The Common Vein Copyright 2008
Ilan Yavitz MD
Ashley Davidoff MD
Definition
Headache is defined as pain in the head that is located above the eyes or the ears, behind the head (occipital), or in the back of the upper neck. There are many causes for headache but among the most common causes are migraine and tension headaches. The vast majority of headaches are benign and self-limiting and result spontaneous resolution. Treatment is symptomatic aided with the use of appropriate analgesics. The most feared headache is the life threatening event of a ruptured Berry aneurysm.
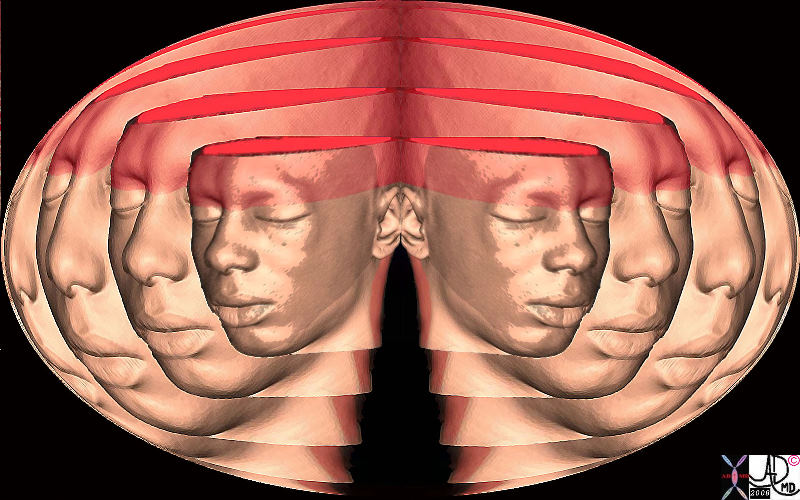
 Headache – Above the Eyes Above the Ears and Behind the neck Headache – Above the Eyes Above the Ears and Behind the neck |
| 74771c06.8 head and neck pain headache abve the eyes above the ears CTscan volume rendering 3D Courtesy Ashley Davidoff MD |
It is estimated that three out of four Americans had a headache at least once during the past year, and approximately forty-five million Americans suffer from chronic headaches, accounting for 80 million doctors’ office visits and more than 400 million dollars spent on over-the-counter pain relievers each year.
Principles
The brain in itself is not sensitive to pain because it lacks pain-sensitive nerve fibers, but several areas of the head can hurt, including the muscles of the neck and head, the meninges and the blood vessels, which do have pain perception, as well as several nerves which extend over the scalp. Inflammation,traction, compression, malignant infiltration, and other disturbances ofpain-sensitive structures lead to headache (1).
Electroencephalography (EEG) is not usually part of the work up for headache, except in the patients with a history of seizures, syncope, or episodes of altered awareness.
Applied Anatomy Only certain cranial structuresare sensitive to pain but there are well over 100 causes of pain and thisrelates to the number of anatomical sites that be the source of pain..
The structures that may be be the source of headache are divided into two sites;extracranial sources and intracranial sources.
Extracranial Sources ofHeadache
- scalp
- muscles
- skull
- arteries – both carotid and vertebral arteries andtheir branches
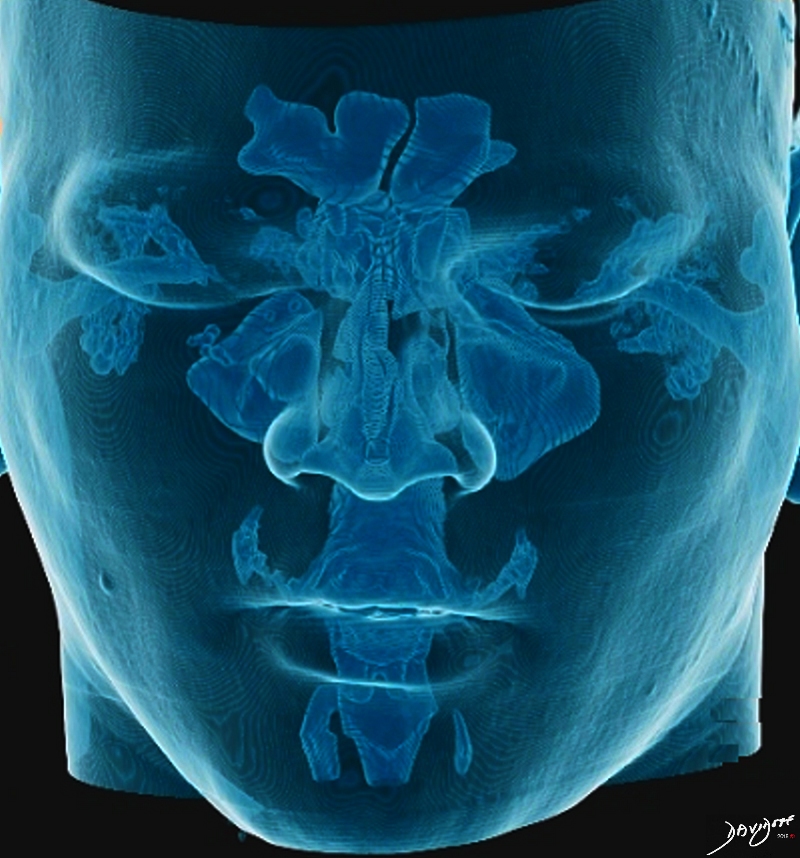
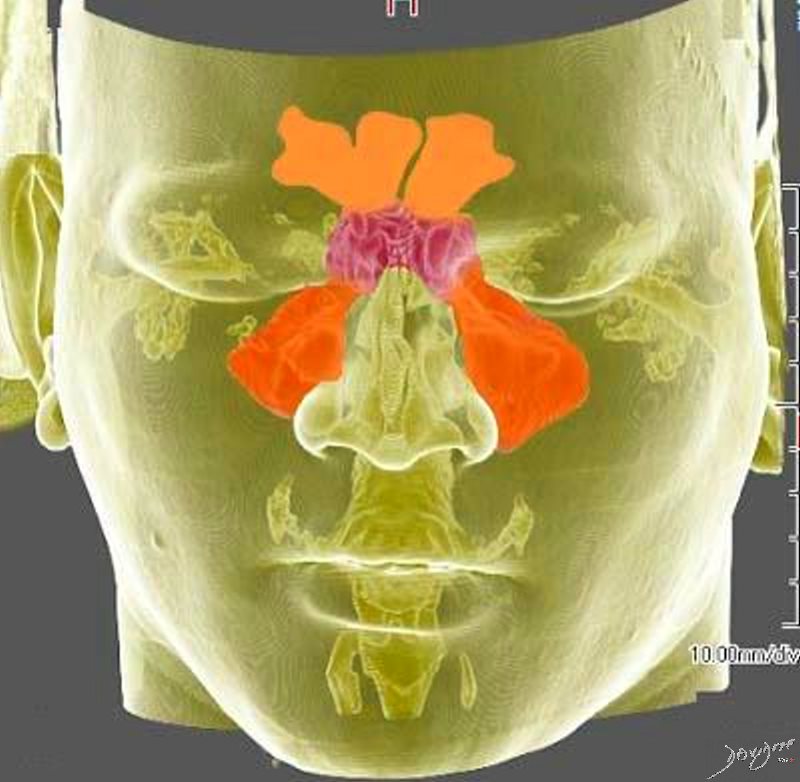
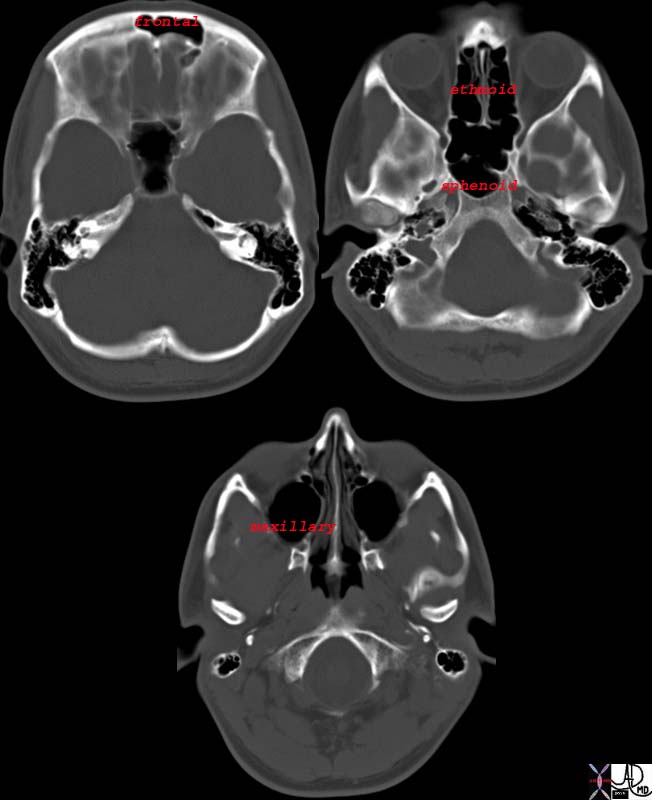
- paranasal sinuses
- orbits and eyes
- mouth teeth andpharynx
- ears
- cervical spine and ligaments
- cervical muscles
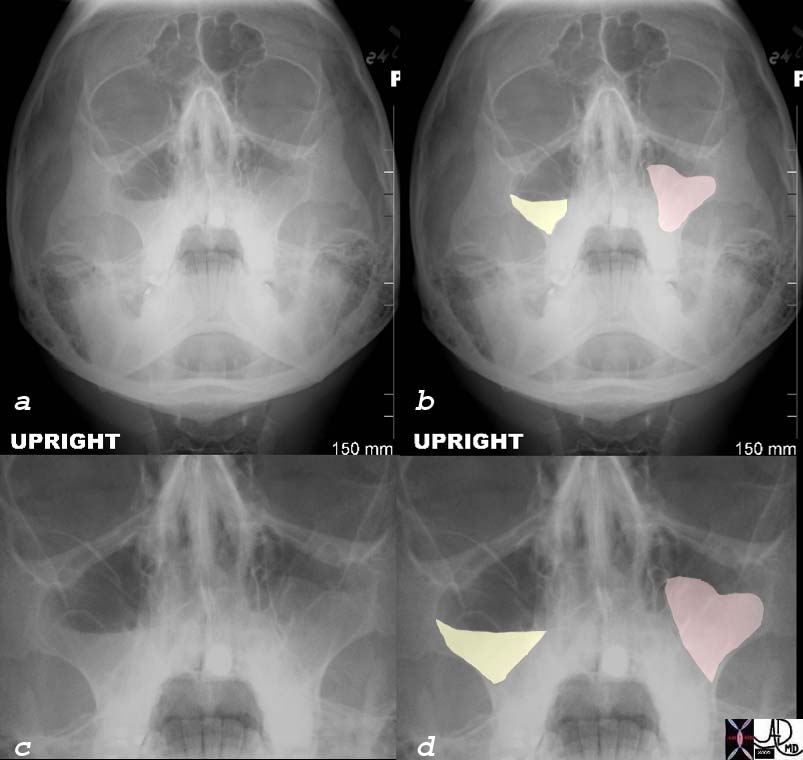
Paranasal Sinuses
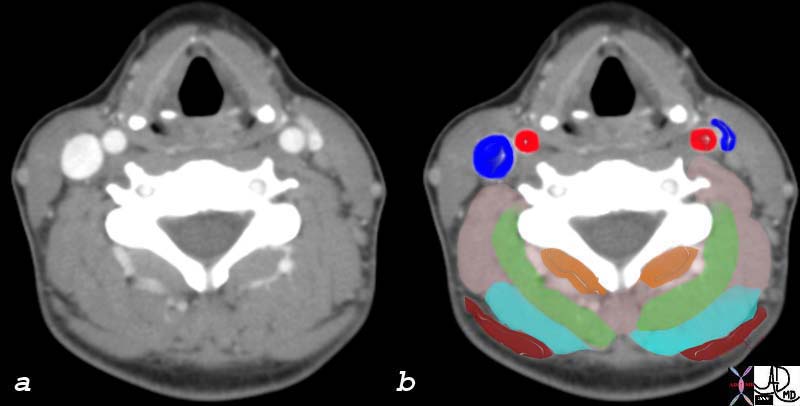
The intracranial structures that may besensitive to pain include;
periosteum cranial nerves meninges meningeal arteries and dural sinuses proximal intracranial arteries sphenoid sinus thalamic nuclei brainstem pain-modulating centers

Severalvascular structures are also sensitive to pain, like intracranial venoussinuses and their large tributaries, the middle meningeal and superficialtemporal arteries. Parts of the dura at the base of the brain, and the arterieswithin the dura and pia-arachnoid, may also be a source of pain 6. Painsensation from the abovementioned structures is transmitted by the fifth(trigeminal) cranial nerve to trigeminal nuclei in the brainstem, which arelargely responsible for processing pain from the face and head 7. Othernerves that can also carry painful stimuli are the facial nerve, whichtransmits impulses from the naso-orbital region, and the ninth and tenthcranial nerves and the first three cervical nerves, which innervate theinferior surface of the tentorium and all of the posterior fossa. Ingeneral, pain from supratentorial structures is referred to the anteriortwo-thirds of the head (trigeminal nerve), and pain from infratentorialstructures is referred to the back of the head and neck (upper cervicalnerves) 6. The seventh, ninth, and tenth cranial nerves referpain to the ear and naso-orbital region. AppliedPhysiology and Pathophysiology Several theories have been developed to tryto explain the mechanisms involved in the genesis of each type of headache, butthere is no general consensus and, despite being such a common condition, itspathophysiology remains poorly understood.It used to be thought that clusterheadaches and migraines were the result of an abnormal vascular reactivity,with aura of migraine being produced by vasoconstriction, and the headachebeing a consequence of vasodilatation. It was also believed thattension-type headaches were a consequence of increased muscle contraction inthe neck and head producing vasoconstriction and ischemia. Both of thesetheories have now been considered insufficient to explain all the complexitiesinvolved in the genesis of the headaches.Migraine is currently thought to havea multifactorial etiology. There is indeed a certain instability in theregulation of the vascular tone which may lead to vasodilatation, and thisdilatation could play a role in the throbbing head pain of the migraine, butthere are also several other processes involved in the pathophysiology ofmigraines. There is an imbalance between excitation and inhibitionof the neurons at various levels of the nervous system, each with its ownconsequences. At the trigeminovascular level, there seems to be an excessiverelease of substance P (substance known to cause pain) and other inflammatorymediators. Another important phenomenon involved is the cortical spreadingdepression (CSD), a self propagating wave of neuronal activation that seems tobe responsible for causing the aura of migraine, and which also results infurther activation of the trigeminal system, producing the release of moreinflammatory mediators 3. Other mechanisms involved are beyondthe scope of this work.In the case of cluster headaches, vasodilatation appearsto be secondary to neuronal dysfunction and it may be responsible for the painand autonomic features of cluster headaches. In this case, as in migraines,disregulation of the trigeminovascular system is likely involved in causingthis vasodilatation. The autonomic symptoms of cluster headaches, such aslacrimation and pupillary constriction, appear to be due to an abnormalactivation of parasympathetic and sympathetic fibers in the central nervoussystem. The periodicity of cluster headaches might be related tochanges in the hypothalamus region of the brain, where