Disease and Pain.
The Common vein Copyright 2008
James Armstrong PA Ashley Davidoff MD
Introduction
As shown in the section on classification of pain in the basic science series, and repeated in the diagram below, there are many disorders that cause pain.
Acute somatic pain signifies imminent and possibly dangerous bodily injury. Its presence evokes an immediate reaction either with a simple reflex or complex reaction. The pain comes and goes and the body as an organism proceeds in a normal fashion thereafter. The pain becomes an experience of the past and is memorialized as a learning experience in the brain. The result is a better prepared response to a similar insult in the future.
Disease however happens! It comes in the context of many pathologies and the body does not like it. Inflammation is commonly the underlying pathophysiology for many of the disorders. Disease is usually (but not exclusively) an intrusion of the visceral sensory system and although the discomfort is still classified as pain, the experience is very different from the acute somatic experience described above. The pain of disease begins as one experience, butmay often fluctuate in parallel to the dynamic reactions of the body as it attempts to counteract the natural history of the inciting process.
Traumatic injury, as in the case of a bone fracture, is easily understood in this vein. On an average of 4-6 weeks healing time, the pain gradually subsides. The inciting injury and bodily response are both finite and predictable. If on the other hand, a chronic progressive or slowly healing disease ensues, then the pain syndrome will reflect the net result of healing versus ongoing pathology.
As shown in the section on classification of pain in the basic science series, and repeated in the diagram below, there are many disorders that cause pain.
Acute somatic pain signifies imminent and possibly dangerous bodily injury. Its presence evokes an immediate reaction either with a simple reflex or complex reaction. The pain comes and goes and the body as an organism proceeds in a normal fashion thereafter. The pain becomes an experience of the past and is memorialized as a learning experience in the brain. The result is a better prepared response to a similar insult in the future.
Disease however happens! It comes in the context of many pathologies and the body does not like it. Inflammation is commonly the underlying pathophysiology for many of the disorders. Disease is usually (but not exclusively) an intrusion of the visceral sensory system and although the discomfort is still classified as pain, the experience is very different from the acute somatic experience described above. The pain of disease begins as one experience, butmay often fluctuate in parallel to the dynamic reactions of the body as it attempts to counteract the natural history of the inciting process.
Traumatic injury, as in the case of a bone fracture, is easily understood in this vein. On an average of 4-6 weeks healing time, the pain gradually subsides. The inciting injury and bodily response are both finite and predictable. If on the other hand, a chronic progressive or slowly healing disease ensues, then the pain syndrome will reflect the net result of healing versus ongoing pathology.
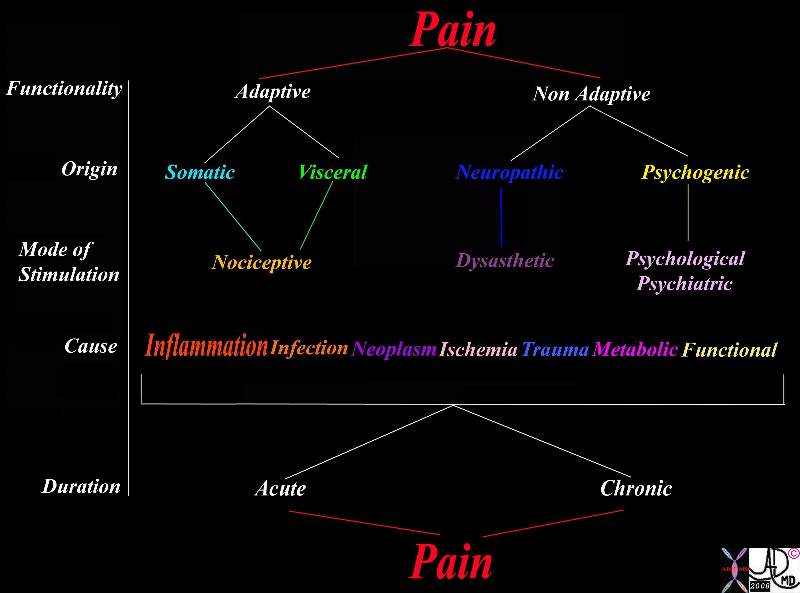 Classification of Pain Classification of Pain |
|
This table explores the variety of ways of classifying pain. The left hand column reveals the classification based on functionality, origin, mode of stimulation, pathological causes and relationship of pain to chronicity. As for functionality, it may be adaptive or non adaptive. The pain may originate from somatic or visceral nociceptors or from damaged nerves in which case it is called neuropathic, or it may be psychogenic. The causes are usually via the inflammatory process but may result from any of the diseases listed.
83199b11.8s pain classification adaptive Non Adaptive somatic visceral nociceptive neuropathic psychogenic dysasthetic psychological psychiatric inflammation infection neoplasm ischemia trauma metabolic functional acute chronic duration cause mode of stimulation origin functionality Courtesy Jamie Armstrong PA Table copyright 2008
|
However, when disease directly impairs the nervous system, the pain becomes neuropathic and not necessarily related to either the aggressiveness of the disease or healing. This is more complex and harder to treat. Such pain occurs with chronic inflammation, chronic ischemia and malignant disease for example. This pain is less dependent on healing rates but more so on the premise of whether or not healing occurs at all. Neuropathic pain can become debilitating and sometimes unrelenting.The complexity that may be added by ongoing social, cultural, and psychological responses makes this the most difficult pain to comprehend on a physical level. We will discuss neuropathic pain in the organic disease section which follows.
Disease 
The mechanisms through which patients experience pain differ according to the injurious process and tissue response. Below we describe the classical disease processes, each with a unique mechanism and subsequent pain signal. The diseases that involve the somatic receptors tend to present with acute pain. Examples including skin lacerations, meningitis, pericarditis, pleurisy, peritonitonitis, and periostitis cause sharp pain. As you may have noted the suffix, “itis” in may of these conditions, tells us that these are all of an inflammatory nature.
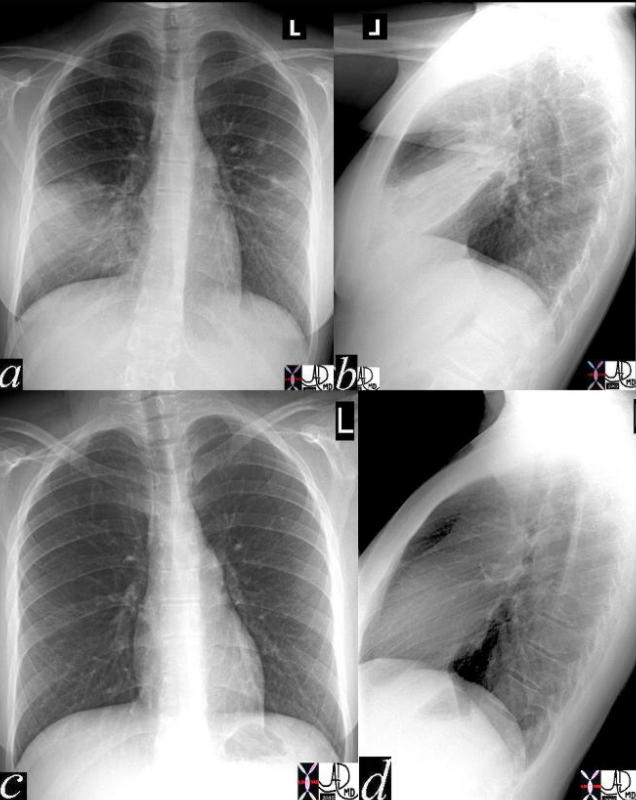
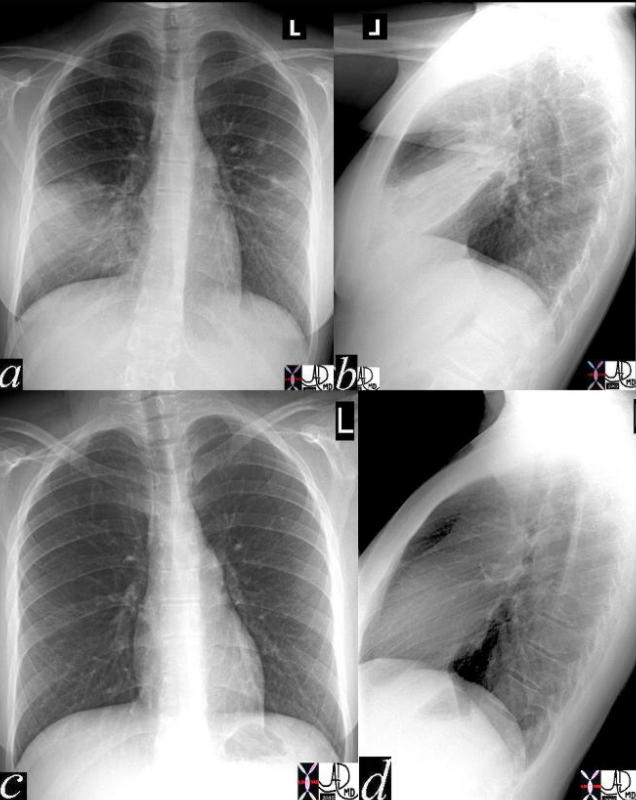
Right UpperLobe Pneumonia
|
|
The chest X-ray in A-P and lateral projection show a pneumonia as a dense area in the right upper lobe (a and b). The pneumonia abuts the pleural surface and incites inflammation of the pleura and causes pain. Images c and d show return to normal 4-6 weeks after initiation of treatment after which time both the pneumonia and the pain have resolved.
41819c02 Courtesy Ashley Davidoff MD medical students code chest CXR imaging lung plain film pneumonia radiology resolution
|

Pneumonia and Pleuritic Pain
|
|
The diagram shows an area of pneumonia (yellow) of the right upper lobe that touches the visceral pleura. The visceral pleura is in intimate contact with the parietal pleura and thus both components become inflamed. With normal breathing, these two surfaces rub each other, and in the case of inflammation they rub each other the wrong way, resulting in pleuritic pain. The pain restricts deep breathing in an attempt to “rest” the pleura, but a pleural effusion, commonly a result of pneumonia, would separate the two by creating a neutral zone between them, and thus prevent their physical contact. The concept of a neutral buffer zone is not a new concept in the ancient discipline of biology.
42540c02a01 lung consolidation pleuritic pain pneumonia RUL pneumonic infiltrate pain on inspiration pleura paietal pleura cough Davidoff Art Courtesy Ashley Davidoff MD
|
Diseases that incite the visceral nociceptors commonly evolve from an increase in pressure within an organ. Distension forces may cause physiological cramps due to “gas pain”, menstrual cramps, and labor. More serious cramps may be caused by obstructive disease processes like bowel obstruction, renal colic, and bilary colic. Many diseases like acute cholecystitis, appendicitis, and cholangitis are a combination of the two.

Distension and Peritonitis
|
|
The CT scan through the abdomen is from a patient with acute cholecytitis. It shows a gallbladder that is distended and is associated with inflammatory exudate surrounding the gallbladder (arrows) and an inflamed area of peritoneum. The pain arises from both the visceral nociceptors due to increased luminal pressure and somatic receptors of the peritoneal lining. The latter pain is aggravated and induced during inspiration, particulalrly when the examining hand puts some pressure in the right upper quadrant (Murphy’s sign), or by pressure from the ultrasound transducer over the visualized gallbladder (sonographic Murphy’s sign).
16157c01s.81 gallbladder edematous wall distended gall bladder edema in the wall fluid in the fat surrounding the gallbladder indurated fat free fluid in Morrison’s pouch acute cholecystitis stones not visible on CT scan pain peritonitis Murphy’s sign inflammation CTscan Courtesy Ashley Davidoff Copyright 2008 All rights reserved
|
Inflammation 
The primary response to any injury in the human body is inflammation. This is an immune mediated defensive cascade of events, initiated by increased vascular perfusion and permeability to the area of insult. Next, a fusion of cellular migration and degranulation leads to a release of peptides that stimulate, among other things, specialized cellular pain receptors known as proteinases. The subsequent signals generated by inflammation cause symptoms that include burning, aching and pressure.
Sensitization of Receptors With Tissue Injury – Changing Thresholds
Within the extracellular space, there are many substances that affect the sensitivity of the free nerve endings, usually to increase the sensitivity or lower the threshold to pain. Inflammation is a classic example as a phenomenon that characteristically induces the production of a variety of extracellular susbstances that either incite pain or sensitize the nerve endings to pain.

Tissue Injury Axon Reflex and Sensitization
|
|
The diagram shows the effect of tissue injury (left side of diagram) that induces the release of prostaglandin, serotonin, bradykinin, and potassium which cause sensitization of the free nerve endings to pain which lowers the threshold to pain. In addition they induce (red arrows) the axon reflex (white arrows) which causes the production and release of substance P from the free nerve endings which cause the release of histamine from the mast cells. The histamine causes vasodilation and exudation into the damaged area. Three of the hallmarks of inflammation are explained in the diagram. Pain, swelling (edema) and hyperemia increased blood flow.
prostaglandin serotonin bradykinin potassium substance P mast cell histamine vasodilation nociceptors pain receptors Davidoff art Copyright 2008 83169b11.8s
|
Pain, or its Latin equivalent “dolor”, is one of the classical hallmarks of inflammation as was described in the latter half of the second century AD by Celsus, a Greek philosopher. Anti-inflammatory agents, mild heat, and cooling tend to reduce the inflammatory reaction and thus reduce the pain. They provide relief by neutralizing the effect of the substances that sensitize or incite the pain.
The pain sensitizing peptide compounds released as a consequence of tissue injury include prostaglandins, serotonin, bradykinin and potassium. They in turn stimulate a local axonal reflex causing the free nerve endings to release substance P or calcitonin and some gene related peptides (CRGP). Substance P and CGRP cause mast cells to release histamine which in turn causes vasodilation and local edema, other hallmarks of the inflammatory process. Some of these substances activate pain through the chemoreceptors including ATP prostanoids and hydrogen ions (acid PH).
This mechanism has one process in mind for you and that is to rest the injured part. A fractured arm becomes hypersensitive to touch or pressure and induces you to hold the part as still as possible, sometimes even employing your other hand and arm to hold the injury as still as possible. This forces one to pure rest to promote healing and to progress without further injury.
Infection 
Infection most often manifests as inflammation. However the pattern and subsequent pain are different. Infection by nature, delays healing. Pain complaints will therefore be more prolonged and progressive. Subsequently, inflammatory pain from infection will endure, deepen or spread until treatment and healing is initiated.

