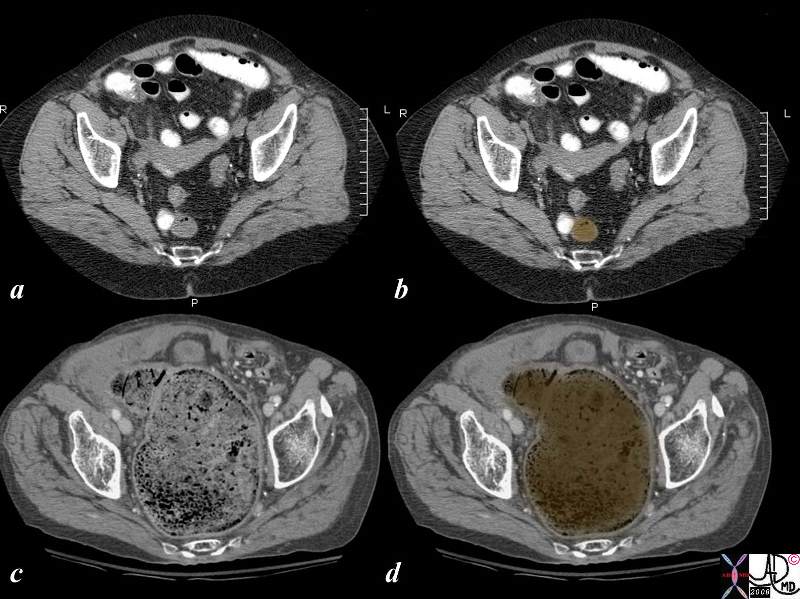
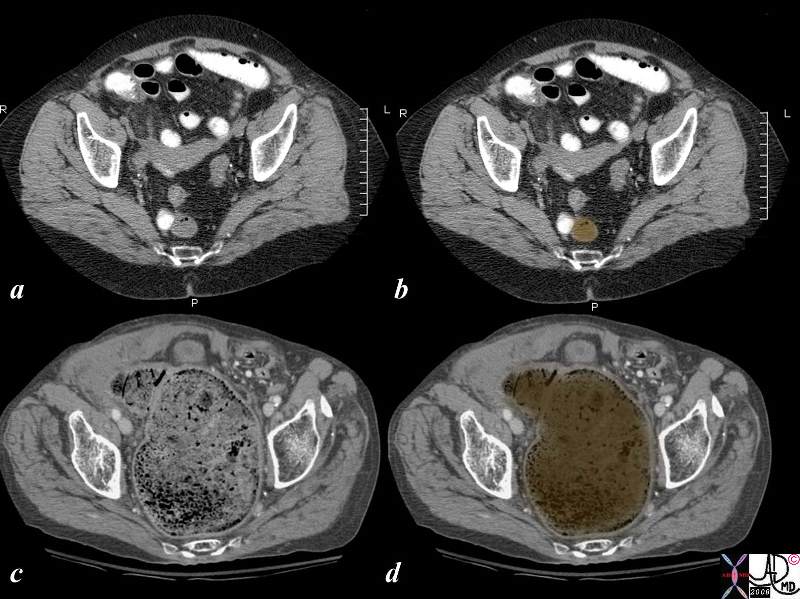 Normal Rectum (above) and Impacted Rectum (below) Normal Rectum (above) and Impacted Rectum (below) |
| The CT scan shows a patient with a normal empty rectum that contains a few bubbles of air (a,b) overlaid in dark orange, and a patient with severe constipation and impaction of feces (c, and d overlay in brown) It is even painful to look at.
colon rectum pain pelvic pain feces fecal impaction constipation mechanical CTscan normal vs abnormal Courtesy Ashley Davidoff MD copyright 2008 18278c02.8s |
Interstitial Cystitis
Interstitial cystitis is a chronic inflammatory disorder bladder mucosa. The cause of interstitial cystitis is unknown, although it is thought to be a syndrome which may have multiple etiologies: autoimmune, infectious, and allergic components.
Clinically symptoms can be very similar to that of acute cystitis and urinary tract infection, so that increased urinary frequency, urgency, dysuria and hematuria are common manifestations.
There is no evidence of infection on culture.
Medical management and support groups are usually instituted. Medications include tri-cyclic antidepressants and antihistamines. It is also recommended that IC patients avoid caffeine, acidic foods, and artificial sweeteners. Occasionally, medications are infused directly into the bladder. Surgery is rarely indicated.
Myofascial Pain Syndrome
Myofascial pain is a chronic pain syndrome that is poorly understood, but thought to be caused by altered focal pain thresholds in the muscle. It is characterized by the presence of specific trigger points which are sensitized and sensitive foci in the muscle and fascia. It may be closely related to fibromyalgia.
Clinically these areas exhibit extreme tenderness since the receptors are a mixture of both somatic and visceral nociceptors. It is usually associated with other symptoms including headaches, fatigue, and depression.
Treatment is non surgical. Myofascial release is a soft tissue treatment that uses gentle massage and stretching of muscle and fascia that has shown to be effective.
Mental Health Disorders
Mental health disorders including sexual abuse, substance abuse and depression can be associated with chronic pelvic pain. (Walker)
The Large Picture of Pelvic Pain
Clinical
As with all medical evaluations, the history is a most important tool to help establish the cause of the pelvic pain. As discussed above, the timing (Acute, cyclical, chronic) frequently is useful in diagnosis. Vaginal discharge or bleeding may make several conditions more likely. Associated symptoms such as urinary or gastrointestinal changes may suggest an etiology other than a gynecological one. History can provide important clues as to the etiology of the pelvic pain. Characteristics such as location, quality, radiation, severity, and duration along with any aggravating or alleviating factors are important to ascertain. Likewise, timing with attention to the relation to menses, bowel movements, urination, and sexual intercourse might suggest a particular pathology.
There are certain clinical pointers on the clinical examination that are very helpful in making a diagnosis. An important physical exam finding in pelvic inflammatory disease is cervical motion tenderness, or uterine or adnexal tenderness on bimanual exam. Frequently, there is evidence of infection with mucopurulent discharge, fevers, and increased numbers of white blood cells on microscopic evaluation of saline washings of vagina.
Ectopic pregnancy may have a classic presentation that includes amenorrhea (no periods for more than 6-7 weeks), pelvic pain, and vaginal bleeding and a positive pregnancy test. Many patients do not have aclassic presentation, however. Anytime a woman of childbearing age presents with pelvic or abdominal pain associated with amenorrhea, one must consider ectopic pregnancy. A positive pregnancy test along with a normal or slightly enlarged, often tender uterus or adnexal mass is highly suggestive of ectopic pregnancy. However, no combination of physical findings can definitively diagnose an ectopic pregnancy.
In the setting of sudden onset of severe adnexal pain or mass, associated with nausea and vomiting, ovarian torsion must have the diagnosis of ovarian torsion excluded on an emrgent basis using ultrasound since time is critical in this disease, and the presentation of pain does not necessarily imply ischemia
Lab Evaluation
Lab Evaluation should always include a pregnancy test in all patients of child bearing years. There are certainly times when either the patient is unaware they are pregnant or do not want others to know that they are pregnant, and missing this diagnosis could be fatal. The most commonly performed pregnancy is either the urine test or serum for human chorionic gonadotropin (hCG). hCG is a pregnancy hormone initially produced by the embryo and later the placenta. It helps maintain the corpus luteum which is necessary to produce progesterone, which in turn is essential for the pregnancy. Urine pregnancy testing can detect hCG levels as low as 20 mIU/ml (in theory) versus serum testing which can detect levels as low as 5 mIU/ml.
Testing for gonorrhea and Chlamydia is mandatory, and given increased risk, the patient should also be tested for HIV.
Imaging
In general, ultrasonography is the first investigative study of choice if a gynecologic problem is suspected. It allows for excellent visualization of the pelvic organs, is relatively inexpensive, and does not expose the patient to ionizing radiation. The use of a transvaginal probe also obviates the need for a full bladder and allows for exquisite detail of the aantomy and pathology.
Other studies used in the evaluation of pelvic pain include sonohysterography. Sterile saline is injected into the uterine cavity, and transvaginal ultrasound is used to evaluate the endometrial cavity. Polyps, submucosal fibroids, and endometrial cancer may be delineated.
CT is of use in several clinical situations. It may be performed if ultrasound findings are equivocal, if the abnormality is beyond the field of a transvaginal probe, or if a non-gynecologic cause of pelvic pain is suspected. CT is particularly important in evaluating suspected pelvic abscesses or hematomas, postpartum complications, complications related to pelvic inflammatory disease, or to exclude bowel disease.
MRI allows for excellent visualization of soft tissue structures with multiplanar views. It is helpful for diagnosing endometriosis and determining the origins of adnexal masses as well as bony and soft tissue injury of muscle. It is the best imaging modality to diagnose adenomyosis and distinguish it from uterine fibroids. It may also demonstrate pelvic varices/venous congestion, though there is scant data evaluating accuracy, sensitivity and specificity.
Hysterosalpingography (HSG) involves injecting radiopaque contrast through the cervix and using fluoroscopy to visualize the uterine cavity and fallopian tubes. It evaluates tubal patency and may delineate subtle distortions in the uterine cavity by polyps or other small masses. HSG is commonly used for infertility evaluation, and may also be considered for chronic pelvic pain.