the ?biologic clock? islocated. In the case of tension-type headaches (TTH) current theories alsoattribute the pain, at least in part, to abnormal vascular reactions and anincreased sensitivity to painful vasodilatation compared to people that doesn’tsuffer from headaches. In this sense, TTH would be on the milder end of a”headache continuum” that has migraines on the more severe end 3. Causesand predisposing factors There are two types of headaches: primaryheadaches and secondary headaches. Primary headaches arenot associated with (caused by) other diseases, while secondary headaches arecaused by some associated disease, ranging from minor conditions to serious andlife threatening ones.Many controversies exist in the literature regarding thenomenclature and classification of headache. The International Headache Society(IHS) developed and published a classification and diagnostic criteria whichlists over 150 different types and sub-types of headaches(2). Wewill simplify the classification and focus on the most common types.PRIMARYHEADACHES The vast majority of all primary headaches fall underthree categories: migraine, tension-type, and cluster headache. Migraine headaches Migraine headaches are the second most commontype of primary headache, affecting 12-16% of the population (Rasmussen, 1995),and causing 150 million lost workdays and 329,000 lost school days each year inthe United States (Stang, 1993).It is more prevalent in women than in men, andit can be divided in two major sub-types: with or without aura.Migrainewithout aura is the commonest subtype of migraine, it has a higher averageattack frequency, and is usually more disabling than migraine with aura. Itmanifests in recurrent headache attacks lasting 4-72 hours. The headache isusually localized to one side of the head (it is commonly bilateral in youngchildren), has a pulsating quality, moderate or severe intensity, andphotophobia and phonophobia are common accompanying symptoms. The headache isoften worsened by routine physical activity, sneezing, rapid head motion, orstraining.Migraine with aura is characterized by attacks of reversiblefocal neurological symptoms (aura) preceding the onset of a headache with thesame features of Migraine without aura.The aura typically developsgradually over 5-20 min and lasts for less than one hour. It usually occursbefore the onset of migraine headache, but it can also occur during or evenafter the headache. Auras may involve visual disturbances, sensory symptoms,speech disturbances and motor weakness.Visual disturbances are the most commontype of aura, accounting for the majority of the neurologic symptoms associatedwith migraine. The most characteristic visual aura of migraine is a ?scintillatingscotoma? (a scotoma is an area of loss of vision), beginning as a hazy spotfrom the center of a visual hemifield followed by shimmering light of differentpatterns expanding peripherally to involve a greater part of the hemifield withscotoma.Numbness and tingling of the lips, lower face, and fingers of one handis the second most common type of aura. Some patients have several types ofaura symptoms that vary with attacks.Both subtypes of migraine headaches (withor without aura) may be preceded by premonitory symptoms that occur hours totwo days before a migraine attack. They include various combinations offatigue, difficulty in concentrating, neck stiffness, sensitivity to light orsound, nausea, blurred vision, yawning and pallor. Tension-type headaches(TTE) TTH is the most common type of primary headache; as many as 80% ofadults have had or will have tension headaches, and it is also more prevalentamong women.It is further subdivided according to its frequency in Infrequentepisodic TTH (occurring once a month or less), Frequent episodic TTH (occurringon more than one but less than fifteen days per month), and Chronic TTH (dailyor very frequent episodes, an average of 15 or more days per month).This kindof headache may feel like pressure or tightness all around the head, mild tomoderate in intensity, has a tendency to wax and wane, and it often radiates tothe neck muscles at the base of the skull. The pain is bilateral,non-pulsating, usually not aggravated by routine physical activity, and isdevoid of typical migrainous features (eg, nausea, vomiting, phonophobia,photophobia, and aura). Some individuals may have overlappingfeatures of both migraine and tension type headache. Those individuals are hardto satisfactorily label with a single diagnosis, but generally should betreated as tension type headache sufferers. The clinical features that appearto be most predictive of migraine compared with tension type headache includenausea, photophobia, phonophobia, and exacerbation by physicalactivity. Cluster headache Cluster headache is relativelyuncommon, affecting less than 1 percent of the population. In contrast withmigraines and TTH, an estimated 85% of cluster headache sufferers aremen. Age of onset is usually 20-40 years, although headaches maybegin in childhood.It is characterized by attacks of severe, strictlyunilateral pain, beginning quickly without warning and reaching maximalintensity within a few minutes. The pain is usually deep, excruciating,continuous, and explosive in quality, usually beginning in or around the eye ortemple.Attacks typically last from 15 minutes to 3 hours, occur from once everyother day to 8 times a day, and are associated with one or more of thefollowing, all of which are ipsilateral: lacrimation and redness of theeye, nasal congestion, rhinorrhea, sweating, pallor, and Horner’s syndrome(eyelid drop and constricted pupil).Attacks usually occur in series (clusterperiods) lasting for weeks or months separated by remission periods usuallylasting months or years. This type of presentation, called episodic, is themost common one, but 10-15% of patients have chronic cluster headache, withattacks occurring for more than 1 year without remission or with remissionslasting less than one month.Over 50 percent of sufferers report that alcohol isa potent precipitant of cluster headaches during a cluster bout; thissensitivity to alcohol ceases when the cluster ends (histamine andnitroglycerine are other well-known triggers). Nitroglycerin, histamine,some foods and smoking can also be precipitants of cluster headaches.Mostpatients with