Osteomyelitis of the Thoracic Spine
|
|
The CT scan in this patient with severe back pain and fever shows destruction of the disc space of T7-T8 as well of both upper and lower involved thoracic vertebra (arrow in b). The transverse image through the space shows bony fragmentation and destruction of the vertebral bodies with bulging paravertebral soft tissue swelling of an evolving abscess (yellow). The red lines reveal somatic visceral periosteal layers that are involved in the inflammatory and infectious process. The pain likely arises from a combination of factors including the swelling caused by the infection (pressure) and involvment of the periostial, pleural, and joint linings.
78031c04.8s pain back thoracic spine intervertebral disc discitis diskitis osteomyelitis soft tissue changes paravertebral periostitis periosteum bone destruction tuberculosis TB question CTscan Courtesy Ashley DAvidoff MD copyright 2008 |
Neoplasm 
Pain in the setting of neoplasm may be acute or chronic and variably related to the cancer. Somatic pain is most commonly related to metastatic bony involvement irritating the periosteum. There may be tumor induced osteolysis with release of prostaglandin E2 which sensitizes the nerves. When the metastases are in the vertebral column, compression fractures or expansile mechanical changes may impinge on the nerves or spinal cord and induce neuropathic pain. Bone involvement may become manifest as a somatic throbbing or aching pain.

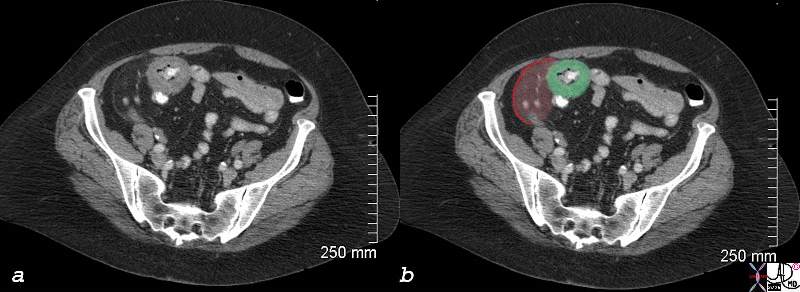
Lytic metastases, Compression Fractures and Cord Impingement
|
|
The sagittal reconstruction of a CT scan shows extensive lytic metastases throughout the thoracic and lumbar spine (green overlay in b). A lytic lesion is also noted in the pubic symphisis. The combination of somatic periosteal nociceptor involvement, mechanical nociceptors that sense the expansion, resulting tissue damage and the release of substances that incite the chemical nociceptors, and possibly damage to the spinal cord and resulting neuropathic pain mechanisms, give adequate cause for pain in this scenario.
75598.8cs03 bone lumbar spine metastasis compression fracture lytic metastases CT scan Courtesy Ashley Davidoff MD copyright 2008
|
When cancer pain is visceral in origin, it is due to pressure effects as the tumor occupies space. In this instance, mechanical nociceptors are stimulated. Alternatively, tissue damage may release of a variety of chemicals including cytokines. K+, bradykinin, interleukin and growth factors that stimulate chemical nociceptors and promote inflammation and a decreased pain threshold. Impingement on nerves or the spinal cord may cause neuropathic pain.
Cancer therapy may also cause pain due to tissue burns from radiation or localized pain at the sight of a chemotherapy injection. Pharmacotherapy, specifically the vinca alakaloids platinols or tamoxifen may also cause pain that may be neuropathic.

Hepatocellular Carcinoma
Space Occupation, Capsular Involvement and Neuropathic Pain
|
|
The pathological specimen from a patient who succumbed to a large hepatocellular carcinoma shows a large space occupying tumor. Pain is theoretically induced by the tumor from a variety of sources. It may originate from the involvement of the tumor that extends to the periphery and capsule of the liver with its somatic nociceptors, from around the neurovascular bundles within the portal triad and its nociceptor component, or from chemical released by the tissue destruction expected by the tumor on surrounding structures. Despite the potential for extreme pain in this situation, the response in each patient is quite variable. For some patients, the pain in this scenario may be more of an ache or discomfort rather than severe incapacitating pain that one may expect from this giant tumor.
24008 liver fx mass portal vein fx invasion satellite nodule multicentric dx hepatocellular carcinoma hepatoma HCC grosspathology Courtesy Barbara Banner MD
|
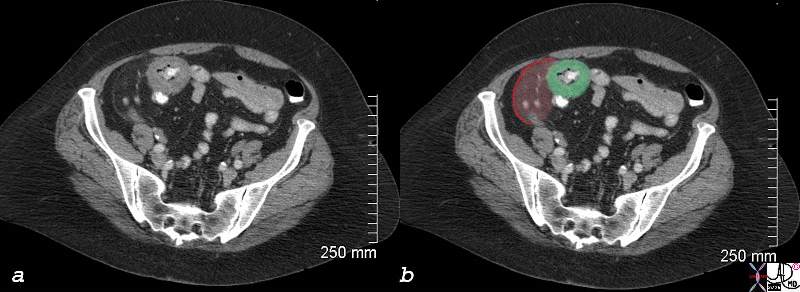
Cecal Carcinoma with Peritoneal Involvement
|
|
In this case the 77year old female patient presents with right lower quadrant pain. The CTscan shows a napkin ring thickening (green) surrounding the region of the cecum subsequently proven to be carcinoma. When restricted to the cecum alone the cecal carcinoma tends to be silent since there is neither significant distension nor peritoneal involvement to incite any nociceptors. These patients usually present when complications such as anemia or obstruction surface. In this patient the neoplasm incited an inflammatory reaction in the surrounding fat (pale see through red) and peritoneum (bright red line) witnessed as a subtle thickening of the peritoneum. This was sufficient to stimulate the nociceptors and incite pain.
83037c03.8s 70 F presents with right lower quadrant pain RLQ colon cecum mass colon carcinoma napkin ring peritoneum peritonism somatic pain induration CTscan Courtesy Ashley Davidoff MD copyright 2008 |
Mechanical Disorders 
Pressure sensitive nociceptors are positioned in both the somatic regions but predominate in the viscera. Stimulation of the pressure sensitive nociceptors is perceived as aching or throbbing and is characteristic of a range of cramps and colic that are “normal” day to day sensations to the more severe pain of childbirth.

Pressure Nociceptors
|
|
The mechanical pressure sensitive nociceptors are dominantly located in the organs and are responsible for sensing pressure changes. The diagram shows a wave of increased pressure (pale yellow) impinging on the free nerve endings of the pressure receptors, with red nerve endings being stimulated by the pressure.
87559pb04b02b11.8s pressure receptors nociceptors mechonoreceptors free nerve endings trees in the body Davidoff art copyright 2008
|
These pains however are seen in pathological situations and the word “ache” or “cramps” seemingly and incorrectly implies a lack of severity. Anybody who has experienced renal colic will tell you that the pain is probaly the most severe pain they have experienced. In fact the stone that can induce the worst pain need only be 2-3mms in diameter or less.
Another pain pathway in the body arises from gamma sensors located in the muscle spindle apparatus of skeletal muscle. These receptors may be activated at rest or with motor function depending on the source. The most common form of muscular pain occurs after strenuous activity when muscle spindles have become relatively overused through stretching and contracting. The resultant achy pain associated with movement has often been controversially described as secondary to lactic acid and oxygen debt to the muscle fibers. One confounding factor however is that neuropathic pain is also transmitted in the same apparatus but at rest. Patients with spinal cord injuries may suffer from muscular pain as part of a syndrome called Central Pain.
Obstruction 
Obstruction of any of the tubular systems within the body and particularly of the gastrointestinal tract can cause pain by stimulating mechanical and pressure sensitive nociceptors in the viscera. The afferent nerve fibers are situated within the viscera and are commonly carried by similar afferent fibers of the sympathetic system.

Small Things Can Cause Big Packages of Pain
|
|
The worst pain of this patients life was caused by a 3mms stone in the right distal ureter seen on this non-contrast CT, as a white speck in image d. In image a, a similar stone remains in the kidney, (arrow) while image b shows mild hydronephrosis, and image c shows hydroureter (arrow).
83149c02.8s right flank pain kidney renal pelvis ureter stone ureterolithiasis hydronephrosis pain delayed nephrogram CTscan Courtesy Ashley Davidoff MD copyright 2008
|
Less severe forms of visceral pain also occur in other obstructive diseases such as small bowel obstruction. There may be many causes but the most common is adhesions from prior surgery. The pain is often accompanied by nausea and vomiting.

Small Bowel Obstruction with Distension
Inciting the Mechanical and Pressure Nociceptors
|
|
The plain film of the abdomen shows dilated loops of small bowel associated with a paucity of gas in the decompressed large bowel. These findings are consistent with small bowel obstruction and were associated with diffuse abdominal aching pain, nausea and vomitting.
00554 small bowel fx dilated fx enlarged dx SBO obstruction plainfilm Courtesy Ashley Davidoff MD DB
|
Distension 
The pain described above is caused by distension but there are other causes of distension that can induce pain. The sudden stretching of a capsule induced by edema, hematoma, or a subacute accumulation of pus can induce pain that can be somatic or visceral.
Trauma 
Trauma can cause pain in many ways including local and systemic manifestations. Somatic,visceral, neuropathic, inflammatory, infectious, mechanical, metabolic, and chemical influences all can play a role.

Severe and Painful Trauma
|
|
The post operative angiogram of the hand is one of the most painful X-rays I have experienced in my career and the image is older than 30 years. The exact history eludes me but there has been obvious traumatic injury to the hand with multiple fractures (black arrows), a transverse skin incision that contains a broad band of air (white arrow), with probable debridement of the severely injured metacarpal row, and extensive pinning and wiring of the thumb following surgical trauma. The combination of the large somatic sensory nociceptor supply to the hand, with the extensive skin, bone, and tissue damage, creates a scenario of extreme pain. It is difficult to perceive the extent of the pain that this poor patient went through. The remarkable feature is the maintenance of blood supply to the hand despite the extensive injury to harder but less pliable bones.
artery bone trauma fracture post op pain artery digital trauma angiography angiogram fractures Courtesy Ashley DAvidoff MD copyright 2008 17496c02.8s
|
Ischemic Pain and other Circulatory Disorders 
Insufficient perfusion of tissue leads to hypoxia which is usually manifested as pain. The discomfort may be somatic as in the classic muscular ache of claudication, or visceral as described by waxing and waning abdominal pain of ischemic bowel syndrome. The pattern of provoking or relieving factors are helpful descriptors in characterizing the supply and demand mismatch of compromised blood flow.
The biochemical changes by nature are complex, but include the loss of high-energy compounds and acidosis due to anaerobic production of lactate. Hydrogen ions are potent stimulators of pain nociceptors. Other algesiogenic chemicals include substance P, K+, kinins, interleukins, adenosine, histamine, and leukotrines. Adenosine has strong associations with ischemic pain as well.