Common imaging techniques useful for evaluation of pelvic pain include ultrasound, computerized tomography, and magnetic resonance imaging.
PID: Transvaginal ultrasound or MRI may show thickened, fluid filled fallopian tubes.
Ectopic Pregnancy: Ultrasound investigation correlated with serial quantitative HCG levels is frequently useful in the diagnosis of ectopic pregnancy (see above)
Potential Complications
- PID: Infertility. Ectopic Pregnancy. Tuboovarian abscess.
- Ectopic Pregnancy: Is the leading cause of pregnancy related death.
- Adnexal Torsion: Necrosis of the ovary
- Ovarian Cysts: vaginal bleeding, rupture leading to hemorrhage.
- Uterine Fibroids
- Appendicitis: Abscess, sepsis.
- Diverticulitis: Abscess, Sepsis.
- Endometriosis: Infertility, dyspareunia.
- PMS: Serious medical complications uncommon, but may cause significant psychosocial issues.
10.Pelvic Adhesions: intestinal obstruction.
11.Fibroids: vaginal bleeding, infertility.
12.Constipation: hemorrhoids, intestinal obstruction.
13.Interstitial Cystitis: Significant psychosocial stress.
Management:
Management: Depends on the underlying etiology and is in general specific to the disease entity.
Red Flags
Pelvic pain can be associated with many significant, potentially life threatening conditions. Other conditions are associated with significant morbidity including infertility.
Certainly a positive pregnancy test associated with pelvic pain and/or bleeding should prompt evaluation for an ectopic pregnancy.
Mucopurulent cervical discharge, fevers, and/or cervical motion tenderness can all be worrisome for pelvic inflammatory disease. Other red flags for PID include a past history of PID and sexually transmitted diseases. Statistically, sexually active females under the age of 26 are at increased risk for PID.
Risk factors for ectopic pregnancies include a previous history of ectopics and PID, and should be considered while evaluated a woman with concerning symptoms. Age greater than 35 is another risk factor.
Male Pelvic Pain: Obviously there is some overlap in the etiologies of female and male non traumatic pelvic pain, but most etiologies are different. Although men can suffer from diverticulitis, kidney stones, urinary tract infections, and constipation, they obviously have different reproductive organs. Male genitourinary organs, including the prostate, penis, and testicles can be the source of both acute and chronic pelvic pain. Men typically do not suffer from cyclical pelvic pain.
Male urethritis can present with minimal to moderate clear to whitish discharge and dysuria. It is associated with Chlamydia approximate 20-50% of the time. In male patients with dysuria, especially under 35 and sexually active, a chlamydial infection should be suspected. Occasionally, the infection can travel upwards and cause epididymitis. This often prevents as unilaterally scrotal pain associated with single sided swelling and erythema. Exam often reveals exquisite tenderness over the epididymis on the affected side.
Testicular torsion is more common in neonates and post pubertal males but can occur at any age. The abrupt onset of severe hemi scrotal pain is suggestive. Classic physical findings include an elevated, swollen and tender hemi-scrotal and lack of cremasteric reflex (lightly stroking the inner thigh results in an involuntary rising of the scrotum on that side). Color Doppler ultrasound is the most useful imaging technique. It is an important diagnosis to make early as the longer the duration, the more difficult it is to save the testicle. Surgical repair is required.
Prostatitis can be acute or chronic and represents several disorders of the prostate involving inflammation. It can be caused by an acute or chronic bacterial infection, or from non infectious etiologies. An acute infection can be caused by infected urine reflux into the prostate or an ascending infection from the urethra. These are treated with antibiotics, often requiring a long duration up to several months. Non infectious prostatitis is not as well understood and is sometimes treated with non steroidal anti inflammatories or alpha 1 blockers.
Constipation and diverticulitis present similarly as they do in females (see above.) Likewise, kidney stones often present with flank pain which may radiate to the scrotum, along with hematuria (blood in the urine). Bladder infections are less common in males, but will present with painful urination, increased urinary frequency, and occasionally hematuria. Because of urethral length, it is more likely that a male urinary tract infection represents some underlying anatomic abnormality.
Patient Information: Pelvic pain is a common condition for both males and females. Female pelvic pain can have many causes, and a few are quite serious. One should seek prompt medical attention for pelvic pain associated with fevers, vaginal pregnancy, if there is a chance of pregnancy, or is associated with vaginal discharge. Painful urination or pelvic pain associated with back pain likewise requires evaluation.
Other conditions may also require further evaluation including symptoms where are recurrent but bothersome and affecting one?s daily routine.
Male pelvic pain can be caused by multiple issues including infections of the prostate, epididymis, or testicle. High fevers, painful urination, or urethral discharge should prompt medical attention.
References:
Chronic Pelvic Pain, Manish K Singh, MD, Assistant Professor, Pain Management, Department of Neurology, Drexel College of Medicine, Hahnemann University Hospital; eMedicine Online, Article Last Updated: Mar 2, 2006.
Uterine Fibroid Tumors: Diagnosis and Treatment: PATRICIA EVANS, MD, and SUSAN BRUNSELL, MD, American Family Physician; May 15, 2007.
CDC, US Department of Health and Human Services, last updated June 2007: http://www.cdc.gov/std/treatment/2006/updated-regimens.htm
Diagnosis and Management of Ectopic Pregnancy ANNE-MARIE LOZEAU, M.D., M.S., and BETH POTTER, M.D.; American Family Physician, November 1, 2005.
Diagnosis and Management of Endometriosis; ANNE L. MOUNSEY, M.D., University of Virginia School of Medicine, Charlottesville, Virginia, ALEX WILGUS, M.D., Lynchburg Family Medicine Residency Program, Lynchburg, Virginia, and DAVID C. SLAWSON, M.D., University of Virginia School of Medicine, Charlottesville, Virginia; American Family Physician, August 15, 2006.
Gynecologic Pain, Dharmesh Kapoor, MD, MBBS, MRCOG; eMedicine; last edited December 7, 2007.
Fleischer AC, Stein SM, Cullinan JA, Warner MA. Color Doppler sonography of adnexal torsion. J Ultrasound Med. Jul 1995;14(7):523-8. [Medline].
Latthe P, Mignini L, Gray R, Hills R, Khan K (2006). “Factors predisposing women to chronic pelvic pain: systematic review“. BMJ 332 (7544): 749?55. doi:10.1136/bmj.38748.697465.55. PMID 16484239.
Peña JE, Ufberg D, Cooney N, Denis AL. Usefulness of Doppler sonography in the diagnosis of ovarian torsion. Fertil Steril. May 2000;73(5):1047-50. [Medline].
Shadinger LL, Andreotti RF, Kurian RL. Preoperative sonographic and clinical characteristics as predictors of ovarian torsion. J Ultrasound Med. Jan 2008;27(1):7-13. [Medline].
Walker E, Katon W, Harrop-Griffiths et al Relationship of chronic pelvic pain to psychiatric diagnoses and childhood sexual abuse Am J Psychiatry 1988 145:75-80
Pelvic Pain Questions
- Pelvic Inflammatory Disease (PID) can involve all of the following signs/symptoms except:
- Fever
- Cervical Motion Tenderness
- Painful urination
- Vaginal Discharge
- Causes of Acute Pelvic Pain include:
- PID
- Ectopic Pregnancy
- Ovarian Torsion
- All of the above
- Classic Signs/Symptoms of Ectopic Pregnancy include all of the following except:
- Amenorrhea (no periods)
- Vaginal bleeding
- Pelvic Pain
- Fever
- Uterine Fibroids (leiomyomas) typically regress with menopause (T/F)
- True
- False
- Acute Appendicitis typically presents wtih:
- Right Lower Quadrant Pain
- Left Lower Quadrant Pain
- Right Upper Quadrant Pain
- Left Upper Quadrant Pain
- Nephrolithiasis (kidney stones) are associated with:
- Flank Pain
- Hematuria (blood in urine)
- Pain radiating to the groin
- All of the above.
- Dyspareunia is :
- Painful intercourse
- Painful urination
- Painful menstruation
- None of the above.