cluster headache are restless and may pace when an attack is inprogress, in contrast to migraine sufferers, who tend to rest in a dark, quietroom. Secondary Headaches Secondary headaches have diversecauses, ranging from serious and life threatening conditions such as braintumors, strokes, meningitis, and subarachnoid hemorrhages to less serious butcommon conditions such as withdrawal from caffeine and discontinuation ofanalgesics.In contrast with the primary headaches, for most secondary headachesthe characteristics of the headache itself are poorly described in thescientific literature. Even for those where it is well described, there areusually few diagnostically important features. Therefore, the correct diagnosisof secondary headaches depends on identifying the presence of a disorder knownto cause headache, and a close temporal relation between the occurrence of theheadache and that other disorder (or other evidence of a causal relationship).Secondary headaches are greatly reduced or resolve within 3 months (or less)after resolution of the causative disorder.There are many different types of secondary headaches; we will focus on the most common ones.Post-traumatic headache Post-traumatic headache can follow direct impact to the head, or sudden acceleration and/or deceleration (whiplash injury). It can occur indifferent patterns, and may closely resemble primary headache disorders, most frequently tension-type headache (1).It can be further subdivided in acute and chronic. They both occur within 7 days after the head trauma, but the chronic persists for more than 3 months after the initial event and it?s often part of the ?post-traumatic syndrome? which includes a variety of symptoms such as equilibrium disturbance,poor concentration, decreased work ability, irritability, depressive mood, and sleep disturbances. Post-traumatic headache can also vary in intensity, and in the most severe cases can be accompanied by loss of consciousness, mental status changes, and/or post-traumatic amnesia. When neuroimaging techniques (e.g., CT of the head) aredone after trauma, several structural abnormalities may be identified, likecerebral hematoma, subarachnoid hemorrhage, subdural hematoma, diffuse axonallesion, skull and fractures for example.
Medication overuse headache(MOH)
Prevalence is about 1 percent of the population, higher in women than in men, and it may occur in patients with tension-type headache, migraine,or cluster headache. It is the consequence of an interaction between a therapeutic agent used excessively (regular overuse for more than 3 months) and a susceptible patient. The best example is overuse of symptomatic headache drugs causing headache in the headache-prone patient. The most common cause of chronic migraine-like headache is overuse of symptomatic migraine drugs and/or analgesics. Chronic tension-type headache is less often associated with medication overuse, but it can also become chronic headache through overuse of analgesics. This type of headache usually resolves or reverts to its previous pattern within 2 months after discontinuation of overused medication
Sinus headache
Frontal headache accompanied by pain in one or more regions of the face, developing simultaneously with an episode of acute rhinosinusitis (which may include purulence in the nasal cavity, nasal obstruction, hyposmia/anosmia and/or fever). Headache and/or facial pain resolve within 7 days after remission or successful treatment of the sinusitis.Although sinus headache is commonly diagnosed by physicians and self-diagnosed by patients, many patients presenting with ?sinus headache? turn out to have migraine without aura, with headache either accompanied by prominent autonomic symptoms in the nose (rhinorrhea, nasal congestion) or triggered by nasal changes (but they don?t have purulent nasal discharge or any of the other features characteristic of acute rhinosinusitis).
TemperomandibularDysfunction
Temporomandibular joint dysfunction syndrome (TMJ) ischaracterized by musculoskeletal pain with dysfunction of the masticatorysystem. Many patients with TMJ complain of headache, and in some cases headacheis its only manifestation, without the patient being aware of a TMJ.Theheadache associated with TMJ is usually localized to one ear or preauriculararea, and it can radiate to the jaw, temple, or neck. The pain is deep, dull,continuous, and usually worse in the morning. It typically is associated with alimitation of jaw motion and deviation of the jaw upon opening. Physicalexamination may reveal tenderness of the muscles of mastication and, lesscommonly, clicking of the joint.
Giant Cell Arteritis
Giant cellarteritis (GCA), also known as temporal arteritis, is a chronic vasculitis ofunknown etiology that commonly presents with a headache. In the US the reported incidence of GCA is approximately 15-20 cases per 100,000 people aged 50 yearsor older, and women are 2-4 times more likely to have GCA than men. Age is the most important risk factor for GCA, as the disease occurs mostly in patients older than 50 years, with incidence increasing with age and peaking in the eighth decade. Headache was the most common symptom, experienced by 72% ofpatients at some time, and was the initial symptom in 33% 5.The head pain tends to be located over the temporal areas but can be frontal oroccipital in location, and the severity can range from mild to severe. Manypatients report scalp tenderness on combing their hair, and tender temporal oroccipital arteries are found in approximately one-third ofpatients. Visual symptoms, including blurriness, double vision or loss ofvision (partial or complete), are present in about a third of the patients, andin as much as half of them the symptoms can become permanent. The onset ofblindness from involvement of the ophthalmic artery is one of the most seriouscomplications of GCA and it may occur without warning; about 50% are unilateraland 50% are bilateral. Newly recognized GCA should be considered a trueneuro-ophthalmic emergency, as prompt treatment with steroids can prevent blindness 4. The definitive diagnosis is usually obtainedthrough a biopsy of the superficial temporal artery, but therapy should not bewithheld pending the performance or results of the biopsy in patients withacute visual loss and high clinical suspicion for GCA.