Chemical Nociceptors
|
|
The diagram illustrates the many chemical factors, each represented in different color and different shapes, that can incite the chemical nociceptors. The hydrogen ion and acidic PH is a common stimulant of these receptors.
87559pb04b02b02b02.8s nociceptors chemical receptors free nerve endings trees in the body hydrogen ion algogenic substances autocids substance C K+ kinins interleukins adenosine histamine leukotrines H+ Davidoff art copyright 2008
|
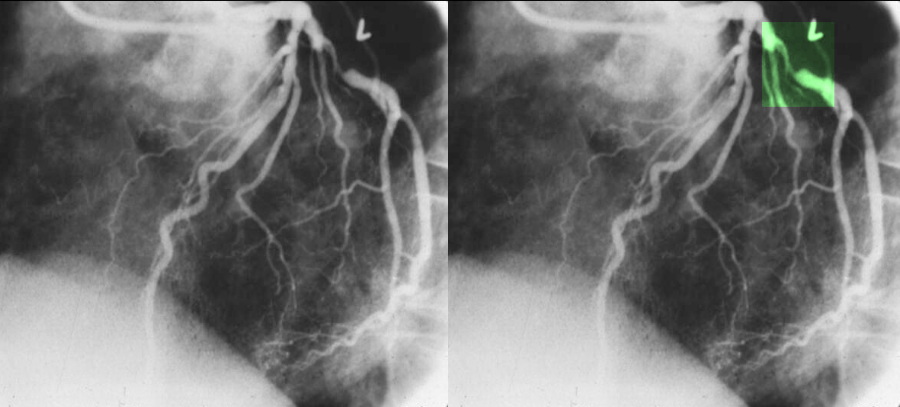
Angina is a common and often debilitating manifestation of ischemic disease. In this case, there is deficiency of oxygen to cardiac muscle inducing discomfort with exercise that is relieved by rest. The underlying cause is narrowing of the coronary arteries by atherosclerosis.
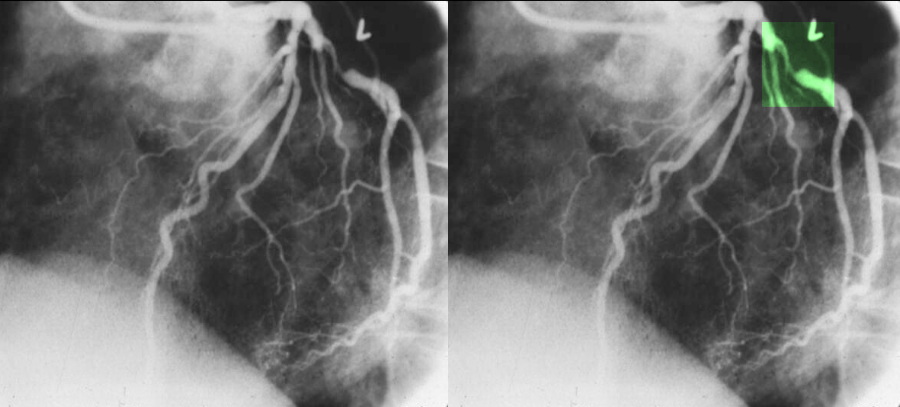
Coronary Stenosis
|
|
The coronary angiogram in the LAO projection shows a severe proximal stenosis (about 90%) of the circumflex with some post stenotic dilatation. The second image has a green overlay indicating the region of disease with the post stenotic dilatation. The narrowing causes angina due to poor oxygen supply and resulting depletion of high energy compounds and acidosis due to anaerobic production of lactate, hydrogen ions, and adenosine.
Courtesy Ashley Davidoff MD. 07023c code heart artery coronary circumflex stenosis atherosclerosis imaging radiology angiography overlay
|
Other Vascular and Circulatory Disorders
Migraine
The blood vessel wall is richly endowed with nociceptors and the pain of migrainous headaches are thought to have a vascular origin. The newer neurovascular theory suggests that the inciting event is a cortical disorder that subsequently causes the vessels to vasodilate and constrict. It is these events which are responsible for the pain.
Venous Congestion
Venous congestion can cause pain on many levels. It is classically seen in patients with acute inflammation. Due to a combination of higher pressures, chemical forces and the vascular response, edema ensues, causing and contributing to the pain. In other patients, the venous congestion may cause swelling of the involved organ and an increase in visceral pressure thus stimulating nociceptors. In patients with acute tricuspid regurgitation, swelling of the liver causes distension of the liver capsule and a somatic type pain. Pelvic congestion syndromes seem to arise from pelvic varicocities commonly acquired during pregnancy and the source of a constant dull pelvic ache. A tiredness or discomfort of the legs is a similar symptom that patients with varicose veins complain of.
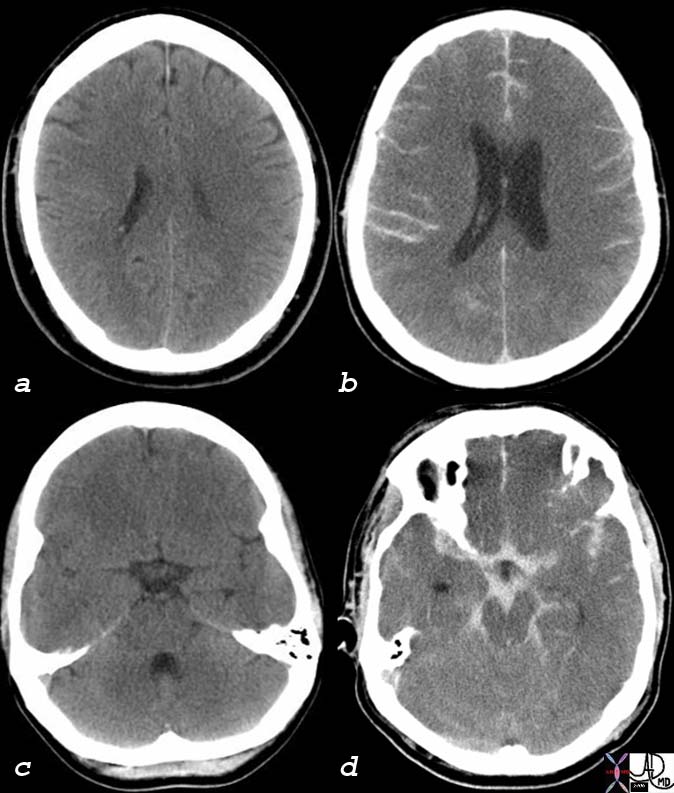
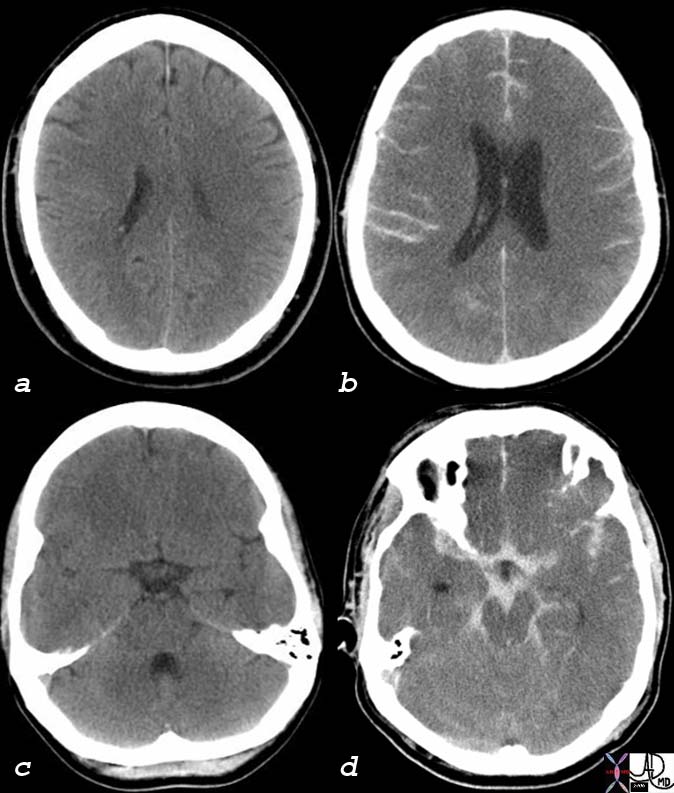
Hemorrhage 
Hemorrhage can cause a variety of pain syndromes ranging from no pain at all such as occurs in a GI bleed, to a mild visceral ache from a muscle bruise, to incapacitating headache pain caused by rupture of a berry aneurysm in the brain.
Severe Headache Awaking the Patient from Sleep
|
|
Pain that awakens a patient from sleep needs special attention since it excludes the supratentorial events of pain, implies severe physical pain, and it may herald a catastrophic event.
89081pd04b02.8s pain headache sleep woken awakened from sleep worst pain in my life headache 10 out of 10 ruptured berry aneurysm bleed blood hemorrhage meninges somatic Davidoff art copyright 2008 |
Normal and Life Threatening
|
|
These two head CT’s are from two different patients who both presented with severe headaches. The first patient (a,c) had a normal study and the headache may have been caused by migraine, cluster, or tension headaches for example. Although these headaches create significant morbidity they are relatively benign in that they are treatable. The second patient (b,d) had a life threatening subarchnoid hemorrhage due to a ruptured aneurysm characterized by the white hemorrhage in the sulci (b) and within the subarachnoid spaces surrounding the midbrain and other structures.(d) It is not practical to perform a CT on every patient who presents with a headache, since it is a very common condition. On the other hand one does not want to miss a life threatening condition that is potentially treatable. Meticullous clinical acumen and prudent clinical judgement is therefore necessary to direct management of patients with headaches and with patients who complain of pain.
The dura has the largest number of nociceptors of the meninges. In acute aneurysmal rupture, the severe pain is caused by stretching and distortionof the blood vessels that are accompanied by the nerves
76059c01 52 male headache neurological deficit normal abnormal brain cerebrum subarachnoid blood subarachnoid hemorrhage Sylvian fissures midbrain basal cisterns cerebellar folia circle of Willis cerebellum sulcus sulci ambient cisterns 4th ventricle dx probable rupture of basilar tip aneurysm berry aneurysm CTscan Courtesy Ashley Davidoff MD 76059c01 76059c02 76059c03
|
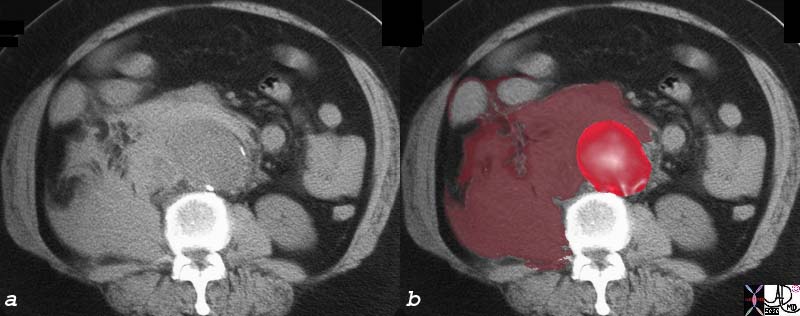
The patient who presents with acute severe back pain, hypotension, and a pulsatile abdominal mass has a diagnosis of a ruptured abdominal aortic aneurysm until proven otherwise. Action should include a prompt and urgent phone call to the vascular surgeon, a phone call to the OR, and an immediate non contrast CT of the abdomen and pelvis. The pain is mostly caused in this instance by a sudden distension of the retroperitoneal tissues inciting deep muscle and connective tissue mechanoreceptors and presumably causing tissue damage with the release of chemicals that incite the chemoreceptors.
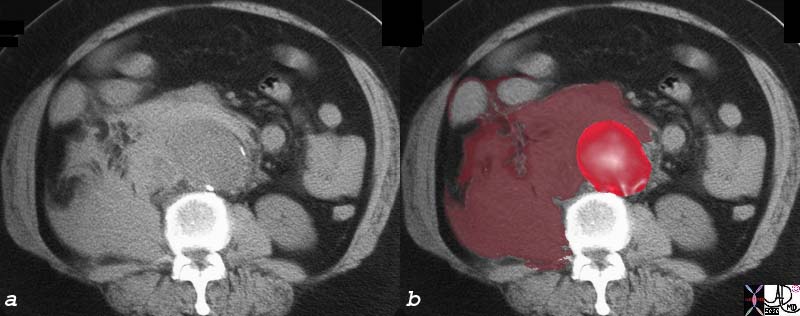
Ruptured Abdominal Aortic Aneurysm
|
| The abdominal CT is from an elderly patient who presents with acute severe back pain and pulsatile abdominal mass. Findings include an abdominal aortic aneurysm (bright red ) and a retroperitoneal bleed toward the right side where there has been a rapid and painful accumulation of blood (maroon) that expands the retroperitoneum and invades and expands the right psoas muscle. This patient suffered from a rupture of an abdominal aortic aneurysm
16548c01 abdominal aorta rupture psoas muscle retroperitoneeum aneurysm AAA back pain CTscan Courtesy Ashley Davidoff MD copyright 2008
|