- Endometriosis can involve:
- Dyspareunia
- Commonly cyclical pain
- Infertility
- All of the above
- Fibroids:
- Sometimes malignant cancers
- Are Benign (non cancerous) growths
- Sometimes arise from the ovary
- None of the above
- A positive pregnancy test along with a normal or slightly enlarged, often tender uterus or adnexal mass is highly suggestive of ectopic pregnancy. (T/F)
- True
- False
- Acute Cystitis is classically associated with:
- Dysuria (painful urination)
- Hematuria (blood in urine)
- Urinary Frequency
- All of the above
- Laboratory measure of hCG (human chorionic gonadotropin) can be a marker for:
- Urinary Tract Infection
- Pregnancy
- Fibroids
- Endometriosis
- Potential Complications of PID include:
- Infertility
- Recurrent PID
- Tubo-ovarian abscess
- All of the above
The preferred imaging technique for ectopic evaluation is:
Plain Xrays
Ultrasound
MRI
CT
Ectopic pregnancies most commonly occur in the:
Uterus
Ovary
Fallopian Tube
Abdomen
- Management of PID typically includes:
- Treatment with a single antibiotic
- Treatment with 2 or more antibiotics
- Watchful waiting
- Surgery
- Management of Diverticulitis:
- Can often be achieved with outpatient antibiotics
- Usually requires surgery
- Can often be managed with analgesia only
- Typically diagnosed by plain x-ray
- Testicular torsion is:
- More common in newborns boys
- Frequently bilaterally (both sides)
- More common in post pubertal boys
- Both a and c
- Acute Prostatitis is:
- Sometimes sexually transmitted
- Caused by retrograde flow of urine
- Always associated with a urinary tract infection
- Both a and b
- Interstitial Cystitis:
- Frequently requires surgery
- Usually cured with antibiotics
- Requires a multidisciplinary approach
- Usually occurs in young children
c
d
d
a
a
d
a
d
b
a
d
b
d
b
c
b
a
d
d
c
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Normal Rectum (above) and Impacted Rectum (below)
The CT scan shows a patient with a normal empty rectum that contains a few bubbles of air (a,b) overlaid in dark orange, and a patient with severe constipation and impaction of feces (c, and d overlay in brown) It is even painful to look at.
colon rectum pain pelvic pain feces fecal impaction constipation mechanical CTscan normal vs abnormal Courtesy Ashley Davidoff MD copyright 2008 18278c02.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Normal Rectum (above) and Impacted Rectum (below)
The CT scan shows a patient with a normal empty rectum that contains a few bubbles of air (a,b) overlaid in dark orange, and a patient with severe constipation and impaction of feces (c, and d overlay in brown) It is even painful to look at.
colon rectum pain pelvic pain feces fecal impaction constipation mechanical CTscan normal vs abnormal Courtesy Ashley Davidoff MD copyright 2008 18278c02.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The CT scan shows a patient with a normal empty rectum that contains a few bubbles of air (a,b) overlaid in dark orange, and a patient with severe constipation and impaction of feces (c, and d overlay in brown) It is even painful to look at.
colon rectum pain pelvic pain feces fecal impaction constipation mechanical CTscan normal vs abnormal Courtesy Ashley Davidoff MD copyright 2008 18278c02.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The CT scan shows a patient with a normal empty rectum that contains a few bubbles of air (a,b) overlaid in dark orange, and a patient with severe constipation and impaction of feces (c, and d overlay in brown) It is even painful to look at.
colon rectum pain pelvic pain feces fecal impaction constipation mechanical CTscan normal vs abnormal Courtesy Ashley Davidoff MD copyright 2008 18278c02.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Normal Rectum (above) and Impacted Rectum (below)
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Normal Rectum (above) and Impacted Rectum (below)
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Acute Diverticulitis – Mouth of Diverticulum is Filled with Pus
This pathological specimen shows the mouth of a diverticulum filled with yellow pus in this patient who had complicated diverticulitis. The tissues surrounding the diverticulum are swollen and red.
12077 colon large bowel fx pus filled purulent diverticulum fx mucosal hyperemia reddening dx acute diverticulitis grosspathology Courtesy Barbara Banner MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Acute Diverticulitis – Mouth of Diverticulum is Filled with Pus
This pathological specimen shows the mouth of a diverticulum filled with yellow pus in this patient who had complicated diverticulitis. The tissues surrounding the diverticulum are swollen and red.
12077 colon large bowel fx pus filled purulent diverticulum fx mucosal hyperemia reddening dx acute diverticulitis grosspathology Courtesy Barbara Banner MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => This pathological specimen shows the mouth of a diverticulum filled with yellow pus in this patient who had complicated diverticulitis. The tissues surrounding the diverticulum are swollen and red.
12077 colon large bowel fx pus filled purulent diverticulum fx mucosal hyperemia reddening dx acute diverticulitis grosspathology Courtesy Barbara Banner MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => This pathological specimen shows the mouth of a diverticulum filled with yellow pus in this patient who had complicated diverticulitis. The tissues surrounding the diverticulum are swollen and red.
12077 colon large bowel fx pus filled purulent diverticulum fx mucosal hyperemia reddening dx acute diverticulitis grosspathology Courtesy Barbara Banner MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Acute Diverticulitis – Mouth of Diverticulum is Filled with Pus
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Acute Diverticulitis – Mouth of Diverticulum is Filled with Pus
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Non inflammed diverticulum (a, b -green), Diverticulitis (c,d), and Pericolic inflammation (red)
The CT scan shows evidence of both diverticulosis and diverticulitis. In images a and b, two small non inflammed outpouchings are seen. The diverticula are outlined in green in b. In the same patient another diverticulum has become inflammed, and diverticulitis is present. This is characterized by induration of the fat around the diverticulum and the colon (maroon) and extension of the inflammatory process to the peritoneal lining (bright red in d). Inflammation of the colon and colonic wall induces visceral pain which is an ache and poorly localized, and inflammation of the peritoneal lining causes a sharp well localised somatic pain that is sensitive to deep palpation.
28582c02 colon descending colon diverticulum diverticulitis pericolic induration acute inflammation acute diverticulitis diverticulosis CTscan Courtesy Ashley Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Non inflammed diverticulum (a, b -green), Diverticulitis (c,d), and Pericolic inflammation (red)
The CT scan shows evidence of both diverticulosis and diverticulitis. In images a and b, two small non inflammed outpouchings are seen. The diverticula are outlined in green in b. In the same patient another diverticulum has become inflammed, and diverticulitis is present. This is characterized by induration of the fat around the diverticulum and the colon (maroon) and extension of the inflammatory process to the peritoneal lining (bright red in d). Inflammation of the colon and colonic wall induces visceral pain which is an ache and poorly localized, and inflammation of the peritoneal lining causes a sharp well localised somatic pain that is sensitive to deep palpation.
28582c02 colon descending colon diverticulum diverticulitis pericolic induration acute inflammation acute diverticulitis diverticulosis CTscan Courtesy Ashley Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The CT scan shows evidence of both diverticulosis and diverticulitis. In images a and b, two small non inflammed outpouchings are seen. The diverticula are outlined in green in b. In the same patient another diverticulum has become inflammed, and diverticulitis is present. This is characterized by induration of the fat around the diverticulum and the colon (maroon) and extension of the inflammatory process to the peritoneal lining (bright red in d). Inflammation of the colon and colonic wall induces visceral pain which is an ache and poorly localized, and inflammation of the peritoneal lining causes a sharp well localised somatic pain that is sensitive to deep palpation.
28582c02 colon descending colon diverticulum diverticulitis pericolic induration acute inflammation acute diverticulitis diverticulosis CTscan Courtesy Ashley Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The CT scan shows evidence of both diverticulosis and diverticulitis. In images a and b, two small non inflammed outpouchings are seen. The diverticula are outlined in green in b. In the same patient another diverticulum has become inflammed, and diverticulitis is present. This is characterized by induration of the fat around the diverticulum and the colon (maroon) and extension of the inflammatory process to the peritoneal lining (bright red in d). Inflammation of the colon and colonic wall induces visceral pain which is an ache and poorly localized, and inflammation of the peritoneal lining causes a sharp well localised somatic pain that is sensitive to deep palpation.
28582c02 colon descending colon diverticulum diverticulitis pericolic induration acute inflammation acute diverticulitis diverticulosis CTscan Courtesy Ashley Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Non inflammed diverticulum (a, b -green), Diverticulitis (c,d), and Pericolic inflammation (red)
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Non inflammed diverticulum (a, b -green), Diverticulitis (c,d), and Pericolic inflammation (red)
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Appendicitis with Significant Perappendiceal Induration
This is a CTscan of a young man who presented with severe somatic pain, well localized to the right lower quadrant. He did not have a fever but had a mildly elevated white cell count. The CT shows an appendix that has a diameter of 8mms., is distended with fluid (yellow in b and d) is surrounded by an hyperemic rim (white rind in a and c – pink around the yellow in b and d) significant induration of the pericolic fat, (maroon) and thickened peritoneum (bright red). It is the latter involvement of the peritoneum that causes the severe well localized somatic pain.
appendix distended colon peritoneal thickening peritonitis CTsca Courteysy Ashley Davidoff MD copyright 2008 44780c01.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Appendicitis with Significant Perappendiceal Induration
This is a CTscan of a young man who presented with severe somatic pain, well localized to the right lower quadrant. He did not have a fever but had a mildly elevated white cell count. The CT shows an appendix that has a diameter of 8mms., is distended with fluid (yellow in b and d) is surrounded by an hyperemic rim (white rind in a and c – pink around the yellow in b and d) significant induration of the pericolic fat, (maroon) and thickened peritoneum (bright red). It is the latter involvement of the peritoneum that causes the severe well localized somatic pain.
appendix distended colon peritoneal thickening peritonitis CTsca Courteysy Ashley Davidoff MD copyright 2008 44780c01.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => This is a CTscan of a young man who presented with severe somatic pain, well localized to the right lower quadrant. He did not have a fever but had a mildly elevated white cell count. The CT shows an appendix that has a diameter of 8mms., is distended with fluid (yellow in b and d) is surrounded by an hyperemic rim (white rind in a and c – pink around the yellow in b and d) significant induration of the pericolic fat, (maroon) and thickened peritoneum (bright red). It is the latter involvement of the peritoneum that causes the severe well localized somatic pain.