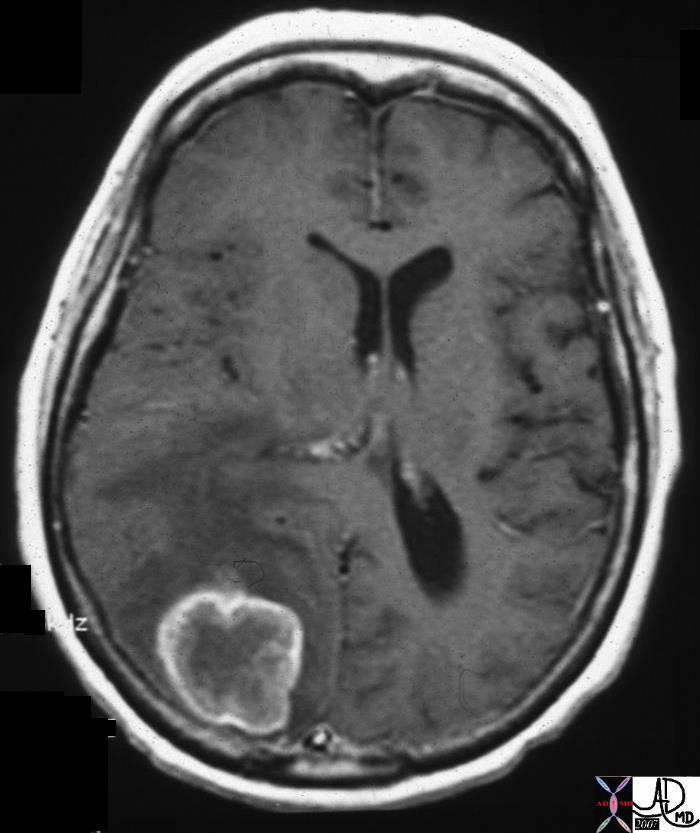
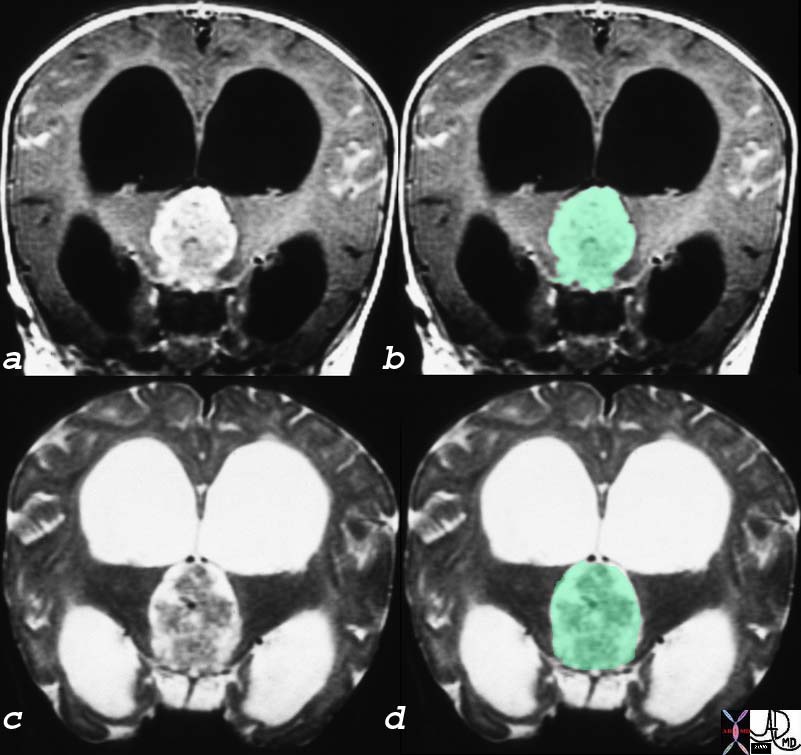
Brain Tumors
Approximately 50percent of patients with brain tumors, either primary or metastatic, willsuffer from headaches, and in many of them headache is the worst symptom theyhave. The headaches are most frequently similar to tension type, and it?s usuallybifrontal but worse on the same side of the tumor. Tumors can produceheadache by two different mechanisms: by compromising or exerting directpressure on a pain-sensitive structure (e.g. the trigeminal nerve), or byobstructing the CSF circulation causing elevated intracranialpressure. When the CSF circulation becomes impaired, headache oftenbecomes generalized and worse in the occipitonuchal area. It?s typicallydescribed as being worse in the morning (on awakening), aggravated by coughingand straining, and often associated with nausea and vomiting 5.Braintumors can also present with focal neurological signs (visual, motor, sensory),altered mental status or seizures.
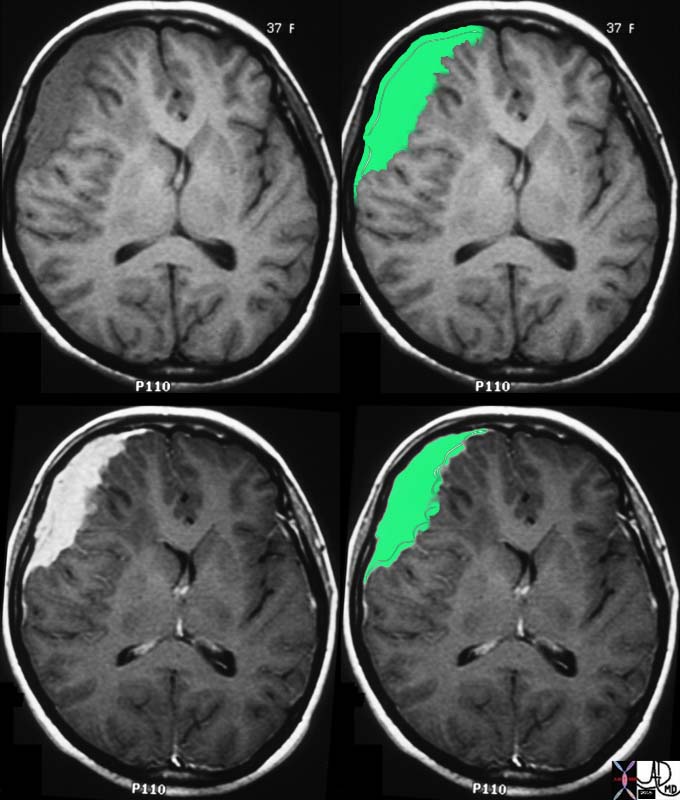
Elevated IntracranialPressure
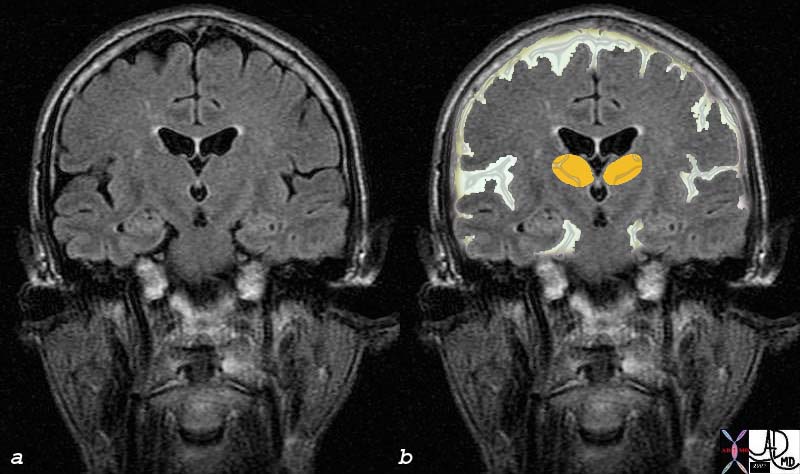
Elevated intracranial pressure (ICP) can occur in different settings including the presence of a brain tumor (as we mentioned above),trauma, impaired CSF circulation, impaired venous outflow from the brain, and hepatic encephalopathy. Elevated ICP headache is characteristically worsened by straining or coughing, and is usually accompanied by vomiting. Physical exam may reveal depressed global consciousness, focal neurological signs,papilledema, and in severe cases, a triad of bradycardia, respiratorydepression, and hypertension known as Cushing’s triad (ominous sign).Idiopathicintracranial hypertension (i.e., pseudotumor cerebri) is a rare condition thatcan occur in young, overweight women, or sometimes in patients taking certainmedications like lithium, oral contraceptives, or large doses of vitamin A. Itis an elevation of the intracranial pressure of unknown mechanism, usuallypresenting with a pulsatile headache, pulsatile tinnitus, associated withnausea or vomiting, and sometimes retroocular pain worsened by eye movement.Papilledema is usually found on funduscopic examination, and the patients mayhave visual blurring which may become permanent if prompt therapy is notinstituted.Another rare cause of elevated ICP is cerebral venous thrombosis(CVT). The thrombosis can be localized to cerebral veins, interfering with thevenous outflow of the brain, or to the dural sinuses, resulting in decreasedCSF absorption. Headache is the most frequent presentation of CVT, and it?susually of gradual onset, but can also be of explosive characteristics (knownas thunderclap headache), similar to the SAH pain.
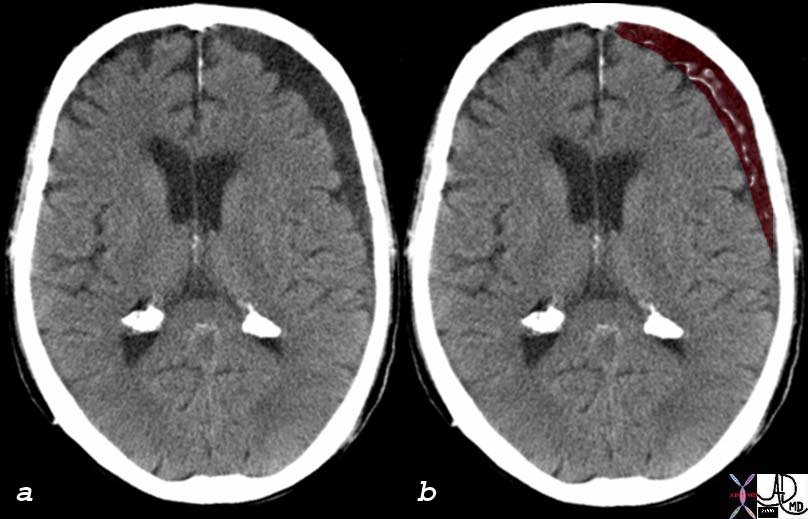
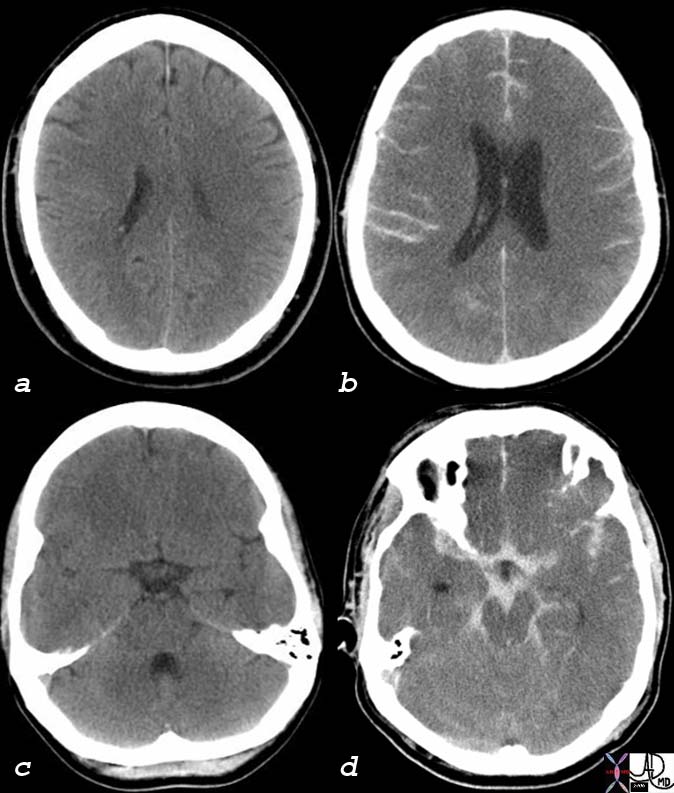
SubarachnoidHemorrhage
Subarachnoid hemorrhage (SAH) is most commonly caused by aruptured intracranial aneurysm, which produces a severe headache of suddenonset that patients often characterize as “the worst headache of theirlife.” Stiff neck is frequently found on physical examination, and adecreased level of consciousness may also be noticed. Up to 60% of the patientsmay experience a “sentinel headache” hours to days prior to theSAH. The sentinel headache typically presents as a severe headachelasting for only a few minutes without associated neurologic abnormalities, andit is caused by a minor leak from the aneurysm prior to itsrupture.