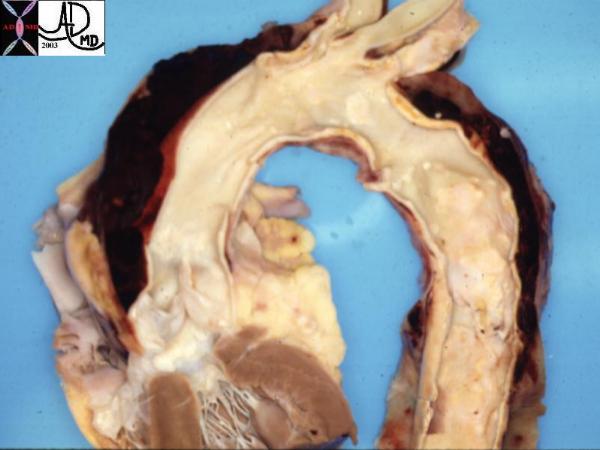
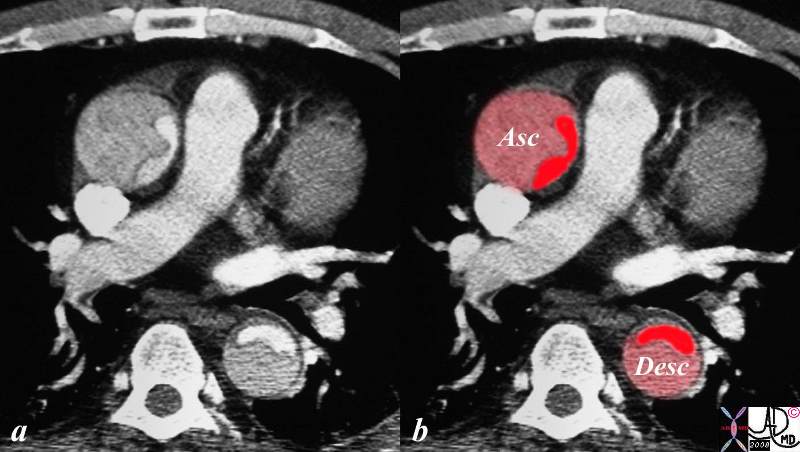
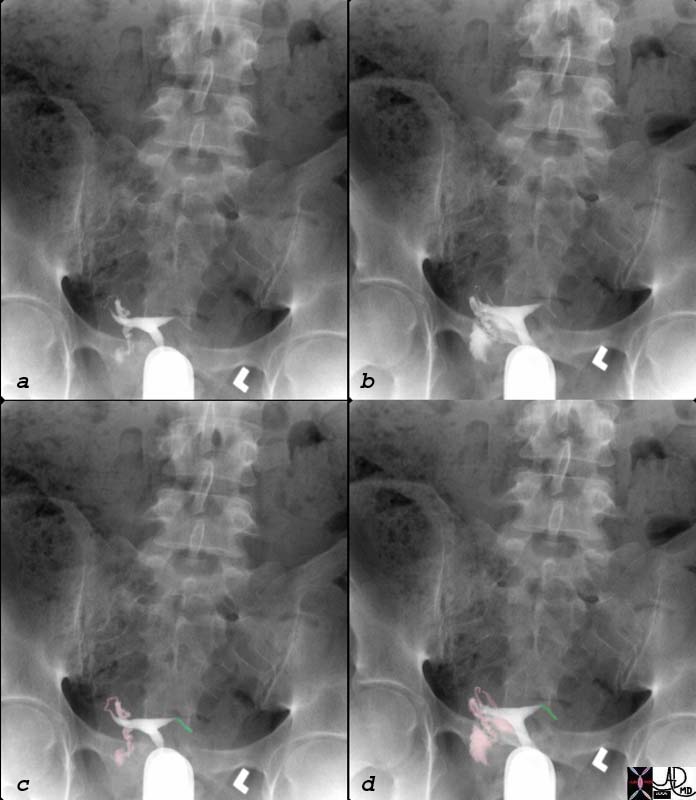
Dissection 
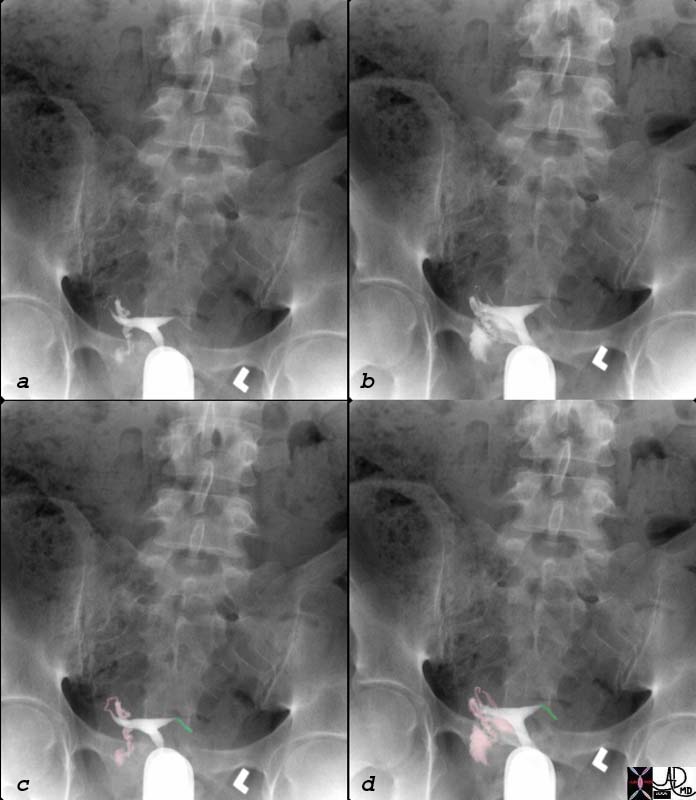
An acute aortic dissection is a cause of hyperacute back pain caused by rapid accumulation of blood within the aortic wall. The subsequent distension incites the pressure receptors. In addition, there may be dissection across the intercostal arteries which become occluded. The pain is often somatic and lancinating due to resultant ischemia of the chest wall. When the dissection involves the ascending aorta, the pain is usually in the anterior chest. A dissection extending to the descending aorta may cause interscapular pain. Aortic dissections can also involve and occlude the right coronary artery in which case it may cause classical cardiac ischemic pain.
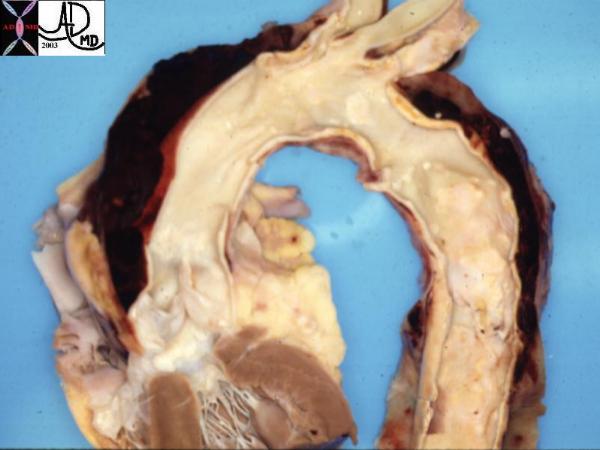
Fatal Acute Dissection
|
|
This pathological specimen shows an aortic dissection (maroon blood clot in wall) starting at the root of the aorta and extending across the arch and into the descending portion. The blood is in the false lumen. The blood that was in the true lumen has been removed..
Courtesy Henri Cuenoud MD 13421 code CVS thorax AO aorta dissection grosspathology
|
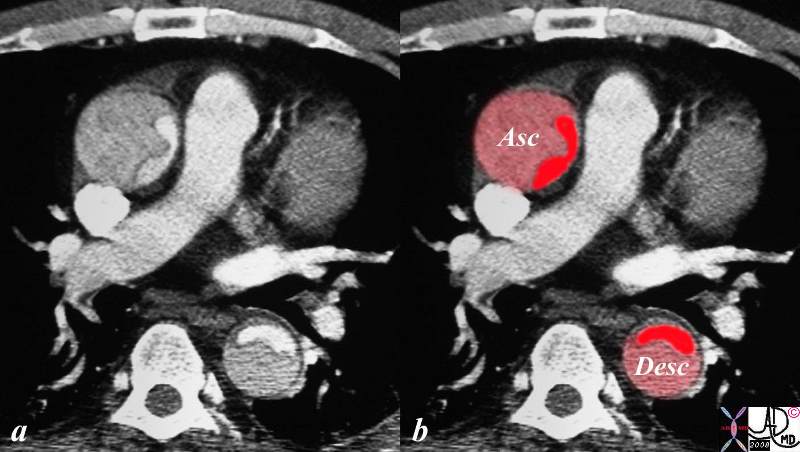
Type A Dissection
|
|
The CT image shows a dissection in the ascending and descending aorta. The lumen consists of the smaller true lumen (bright red) and the false lumen (larger with dull red) The patient presented with classical severe chest pain that radiated to the back. The involvement of the ascending aorta make s it a type A dissection and therefore treatment requires surgical repair. In this patient however the dissection extended to the descending aorta as well. Either way a type A dissection requires surgery.
20448c03.8s descending aorta ascending aorta fx dissection fx crescent dx aortic dissection type A CTscan Courtesy Ashley Davidoff MD DB
|

Other Hemorrhages and Ruptures 
Pulmonary hemorrhage can be extensive but painless as the pulmonary parenchyma is not nociceptive. However the pleura are richly endowed with nociceptors and when pleura is involved with inflammation as noted above, pain can be sharp and somatic.
 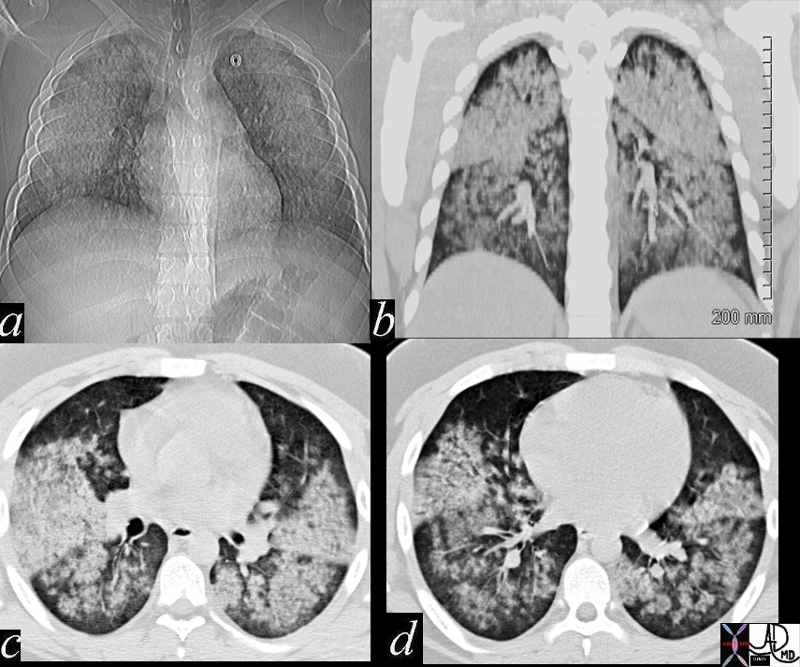
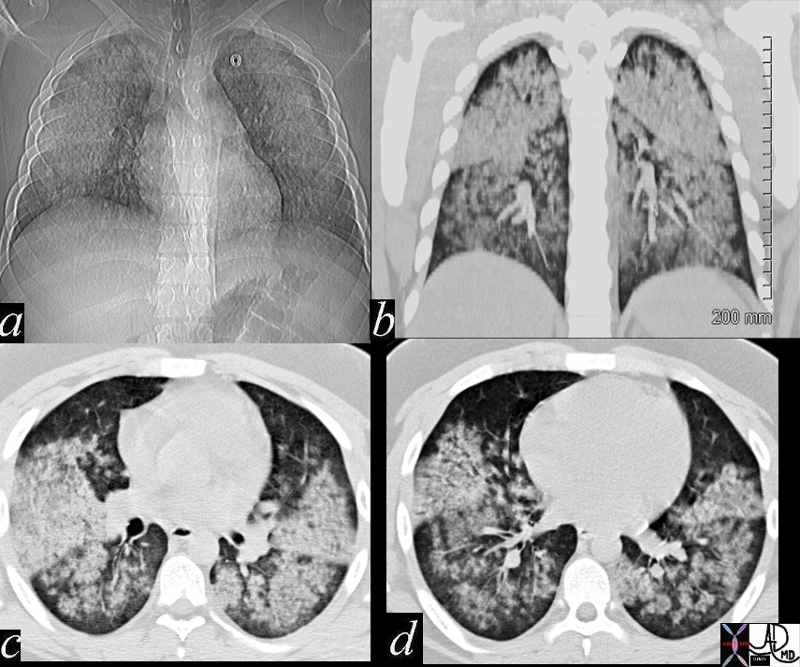
Pulmonary Hemorrhage Extensive Disease – No Pain
|
|
This 20 year old male patient presented with hemoptysis and renal failure, and following renal biopsy a diagnosis of Wegener’s granulomatosis was made. The CT shows extensive pulmonary hemorrhage characterized by white nodular infiltrates, but there was nopain associated with the extensive pulmonary findings.
47711c01 20 year old male presents with hemoptysis and renal failure chest lungs upper lobes lower lobes infiltrates acinar infiltrates fluffy infiltrates almost symmetrical fx bilateral pulmonary infiltrates renal biopsy dx Wegener’s granulomatosis with pulmonary hemorrhage blood character CTscan Daviddoff MD 47711c02
|
Hemorrhage into the peritoneal cavity is also surprisingly non-painful, though hemorrhage into the omentum as seen in trauma and following rupture of an ovarian hemorrhagic cyst can be extremely painful. The patient may present with peritonism and simulate peritonitis.
  
Football Player with Traumatic Bleed into the Greater Abdomen
|
|
This football player presented severe abdominal pain in the right upper quadrant pain with peritonism following a football game. The pain was of such concern that he was taken to the OR where hemorrhage into the greater omentum was diagnosed. In this instance pain was presumably caused by blood acting on chemoreceptors in the omentum.
44692c.8s young college football player who presents with RUQ pain and fever with normal gallbadder by USscan fx mesentery greater omentum transverse colon large bowel RUQ fx induration dx hemorrhagic bleeding of right sided component of colonic greater omentum due to traumatic injury surgical proof CTscan coronal ddx appendagitis Courtesy Ashley Davidoff MD 44692 44694 gastrocolic ligament lesser omentum copyright 2008
|
Other Ruptures 
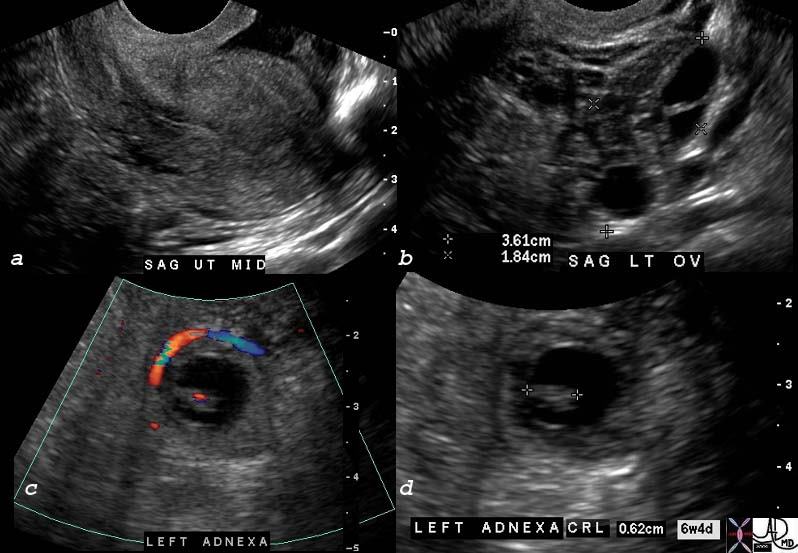
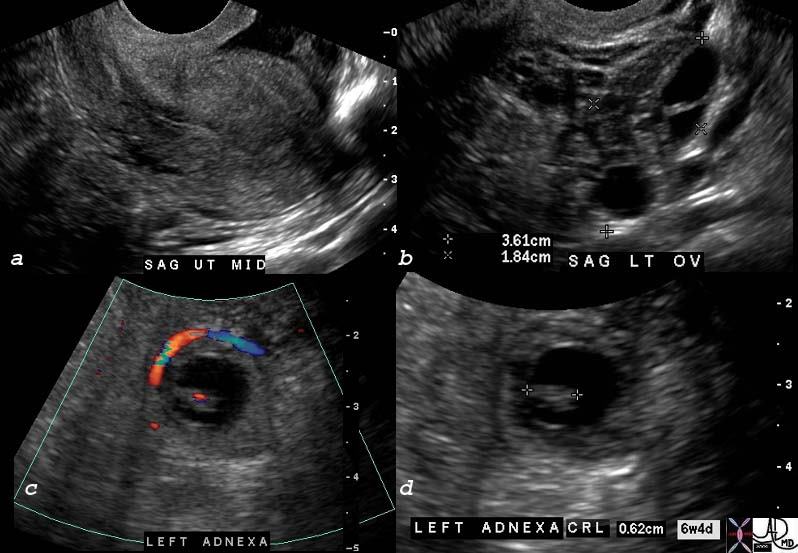
Ectopic pregnancy is another clinical scenario where a combination of rupture and hemorrhage creates an extremely painful and dramatic clinical presentation.
Ectopic Pregnancy
|
|
The ultrasound images from a 32 year old female who presented with severe pelvic pain and a positive HCG. Image (a) shows a normal left ovary with follicles (overlaid in b with lightpink) with fluid later shown to be blood laterally (maroon). Within the left adnexa, a gestational sac surrounded by a ring of blood flow surrounds a fetal pole within the sac (c). The fetal pole has s a beating heart (red dot in c) and measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. The uterus was empty. These findings are consistent with an ectopic pregnancy.
75791c03 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = left ovary complex free fluid probably blood and hemorrhage b = left ovary complex free fluid probably blood and hemorrhage c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01
|