appendix distended colon peritoneal thickening peritonitis CTsca Courteysy Ashley Davidoff MD copyright 2008 44780c01.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => This is a CTscan of a young man who presented with severe somatic pain, well localized to the right lower quadrant. He did not have a fever but had a mildly elevated white cell count. The CT shows an appendix that has a diameter of 8mms., is distended with fluid (yellow in b and d) is surrounded by an hyperemic rim (white rind in a and c – pink around the yellow in b and d) significant induration of the pericolic fat, (maroon) and thickened peritoneum (bright red). It is the latter involvement of the peritoneum that causes the severe well localized somatic pain.
appendix distended colon peritoneal thickening peritonitis CTsca Courteysy Ashley Davidoff MD copyright 2008 44780c01.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Appendicitis with Significant Perappendiceal Induration
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Appendicitis with Significant Perappendiceal Induration
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Appendicitis
The ultrasound shows an enlarged (>6mm) appendix with a fecolith in its distal end and which revealed non compressibility and tenderness . The appendix is identified as a blind ending sausage shaped structure in the right lower quadrant
30066 32F RLQ pain colon appendix fx distended enlarged 12mm thickened fx fluid filled dx acute appendicitis USscan Courtesy Ashley Davidoff MD 30066 30067 30074 30076 30077
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Appendicitis
The ultrasound shows an enlarged (>6mm) appendix with a fecolith in its distal end and which revealed non compressibility and tenderness . The appendix is identified as a blind ending sausage shaped structure in the right lower quadrant
30066 32F RLQ pain colon appendix fx distended enlarged 12mm thickened fx fluid filled dx acute appendicitis USscan Courtesy Ashley Davidoff MD 30066 30067 30074 30076 30077
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The ultrasound shows an enlarged (>6mm) appendix with a fecolith in its distal end and which revealed non compressibility and tenderness . The appendix is identified as a blind ending sausage shaped structure in the right lower quadrant
30066 32F RLQ pain colon appendix fx distended enlarged 12mm thickened fx fluid filled dx acute appendicitis USscan Courtesy Ashley Davidoff MD 30066 30067 30074 30076 30077
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The ultrasound shows an enlarged (>6mm) appendix with a fecolith in its distal end and which revealed non compressibility and tenderness . The appendix is identified as a blind ending sausage shaped structure in the right lower quadrant
30066 32F RLQ pain colon appendix fx distended enlarged 12mm thickened fx fluid filled dx acute appendicitis USscan Courtesy Ashley Davidoff MD 30066 30067 30074 30076 30077
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Appendicitis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Appendicitis
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/30077.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/05/30076.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/05/30074.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/05/30067.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/05/30066.jpg
http://thecommonvein.net/media/30066.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Normal and Necrotic
These two pathological specimens of the gallbladder show a normal lily white appendix on the left and a severely inflammed, blackened and necrotic appendix on the right.
02559 colon large bowel appendix grosspathology Courtesy Ted Gulkin MD
courtesy Barbara Banner MD 02435 colon appendix dx black fx distended fx enlarged fx discoloration discolored dx acute gangrenous appendicitis dx ischemic necrosis dx acute appendicitis necrotic grosspathology Courtesy Dr Gutkin
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Normal and Necrotic
These two pathological specimens of the gallbladder show a normal lily white appendix on the left and a severely inflammed, blackened and necrotic appendix on the right.
02559 colon large bowel appendix grosspathology Courtesy Ted Gulkin MD
courtesy Barbara Banner MD 02435 colon appendix dx black fx distended fx enlarged fx discoloration discolored dx acute gangrenous appendicitis dx ischemic necrosis dx acute appendicitis necrotic grosspathology Courtesy Dr Gutkin
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => These two pathological specimens of the gallbladder show a normal lily white appendix on the left and a severely inflammed, blackened and necrotic appendix on the right.
02559 colon large bowel appendix grosspathology Courtesy Ted Gulkin MD
courtesy Barbara Banner MD 02435 colon appendix dx black fx distended fx enlarged fx discoloration discolored dx acute gangrenous appendicitis dx ischemic necrosis dx acute appendicitis necrotic grosspathology Courtesy Dr Gutkin
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => These two pathological specimens of the gallbladder show a normal lily white appendix on the left and a severely inflammed, blackened and necrotic appendix on the right.
02559 colon large bowel appendix grosspathology Courtesy Ted Gulkin MD
courtesy Barbara Banner MD 02435 colon appendix dx black fx distended fx enlarged fx discoloration discolored dx acute gangrenous appendicitis dx ischemic necrosis dx acute appendicitis necrotic grosspathology Courtesy Dr Gutkin
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Normal and Necrotic
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Normal and Necrotic
)
https://beta.thecommonvein.net/wp-content/uploads/2023/04/02559.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/04/02435.jpg
http://thecommonvein.net/media/02559.JPG http://thecommonvein.net/media/02435.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Prolapsing Submucosal Fibroid
This patient presented to the emergency room with severe crampy abdominal pain and a known history of a submucosal fibroid. The MRI shows the fibroid (dark pink) orotruding and expanding the cervix in the sagital view, and in the coronal view it is seen as a hyperemic structure (c) surrounded by lighter pink myometrium.
pain uterus submucosal fibroid prolapse MRI Courtesy Ashley DAvidoff MD copyright 2008 16265c01.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Prolapsing Submucosal Fibroid
This patient presented to the emergency room with severe crampy abdominal pain and a known history of a submucosal fibroid. The MRI shows the fibroid (dark pink) orotruding and expanding the cervix in the sagital view, and in the coronal view it is seen as a hyperemic structure (c) surrounded by lighter pink myometrium.
pain uterus submucosal fibroid prolapse MRI Courtesy Ashley DAvidoff MD copyright 2008 16265c01.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => This patient presented to the emergency room with severe crampy abdominal pain and a known history of a submucosal fibroid. The MRI shows the fibroid (dark pink) orotruding and expanding the cervix in the sagital view, and in the coronal view it is seen as a hyperemic structure (c) surrounded by lighter pink myometrium.
pain uterus submucosal fibroid prolapse MRI Courtesy Ashley DAvidoff MD copyright 2008 16265c01.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => This patient presented to the emergency room with severe crampy abdominal pain and a known history of a submucosal fibroid. The MRI shows the fibroid (dark pink) orotruding and expanding the cervix in the sagital view, and in the coronal view it is seen as a hyperemic structure (c) surrounded by lighter pink myometrium.
pain uterus submucosal fibroid prolapse MRI Courtesy Ashley DAvidoff MD copyright 2008 16265c01.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Prolapsing Submucosal Fibroid
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Prolapsing Submucosal Fibroid
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Retained Products of Conception
The ultrasound is from a 46 patient who presents with bleeding and pain 9 weeks into her pregnancy. Doppler study shows no fetal pole nor fetal heart beat. Findings include a thickened endometrium (light pink) with a focal area in the posterior and fundal portion of the endometrium (dark pink with red blood vessel inside) that enhances, consistent with retained products of conception and spontaneous abortion.
SAB US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008 83222c02.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Retained Products of Conception
The ultrasound is from a 46 patient who presents with bleeding and pain 9 weeks into her pregnancy. Doppler study shows no fetal pole nor fetal heart beat. Findings include a thickened endometrium (light pink) with a focal area in the posterior and fundal portion of the endometrium (dark pink with red blood vessel inside) that enhances, consistent with retained products of conception and spontaneous abortion.
SAB US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008 83222c02.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The ultrasound is from a 46 patient who presents with bleeding and pain 9 weeks into her pregnancy. Doppler study shows no fetal pole nor fetal heart beat. Findings include a thickened endometrium (light pink) with a focal area in the posterior and fundal portion of the endometrium (dark pink with red blood vessel inside) that enhances, consistent with retained products of conception and spontaneous abortion.
SAB US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008 83222c02.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The ultrasound is from a 46 patient who presents with bleeding and pain 9 weeks into her pregnancy. Doppler study shows no fetal pole nor fetal heart beat. Findings include a thickened endometrium (light pink) with a focal area in the posterior and fundal portion of the endometrium (dark pink with red blood vessel inside) that enhances, consistent with retained products of conception and spontaneous abortion.
SAB US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008 83222c02.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Retained Products of Conception
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Retained Products of Conception
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Empty uterus – No IUD, with Normal Left Ovary and Viable Adnexal Ectopic Pregnancy
The ultrasound images from a 32 year old female who presented with severe pelvic pain and a positive HCG. Image (a) shows a normal uterus with no intrauterine pregnancy. Image b shows a left ovary with follicles. Within the left adnexa, a fetal pole with beating heart (red dot in c) measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. These findings are consistent with an ectopic pregnancy.
75791c01 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = no intraurterine pregnancy complex free fluid probably blood and hemorrhage b = normal left ovary c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Empty uterus – No IUD, with Normal Left Ovary and Viable Adnexal Ectopic Pregnancy
The ultrasound images from a 32 year old female who presented with severe pelvic pain and a positive HCG. Image (a) shows a normal uterus with no intrauterine pregnancy. Image b shows a left ovary with follicles. Within the left adnexa, a fetal pole with beating heart (red dot in c) measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. These findings are consistent with an ectopic pregnancy.