Meningitis
Meningitis is an inflammation of theleptomeninges and underlying subarachnoid cerebrospinal fluid (CSF), and itsincidence is 2-3 cases per 100,000 people. Meningitis and meningoencephalitisboth have headache as a major symptom. Pain is often severe, retro-orbital andworsened by moving the eyes. Headache is a key symptom of meningealsyndrome or meningism consisting usually of headache, neck stiffness andphotophobia. Other classic symptoms and signs of meningitis are fever andchills, vomiting, seizures (30-40% in children, 20-30% in adults), focalneurologic symptoms, and altered sensorium (confusion may be sole presentingcomplaint, especially in elderly). Meningitis has a high morbidity andmortality, and it?s crucial to recognize meningitis on initial presentation andto begin antibiotic treatment as soon as possible (within the first 30 minutesin the ED), for any delay in instituting treatment may lead to permanentneurological sequelae or death.

Headache Associated with Refractive Errors
Eyestrain: Patients frequently attribute headaches to eye strain, and the IHSrecognizes headaches associated with refractive errors (HARE). Headaches areonly rarely due to refractive error alone, but correcting vision may improveheadache symptoms in some of these patients. HARE presents as a recurrentmild headache, frontal and in the eyes themselves, which develops in closetemporal relation to the refractive error, is absent on awakening andaggravated by prolonged visual tasks at the distance or angle where vision isimpaired. Headache and eye pain resolve within 7 days, and do not recur,after full correction of the refractive error 2.
Arterial Hypertension
There is a common belief, particularly among patients, that hypertension can cause headaches. While this is true in the case of hypertensive emergencies, it is probably not true for typical migraine or tension headaches. Mild (140-159/90-99 mm Hg) or moderate (160-179/100-109 mmHg) chronic arterial hypertension does not appear to cause headache. Whether moderate hypertension predisposes to headache at all remains controversial, butthere is little evidence that it does. Ambulatory blood pressure monitoring inpatients with mild and moderate hypertension has shown no convincing relationshipbetween blood pressure fluctuations over a 24-hour period and presence orabsence of headache 2.
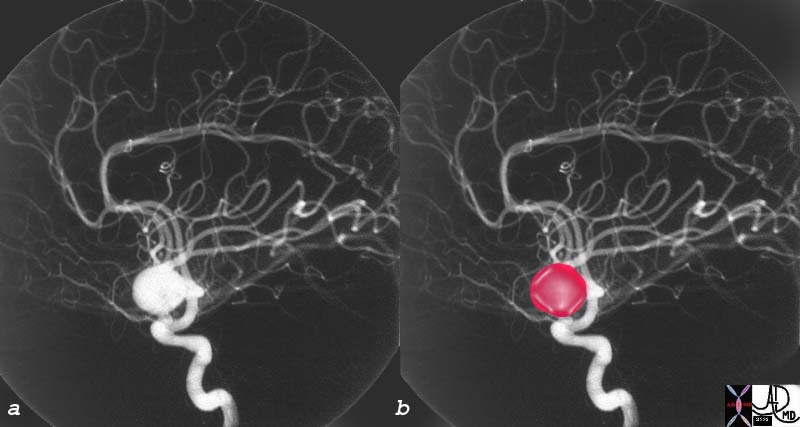
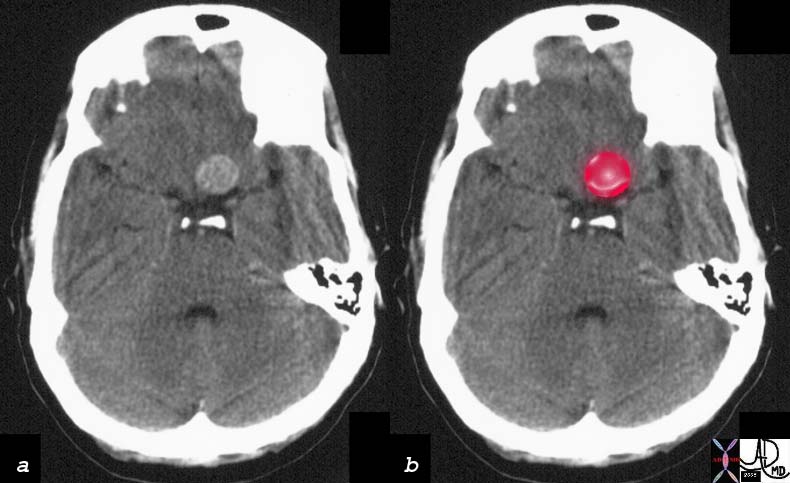
Subarachnoid Hemorrhage
Ruptured Berry Aneurysm
The “worst headache of my life” sends shivers down the caregivers back, since if the headache is truly caused by a subarachnoid bleed then the patient has a 50-50 chance of-coming out alive or without significant deficit. The aneurysm is characterized by focal dilatation or sacculation of one or more of the intracranial arteries of the brain.
The cause is multifactorial including congenital weakness of the wall, and acquired factors such as hypertension and turbulence at the branch points.The focal outpouching has a predisposition to rupture.
Structurally berry aneurysms are more common in the anterior circulation, are multicentric in 20-30% of patients, and commonly occur at branch points.
Functionally only the giant aneurysms(greater than 2.5cms) will affect function by compressing on other structures. The risk of rupture is the most feared complication of berry aneurysms, and it is the most common cause of spontaneous subarachnoidbleeding. The aneurysm may also rupture into the brain substance, intothe ventricles, or into the subdural space. About 60% of patients willhave a catastropic outcome either succumbing or having a permanent significantdeficit and the reamining 40% will have a relatively favorableoutcome.
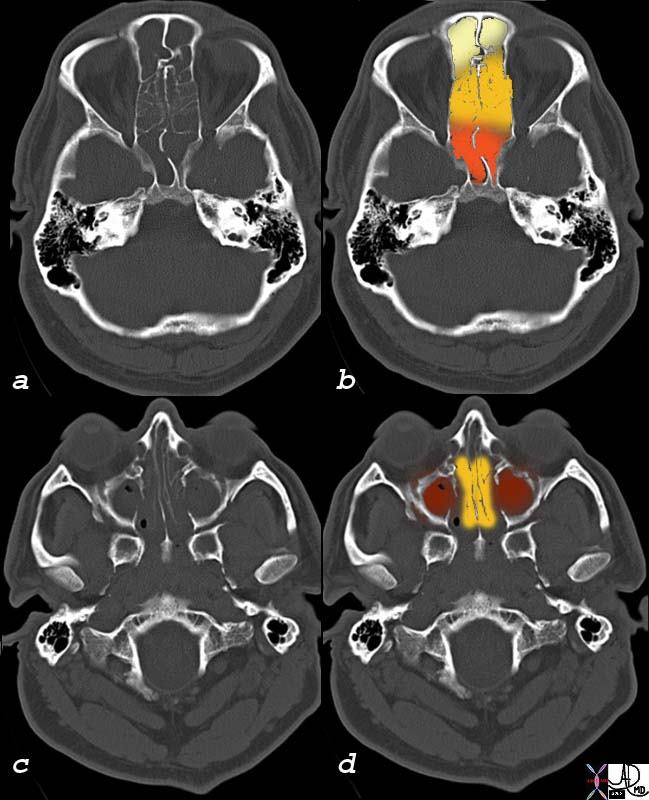
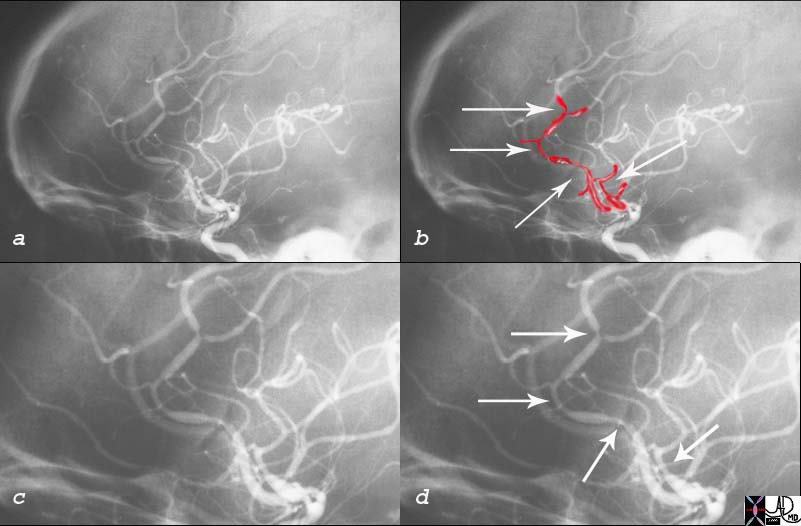
Clinically the smaller aneurysm are asymptomatic. When theyrupture the presentation is dramatic with the acute onset of a headache whichclassically is described as the most severe headache ever experienced by thepatient.The diagnosis is documeneted by finding acute bleeed mostcommonly in the subarachnoid space, characterized by hyperdense blood in thesulci on a non contrast CT. The bleed may occur or extend into thecerebral substance, or into the ventricles or subdural space. An angiogram is required to accurately localize the aneurysm and plan therapy.Treatment optionsinclude transcatheter embolization or surgical clipping at the base of theaneurysm.