Metabolic Causes 
The metabolic causes of abdominal pain tend to be quite uncommon. One example, diabetic ketoacidosis will cause pain from the acute fatty change of the liver with swelling and capsular distension. Abdominal pain in an Addisonian crisis is also described but the condition is rare. Porphyria, another rare metabolic disorder is a genetic defect resulting in a paucity of the enzyme porphobilinogen-deaminase. The deficiency causes an accumulation of precursors, porphobilinogen and amino-levulinic acid (ALA) which induce an autonomic neuropathy and hence pain.
Functional Causes 
Functional pain is common, complex and often a diagnosis of exclusion. This pain is usually a collection of many diseases that have psychosocial and psycho-cultural elements that are difficult to define and difficult to treat. Many headaches, tension aches, atypical chest pains, vague abdominal pains, irritable bowel syndrome, chronic functional abdominal pain, fibromyalgia, chronic fatigue syndromes fit into this category.
Conclusion 
Pain is a common symptom and can reflect a wide variety of diseases. Inflammatory and mechanical injury are the most common causes of pain. The chemical mediators produced by these insults either lower the threshold to pain or induce pain themselves. Embryology and the distribution of pain receptors account for variations in pain perception. There are nociceptors sensitive to pricking or sharp objects that exist in high concentration in the somatic structures thus producing sharp, well localized pains. On the other hand, nociceptors sensitive to pressure are concentrated in the viscera and produce ill defined dull aches. Cross over situations occur and anybody experiencing gas cramps would agree that their pains are far from dull. In addition, there are many situations where somatic and visceral pains are both present as was described in the case of acute cholecytitis. Neuropathic pain is not as common as the somatic and visceral pain and tends to manifest as chronic pain. Functional pains are common, complex and difficult for both the patient and the caregiver. Often treatment of this pain type is multimodal and requires a combination of experts to direct management.