75791c01 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = no intraurterine pregnancy complex free fluid probably blood and hemorrhage b = normal left ovary c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The ultrasound images from a 32 year old female who presented with severe pelvic pain and a positive HCG. Image (a) shows a normal uterus with no intrauterine pregnancy. Image b shows a left ovary with follicles. Within the left adnexa, a fetal pole with beating heart (red dot in c) measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. These findings are consistent with an ectopic pregnancy.
75791c01 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = no intraurterine pregnancy complex free fluid probably blood and hemorrhage b = normal left ovary c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The ultrasound images from a 32 year old female who presented with severe pelvic pain and a positive HCG. Image (a) shows a normal uterus with no intrauterine pregnancy. Image b shows a left ovary with follicles. Within the left adnexa, a fetal pole with beating heart (red dot in c) measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. These findings are consistent with an ectopic pregnancy.
75791c01 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = no intraurterine pregnancy complex free fluid probably blood and hemorrhage b = normal left ovary c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Empty uterus – No IUD, with Normal Left Ovary and Viable Adnexal Ectopic Pregnancy
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Empty uterus – No IUD, with Normal Left Ovary and Viable Adnexal Ectopic Pregnancy
)
https://beta.thecommonvein.net/wp-content/uploads/2023/06/75792c01.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/75791c03.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/75791c01.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/75791.jpg
http://thecommonvein.net/media/75791c01.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
The Normal Fallopian Tubes
46376 4376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
The Normal Fallopian Tubes
46376 4376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] =>
[lastElementChild] =>
[childElementCount] => 0
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => 46376 4376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => 46376 4376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The Normal Fallopian Tubes
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The Normal Fallopian Tubes
)
https://beta.thecommonvein.net/wp-content/uploads/2023/06/46376.jpg
http://thecommonvein.net/media/46376b01b01b03.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Normal (above) and Endometritis (below)
The CTscan through the pelvis in the top image shows a heart shaped fluid filled endometrium with no enhancement of the mucosa and this patient was normal except for a focal probable physiologic process in the left adnexa and a small amount of free fluid in the right pararectal space. The second image is from a 20 year old female with severe colitis who demonstrates an enhancing endometrium that is suggestive of acute endomtritis. In addition she has a large amount of ascites allowing us to visualize both ovaries and broad ligaments.
46355
45318 hx 20 F with acute diarrhea and abdominal pain uterus endometrium fx fluid filled adnexa ovary ovaries normal fx ascites fx fluid in the rectum dx infectious colitis CTscan Courtesy Ashley Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Normal (above) and Endometritis (below)
The CTscan through the pelvis in the top image shows a heart shaped fluid filled endometrium with no enhancement of the mucosa and this patient was normal except for a focal probable physiologic process in the left adnexa and a small amount of free fluid in the right pararectal space. The second image is from a 20 year old female with severe colitis who demonstrates an enhancing endometrium that is suggestive of acute endomtritis. In addition she has a large amount of ascites allowing us to visualize both ovaries and broad ligaments.
46355
45318 hx 20 F with acute diarrhea and abdominal pain uterus endometrium fx fluid filled adnexa ovary ovaries normal fx ascites fx fluid in the rectum dx infectious colitis CTscan Courtesy Ashley Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The CTscan through the pelvis in the top image shows a heart shaped fluid filled endometrium with no enhancement of the mucosa and this patient was normal except for a focal probable physiologic process in the left adnexa and a small amount of free fluid in the right pararectal space. The second image is from a 20 year old female with severe colitis who demonstrates an enhancing endometrium that is suggestive of acute endomtritis. In addition she has a large amount of ascites allowing us to visualize both ovaries and broad ligaments.
46355
45318 hx 20 F with acute diarrhea and abdominal pain uterus endometrium fx fluid filled adnexa ovary ovaries normal fx ascites fx fluid in the rectum dx infectious colitis CTscan Courtesy Ashley Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The CTscan through the pelvis in the top image shows a heart shaped fluid filled endometrium with no enhancement of the mucosa and this patient was normal except for a focal probable physiologic process in the left adnexa and a small amount of free fluid in the right pararectal space. The second image is from a 20 year old female with severe colitis who demonstrates an enhancing endometrium that is suggestive of acute endomtritis. In addition she has a large amount of ascites allowing us to visualize both ovaries and broad ligaments.
46355
45318 hx 20 F with acute diarrhea and abdominal pain uterus endometrium fx fluid filled adnexa ovary ovaries normal fx ascites fx fluid in the rectum dx infectious colitis CTscan Courtesy Ashley Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Normal (above) and Endometritis (below)
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Normal (above) and Endometritis (below)
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Left Ovarian Abscess
The CT is from a 36 year old female recently post cesarian section who developed pain the left lower quadrant, fever and rigors. She has a known fibroid uterus but a new tender mass was found in her left adnexa. The CTscan shows a large cystic collection in the left adnexa(dark yellow) with an enhancing rind. Pus was aspirated under ultrasound guidance , and a diagnosis of an ovarian abscess was made. She was treated on antibiotics and she subsequently her pain and fever resolved . The axial view (a,d) shows a 10.7 cms abscess. The coronal view (b,e) shows the large abscess in the left adnexa with a smaller abscess just below it (yellow) adnexa with the uterus and its endometrial cavity(maroon) and a fibroid in orange. The sagittal view (c,f) shows an irregular uterus (pink) with endometrial cavity (maroon) and a few fibroids (orange)
pain ovary PID pelvic inflammatory disease infection abscess CTscan Ashley DAvidoff MD copyright 2008 83287c03.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Left Ovarian Abscess
The CT is from a 36 year old female recently post cesarian section who developed pain the left lower quadrant, fever and rigors. She has a known fibroid uterus but a new tender mass was found in her left adnexa. The CTscan shows a large cystic collection in the left adnexa(dark yellow) with an enhancing rind. Pus was aspirated under ultrasound guidance , and a diagnosis of an ovarian abscess was made. She was treated on antibiotics and she subsequently her pain and fever resolved . The axial view (a,d) shows a 10.7 cms abscess. The coronal view (b,e) shows the large abscess in the left adnexa with a smaller abscess just below it (yellow) adnexa with the uterus and its endometrial cavity(maroon) and a fibroid in orange. The sagittal view (c,f) shows an irregular uterus (pink) with endometrial cavity (maroon) and a few fibroids (orange)
pain ovary PID pelvic inflammatory disease infection abscess CTscan Ashley DAvidoff MD copyright 2008 83287c03.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The CT is from a 36 year old female recently post cesarian section who developed pain the left lower quadrant, fever and rigors. She has a known fibroid uterus but a new tender mass was found in her left adnexa. The CTscan shows a large cystic collection in the left adnexa(dark yellow) with an enhancing rind. Pus was aspirated under ultrasound guidance , and a diagnosis of an ovarian abscess was made. She was treated on antibiotics and she subsequently her pain and fever resolved . The axial view (a,d) shows a 10.7 cms abscess. The coronal view (b,e) shows the large abscess in the left adnexa with a smaller abscess just below it (yellow) adnexa with the uterus and its endometrial cavity(maroon) and a fibroid in orange. The sagittal view (c,f) shows an irregular uterus (pink) with endometrial cavity (maroon) and a few fibroids (orange)
pain ovary PID pelvic inflammatory disease infection abscess CTscan Ashley DAvidoff MD copyright 2008 83287c03.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The CT is from a 36 year old female recently post cesarian section who developed pain the left lower quadrant, fever and rigors. She has a known fibroid uterus but a new tender mass was found in her left adnexa. The CTscan shows a large cystic collection in the left adnexa(dark yellow) with an enhancing rind. Pus was aspirated under ultrasound guidance , and a diagnosis of an ovarian abscess was made. She was treated on antibiotics and she subsequently her pain and fever resolved . The axial view (a,d) shows a 10.7 cms abscess. The coronal view (b,e) shows the large abscess in the left adnexa with a smaller abscess just below it (yellow) adnexa with the uterus and its endometrial cavity(maroon) and a fibroid in orange. The sagittal view (c,f) shows an irregular uterus (pink) with endometrial cavity (maroon) and a few fibroids (orange)
pain ovary PID pelvic inflammatory disease infection abscess CTscan Ashley DAvidoff MD copyright 2008 83287c03.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Left Ovarian Abscess
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Left Ovarian Abscess
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Left Sided Ruptured Hemorrhagic Cyst with Free Blood in the Pelvis and Bleeding onto the Greater Omentum RLQ (pink)
This CT scan is that of a 27 year old female who presented with acute lower pelvic pain in mid cycle. The findings of free blood in the pelvis (maroon) the cyst (yellow) with an enhancing rim (bright red) and spillage of blood onto the greater omentum (pink let anterior) are consistent with a ruptured hemorrhagic cyst . The intense ring around the cyst suggests that a corpus luteum cyst has formed already.