Clinical presentation of headaches -General
A careful history and physical examination remain the mostimportant part of the assessment of the headache patient. A thorough history isthe single most important factor in establishing a headache diagnosis anddetermining the future work-up and treatment plan.
History
Precipitating factors
Migraines may be precipitated by bright light, menstruation, weather changes, caffeine withdrawal, sleeping longer or less than usual, and ingested substances such as alcohol or certain foods. If bending, lifting, coughing, or Valsalva?s maneuver produces a headache, an intracranial lesion must be considered; however, mostexertional and cough headaches are benign. Alcohol is often a potentprecipitant of cluster headaches.
Duration
Migraine painusually lasts 6 to 36 hrs, whereas cluster headache characteristically lasts45-120 min. Tension-type headaches commonly build up over hours and may lastdays to years.
Onset
Cluster headaches often awaken pts from a soundsleep and have a tendency to occur at the same time each day in a given person.Migraines can occur at any time during the day or night but usually begins inthe morning. A headache of recent onset that disturbs sleep or is worse onwaking may be caused by increased intracranial pressure. TTH are typicallypresent during much of the day and are often more severe late in theday. Headache of instantaneous onset suggest an intracranial hemorrhage,usually in the subarachnoid space.
Character
Migraine often has apulsating quality. Cluster headache is characteristically severe, boring,steady, and it has a certain frequency and periodicity of occurrence whichhelps to identify it. TTH are usually described as a feeling of fullness, tightness,or pressure, or as being like a cap, band, orvice.
Situation
Migraine is most often unilateral, commonly in thefrontotemporal region, but it may be generalized. Cluster headaches arevirtually always unilateral during an attack and are typically centered in,behind, or about the eye. A typical TTH is generalized, although itmay originate across the nuchal muscles only to spread and perhaps predominatein the frontal or occipital regions.
Severity
Migraine pain usuallypeaks within 1-2 hrs of onset and is of moderate to severeintensity. Cluster headache is typically maximal immediately if thepatient awakens with the headache in progress or peaks within a few min if itbegins during wakefulness, but in either situation it is usually very severe,excruciating.A new sudden, severe headache that is maximal at onset suggestsintracranial hemorrhage, cerebral venous sinus thrombosis, or pituitaryapoplexy.
Aggravating factors
For migraine headaches the most common aggravating factors are straining, bending over, bright lights, and certain smells. One of the classical criteria for the distintion between migraines and TTH is that physical activity, light, and noise, are frequent aggravating factors for migraines but not for TTH, but some recent studies have shown that those factors can also aggravate the a tension-type headache in as many as 50% of the cases. For clusters, though there are specific triggers, in the form of vasodilators, that cause cluster headaches, the aggravating factors are highly individualized. In patients with increased intracranial pressure (e.g. brain tumors) headache may worsen with bending over, and worsening headache may also follow maneuvers that raise intrathoracic pressure, such as coughing, sneezing, or the Valsalva maneuver. Relieving factors Rest, especially sleep and avoidance of light and noise tends to provide relief to the migraine sufferer. Massage or heat may alleviate the pain associated with a TTH. Local application of pressure over the affected eye or ipsilateral temporal artery, and local application of heat or cold, may ameliorate the pain of cluster headache 5. Associated symptoms Migraines, as we described above, can be associated with several neurological symptoms (aura). Also, physiologic data suggest that muscle tension may be at least as likely to occur in migraine as it is in tension-type headache. More specifically, neck pain recently has been demonstrated to be quite common not only in TTH but also in migraine, and that?s why the presence of neck pain should not automatically trigger a diagnosis of tension-type headache. SAH can also have neck and back pain, but its explosive characteristics helps distinguishing it from other causes. It frequently presents with vomiting and altered mental status (including deep coma). Cluster headache is commonly associated with some ipsilateral signs, like lacrimation and redness of the eye, nasal congestion, sweating, pallor, and Horner’s syndrome. Nausea or vomiting is commonly present in patients with brain tumors. Other associated signs can be focal neurological findings, visual changes, and seizures. Meningitis is usually associated with nausea, photophobia and/or phonophobia, neck stiffness, and change in mental status. Physical Examination In the patient with headache, the physical exam is often unrevealing. However, some findings, if present, can yield important clues about the underlying cause. The examination should begin by taking the vital signs, and then assessing the general status of the patient, determining whether the patient looks ill, toxic, anxious or depressed, and if the patient is oriented or confused. It is extremely important to perform a neurological examination, including examination of the mental status, gait, cranial nerves, motor system, and sensory system. A funduscopic exam should also be done to look for signs of papilledema. The skull and cervical spine should also be examined. The skull should be palpated for lumps and local tenderness. Thickened, tender, irregular temporal arteries with an associated reduction in pulse suggest GCA. In TTH the scalp muscles may be tender. In a patient that presents with altered mental status, the exam has to include looking for any signs of head trauma. Nuchal rigidity on passive neck flexion and Kernig?s sign (flexing the patient?s hip 90 degrees and then extending the patient?s knee causes pain) are evidence of meningeal irritation. Labs When, based on the history and physical examination, the patient is clearly suffering from a primary headache, there is usually no need for any specific workup. If routine blood tests are performed in patients with primary headaches the results should be unremarkable. Specific tests should be obtained if there is a clinical suspicion of underlying conditions (secondary headaches). In these situations, a complete blood count (CBC), electrolytes, glucose, BUN and creatinine, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) can be checked. The CBC can be abnormal in inflammatory conditions (like GCA) and in infections (like meningitis). The ESR and CRP are usually elevated in cases of GCA. A blood gas analysis with a cooximeter can detect toxic levels of carbon monoxide (cause of headache during winter time mainly). Cerebrospinal fluid (CSF) examination obtained through a spinal tap (also known as lumbar puncture) is vital for the diagnosis of meningitis, and can also aid in the diagnostic evaluation of encephalitis, SAH, and certain types of malignancies that can affect the CSF. If the patient has altered mental status, or papilledema in the funduscopic exam, or any focal neurological signs, a CT of the head should be obtained prior to performing a spinal tap to exclude the presence of intracranial hypertension, for a spinal tap performed in that setting could lead to severe damage or death. A spinal tap also allows for the measurement of the CSF pressure, which is important given the fact that either elevated or decreased pressures can produce headache. Ironically, the lumbar puncture itself can produce a headache secondary to decreased CSF pressure after the procedure, which usually resolves after a few hours or days with bed rest and good hydration, but can also, in rare occasions, persist for several weeks or even months 5. Electroencephalography (EEG) is not usually part of the work up for headache, except in the patients with a history of seizures, syncope, or episodes of altered awareness. Imaging Neuroimaging studies are not to be ordered indiscriminately in every headache patient, but they can prove to be extremely useful in certain clinical situations. Any recent significant change in the pattern, frequency or severity of headaches (especially if the headache is getting worse despite appropriate therapy), or the presence of focal neurological signs or symptoms, should include neuroimaging as part of the workup. Patients with an orbital bruit, otorrhagia, or leaking of clear fluid through the nose after head trauma, as well as patients that have onset of headache with exertion, cough, or sexual activity, or onset of headache after age 40 years, also need to undergo head imaging. Tumors, hematomas, cerebral infarctions, abscesses, and many other processes can be identified with computed tomographic (CT) scanning and magnetic resonance imaging (MRI) 5. The pituitary gland, the craniocervical junction, the cervical spinal cord and exiting nerve roots, and the white matter of the brain are better evaluated by MRI. CT can be helpful for evaluating abnormalities of the skull, orbit, sinuses, facial bones, cervical spine, and recent subarachnoid hemorrhage. A non-contrast CT of the head should be the first study done in a patient in which an intracranial bleed is suspected. As a general rule, CT is the optimal imaging study for evaluating a patient with acute onset of headache. MRI might provide a better evaluation in cases of subacute and chronic headache, or when posterior fossa or vascular lesions are suspected, but even in those cases CT is usually the first imaging study obtained. Potential Complications Some secondary headaches can lead to severe complications if the underlying condition is not controlled with therapy. Post-traumatic headache might be caused by different underlying conditions, and some of them, like a hematoma (cerebral, subdural, or extradural) or diffuse axonal injury, can lead to permanent neurological damage or death. Any cause of increased