Spontaneous Subcapsular Hematoma in Pregnancy
|
|
The MRI through the liver is from a 40year old pregnant patient with acute abdominal pain, preeclampsia , elevated liver enzymes, low platelet count, and hemolysis, all characteristic of the HELLP syndrome. The MRI shows a 4 cms subcapsular, non enhancing subcapsular hematoma anterior to the left lobe of the liver that caused acute stretching of the liver capsule and severe abdominal pain.
83209c.81s 40 year female pregnant pregnancy presents with acute abdominal pain MRI shows a sponataneous subcapsular hematoma hemorrhage liver subcapsular hematoma blood HELLP syndrome: “H” for hemolysis (breakage of red blood cells), “EL” for elevated liver enzymes, “LP” for low platelet count complication of preeclampsia and eclampsia (toxemia) of pregnancy, occuring in 25% of these pregnancies. symptoms malaise, nausea and/or vomiting, pain in the upper abdomen. edema Proteinuria Blood pressure may be elevated. Occasionally, coma can result from hypoglycemia Women with a history of HELLP syndrome increased risk for complications in future pregnancies MRI Courtesy Ashley Davidoff MD copyright 2008
|
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] =>
[nodeName] => table
[nodeValue] =>
Spontaneous Subcapsular Hematoma in Pregnancy
The MRI through the liver is from a 40year old pregnant patient with acute abdominal pain, preeclampsia , elevated liver enzymes, low platelet count, and hemolysis, all characteristic of the HELLP syndrome. The MRI shows a 4 cms subcapsular, non enhancing subcapsular hematoma anterior to the left lobe of the liver that caused acute stretching of the liver capsule and severe abdominal pain.
83209c.81s 40 year female pregnant pregnancy presents with acute abdominal pain MRI shows a sponataneous subcapsular hematoma hemorrhage liver subcapsular hematoma blood HELLP syndrome: “H” for hemolysis (breakage of red blood cells), “EL” for elevated liver enzymes, “LP” for low platelet count complication of preeclampsia and eclampsia (toxemia) of pregnancy, occuring in 25% of these pregnancies. symptoms malaise, nausea and/or vomiting, pain in the upper abdomen. edema Proteinuria Blood pressure may be elevated. Occasionally, coma can result from hypoglycemia Women with a history of HELLP syndrome increased risk for complications in future pregnancies MRI Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Spontaneous Subcapsular Hematoma in Pregnancy
The MRI through the liver is from a 40year old pregnant patient with acute abdominal pain, preeclampsia , elevated liver enzymes, low platelet count, and hemolysis, all characteristic of the HELLP syndrome. The MRI shows a 4 cms subcapsular, non enhancing subcapsular hematoma anterior to the left lobe of the liver that caused acute stretching of the liver capsule and severe abdominal pain.
83209c.81s 40 year female pregnant pregnancy presents with acute abdominal pain MRI shows a sponataneous subcapsular hematoma hemorrhage liver subcapsular hematoma blood HELLP syndrome: “H” for hemolysis (breakage of red blood cells), “EL” for elevated liver enzymes, “LP” for low platelet count complication of preeclampsia and eclampsia (toxemia) of pregnancy, occuring in 25% of these pregnancies. symptoms malaise, nausea and/or vomiting, pain in the upper abdomen. edema Proteinuria Blood pressure may be elevated. Occasionally, coma can result from hypoglycemia Women with a history of HELLP syndrome increased risk for complications in future pregnancies MRI Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The MRI through the liver is from a 40year old pregnant patient with acute abdominal pain, preeclampsia , elevated liver enzymes, low platelet count, and hemolysis, all characteristic of the HELLP syndrome. The MRI shows a 4 cms subcapsular, non enhancing subcapsular hematoma anterior to the left lobe of the liver that caused acute stretching of the liver capsule and severe abdominal pain.
83209c.81s 40 year female pregnant pregnancy presents with acute abdominal pain MRI shows a sponataneous subcapsular hematoma hemorrhage liver subcapsular hematoma blood HELLP syndrome: “H” for hemolysis (breakage of red blood cells), “EL” for elevated liver enzymes, “LP” for low platelet count complication of preeclampsia and eclampsia (toxemia) of pregnancy, occuring in 25% of these pregnancies. symptoms malaise, nausea and/or vomiting, pain in the upper abdomen. edema Proteinuria Blood pressure may be elevated. Occasionally, coma can result from hypoglycemia Women with a history of HELLP syndrome increased risk for complications in future pregnancies MRI Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The MRI through the liver is from a 40year old pregnant patient with acute abdominal pain, preeclampsia , elevated liver enzymes, low platelet count, and hemolysis, all characteristic of the HELLP syndrome. The MRI shows a 4 cms subcapsular, non enhancing subcapsular hematoma anterior to the left lobe of the liver that caused acute stretching of the liver capsule and severe abdominal pain.
83209c.81s 40 year female pregnant pregnancy presents with acute abdominal pain MRI shows a sponataneous subcapsular hematoma hemorrhage liver subcapsular hematoma blood HELLP syndrome: “H” for hemolysis (breakage of red blood cells), “EL” for elevated liver enzymes, “LP” for low platelet count complication of preeclampsia and eclampsia (toxemia) of pregnancy, occuring in 25% of these pregnancies. symptoms malaise, nausea and/or vomiting, pain in the upper abdomen. edema Proteinuria Blood pressure may be elevated. Occasionally, coma can result from hypoglycemia Women with a history of HELLP syndrome increased risk for complications in future pregnancies MRI Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Spontaneous Subcapsular Hematoma in Pregnancy
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Spontaneous Subcapsular Hematoma in Pregnancy
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Ectopic Pregnancy
The ultrasound images from a 32 year old female who presented with severe pelvic pain and a positive HCG. Image (a) shows a normal left ovary with follicles (overlaid in b with lightpink) with fluid later shown to be blood laterally (maroon). Within the left adnexa, a gestational sac surrounded by a ring of blood flow surrounds a fetal pole within the sac (c). The fetal pole has s a beating heart (red dot in c) and measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. The uterus was empty. These findings are consistent with an ectopic pregnancy.
75791c03 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = left ovary complex free fluid probably blood and hemorrhage b = left ovary complex free fluid probably blood and hemorrhage c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Ectopic Pregnancy
The ultrasound images from a 32 year old female who presented with severe pelvic pain and a positive HCG. Image (a) shows a normal left ovary with follicles (overlaid in b with lightpink) with fluid later shown to be blood laterally (maroon). Within the left adnexa, a gestational sac surrounded by a ring of blood flow surrounds a fetal pole within the sac (c). The fetal pole has s a beating heart (red dot in c) and measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. The uterus was empty. These findings are consistent with an ectopic pregnancy.
75791c03 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = left ovary complex free fluid probably blood and hemorrhage b = left ovary complex free fluid probably blood and hemorrhage c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The ultrasound images from a 32 year old female who presented with severe pelvic pain and a positive HCG. Image (a) shows a normal left ovary with follicles (overlaid in b with lightpink) with fluid later shown to be blood laterally (maroon). Within the left adnexa, a gestational sac surrounded by a ring of blood flow surrounds a fetal pole within the sac (c). The fetal pole has s a beating heart (red dot in c) and measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. The uterus was empty. These findings are consistent with an ectopic pregnancy.
75791c03 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = left ovary complex free fluid probably blood and hemorrhage b = left ovary complex free fluid probably blood and hemorrhage c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The ultrasound images from a 32 year old female who presented with severe pelvic pain and a positive HCG. Image (a) shows a normal left ovary with follicles (overlaid in b with lightpink) with fluid later shown to be blood laterally (maroon). Within the left adnexa, a gestational sac surrounded by a ring of blood flow surrounds a fetal pole within the sac (c). The fetal pole has s a beating heart (red dot in c) and measures 6.2mm in (d) corresponding to a gestational age of 6 weeks and 4 days. The uterus was empty. These findings are consistent with an ectopic pregnancy.
75791c03 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = left ovary complex free fluid probably blood and hemorrhage b = left ovary complex free fluid probably blood and hemorrhage c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Ectopic Pregnancy
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Ectopic Pregnancy
)
https://beta.thecommonvein.net/wp-content/uploads/2023/06/75792c01.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/75791c03.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/75791c01.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/75791.jpg
http://www.thecommonvein.net/media/75791c03.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Football Player with Traumatic Bleed into the Greater Abdomen
This football player presented severe abdominal pain in the right upper quadrant pain with peritonism following a football game. The pain was of such concern that he was taken to the OR where hemorrhage into the greater omentum was diagnosed. In this instance pain was presumably caused by blood acting on chemoreceptors in the omentum.
44692c.8s young college football player who presents with RUQ pain and fever with normal gallbadder by USscan fx mesentery greater omentum transverse colon large bowel RUQ fx induration dx hemorrhagic bleeding of right sided component of colonic greater omentum due to traumatic injury surgical proof CTscan coronal ddx appendagitis Courtesy Ashley Davidoff MD 44692 44694 gastrocolic ligament lesser omentum copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Football Player with Traumatic Bleed into the Greater Abdomen
This football player presented severe abdominal pain in the right upper quadrant pain with peritonism following a football game. The pain was of such concern that he was taken to the OR where hemorrhage into the greater omentum was diagnosed. In this instance pain was presumably caused by blood acting on chemoreceptors in the omentum.
44692c.8s young college football player who presents with RUQ pain and fever with normal gallbadder by USscan fx mesentery greater omentum transverse colon large bowel RUQ fx induration dx hemorrhagic bleeding of right sided component of colonic greater omentum due to traumatic injury surgical proof CTscan coronal ddx appendagitis Courtesy Ashley Davidoff MD 44692 44694 gastrocolic ligament lesser omentum copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
This football player presented severe abdominal pain in the right upper quadrant pain with peritonism following a football game. The pain was of such concern that he was taken to the OR where hemorrhage into the greater omentum was diagnosed. In this instance pain was presumably caused by blood acting on chemoreceptors in the omentum.
44692c.8s young college football player who presents with RUQ pain and fever with normal gallbadder by USscan fx mesentery greater omentum transverse colon large bowel RUQ fx induration dx hemorrhagic bleeding of right sided component of colonic greater omentum due to traumatic injury surgical proof CTscan coronal ddx appendagitis Courtesy Ashley Davidoff MD 44692 44694 gastrocolic ligament lesser omentum copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
This football player presented severe abdominal pain in the right upper quadrant pain with peritonism following a football game. The pain was of such concern that he was taken to the OR where hemorrhage into the greater omentum was diagnosed. In this instance pain was presumably caused by blood acting on chemoreceptors in the omentum.
44692c.8s young college football player who presents with RUQ pain and fever with normal gallbadder by USscan fx mesentery greater omentum transverse colon large bowel RUQ fx induration dx hemorrhagic bleeding of right sided component of colonic greater omentum due to traumatic injury surgical proof CTscan coronal ddx appendagitis Courtesy Ashley Davidoff MD 44692 44694 gastrocolic ligament lesser omentum copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Football Player with Traumatic Bleed into the Greater Abdomen
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Football Player with Traumatic Bleed into the Greater Abdomen
)
https://beta.thecommonvein.net/wp-content/uploads/2023/06/44692c.8s.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/44694.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/44692.jpg
http://www.thecommonvein.net/media/44692c.8s.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Pulmonary Hemorrhage Extensive Disease – No Pain
This 20 year old male patient presented with hemoptysis and renal failure, and following renal biopsy a diagnosis of Wegener’s granulomatosis was made. The CT shows extensive pulmonary hemorrhage characterized by white nodular infiltrates, but there was nopain associated with the extensive pulmonary findings.
47711c01 20 year old male presents with hemoptysis and renal failure chest lungs upper lobes lower lobes infiltrates acinar infiltrates fluffy infiltrates almost symmetrical fx bilateral pulmonary infiltrates renal biopsy dx Wegener’s granulomatosis with pulmonary hemorrhage blood character CTscan Daviddoff MD 47711c02
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Pulmonary Hemorrhage Extensive Disease – No Pain
This 20 year old male patient presented with hemoptysis and renal failure, and following renal biopsy a diagnosis of Wegener’s granulomatosis was made. The CT shows extensive pulmonary hemorrhage characterized by white nodular infiltrates, but there was nopain associated with the extensive pulmonary findings.
47711c01 20 year old male presents with hemoptysis and renal failure chest lungs upper lobes lower lobes infiltrates acinar infiltrates fluffy infiltrates almost symmetrical fx bilateral pulmonary infiltrates renal biopsy dx Wegener’s granulomatosis with pulmonary hemorrhage blood character CTscan Daviddoff MD 47711c02
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
This 20 year old male patient presented with hemoptysis and renal failure, and following renal biopsy a diagnosis of Wegener’s granulomatosis was made. The CT shows extensive pulmonary hemorrhage characterized by white nodular infiltrates, but there was nopain associated with the extensive pulmonary findings.
47711c01 20 year old male presents with hemoptysis and renal failure chest lungs upper lobes lower lobes infiltrates acinar infiltrates fluffy infiltrates almost symmetrical fx bilateral pulmonary infiltrates renal biopsy dx Wegener’s granulomatosis with pulmonary hemorrhage blood character CTscan Daviddoff MD 47711c02
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
This 20 year old male patient presented with hemoptysis and renal failure, and following renal biopsy a diagnosis of Wegener’s granulomatosis was made. The CT shows extensive pulmonary hemorrhage characterized by white nodular infiltrates, but there was nopain associated with the extensive pulmonary findings.
47711c01 20 year old male presents with hemoptysis and renal failure chest lungs upper lobes lower lobes infiltrates acinar infiltrates fluffy infiltrates almost symmetrical fx bilateral pulmonary infiltrates renal biopsy dx Wegener’s granulomatosis with pulmonary hemorrhage blood character CTscan Daviddoff MD 47711c02
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Pulmonary Hemorrhage Extensive Disease – No Pain
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Pulmonary Hemorrhage Extensive Disease – No Pain
)
https://beta.thecommonvein.net/wp-content/uploads/2023/06/47711c02.jpg https://beta.thecommonvein.net/wp-content/uploads/2023/06/47711c01.jpg
http://www.thecommonvein.net/search/assets/47711c01.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Type A Dissection
The CT image shows a dissection in the ascending and descending aorta. The lumen consists of the smaller true lumen (bright red) and the false lumen (larger with dull red) The patient presented with classical severe chest pain that radiated to the back. The involvement of the ascending aorta make s it a type A dissection and therefore treatment requires surgical repair. In this patient however the dissection extended to the descending aorta as well. Either way a type A dissection requires surgery.
20448c03.8s descending aorta ascending aorta fx dissection fx crescent dx aortic dissection type A CTscan Courtesy Ashley Davidoff MD DB
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Type A Dissection
The CT image shows a dissection in the ascending and descending aorta. The lumen consists of the smaller true lumen (bright red) and the false lumen (larger with dull red) The patient presented with classical severe chest pain that radiated to the back. The involvement of the ascending aorta make s it a type A dissection and therefore treatment requires surgical repair. In this patient however the dissection extended to the descending aorta as well. Either way a type A dissection requires surgery.
20448c03.8s descending aorta ascending aorta fx dissection fx crescent dx aortic dissection type A CTscan Courtesy Ashley Davidoff MD DB
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The CT image shows a dissection in the ascending and descending aorta. The lumen consists of the smaller true lumen (bright red) and the false lumen (larger with dull red) The patient presented with classical severe chest pain that radiated to the back. The involvement of the ascending aorta make s it a type A dissection and therefore treatment requires surgical repair. In this patient however the dissection extended to the descending aorta as well. Either way a type A dissection requires surgery.
20448c03.8s descending aorta ascending aorta fx dissection fx crescent dx aortic dissection type A CTscan Courtesy Ashley Davidoff MD DB
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The CT image shows a dissection in the ascending and descending aorta. The lumen consists of the smaller true lumen (bright red) and the false lumen (larger with dull red) The patient presented with classical severe chest pain that radiated to the back. The involvement of the ascending aorta make s it a type A dissection and therefore treatment requires surgical repair. In this patient however the dissection extended to the descending aorta as well. Either way a type A dissection requires surgery.
20448c03.8s descending aorta ascending aorta fx dissection fx crescent dx aortic dissection type A CTscan Courtesy Ashley Davidoff MD DB
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Type A Dissection
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Type A Dissection
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Fatal Acute Dissection
This pathological specimen shows an aortic dissection (maroon blood clot in wall) starting at the root of the aorta and extending across the arch and into the descending portion. The blood is in the false lumen. The blood that was in the true lumen has been removed..
Courtesy Henri Cuenoud MD 13421 code CVS thorax AO aorta dissection grosspathology
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Fatal Acute Dissection
This pathological specimen shows an aortic dissection (maroon blood clot in wall) starting at the root of the aorta and extending across the arch and into the descending portion. The blood is in the false lumen. The blood that was in the true lumen has been removed..
Courtesy Henri Cuenoud MD 13421 code CVS thorax AO aorta dissection grosspathology
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
This pathological specimen shows an aortic dissection (maroon blood clot in wall) starting at the root of the aorta and extending across the arch and into the descending portion. The blood is in the false lumen. The blood that was in the true lumen has been removed..
Courtesy Henri Cuenoud MD 13421 code CVS thorax AO aorta dissection grosspathology
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
This pathological specimen shows an aortic dissection (maroon blood clot in wall) starting at the root of the aorta and extending across the arch and into the descending portion. The blood is in the false lumen. The blood that was in the true lumen has been removed..
Courtesy Henri Cuenoud MD 13421 code CVS thorax AO aorta dissection grosspathology
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Fatal Acute Dissection
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Fatal Acute Dissection
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Ruptured Abdominal Aortic Aneurysm
The abdominal CT is from an elderly patient who presents with acute severe back pain and pulsatile abdominal mass. Findings include an abdominal aortic aneurysm (bright red ) and a retroperitoneal bleed toward the right side where there has been a rapid and painful accumulation of blood (maroon) that expands the retroperitoneum and invades and expands the right psoas muscle. This patient suffered from a rupture of an abdominal aortic aneurysm