24480c01 27 year old female presented with lower abdominal pain pelvic pain ovary fx cyst cul de sac blood free blood hyperdense corpus luteum cyst greater ometum congested fx enhancing dx hemorhagic ovarian cyst CT scan C- CTscan Courtesy Ashley DAvidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Left Sided Ruptured Hemorrhagic Cyst with Free Blood in the Pelvis and Bleeding onto the Greater Omentum RLQ (pink)
This CT scan is that of a 27 year old female who presented with acute lower pelvic pain in mid cycle. The findings of free blood in the pelvis (maroon) the cyst (yellow) with an enhancing rim (bright red) and spillage of blood onto the greater omentum (pink let anterior) are consistent with a ruptured hemorrhagic cyst . The intense ring around the cyst suggests that a corpus luteum cyst has formed already.
24480c01 27 year old female presented with lower abdominal pain pelvic pain ovary fx cyst cul de sac blood free blood hyperdense corpus luteum cyst greater ometum congested fx enhancing dx hemorhagic ovarian cyst CT scan C- CTscan Courtesy Ashley DAvidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => This CT scan is that of a 27 year old female who presented with acute lower pelvic pain in mid cycle. The findings of free blood in the pelvis (maroon) the cyst (yellow) with an enhancing rim (bright red) and spillage of blood onto the greater omentum (pink let anterior) are consistent with a ruptured hemorrhagic cyst . The intense ring around the cyst suggests that a corpus luteum cyst has formed already.
24480c01 27 year old female presented with lower abdominal pain pelvic pain ovary fx cyst cul de sac blood free blood hyperdense corpus luteum cyst greater ometum congested fx enhancing dx hemorhagic ovarian cyst CT scan C- CTscan Courtesy Ashley DAvidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => This CT scan is that of a 27 year old female who presented with acute lower pelvic pain in mid cycle. The findings of free blood in the pelvis (maroon) the cyst (yellow) with an enhancing rim (bright red) and spillage of blood onto the greater omentum (pink let anterior) are consistent with a ruptured hemorrhagic cyst . The intense ring around the cyst suggests that a corpus luteum cyst has formed already.
24480c01 27 year old female presented with lower abdominal pain pelvic pain ovary fx cyst cul de sac blood free blood hyperdense corpus luteum cyst greater ometum congested fx enhancing dx hemorhagic ovarian cyst CT scan C- CTscan Courtesy Ashley DAvidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Left Sided Ruptured Hemorrhagic Cyst with Free Blood in the Pelvis and Bleeding onto the Greater Omentum RLQ (pink)
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Left Sided Ruptured Hemorrhagic Cyst with Free Blood in the Pelvis and Bleeding onto the Greater Omentum RLQ (pink)
)
https://beta.thecommonvein.net/wp-content/uploads/2023/05/24480c01.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
83268c02.8c
26 year old female presents with acute midcycle right lower quadrant pain without a fever, associated with peritonism in the right lower quadrant. Differential diagnosis included appendicitis, ruptured cyst, torsion, endometrioma and ectopic pregnancy, but her HCG was normal.
The CTscan shows acute hemorrhage in a cyst int the right adnexa consistent with a hemorrhagic and ruptured follicle, (maroon nodule with a pink circle in b), but also shows a large amount of blood and fluid, some accumulating in the right lower quadrant, (light pink anteriorly on right in b) some in the cul de sac (bright red sediment, and light pink supernatant in b) and some in the greater omentum on the right side (maroon in d). It is the latter component that incites the somatic nocicptors of the peritoneum to simulate peritonitis.
The patient was treated conservatively and improved over the next 24-48 hours.
pain ovary mittelschmerz hemorrhage rupture right lower quadrant pain RLQ peritonism peritonitis CTscan Courtesy Ashley Davidoff MD copyright 2008 83268c02.8c
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
83268c02.8c
26 year old female presents with acute midcycle right lower quadrant pain without a fever, associated with peritonism in the right lower quadrant. Differential diagnosis included appendicitis, ruptured cyst, torsion, endometrioma and ectopic pregnancy, but her HCG was normal.
The CTscan shows acute hemorrhage in a cyst int the right adnexa consistent with a hemorrhagic and ruptured follicle, (maroon nodule with a pink circle in b), but also shows a large amount of blood and fluid, some accumulating in the right lower quadrant, (light pink anteriorly on right in b) some in the cul de sac (bright red sediment, and light pink supernatant in b) and some in the greater omentum on the right side (maroon in d). It is the latter component that incites the somatic nocicptors of the peritoneum to simulate peritonitis.
The patient was treated conservatively and improved over the next 24-48 hours.
pain ovary mittelschmerz hemorrhage rupture right lower quadrant pain RLQ peritonism peritonitis CTscan Courtesy Ashley Davidoff MD copyright 2008 83268c02.8c
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => 26 year old female presents with acute midcycle right lower quadrant pain without a fever, associated with peritonism in the right lower quadrant. Differential diagnosis included appendicitis, ruptured cyst, torsion, endometrioma and ectopic pregnancy, but her HCG was normal.
The CTscan shows acute hemorrhage in a cyst int the right adnexa consistent with a hemorrhagic and ruptured follicle, (maroon nodule with a pink circle in b), but also shows a large amount of blood and fluid, some accumulating in the right lower quadrant, (light pink anteriorly on right in b) some in the cul de sac (bright red sediment, and light pink supernatant in b) and some in the greater omentum on the right side (maroon in d). It is the latter component that incites the somatic nocicptors of the peritoneum to simulate peritonitis.
The patient was treated conservatively and improved over the next 24-48 hours.
pain ovary mittelschmerz hemorrhage rupture right lower quadrant pain RLQ peritonism peritonitis CTscan Courtesy Ashley Davidoff MD copyright 2008 83268c02.8c
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => 26 year old female presents with acute midcycle right lower quadrant pain without a fever, associated with peritonism in the right lower quadrant. Differential diagnosis included appendicitis, ruptured cyst, torsion, endometrioma and ectopic pregnancy, but her HCG was normal.
The CTscan shows acute hemorrhage in a cyst int the right adnexa consistent with a hemorrhagic and ruptured follicle, (maroon nodule with a pink circle in b), but also shows a large amount of blood and fluid, some accumulating in the right lower quadrant, (light pink anteriorly on right in b) some in the cul de sac (bright red sediment, and light pink supernatant in b) and some in the greater omentum on the right side (maroon in d). It is the latter component that incites the somatic nocicptors of the peritoneum to simulate peritonitis.
The patient was treated conservatively and improved over the next 24-48 hours.
pain ovary mittelschmerz hemorrhage rupture right lower quadrant pain RLQ peritonism peritonitis CTscan Courtesy Ashley Davidoff MD copyright 2008 83268c02.8c
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => 83268c02.8c
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => 83268c02.8c
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Hemorrhage into a Cyst with Clot Formation
The ultrasound (a,b,c) and CTscan (d,e) are from a 39year old female with midcycle pain and show linear stranding and soft tissue changes into a large cyst in the left adnexa (a and b), with the hemorrhage outlined in maroon in b and displaced crescentic ovary in pink. The hemorrhage consists of soft tissue components (dark maroon in b) and the lighter maroon overlies the fibrinous and linear component of the clot that is better visualized in a. The doppler study in c, shows no color in the cyst implying that it is a non vascular structure. These findings are most characteristic of a cyst that has hemorrhaged into the cyst but without rupture of the cyst. The sudden distension of the cyst incites the pressure receptors and accounts for the pain.
The CTscan limoited to the bladder and left adnexa in d, shows a rounded complex lesion in the left adnexa with a fluid fluid level overlaid in maroon in e. This reflects sedimented red cells that were free to fall to the dependant portion of the hemorrhagic cyst.
ovary cyst hemorrhage clot fibrin pain midcycle USscan ultrasound Courtesy Ashley Davidoff MD copyright 2008 83279c02.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Hemorrhage into a Cyst with Clot Formation
The ultrasound (a,b,c) and CTscan (d,e) are from a 39year old female with midcycle pain and show linear stranding and soft tissue changes into a large cyst in the left adnexa (a and b), with the hemorrhage outlined in maroon in b and displaced crescentic ovary in pink. The hemorrhage consists of soft tissue components (dark maroon in b) and the lighter maroon overlies the fibrinous and linear component of the clot that is better visualized in a. The doppler study in c, shows no color in the cyst implying that it is a non vascular structure. These findings are most characteristic of a cyst that has hemorrhaged into the cyst but without rupture of the cyst. The sudden distension of the cyst incites the pressure receptors and accounts for the pain.
The CTscan limoited to the bladder and left adnexa in d, shows a rounded complex lesion in the left adnexa with a fluid fluid level overlaid in maroon in e. This reflects sedimented red cells that were free to fall to the dependant portion of the hemorrhagic cyst.
ovary cyst hemorrhage clot fibrin pain midcycle USscan ultrasound Courtesy Ashley Davidoff MD copyright 2008 83279c02.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The ultrasound (a,b,c) and CTscan (d,e) are from a 39year old female with midcycle pain and show linear stranding and soft tissue changes into a large cyst in the left adnexa (a and b), with the hemorrhage outlined in maroon in b and displaced crescentic ovary in pink. The hemorrhage consists of soft tissue components (dark maroon in b) and the lighter maroon overlies the fibrinous and linear component of the clot that is better visualized in a. The doppler study in c, shows no color in the cyst implying that it is a non vascular structure. These findings are most characteristic of a cyst that has hemorrhaged into the cyst but without rupture of the cyst. The sudden distension of the cyst incites the pressure receptors and accounts for the pain.