intracranial pressure can also lead to great neurological damage or death if it causes compression or displacement of different parts of the nervous system. Giant cell arteritis, as well as pseudotumor cerebri, can produce permanent visual loss if not treated. Hypertensive emergencies can lead to a stroke or to cardiovascular damage if not treated, and meningitis can cause permanent neurological sequelae, or death, if not promptly treated. Management Therapy for migraines can be divided in two main groups: prophylaxis and treatment of the acute attacks. Prophylactic agents are indicated in patients with frequent migraines that significantly interfere with their daily routine despite acute treatment. Several agents can, in various degrees, reduce the frequency and intensity of migraine attacks. Several antihypertensive agents (e.g.: metoprolol, verapamil, enalapril), some antidepressants (e.g.: amitriptyline, mirtazapine), anticonvulsants like valproate, gabapentin, and topiramate, as well as some non-steroidal anti-inflammatory drugs (NSAIDs) like naproxen, can all be used for prophylaxis. About 50 to 75% of patients given these drugs will have a 50% reduction in the frequency of migraine attacks 3. Alternative techniques like herbal medicine, acupuncture, relaxation techniques, biofeedback, and behavioral therapy, may provide benefit in some patients, and can be combined with the prophylactic agents mentioned before. There are many different agents that can be used for the abortive treatment of acute migraine headaches. All NSAIDs (e.g.: ibuprofen, naproxen, diclofenac, aspirin), as well as acetaminophen, may be beneficial in some patients, but they are probably not enough, if used as sole agents, to abort moderate to severe attacks. A group of drugs often used for acute migraines is the Triptans (e.g.: sumatriptan, zolmitriptan, naratriptan). They are usually very effective, but the multiple drug interactions that may occur with their use, as well as the multiple contraindications for their use (e.g.: ischemic cardiovascular disease, uncontrolled hypertension, pregnancy), preclude its use in some patients. Another group of agents used for abortive therapy is the Ergots (e.g.: ergotamine, dihydroergotamine), and their use is also limited by multiple contraindications (coronary artery disease, peripheral vascular disease, hypertension, and renal or hepatic disease). Some antiemetics, like metoclopramide, are also effective, and they are frequently used in combination with other agents (e.g.: dihydroergotamine). They are especially useful in patients that present with significant nausea and vomiting. For cluster headaches there is also prophylactic and abortive therapy. Inhalation of 100% oxygen by nonrebreathing masks is a very effective abortive therapy for acute clusters, producing relief in approximately 75% of the cases after 20 minutes of therapy. Subcutaneous sumatriptan is also effective in aborting acute clusters, with onset of action and efficacy rates similar to oxygen therapy. Sumatriptan may also be given intranasal, being equally effective but slower to produce a response. Therapy with 100% oxygen has no contraindications (except maybe COPD patients who retain carbon dioxide), whereas sumatriptan is contraindicated in patients with ischemic cardiovascular disease or uncontrolled hypertension because of its vasoconstrictive properties. Besides abortive therapy, prophylactic therapy should also be started as soon as possible at the onset of a cluster episode. Several drugs have been found to reduce attack frequency and analgesic consumption, like verapamil, prednisone, and lithium. Patients that do not respond to medications may benefit from more radical and aggressive therapies, like complete or partial section of the trigeminal nerve, or greater occipital nerve blockade. Deep brain stimulation of the posterior hypothalamic gray matter is an experimental method that has also been effective in some patients with intractable cluster headache 3. For episodic tension-type headaches, simple analgesics such as acetaminophen or ibuprophen are the drugs of choice for abortive therapy. If the patient is suffering from chronic TTH, prophylactic therapy might be indicated to reduce the frequency or severity of the episodes. Tricyclic antidepressants, or other antidepressants like serotonin blockers, are considered to be effective in preventing chronic headaches, and are the most commonly used agents for prophylaxis. Alternative techniques that may provide some additional benefit to chronic TTH sufferers are biofeedback, relaxation therapy, psychotherapy, and physical therapy, either alone or in combination with antidepressant medications 3. Red Flags There are several important factors that can help to differentiate the small number of patients with life-threatening headaches from the overwhelming majority with benign primary headaches. Failure to recognize these alarm signs can have potentially fatal consequences. Sudden onset of headache, or severe persistent headache that reaches maximal intensity within a few seconds or minutes after the onset of pain, could be caused by a subarachnoid hemorrhage, for example, which often presents with sudden onset of excruciating pain. Cluster headache may sometimes be confused with a serious headache, since the pain can reach full intensity within minutes, but its typical features allows for the differentiation. The absence of similar headaches in the past is another finding that suggests a possible serious disorder. The “first” or “worst” headache of my life is a description that sometimes accompanies an intracranial hemorrhage or central nervous system infection. A worsening pattern of headache suggests a mass lesion, subdural hematoma, or medication overuse headache. The presence of nausea, vomiting, increased headache with changes in body position (particularly bending over), and an abnormal neurologic examination suggest the headache was caused by a tumor Any new focal or nonfocal neurologic abnormality warrants further evaluation. The findings may be quite subtle, such as slight pupillary asymmetry, unilateral pronator drift, or extensor plantar response, or pronounced, such as unilateral vision loss, ataxia, or seizure. Focal neurologic findings can accompany a number of secondary causes of headache, including intracranial hemorrhage, acute narrow angle glaucoma, and carotid or vertebral artery dissection. Nonfocal alterations in mental status more commonly characterize other secondary causes of headache, including subarachnoid hemorrhage, meningitis, and toxins such as carbon monoxide. Fever associated with severe headache may be caused by intracranial infection (e.g., meningitis). Change in mental status, personality, or fluctuation in the level of consciousness suggests a potentially serious abnormality. Obtundation and confusion increase the likelihood of meningitis, encephalitis, subarachnoid hemorrhage (SAH), or other space-occupying lesion. Head pain that spreads into the lower neck and between the shoulders may indicate meningeal irritation due to either infection or subarachnoid blood; it is not typical of a benign process. Patients over 50 years of age with new onset or progressively worsening headache are at significantly greater risk of a dangerous cause of their symptoms, including an intracranial mass lesion and temporal arteritis Meningismus (e.g., stiff neck) may indicate meningitis or SAH. This is less sensitive and less specific in adults older than 60 years. Headache presenting with fever and petechial or purpuric rash is concerning for the presence of bacterial meningitis. Some ophthalmologic findings, when present, should raise the possibility of a serious condition. Papilledema (blurring of the optic disks seen during funduscopic exam) is indicative of increased intracranial pressure, possibly due to a tumor. Loss of vision can be seen with temporal arteritis, optic neuritis, carotid artery dissection, or in acute narrow angle glaucoma Also, a new headache type in a patient with cancer suggests metastasis, and warrants further workup. Patient information The vast majority of headaches are of benign nature and do not pose any risk for the patients, but in some cases headaches can be a manifestation of an underlying condition that, if unrecognized, may lead to dire consequences. Seek emergency care if: 1) Sudden onset of significant headache (?thunderclap? headache). 2) It is the ?first? or ?worst headache of your life? 3) Changes in mental status (e.g., altered consciousness, personality changes) or seizures. 4) New headache with fever, stiff neck, skin rash. 5) A new headache associated with neurologic symptoms (e.g., weakness, numbness, impaired vision). While migraine headache can sometimes cause these symptoms, a person should be evaluated urgently the first time these symptoms appear 3. See a doctor if: 1) Persistent, or very frequent headache 2) Worsening pattern of headache, or headache that interferes with the person?s daily activities. 3) Presence of nausea, vomiting, worsening of pain with bending over, staining or coughing. Useful information for the patients on this topic can be found on these websites:
- www.patients.uptodate.com
- www.nlm.nih.gov/medlineplus/healthtopics.html
- www.achenet.org
- www.ahsnet.org
- www.i-h-s.org
References 1: Neurology in Clinical Practice, Walter G. Bradley et al, 4th edition, 2004. 2: The international classification of headache disorders; Cephalalgia, Volume 24 Supplement 1, 2004. 3: UpToDate online, accessed at www.uptodate.com 4: Manolette R Roque, eMedicine article on Giant cell arteritis. 5: Neurology in Clinical Practice, Walter G. Bradley et al, 4th edition, 2004. 6: Principles of Neurology, 8th edition, Allan H. Ropper and Robert H. Brown. 7: The Headaches, J. Olesen et al, 1993. Web References 1: Levin Morris The Many Causes of Headaches Postgraduate Medicine Volume 112: No.6 December 2002 MCQ 1) A 71-year-old woman presents with a history of 4 days of headache, blurry vision, and scalp tenderness over her left temple when she combs her hair. Which one of the following options does NOT apply to the type of headache this patient has?