16548c01 abdominal aorta rupture psoas muscle retroperitoneeum aneurysm AAA back pain CTscan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Ruptured Abdominal Aortic Aneurysm
The abdominal CT is from an elderly patient who presents with acute severe back pain and pulsatile abdominal mass. Findings include an abdominal aortic aneurysm (bright red ) and a retroperitoneal bleed toward the right side where there has been a rapid and painful accumulation of blood (maroon) that expands the retroperitoneum and invades and expands the right psoas muscle. This patient suffered from a rupture of an abdominal aortic aneurysm
16548c01 abdominal aorta rupture psoas muscle retroperitoneeum aneurysm AAA back pain CTscan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => The abdominal CT is from an elderly patient who presents with acute severe back pain and pulsatile abdominal mass. Findings include an abdominal aortic aneurysm (bright red ) and a retroperitoneal bleed toward the right side where there has been a rapid and painful accumulation of blood (maroon) that expands the retroperitoneum and invades and expands the right psoas muscle. This patient suffered from a rupture of an abdominal aortic aneurysm
16548c01 abdominal aorta rupture psoas muscle retroperitoneeum aneurysm AAA back pain CTscan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => The abdominal CT is from an elderly patient who presents with acute severe back pain and pulsatile abdominal mass. Findings include an abdominal aortic aneurysm (bright red ) and a retroperitoneal bleed toward the right side where there has been a rapid and painful accumulation of blood (maroon) that expands the retroperitoneum and invades and expands the right psoas muscle. This patient suffered from a rupture of an abdominal aortic aneurysm
16548c01 abdominal aorta rupture psoas muscle retroperitoneeum aneurysm AAA back pain CTscan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Ruptured Abdominal Aortic Aneurysm
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Ruptured Abdominal Aortic Aneurysm
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Normal and Life Threatening
These two head CT’s are from two different patients who both presented with severe headaches. The first patient (a,c) had a normal study and the headache may have been caused by migraine, cluster, or tension headaches for example. Although these headaches create significant morbidity they are relatively benign in that they are treatable. The second patient (b,d) had a life threatening subarchnoid hemorrhage due to a ruptured aneurysm characterized by the white hemorrhage in the sulci (b) and within the subarachnoid spaces surrounding the midbrain and other structures.(d) It is not practical to perform a CT on every patient who presents with a headache, since it is a very common condition. On the other hand one does not want to miss a life threatening condition that is potentially treatable. Meticullous clinical acumen and prudent clinical judgement is therefore necessary to direct management of patients with headaches and with patients who complain of pain.
The dura has the largest number of nociceptors of the meninges. In acute aneurysmal rupture, the severe pain is caused by stretching and distortionof the blood vessels that are accompanied by the nerves
76059c01 52 male headache neurological deficit normal abnormal brain cerebrum subarachnoid blood subarachnoid hemorrhage Sylvian fissures midbrain basal cisterns cerebellar folia circle of Willis cerebellum sulcus sulci ambient cisterns 4th ventricle dx probable rupture of basilar tip aneurysm berry aneurysm CTscan Courtesy Ashley Davidoff MD 76059c01 76059c02 76059c03
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Normal and Life Threatening
These two head CT’s are from two different patients who both presented with severe headaches. The first patient (a,c) had a normal study and the headache may have been caused by migraine, cluster, or tension headaches for example. Although these headaches create significant morbidity they are relatively benign in that they are treatable. The second patient (b,d) had a life threatening subarchnoid hemorrhage due to a ruptured aneurysm characterized by the white hemorrhage in the sulci (b) and within the subarachnoid spaces surrounding the midbrain and other structures.(d) It is not practical to perform a CT on every patient who presents with a headache, since it is a very common condition. On the other hand one does not want to miss a life threatening condition that is potentially treatable. Meticullous clinical acumen and prudent clinical judgement is therefore necessary to direct management of patients with headaches and with patients who complain of pain.
The dura has the largest number of nociceptors of the meninges. In acute aneurysmal rupture, the severe pain is caused by stretching and distortionof the blood vessels that are accompanied by the nerves
76059c01 52 male headache neurological deficit normal abnormal brain cerebrum subarachnoid blood subarachnoid hemorrhage Sylvian fissures midbrain basal cisterns cerebellar folia circle of Willis cerebellum sulcus sulci ambient cisterns 4th ventricle dx probable rupture of basilar tip aneurysm berry aneurysm CTscan Courtesy Ashley Davidoff MD 76059c01 76059c02 76059c03
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
These two head CT’s are from two different patients who both presented with severe headaches. The first patient (a,c) had a normal study and the headache may have been caused by migraine, cluster, or tension headaches for example. Although these headaches create significant morbidity they are relatively benign in that they are treatable. The second patient (b,d) had a life threatening subarchnoid hemorrhage due to a ruptured aneurysm characterized by the white hemorrhage in the sulci (b) and within the subarachnoid spaces surrounding the midbrain and other structures.(d) It is not practical to perform a CT on every patient who presents with a headache, since it is a very common condition. On the other hand one does not want to miss a life threatening condition that is potentially treatable. Meticullous clinical acumen and prudent clinical judgement is therefore necessary to direct management of patients with headaches and with patients who complain of pain.
The dura has the largest number of nociceptors of the meninges. In acute aneurysmal rupture, the severe pain is caused by stretching and distortionof the blood vessels that are accompanied by the nerves
76059c01 52 male headache neurological deficit normal abnormal brain cerebrum subarachnoid blood subarachnoid hemorrhage Sylvian fissures midbrain basal cisterns cerebellar folia circle of Willis cerebellum sulcus sulci ambient cisterns 4th ventricle dx probable rupture of basilar tip aneurysm berry aneurysm CTscan Courtesy Ashley Davidoff MD 76059c01 76059c02 76059c03
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
These two head CT’s are from two different patients who both presented with severe headaches. The first patient (a,c) had a normal study and the headache may have been caused by migraine, cluster, or tension headaches for example. Although these headaches create significant morbidity they are relatively benign in that they are treatable. The second patient (b,d) had a life threatening subarchnoid hemorrhage due to a ruptured aneurysm characterized by the white hemorrhage in the sulci (b) and within the subarachnoid spaces surrounding the midbrain and other structures.(d) It is not practical to perform a CT on every patient who presents with a headache, since it is a very common condition. On the other hand one does not want to miss a life threatening condition that is potentially treatable. Meticullous clinical acumen and prudent clinical judgement is therefore necessary to direct management of patients with headaches and with patients who complain of pain.
The dura has the largest number of nociceptors of the meninges. In acute aneurysmal rupture, the severe pain is caused by stretching and distortionof the blood vessels that are accompanied by the nerves
76059c01 52 male headache neurological deficit normal abnormal brain cerebrum subarachnoid blood subarachnoid hemorrhage Sylvian fissures midbrain basal cisterns cerebellar folia circle of Willis cerebellum sulcus sulci ambient cisterns 4th ventricle dx probable rupture of basilar tip aneurysm berry aneurysm CTscan Courtesy Ashley Davidoff MD 76059c01 76059c02 76059c03
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Normal and Life Threatening
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Normal and Life Threatening
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Severe Headache Awaking the Patient from Sleep
Pain that awakens a patient from sleep needs special attention since it excludes the supratentorial events of pain, implies severe physical pain, and it may herald a catastrophic event.
89081pd04b02.8s pain headache sleep woken awakened from sleep worst pain in my life headache 10 out of 10 ruptured berry aneurysm bleed blood hemorrhage meninges somatic Davidoff art copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Severe Headache Awaking the Patient from Sleep
Pain that awakens a patient from sleep needs special attention since it excludes the supratentorial events of pain, implies severe physical pain, and it may herald a catastrophic event.
89081pd04b02.8s pain headache sleep woken awakened from sleep worst pain in my life headache 10 out of 10 ruptured berry aneurysm bleed blood hemorrhage meninges somatic Davidoff art copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Pain that awakens a patient from sleep needs special attention since it excludes the supratentorial events of pain, implies severe physical pain, and it may herald a catastrophic event.
89081pd04b02.8s pain headache sleep woken awakened from sleep worst pain in my life headache 10 out of 10 ruptured berry aneurysm bleed blood hemorrhage meninges somatic Davidoff art copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Pain that awakens a patient from sleep needs special attention since it excludes the supratentorial events of pain, implies severe physical pain, and it may herald a catastrophic event.
89081pd04b02.8s pain headache sleep woken awakened from sleep worst pain in my life headache 10 out of 10 ruptured berry aneurysm bleed blood hemorrhage meninges somatic Davidoff art copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Severe Headache Awaking the Patient from Sleep
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Severe Headache Awaking the Patient from Sleep
)
https://beta.thecommonvein.net/wp-content/uploads/2023/08/89081p.jpg
http://www.thecommonvein.net/media/89081pd04b02.8s_1.jpg
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Coronary Stenosis
The coronary angiogram in the LAO projection shows a severe proximal stenosis (about 90%) of the circumflex with some post stenotic dilatation. The second image has a green overlay indicating the region of disease with the post stenotic dilatation. The narrowing causes angina due to poor oxygen supply and resulting depletion of high energy compounds and acidosis due to anaerobic production of lactate, hydrogen ions, and adenosine.
Courtesy Ashley Davidoff MD. 07023c code heart artery coronary circumflex stenosis atherosclerosis imaging radiology angiography overlay
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Coronary Stenosis
The coronary angiogram in the LAO projection shows a severe proximal stenosis (about 90%) of the circumflex with some post stenotic dilatation. The second image has a green overlay indicating the region of disease with the post stenotic dilatation. The narrowing causes angina due to poor oxygen supply and resulting depletion of high energy compounds and acidosis due to anaerobic production of lactate, hydrogen ions, and adenosine.
Courtesy Ashley Davidoff MD. 07023c code heart artery coronary circumflex stenosis atherosclerosis imaging radiology angiography overlay
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The coronary angiogram in the LAO projection shows a severe proximal stenosis (about 90%) of the circumflex with some post stenotic dilatation. The second image has a green overlay indicating the region of disease with the post stenotic dilatation. The narrowing causes angina due to poor oxygen supply and resulting depletion of high energy compounds and acidosis due to anaerobic production of lactate, hydrogen ions, and adenosine.
Courtesy Ashley Davidoff MD. 07023c code heart artery coronary circumflex stenosis atherosclerosis imaging radiology angiography overlay
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The coronary angiogram in the LAO projection shows a severe proximal stenosis (about 90%) of the circumflex with some post stenotic dilatation. The second image has a green overlay indicating the region of disease with the post stenotic dilatation. The narrowing causes angina due to poor oxygen supply and resulting depletion of high energy compounds and acidosis due to anaerobic production of lactate, hydrogen ions, and adenosine.
Courtesy Ashley Davidoff MD. 07023c code heart artery coronary circumflex stenosis atherosclerosis imaging radiology angiography overlay
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Coronary Stenosis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Coronary Stenosis
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Chemical Nociceptors
The diagram illustrates the many chemical factors, each represented in different color and different shapes, that can incite the chemical nociceptors. The hydrogen ion and acidic PH is a common stimulant of these receptors.
87559pb04b02b02b02.8s nociceptors chemical receptors free nerve endings trees in the body hydrogen ion algogenic substances autocids substance C K+ kinins interleukins adenosine histamine leukotrines H+ Davidoff art copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Chemical Nociceptors
The diagram illustrates the many chemical factors, each represented in different color and different shapes, that can incite the chemical nociceptors. The hydrogen ion and acidic PH is a common stimulant of these receptors.
87559pb04b02b02b02.8s nociceptors chemical receptors free nerve endings trees in the body hydrogen ion algogenic substances autocids substance C K+ kinins interleukins adenosine histamine leukotrines H+ Davidoff art copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The diagram illustrates the many chemical factors, each represented in different color and different shapes, that can incite the chemical nociceptors. The hydrogen ion and acidic PH is a common stimulant of these receptors.
87559pb04b02b02b02.8s nociceptors chemical receptors free nerve endings trees in the body hydrogen ion algogenic substances autocids substance C K+ kinins interleukins adenosine histamine leukotrines H+ Davidoff art copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The diagram illustrates the many chemical factors, each represented in different color and different shapes, that can incite the chemical nociceptors. The hydrogen ion and acidic PH is a common stimulant of these receptors.
87559pb04b02b02b02.8s nociceptors chemical receptors free nerve endings trees in the body hydrogen ion algogenic substances autocids substance C K+ kinins interleukins adenosine histamine leukotrines H+ Davidoff art copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Chemical Nociceptors
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Chemical Nociceptors
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Severe and Painful Trauma
The post operative angiogram of the hand is one of the most painful X-rays I have experienced in my career and the image is older than 30 years. The exact history eludes me but there has been obvious traumatic injury to the hand with multiple fractures (black arrows), a transverse skin incision that contains a broad band of air (white arrow), with probable debridement of the severely injured metacarpal row, and extensive pinning and wiring of the thumb following surgical trauma. The combination of the large somatic sensory nociceptor supply to the hand, with the extensive skin, bone, and tissue damage, creates a scenario of extreme pain. It is difficult to perceive the extent of the pain that this poor patient went through. The remarkable feature is the maintenance of blood supply to the hand despite the extensive injury to harder but less pliable bones.
artery bone trauma fracture post op pain artery digital trauma angiography angiogram fractures Courtesy Ashley DAvidoff MD copyright 2008 17496c02.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Severe and Painful Trauma
The post operative angiogram of the hand is one of the most painful X-rays I have experienced in my career and the image is older than 30 years. The exact history eludes me but there has been obvious traumatic injury to the hand with multiple fractures (black arrows), a transverse skin incision that contains a broad band of air (white arrow), with probable debridement of the severely injured metacarpal row, and extensive pinning and wiring of the thumb following surgical trauma. The combination of the large somatic sensory nociceptor supply to the hand, with the extensive skin, bone, and tissue damage, creates a scenario of extreme pain. It is difficult to perceive the extent of the pain that this poor patient went through. The remarkable feature is the maintenance of blood supply to the hand despite the extensive injury to harder but less pliable bones.
artery bone trauma fracture post op pain artery digital trauma angiography angiogram fractures Courtesy Ashley DAvidoff MD copyright 2008 17496c02.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The post operative angiogram of the hand is one of the most painful X-rays I have experienced in my career and the image is older than 30 years. The exact history eludes me but there has been obvious traumatic injury to the hand with multiple fractures (black arrows), a transverse skin incision that contains a broad band of air (white arrow), with probable debridement of the severely injured metacarpal row, and extensive pinning and wiring of the thumb following surgical trauma. The combination of the large somatic sensory nociceptor supply to the hand, with the extensive skin, bone, and tissue damage, creates a scenario of extreme pain. It is difficult to perceive the extent of the pain that this poor patient went through. The remarkable feature is the maintenance of blood supply to the hand despite the extensive injury to harder but less pliable bones.
artery bone trauma fracture post op pain artery digital trauma angiography angiogram fractures Courtesy Ashley DAvidoff MD copyright 2008 17496c02.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The post operative angiogram of the hand is one of the most painful X-rays I have experienced in my career and the image is older than 30 years. The exact history eludes me but there has been obvious traumatic injury to the hand with multiple fractures (black arrows), a transverse skin incision that contains a broad band of air (white arrow), with probable debridement of the severely injured metacarpal row, and extensive pinning and wiring of the thumb following surgical trauma. The combination of the large somatic sensory nociceptor supply to the hand, with the extensive skin, bone, and tissue damage, creates a scenario of extreme pain. It is difficult to perceive the extent of the pain that this poor patient went through. The remarkable feature is the maintenance of blood supply to the hand despite the extensive injury to harder but less pliable bones.
artery bone trauma fracture post op pain artery digital trauma angiography angiogram fractures Courtesy Ashley DAvidoff MD copyright 2008 17496c02.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Severe and Painful Trauma
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Severe and Painful Trauma
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Small Bowel Obstruction with Distension
Inciting the Mechanical and Pressure Nociceptors
The plain film of the abdomen shows dilated loops of small bowel associated with a paucity of gas in the decompressed large bowel. These findings are consistent with small bowel obstruction and were associated with diffuse abdominal aching pain, nausea and vomitting.
00554 small bowel fx dilated fx enlarged dx SBO obstruction plainfilm Courtesy Ashley Davidoff MD DB
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Small Bowel Obstruction with Distension
Inciting the Mechanical and Pressure Nociceptors
The plain film of the abdomen shows dilated loops of small bowel associated with a paucity of gas in the decompressed large bowel. These findings are consistent with small bowel obstruction and were associated with diffuse abdominal aching pain, nausea and vomitting.
00554 small bowel fx dilated fx enlarged dx SBO obstruction plainfilm Courtesy Ashley Davidoff MD DB
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The plain film of the abdomen shows dilated loops of small bowel associated with a paucity of gas in the decompressed large bowel. These findings are consistent with small bowel obstruction and were associated with diffuse abdominal aching pain, nausea and vomitting.
00554 small bowel fx dilated fx enlarged dx SBO obstruction plainfilm Courtesy Ashley Davidoff MD DB
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The plain film of the abdomen shows dilated loops of small bowel associated with a paucity of gas in the decompressed large bowel. These findings are consistent with small bowel obstruction and were associated with diffuse abdominal aching pain, nausea and vomitting.