The CTscan limoited to the bladder and left adnexa in d, shows a rounded complex lesion in the left adnexa with a fluid fluid level overlaid in maroon in e. This reflects sedimented red cells that were free to fall to the dependant portion of the hemorrhagic cyst.
ovary cyst hemorrhage clot fibrin pain midcycle USscan ultrasound Courtesy Ashley Davidoff MD copyright 2008 83279c02.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The ultrasound (a,b,c) and CTscan (d,e) are from a 39year old female with midcycle pain and show linear stranding and soft tissue changes into a large cyst in the left adnexa (a and b), with the hemorrhage outlined in maroon in b and displaced crescentic ovary in pink. The hemorrhage consists of soft tissue components (dark maroon in b) and the lighter maroon overlies the fibrinous and linear component of the clot that is better visualized in a. The doppler study in c, shows no color in the cyst implying that it is a non vascular structure. These findings are most characteristic of a cyst that has hemorrhaged into the cyst but without rupture of the cyst. The sudden distension of the cyst incites the pressure receptors and accounts for the pain.
The CTscan limoited to the bladder and left adnexa in d, shows a rounded complex lesion in the left adnexa with a fluid fluid level overlaid in maroon in e. This reflects sedimented red cells that were free to fall to the dependant portion of the hemorrhagic cyst.
ovary cyst hemorrhage clot fibrin pain midcycle USscan ultrasound Courtesy Ashley Davidoff MD copyright 2008 83279c02.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Hemorrhage into a Cyst with Clot Formation
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Hemorrhage into a Cyst with Clot Formation
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Normal (a) and Large Unruptured Follicles (b)
The ultrasound shows a normal left ovary with small Graaffian follicles (a) and an enlarged ovary with two unruptured simple cysts (b) The latter study is from is from a 46 year female who presents with pelvic discomfort. The transvaginal ultrasound (b) shows a large 6cms ovary that contains two cysts each about 2cms in size.. The ovary is about twice to 3 times normal in size and the distension presumably causes the discomfort. The cysts are simple in nature without hemorrhage.
ovary pain cysts discomfort nrmal variant enlarged normal follicles USscan ultrasound copyright 2008 Courtesy Ashley Davidoff MD 83269c.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Normal (a) and Large Unruptured Follicles (b)
The ultrasound shows a normal left ovary with small Graaffian follicles (a) and an enlarged ovary with two unruptured simple cysts (b) The latter study is from is from a 46 year female who presents with pelvic discomfort. The transvaginal ultrasound (b) shows a large 6cms ovary that contains two cysts each about 2cms in size.. The ovary is about twice to 3 times normal in size and the distension presumably causes the discomfort. The cysts are simple in nature without hemorrhage.
ovary pain cysts discomfort nrmal variant enlarged normal follicles USscan ultrasound copyright 2008 Courtesy Ashley Davidoff MD 83269c.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The ultrasound shows a normal left ovary with small Graaffian follicles (a) and an enlarged ovary with two unruptured simple cysts (b) The latter study is from is from a 46 year female who presents with pelvic discomfort. The transvaginal ultrasound (b) shows a large 6cms ovary that contains two cysts each about 2cms in size.. The ovary is about twice to 3 times normal in size and the distension presumably causes the discomfort. The cysts are simple in nature without hemorrhage.
ovary pain cysts discomfort nrmal variant enlarged normal follicles USscan ultrasound copyright 2008 Courtesy Ashley Davidoff MD 83269c.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The ultrasound shows a normal left ovary with small Graaffian follicles (a) and an enlarged ovary with two unruptured simple cysts (b) The latter study is from is from a 46 year female who presents with pelvic discomfort. The transvaginal ultrasound (b) shows a large 6cms ovary that contains two cysts each about 2cms in size.. The ovary is about twice to 3 times normal in size and the distension presumably causes the discomfort. The cysts are simple in nature without hemorrhage.
ovary pain cysts discomfort nrmal variant enlarged normal follicles USscan ultrasound copyright 2008 Courtesy Ashley Davidoff MD 83269c.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Normal (a) and Large Unruptured Follicles (b)
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Normal (a) and Large Unruptured Follicles (b)
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Ovulation and Mittelschmerz
The transvaginal ultrasound focuses on the ovary (pink oval structure) of a young woman who was complaining of midcycle pain. A decompressed Graaffian follicle (inverted teardrop shaped yellow structure in the ovary) is seen emptying its contents into the peritoneal cavity, causing a triangular shaped accumulation of fluid in the peritoneal cavity (yellow triangle). It is the shape of the follicle and its proximity to the fluid in the peritoneum together with the concordant site of the pain that allowed the diagnosis of mittelschmerz to be made.
47025c01 young patient with known ovulation one day earlier ovary Graafian follicle rupture tear drop shape pear shaped ovulation physiology normal anatomy USscan Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Ovulation and Mittelschmerz
The transvaginal ultrasound focuses on the ovary (pink oval structure) of a young woman who was complaining of midcycle pain. A decompressed Graaffian follicle (inverted teardrop shaped yellow structure in the ovary) is seen emptying its contents into the peritoneal cavity, causing a triangular shaped accumulation of fluid in the peritoneal cavity (yellow triangle). It is the shape of the follicle and its proximity to the fluid in the peritoneum together with the concordant site of the pain that allowed the diagnosis of mittelschmerz to be made.
47025c01 young patient with known ovulation one day earlier ovary Graafian follicle rupture tear drop shape pear shaped ovulation physiology normal anatomy USscan Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The transvaginal ultrasound focuses on the ovary (pink oval structure) of a young woman who was complaining of midcycle pain. A decompressed Graaffian follicle (inverted teardrop shaped yellow structure in the ovary) is seen emptying its contents into the peritoneal cavity, causing a triangular shaped accumulation of fluid in the peritoneal cavity (yellow triangle). It is the shape of the follicle and its proximity to the fluid in the peritoneum together with the concordant site of the pain that allowed the diagnosis of mittelschmerz to be made.
47025c01 young patient with known ovulation one day earlier ovary Graafian follicle rupture tear drop shape pear shaped ovulation physiology normal anatomy USscan Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The transvaginal ultrasound focuses on the ovary (pink oval structure) of a young woman who was complaining of midcycle pain. A decompressed Graaffian follicle (inverted teardrop shaped yellow structure in the ovary) is seen emptying its contents into the peritoneal cavity, causing a triangular shaped accumulation of fluid in the peritoneal cavity (yellow triangle). It is the shape of the follicle and its proximity to the fluid in the peritoneum together with the concordant site of the pain that allowed the diagnosis of mittelschmerz to be made.
47025c01 young patient with known ovulation one day earlier ovary Graafian follicle rupture tear drop shape pear shaped ovulation physiology normal anatomy USscan Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Ovulation and Mittelschmerz
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Ovulation and Mittelschmerz
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Endometrioma Left Ovary
25 year old female presents with painful menses. The ultrasound shows a cystic mass in the pelvis with a large amount of debris in the cystic cavity consistent with a chocolate cyst. Although the appearance is consistent with endometriosis, a hemorrhagic cycts is possible and the distiction may only be made pathologicallly
uterus pain ovary hemorrhagic cyst endometrioma 83261c01.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Endometrioma Left Ovary
25 year old female presents with painful menses. The ultrasound shows a cystic mass in the pelvis with a large amount of debris in the cystic cavity consistent with a chocolate cyst. Although the appearance is consistent with endometriosis, a hemorrhagic cycts is possible and the distiction may only be made pathologicallly
uterus pain ovary hemorrhagic cyst endometrioma 83261c01.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => 25 year old female presents with painful menses. The ultrasound shows a cystic mass in the pelvis with a large amount of debris in the cystic cavity consistent with a chocolate cyst. Although the appearance is consistent with endometriosis, a hemorrhagic cycts is possible and the distiction may only be made pathologicallly
uterus pain ovary hemorrhagic cyst endometrioma 83261c01.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => 25 year old female presents with painful menses. The ultrasound shows a cystic mass in the pelvis with a large amount of debris in the cystic cavity consistent with a chocolate cyst. Although the appearance is consistent with endometriosis, a hemorrhagic cycts is possible and the distiction may only be made pathologicallly
uterus pain ovary hemorrhagic cyst endometrioma 83261c01.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Endometrioma Left Ovary
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Endometrioma Left Ovary
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Denuded Endometrium
The longitudinal view of the uterus is shown in the ultrasound of this young patient who was having severe pain during her menses. The images show part of the endometrial lining within the lumen (maroon), with a small amount of blood (bright red), and the remaining endometrium lining (pink). The denuded endometrium and associated clots cause prostaglandins to be released which induce muscle contraction, and these are the primary cause of the pain.
83218c02.8s 42F pain during menses menstrual cycle cyclical pain uterus endometrium shedding of the endometrium contraction expulsion menstrual cramps US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Denuded Endometrium
The longitudinal view of the uterus is shown in the ultrasound of this young patient who was having severe pain during her menses. The images show part of the endometrial lining within the lumen (maroon), with a small amount of blood (bright red), and the remaining endometrium lining (pink). The denuded endometrium and associated clots cause prostaglandins to be released which induce muscle contraction, and these are the primary cause of the pain.