- a)Visual symptoms are present in about a third of the patients
- b)Age is the main risk factor, most of the cases occurring in people older than 50
- c)Steroids are usually very effective for this type of headache
- d)A biopsy of the temporal artery should be performed for accurate diagnosis, and the start of therapy should be withheld until the results of the biopsy are back
2) Which option is true regarding Migraine headaches?
- a)Migraine with aura is the most common subtype of migraine
- b)Migraine with aura has a higher average attack frequency, and is usually more disabling than migraine without aura
- c)Migraine pain characteristically lasts 45-120 minutes, and is usually not modified by physical activity
- d)Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), when checked on migraine patients, are usually within normal range.
3) Migraine with aura is characterized by attacks of reversible focal neurological symptoms. Which of the following is true regarding this entity?
- a)Visual disturbances are the most common type of aura, accounting for the majority of the neurologic symptoms associated with migraine.
- b)The most characteristic visual aura of migraine is called ?amaurosis fugax?, and it?s characterized by a sudden loss of central vision that goes back to normal within a few minutes.
- c)The migraine aura is usually of sudden onset and lasts for several hours, but usually goes away before the migraine headache starts.
- d)The aura is commonly caused by vascular malformations within the brain.
4) A 28-year-old male presents with a history of recurrent attacks of severe, strictly unilateral pain, with ipsilateral lacrimation and eye congestion, occurring every other day for the past week. What is the best next step in the management of this patient?
- a)Perform a lumbar puncture to obtain cerebrospinal fluid for analysis
- b)First obtain a computed tomographic scan of the head to make sure there are no signs of intracranial hypertension
- c)Inhalation of 100% oxygen by a nonrebreathing mask during the attacks
- d)Refer the patient for urgent section of the trigeminal nerve to alleviate his symptoms
5) Disregulation of the trigeminovascular system is likely involved in the genesis of both migraine headaches and cluster headaches (T or F) 6) A 34-year-old woman presents to the Emergency Department complaining of severe headache. It started suddenly while she was doing laundry 4 hours ago, and it feels like the worst headache of her life. She is alert and oriented, and has no focal neurological findings in physical exam. Which one of the following is true regarding her case?
- a)Her type of headache is third in frequency among primary headaches after tension-type headaches and migraines.
- b)She probably has a “sentinel headache” caused by a minor leak from an aneurysm, and she should be immediately started on steroids to prevent a full-blown subarachnoid hemorrhage (SAH)
- c)We can be fairly certain she doesn’t have a SAH because of the lack of abnormal neurological signs
- d)A CT scan of the head might reveal the right diagnosis.
7) Which of the following statements regarding the role of physical exam in the differential diagnosis of headaches is more accurate?
- a)Papilledema is often found in the funduscopic eye exam in patients with elevated intracranial pressure
- b)In the patient with headache, the physical exam is often more revealing than the history
- c)If giant cell arteritis is suspected the examiner should avoid palpating the skull in the temporal areas
- d)If nuchal rigidity (stiff neck) is found on a headache patient, then the diagnosis is meningitis and no further work up is needed.
8) Which statement is true regarding sex predominance in the different types of headache?
- a)All types of headache are more prevalent in women
- b)Cluster headaches are seen more frequently in men
- c)Primary headaches are more prevalent in women, while secondary headaches are more prevalent in men
- d)Migraine with aura typically occurs in women, whereas migraine without aura can occur in both women and men
9) A 20 year old woman complains of getting a bad headache every time she gets her period. The pain is unilateral, localized to the frontotemporal region, pulsating, severe, and it gets even worse with physical activity or bright lights. She sometimes gets a similar headache when she doesn?t get enough sleep at night. What would you tell this patient regarding her headache?
- a)She could benefit from a trial of oxygen therapy, which is quite effective aborting this kind of attacks
- b)Given the fact that she?s been getting these headaches for longer than 3 months, she should refrain from taking pain medications during the attacks to avoid getting medication overuse headache
- c)Sumatriptan could be quite effective to treat her headache
- d)She may start having visual blurring which may become permanent if prompt therapy is not instituted
10) A 62 year old man has been suffering from daily headaches for the past couple of weeks. The pain is worse in the morning (on awakening), aggravated by coughing, and sometimes associated with nausea and vomiting. What?s the best next step in the management of this patient?
- a)A CT of the head should be obtained
- b)His headache is very likely to be secondary to undiagnosed arterial hypertension
- c)Treatment with some antidepressants (e.g. amitriptyline) can help reduce the frequency and intensity of the attacks
- d)Start him on non–steroidal anti-inflammatory drugs (NSAIDs) like naproxen, and add sumatriptan or ergotamine if no significant improvement is seen in the first few days of treatment
11) A 19 year old female college student presents with a 12 hour history of fever, malaise, and head pain that spreads into the lower neck and between the shoulders. On physical exam the patient appears to be in deep sleep, difficult to wake up, and when she does wake up she talks nonsense and goes right back to sleep. Which of the following options apply to this case?
- a)A lumbar puncture should be performed immediately to obtain cerebrospinal fluid for analysis
- b)A lumbar puncture is indicated, but a CT of the head should be obtained first
- c)Antibiotics should be started within 12 hours after the patient is first seen, even if the results of the lumbar puncture are not back yet
- d)Antibiotics would probably not be useful in her case, for the cause of her headache is likely to be a ruptured intracranial aneurysm
12) Which of the following statements regarding laboratory tests in the workup of headaches is true?
- a)If the patient is clearly suffering from a secondary headache there is usually no need to get any laboratory or imaging test
- b)The erythrocyte sedimentation rate is usually elevated in cases of giant cell arteritis
- c)Electroencephalography is a very useful test in the workup of patients that present with headache as their only symptom
- d)All of the above
13) A 72 year old man with a history of uncontrolled arterial hypertension and atrial fibrillation treated with coumadin presents with sudden onset of severe headache, vomiting, and progressive lethargy. His vital signs are remarkable for a blood pressure of 177/106, and the physical exam reveals a dilated left pupil. What would be the best next step in the management of this patient?
- a)The patient might have suffered an intracranial bleed, so an MRI of the head should be performed for diagnosis
- b)A CT of the head would be the imaging test of choice for him
- c)A lumbar puncture should be performed as soon as possible
- d)Aggressive anti-hypertension treatment should be started immediately to return the blood pressure to the normal range
14) Which of the following statements is true?
- a)Sudden onset of headache, or severe persistent headache that reaches maximal intensity within a few seconds or minutes after the onset of pain, is very suspicious for the presence of a brain tumor and should prompt a neurosurgical consult
- b)The “first” or “worst” headache of my life is a description that typically accompanies a giant cell arteritis (temporal arteritis).
- c)Physical activity, light, and noise, are classic aggravating factors for tension-type headaches, which helps distinguishing this type of headache from migraines.
- d)None of the above.
15) Which of the following symptoms are most suspicious for a brain tumor as the cause of headache?
- a)Numbness and tingling of the lips, lower face, and fingers of one hand.
- b)Worsening of the headache with physical activity
- c)Worsening of the headache with bending over
- d)Seeing a hazy spot in the center of a visual field followed by a shimmering light of different patterns.
16) A 63 year old woman presents with a two day history of headache, associated with a fluctuation in the level of consciousness (confusion first, then lethargy). Which of the following options is more likely the cause of her headache?
- a)Giant cell arteritis (temporal arteritis)
- b)Encephalitis
- c)Migraine with aura
- d)Headache associated with refractive errors (HARE)
17) Which of the following would be considered ?red flags? in patients with headache?
- a)Headache associated with fever and generalized rash
- b)Headache associated with changes in mental status
- c)Patients over 50 years of age with new onset or progressively worsening headache
- d)All of the above
18) A 35 year old man has been suffering from recurrent episodes of headache that are usually preceded by nausea, blurred vision, yawning and difficulty concentrating that occur one day prior to the onset of the pain. Which one of the following statements applies to this case?
- a)He may be suffering from cluster headaches
- b)Both migraine with aura and migraine without aura can present this way
- c)He may have a case of idiopathic intracranial hypertension (pseudotumor cerebri)
- d)His symptoms are suspicious for the presence of a cerebral venous thrombosis (CVT).
19) A 46 year old woman who has been taking ibuprophen and sumatriptan on a daily basis for the treatment of her migraine headaches for the past several months complains of not having a single day go by without her suffering from a headache. What should you tell the patient regarding her condition?
- a)She most likely developed a brain tumor that is worsening her headaches.
- b)She is probably alternating between migraine headaches and tension-type headaches, causing her migraines to seem more frequent than they really are.
- c)She needs to increase the dose of her pain medications, and probably add some other agent for prophylaxis.
- d)She is probably overusing her pain medications, and her headache would likely revert to its previous pattern within 2 months if she discontinues the overused medications.
20) Which of the following secondary headaches is most likely to present with meningismus (e.g., stiff neck)?
- a)Brain tumor.
- b)Post-traumatic headache.
- c)Subarachnoid hemorrhage.
- d)Cerebral venous thrombosis (CVT).
Correct answers: 1) D 2) D 3) A 4) C 5) TRUE 6) D 7) A 8) B 9) C 10) A 11) B 12) B 13) B 14) D 15) C 16) B 17) D 18) B 19) D 20) C