83218c02.8s 42F pain during menses menstrual cycle cyclical pain uterus endometrium shedding of the endometrium contraction expulsion menstrual cramps US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The longitudinal view of the uterus is shown in the ultrasound of this young patient who was having severe pain during her menses. The images show part of the endometrial lining within the lumen (maroon), with a small amount of blood (bright red), and the remaining endometrium lining (pink). The denuded endometrium and associated clots cause prostaglandins to be released which induce muscle contraction, and these are the primary cause of the pain.
83218c02.8s 42F pain during menses menstrual cycle cyclical pain uterus endometrium shedding of the endometrium contraction expulsion menstrual cramps US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The longitudinal view of the uterus is shown in the ultrasound of this young patient who was having severe pain during her menses. The images show part of the endometrial lining within the lumen (maroon), with a small amount of blood (bright red), and the remaining endometrium lining (pink). The denuded endometrium and associated clots cause prostaglandins to be released which induce muscle contraction, and these are the primary cause of the pain.
83218c02.8s 42F pain during menses menstrual cycle cyclical pain uterus endometrium shedding of the endometrium contraction expulsion menstrual cramps US ultrasound USscan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Denuded Endometrium
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Denuded Endometrium
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Acute Debilitating Pelvic Pain – Artistic Rendition
89081pd04b09.8s pain abdomen sleep woken awakened from sleep somatic peritoneal peritonitis Davidoff art copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Acute Debilitating Pelvic Pain – Artistic Rendition
89081pd04b09.8s pain abdomen sleep woken awakened from sleep somatic peritoneal peritonitis Davidoff art copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] =>
[lastElementChild] =>
[childElementCount] => 0
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => 89081pd04b09.8s pain abdomen sleep woken awakened from sleep somatic peritoneal peritonitis Davidoff art copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => 89081pd04b09.8s pain abdomen sleep woken awakened from sleep somatic peritoneal peritonitis Davidoff art copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Acute Debilitating Pelvic Pain – Artistic Rendition
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Acute Debilitating Pelvic Pain – Artistic Rendition
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Hysterosalpingogram Fallopian Tubes
46376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MDpelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Hysterosalpingogram Fallopian Tubes
46376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MDpelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] =>
[lastElementChild] =>
[childElementCount] => 0
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => 46376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MDpelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => 46376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MDpelvis uterus Fallopian tubes fimbrae uterus uterine cavity cervix vagina fornix hysterosalpingogram Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Hysterosalpingogram Fallopian Tubes
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Hysterosalpingogram Fallopian Tubes
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Normal Ovary with Follicles
The transvaginal ultrasound shows a normal right ovary in longitudinal view containing black cystic follicles that are all about the same size and are all less than 1cms in diameter.
71689 ovary follicles normal anatomy function physiology TCV Applied Biology Cycle time USscan Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Normal Ovary with Follicles
The transvaginal ultrasound shows a normal right ovary in longitudinal view containing black cystic follicles that are all about the same size and are all less than 1cms in diameter.
71689 ovary follicles normal anatomy function physiology TCV Applied Biology Cycle time USscan Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The transvaginal ultrasound shows a normal right ovary in longitudinal view containing black cystic follicles that are all about the same size and are all less than 1cms in diameter.
71689 ovary follicles normal anatomy function physiology TCV Applied Biology Cycle time USscan Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The transvaginal ultrasound shows a normal right ovary in longitudinal view containing black cystic follicles that are all about the same size and are all less than 1cms in diameter.
71689 ovary follicles normal anatomy function physiology TCV Applied Biology Cycle time USscan Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Normal Ovary with Follicles
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Normal Ovary with Follicles
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
The Almond
The almond not only has the same shape as the ovary, but also has almost the same size.
82470.81s fruit nut food food in the body shape almond ovary amygdala Davidoff photography copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
The Almond
The almond not only has the same shape as the ovary, but also has almost the same size.
82470.81s fruit nut food food in the body shape almond ovary amygdala Davidoff photography copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The almond not only has the same shape as the ovary, but also has almost the same size.
82470.81s fruit nut food food in the body shape almond ovary amygdala Davidoff photography copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The almond not only has the same shape as the ovary, but also has almost the same size.
82470.81s fruit nut food food in the body shape almond ovary amygdala Davidoff photography copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The Almond
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The Almond
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
The Normal Uterus End of Luteal (Secretory) Phase
The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
The Normal Uterus End of Luteal (Secretory) Phase
The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The Normal Uterus End of Luteal (Secretory) Phase
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The Normal Uterus End of Luteal (Secretory) Phase
)
https://beta.thecommonvein.net/wp-content/uploads/2023/06/46315.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
The Normal Uterus End of Luteal (Secretory) Phase
The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
The Normal Uterus End of Luteal (Secretory) Phase
The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The endometrial stripe is now seen as a much thickened three times thicker than in the proliferative phase and measures about 1.5cms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The Normal Uterus End of Luteal (Secretory) Phase
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The Normal Uterus End of Luteal (Secretory) Phase
)
https://beta.thecommonvein.net/wp-content/uploads/2023/06/46315.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
The Normal Uterus During Follicular (Proliferative) Phase
The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The pearshaped structure, wirth fundus to the left of the image and lower uterine segment measures 8.7cms in length. The endometrial stripe is seen in the center as an echogenic line and measures about 5mms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
The Normal Uterus During Follicular (Proliferative) Phase
The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The pearshaped structure, wirth fundus to the left of the image and lower uterine segment measures 8.7cms in length. The endometrial stripe is seen in the center as an echogenic line and measures about 5mms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The pearshaped structure, wirth fundus to the left of the image and lower uterine segment measures 8.7cms in length. The endometrial stripe is seen in the center as an echogenic line and measures about 5mms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The longitudinal view of the uterus is depicted by using transvaginal ultrasound. The pearshaped structure, wirth fundus to the left of the image and lower uterine segment measures 8.7cms in length. The endometrial stripe is seen in the center as an echogenic line and measures about 5mms.
46315 uterus endometrium shape normal anatomy USscan Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The Normal Uterus During Follicular (Proliferative) Phase
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The Normal Uterus During Follicular (Proliferative) Phase
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Pregnancy – Physiological and Temporary Space Occupation
The MRI shows a fetus with vertex (head) presentation lying within the gestational sac filled with fluid (white), taking up the space of the pelvic cavity and to some extent the abdominal cavity and displacing normal structures into the abdomen.
46704 abdomen pregnancy fetus baby head brain lungs amniotic cavity amniotic fluid normal anatomy physiology MRI T2 weighted Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Pregnancy – Physiological and Temporary Space Occupation
The MRI shows a fetus with vertex (head) presentation lying within the gestational sac filled with fluid (white), taking up the space of the pelvic cavity and to some extent the abdominal cavity and displacing normal structures into the abdomen.
46704 abdomen pregnancy fetus baby head brain lungs amniotic cavity amniotic fluid normal anatomy physiology MRI T2 weighted Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The MRI shows a fetus with vertex (head) presentation lying within the gestational sac filled with fluid (white), taking up the space of the pelvic cavity and to some extent the abdominal cavity and displacing normal structures into the abdomen.
46704 abdomen pregnancy fetus baby head brain lungs amniotic cavity amniotic fluid normal anatomy physiology MRI T2 weighted Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The MRI shows a fetus with vertex (head) presentation lying within the gestational sac filled with fluid (white), taking up the space of the pelvic cavity and to some extent the abdominal cavity and displacing normal structures into the abdomen.
46704 abdomen pregnancy fetus baby head brain lungs amniotic cavity amniotic fluid normal anatomy physiology MRI T2 weighted Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Pregnancy – Physiological and Temporary Space Occupation
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Pregnancy – Physiological and Temporary Space Occupation
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
The Normal Pelvis
The bony pelvis is shown in the above CT scan reconstruction. While the iliac crests and ischia and pubic symphisis are well shown, the sacral component is hidden by parts of the gastrointestinal tract.
71198b01 pelvis bone iliac crest pubic symphisis hip ischial tuberosity pubic bone normal anatomy CTscan 3D Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
The Normal Pelvis
The bony pelvis is shown in the above CT scan reconstruction. While the iliac crests and ischia and pubic symphisis are well shown, the sacral component is hidden by parts of the gastrointestinal tract.
71198b01 pelvis bone iliac crest pubic symphisis hip ischial tuberosity pubic bone normal anatomy CTscan 3D Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The bony pelvis is shown in the above CT scan reconstruction. While the iliac crests and ischia and pubic symphisis are well shown, the sacral component is hidden by parts of the gastrointestinal tract.
71198b01 pelvis bone iliac crest pubic symphisis hip ischial tuberosity pubic bone normal anatomy CTscan 3D Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The bony pelvis is shown in the above CT scan reconstruction. While the iliac crests and ischia and pubic symphisis are well shown, the sacral component is hidden by parts of the gastrointestinal tract.
71198b01 pelvis bone iliac crest pubic symphisis hip ischial tuberosity pubic bone normal anatomy CTscan 3D Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The Normal Pelvis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The Normal Pelvis
)
 Acute Debilitating Pelvic Pain – Artistic Rendition
Acute Debilitating Pelvic Pain – Artistic Rendition
 The Normal Fallopian Tubes
The Normal Fallopian Tubes