00554 small bowel fx dilated fx enlarged dx SBO obstruction plainfilm Courtesy Ashley Davidoff MD DB
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Small Bowel Obstruction with Distension
Inciting the Mechanical and Pressure Nociceptors
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Small Bowel Obstruction with Distension
Inciting the Mechanical and Pressure Nociceptors
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Small Things Can Cause Big Packages of Pain
The worst pain of this patients life was caused by a 3mms stone in the right distal ureter seen on this non-contrast CT, as a white speck in image d. In image a, a similar stone remains in the kidney, (arrow) while image b shows mild hydronephrosis, and image c shows hydroureter (arrow).
83149c02.8s right flank pain kidney renal pelvis ureter stone ureterolithiasis hydronephrosis pain delayed nephrogram CTscan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Small Things Can Cause Big Packages of Pain
The worst pain of this patients life was caused by a 3mms stone in the right distal ureter seen on this non-contrast CT, as a white speck in image d. In image a, a similar stone remains in the kidney, (arrow) while image b shows mild hydronephrosis, and image c shows hydroureter (arrow).
83149c02.8s right flank pain kidney renal pelvis ureter stone ureterolithiasis hydronephrosis pain delayed nephrogram CTscan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The worst pain of this patients life was caused by a 3mms stone in the right distal ureter seen on this non-contrast CT, as a white speck in image d. In image a, a similar stone remains in the kidney, (arrow) while image b shows mild hydronephrosis, and image c shows hydroureter (arrow).
83149c02.8s right flank pain kidney renal pelvis ureter stone ureterolithiasis hydronephrosis pain delayed nephrogram CTscan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The worst pain of this patients life was caused by a 3mms stone in the right distal ureter seen on this non-contrast CT, as a white speck in image d. In image a, a similar stone remains in the kidney, (arrow) while image b shows mild hydronephrosis, and image c shows hydroureter (arrow).
83149c02.8s right flank pain kidney renal pelvis ureter stone ureterolithiasis hydronephrosis pain delayed nephrogram CTscan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Small Things Can Cause Big Packages of Pain
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Small Things Can Cause Big Packages of Pain
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Pressure Nociceptors
The mechanical pressure sensitive nociceptors are dominantly located in the organs and are responsible for sensing pressure changes. The diagram shows a wave of increased pressure (pale yellow) impinging on the free nerve endings of the pressure receptors, with red nerve endings being stimulated by the pressure.
87559pb04b02b11.8s pressure receptors nociceptors mechonoreceptors free nerve endings trees in the body Davidoff art copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Pressure Nociceptors
The mechanical pressure sensitive nociceptors are dominantly located in the organs and are responsible for sensing pressure changes. The diagram shows a wave of increased pressure (pale yellow) impinging on the free nerve endings of the pressure receptors, with red nerve endings being stimulated by the pressure.
87559pb04b02b11.8s pressure receptors nociceptors mechonoreceptors free nerve endings trees in the body Davidoff art copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The mechanical pressure sensitive nociceptors are dominantly located in the organs and are responsible for sensing pressure changes. The diagram shows a wave of increased pressure (pale yellow) impinging on the free nerve endings of the pressure receptors, with red nerve endings being stimulated by the pressure.
87559pb04b02b11.8s pressure receptors nociceptors mechonoreceptors free nerve endings trees in the body Davidoff art copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The mechanical pressure sensitive nociceptors are dominantly located in the organs and are responsible for sensing pressure changes. The diagram shows a wave of increased pressure (pale yellow) impinging on the free nerve endings of the pressure receptors, with red nerve endings being stimulated by the pressure.
87559pb04b02b11.8s pressure receptors nociceptors mechonoreceptors free nerve endings trees in the body Davidoff art copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Pressure Nociceptors
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Pressure Nociceptors
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Cecal Carcinoma with Peritoneal Involvement
In this case the 77year old female patient presents with right lower quadrant pain. The CTscan shows a napkin ring thickening (green) surrounding the region of the cecum subsequently proven to be carcinoma. When restricted to the cecum alone the cecal carcinoma tends to be silent since there is neither significant distension nor peritoneal involvement to incite any nociceptors. These patients usually present when complications such as anemia or obstruction surface. In this patient the neoplasm incited an inflammatory reaction in the surrounding fat (pale see through red) and peritoneum (bright red line) witnessed as a subtle thickening of the peritoneum. This was sufficient to stimulate the nociceptors and incite pain.
83037c03.8s 70 F presents with right lower quadrant pain RLQ colon cecum mass colon carcinoma napkin ring peritoneum peritonism somatic pain induration CTscan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Cecal Carcinoma with Peritoneal Involvement
In this case the 77year old female patient presents with right lower quadrant pain. The CTscan shows a napkin ring thickening (green) surrounding the region of the cecum subsequently proven to be carcinoma. When restricted to the cecum alone the cecal carcinoma tends to be silent since there is neither significant distension nor peritoneal involvement to incite any nociceptors. These patients usually present when complications such as anemia or obstruction surface. In this patient the neoplasm incited an inflammatory reaction in the surrounding fat (pale see through red) and peritoneum (bright red line) witnessed as a subtle thickening of the peritoneum. This was sufficient to stimulate the nociceptors and incite pain.
83037c03.8s 70 F presents with right lower quadrant pain RLQ colon cecum mass colon carcinoma napkin ring peritoneum peritonism somatic pain induration CTscan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
In this case the 77year old female patient presents with right lower quadrant pain. The CTscan shows a napkin ring thickening (green) surrounding the region of the cecum subsequently proven to be carcinoma. When restricted to the cecum alone the cecal carcinoma tends to be silent since there is neither significant distension nor peritoneal involvement to incite any nociceptors. These patients usually present when complications such as anemia or obstruction surface. In this patient the neoplasm incited an inflammatory reaction in the surrounding fat (pale see through red) and peritoneum (bright red line) witnessed as a subtle thickening of the peritoneum. This was sufficient to stimulate the nociceptors and incite pain.
83037c03.8s 70 F presents with right lower quadrant pain RLQ colon cecum mass colon carcinoma napkin ring peritoneum peritonism somatic pain induration CTscan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
In this case the 77year old female patient presents with right lower quadrant pain. The CTscan shows a napkin ring thickening (green) surrounding the region of the cecum subsequently proven to be carcinoma. When restricted to the cecum alone the cecal carcinoma tends to be silent since there is neither significant distension nor peritoneal involvement to incite any nociceptors. These patients usually present when complications such as anemia or obstruction surface. In this patient the neoplasm incited an inflammatory reaction in the surrounding fat (pale see through red) and peritoneum (bright red line) witnessed as a subtle thickening of the peritoneum. This was sufficient to stimulate the nociceptors and incite pain.
83037c03.8s 70 F presents with right lower quadrant pain RLQ colon cecum mass colon carcinoma napkin ring peritoneum peritonism somatic pain induration CTscan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Cecal Carcinoma with Peritoneal Involvement
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Cecal Carcinoma with Peritoneal Involvement
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Hepatocellular Carcinoma
Space Occupation, Capsular Involvement and Neuropathic Pain
The pathological specimen from a patient who succumbed to a large hepatocellular carcinoma shows a large space occupying tumor. Pain is theoretically induced by the tumor from a variety of sources. It may originate from the involvement of the tumor that extends to the periphery and capsule of the liver with its somatic nociceptors, from around the neurovascular bundles within the portal triad and its nociceptor component, or from chemical released by the tissue destruction expected by the tumor on surrounding structures. Despite the potential for extreme pain in this situation, the response in each patient is quite variable. For some patients, the pain in this scenario may be more of an ache or discomfort rather than severe incapacitating pain that one may expect from this giant tumor.
24008 liver fx mass portal vein fx invasion satellite nodule multicentric dx hepatocellular carcinoma hepatoma HCC grosspathology Courtesy Barbara Banner MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Hepatocellular Carcinoma
Space Occupation, Capsular Involvement and Neuropathic Pain
The pathological specimen from a patient who succumbed to a large hepatocellular carcinoma shows a large space occupying tumor. Pain is theoretically induced by the tumor from a variety of sources. It may originate from the involvement of the tumor that extends to the periphery and capsule of the liver with its somatic nociceptors, from around the neurovascular bundles within the portal triad and its nociceptor component, or from chemical released by the tissue destruction expected by the tumor on surrounding structures. Despite the potential for extreme pain in this situation, the response in each patient is quite variable. For some patients, the pain in this scenario may be more of an ache or discomfort rather than severe incapacitating pain that one may expect from this giant tumor.
24008 liver fx mass portal vein fx invasion satellite nodule multicentric dx hepatocellular carcinoma hepatoma HCC grosspathology Courtesy Barbara Banner MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The pathological specimen from a patient who succumbed to a large hepatocellular carcinoma shows a large space occupying tumor. Pain is theoretically induced by the tumor from a variety of sources. It may originate from the involvement of the tumor that extends to the periphery and capsule of the liver with its somatic nociceptors, from around the neurovascular bundles within the portal triad and its nociceptor component, or from chemical released by the tissue destruction expected by the tumor on surrounding structures. Despite the potential for extreme pain in this situation, the response in each patient is quite variable. For some patients, the pain in this scenario may be more of an ache or discomfort rather than severe incapacitating pain that one may expect from this giant tumor.
24008 liver fx mass portal vein fx invasion satellite nodule multicentric dx hepatocellular carcinoma hepatoma HCC grosspathology Courtesy Barbara Banner MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The pathological specimen from a patient who succumbed to a large hepatocellular carcinoma shows a large space occupying tumor. Pain is theoretically induced by the tumor from a variety of sources. It may originate from the involvement of the tumor that extends to the periphery and capsule of the liver with its somatic nociceptors, from around the neurovascular bundles within the portal triad and its nociceptor component, or from chemical released by the tissue destruction expected by the tumor on surrounding structures. Despite the potential for extreme pain in this situation, the response in each patient is quite variable. For some patients, the pain in this scenario may be more of an ache or discomfort rather than severe incapacitating pain that one may expect from this giant tumor.
24008 liver fx mass portal vein fx invasion satellite nodule multicentric dx hepatocellular carcinoma hepatoma HCC grosspathology Courtesy Barbara Banner MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Hepatocellular Carcinoma
Space Occupation, Capsular Involvement and Neuropathic Pain
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Hepatocellular Carcinoma
Space Occupation, Capsular Involvement and Neuropathic Pain
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Lytic metastases, Compression Fractures and Cord Impingement
The sagittal reconstruction of a CT scan shows extensive lytic metastases throughout the thoracic and lumbar spine (green overlay in b). A lytic lesion is also noted in the pubic symphisis. The combination of somatic periosteal nociceptor involvement, mechanical nociceptors that sense the expansion, resulting tissue damage and the release of substances that incite the chemical nociceptors, and possibly damage to the spinal cord and resulting neuropathic pain mechanisms, give adequate cause for pain in this scenario.
75598.8cs03 bone lumbar spine metastasis compression fracture lytic metastases CT scan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Lytic metastases, Compression Fractures and Cord Impingement
The sagittal reconstruction of a CT scan shows extensive lytic metastases throughout the thoracic and lumbar spine (green overlay in b). A lytic lesion is also noted in the pubic symphisis. The combination of somatic periosteal nociceptor involvement, mechanical nociceptors that sense the expansion, resulting tissue damage and the release of substances that incite the chemical nociceptors, and possibly damage to the spinal cord and resulting neuropathic pain mechanisms, give adequate cause for pain in this scenario.
75598.8cs03 bone lumbar spine metastasis compression fracture lytic metastases CT scan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 3
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The sagittal reconstruction of a CT scan shows extensive lytic metastases throughout the thoracic and lumbar spine (green overlay in b). A lytic lesion is also noted in the pubic symphisis. The combination of somatic periosteal nociceptor involvement, mechanical nociceptors that sense the expansion, resulting tissue damage and the release of substances that incite the chemical nociceptors, and possibly damage to the spinal cord and resulting neuropathic pain mechanisms, give adequate cause for pain in this scenario.
75598.8cs03 bone lumbar spine metastasis compression fracture lytic metastases CT scan Courtesy Ashley Davidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The sagittal reconstruction of a CT scan shows extensive lytic metastases throughout the thoracic and lumbar spine (green overlay in b). A lytic lesion is also noted in the pubic symphisis. The combination of somatic periosteal nociceptor involvement, mechanical nociceptors that sense the expansion, resulting tissue damage and the release of substances that incite the chemical nociceptors, and possibly damage to the spinal cord and resulting neuropathic pain mechanisms, give adequate cause for pain in this scenario.
75598.8cs03 bone lumbar spine metastasis compression fracture lytic metastases CT scan Courtesy Ashley Davidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Lytic metastases, Compression Fractures and Cord Impingement
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Lytic metastases, Compression Fractures and Cord Impingement
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Osteomyelitis of the Thoracic Spine
The CT scan in this patient with severe back pain and fever shows destruction of the disc space of T7-T8 as well of both upper and lower involved thoracic vertebra (arrow in b). The transverse image through the space shows bony fragmentation and destruction of the vertebral bodies with bulging paravertebral soft tissue swelling of an evolving abscess (yellow). The red lines reveal somatic visceral periosteal layers that are involved in the inflammatory and infectious process. The pain likely arises from a combination of factors including the swelling caused by the infection (pressure) and involvment of the periostial, pleural, and joint linings.
78031c04.8s pain back thoracic spine intervertebral disc discitis diskitis osteomyelitis soft tissue changes paravertebral periostitis periosteum bone destruction tuberculosis TB question CTscan Courtesy Ashley DAvidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Osteomyelitis of the Thoracic Spine
The CT scan in this patient with severe back pain and fever shows destruction of the disc space of T7-T8 as well of both upper and lower involved thoracic vertebra (arrow in b). The transverse image through the space shows bony fragmentation and destruction of the vertebral bodies with bulging paravertebral soft tissue swelling of an evolving abscess (yellow). The red lines reveal somatic visceral periosteal layers that are involved in the inflammatory and infectious process. The pain likely arises from a combination of factors including the swelling caused by the infection (pressure) and involvment of the periostial, pleural, and joint linings.
78031c04.8s pain back thoracic spine intervertebral disc discitis diskitis osteomyelitis soft tissue changes paravertebral periostitis periosteum bone destruction tuberculosis TB question CTscan Courtesy Ashley DAvidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The CT scan in this patient with severe back pain and fever shows destruction of the disc space of T7-T8 as well of both upper and lower involved thoracic vertebra (arrow in b). The transverse image through the space shows bony fragmentation and destruction of the vertebral bodies with bulging paravertebral soft tissue swelling of an evolving abscess (yellow). The red lines reveal somatic visceral periosteal layers that are involved in the inflammatory and infectious process. The pain likely arises from a combination of factors including the swelling caused by the infection (pressure) and involvment of the periostial, pleural, and joint linings.
78031c04.8s pain back thoracic spine intervertebral disc discitis diskitis osteomyelitis soft tissue changes paravertebral periostitis periosteum bone destruction tuberculosis TB question CTscan Courtesy Ashley DAvidoff MD copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The CT scan in this patient with severe back pain and fever shows destruction of the disc space of T7-T8 as well of both upper and lower involved thoracic vertebra (arrow in b). The transverse image through the space shows bony fragmentation and destruction of the vertebral bodies with bulging paravertebral soft tissue swelling of an evolving abscess (yellow). The red lines reveal somatic visceral periosteal layers that are involved in the inflammatory and infectious process. The pain likely arises from a combination of factors including the swelling caused by the infection (pressure) and involvment of the periostial, pleural, and joint linings.
78031c04.8s pain back thoracic spine intervertebral disc discitis diskitis osteomyelitis soft tissue changes paravertebral periostitis periosteum bone destruction tuberculosis TB question CTscan Courtesy Ashley DAvidoff MD copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Osteomyelitis of the Thoracic Spine
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Osteomyelitis of the Thoracic Spine
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Tissue Injury Axon Reflex and Sensitization
The diagram shows the effect of tissue injury (left side of diagram) that induces the release of prostaglandin, serotonin, bradykinin, and potassium which cause sensitization of the free nerve endings to pain which lowers the threshold to pain. In addition they induce (red arrows) the axon reflex (white arrows) which causes the production and release of substance P from the free nerve endings which cause the release of histamine from the mast cells. The histamine causes vasodilation and exudation into the damaged area. Three of the hallmarks of inflammation are explained in the diagram. Pain, swelling (edema) and hyperemia increased blood flow.
prostaglandin serotonin bradykinin potassium substance P mast cell histamine vasodilation nociceptors pain receptors Davidoff art Copyright 2008 83169b11.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Tissue Injury Axon Reflex and Sensitization
The diagram shows the effect of tissue injury (left side of diagram) that induces the release of prostaglandin, serotonin, bradykinin, and potassium which cause sensitization of the free nerve endings to pain which lowers the threshold to pain. In addition they induce (red arrows) the axon reflex (white arrows) which causes the production and release of substance P from the free nerve endings which cause the release of histamine from the mast cells. The histamine causes vasodilation and exudation into the damaged area. Three of the hallmarks of inflammation are explained in the diagram. Pain, swelling (edema) and hyperemia increased blood flow.
prostaglandin serotonin bradykinin potassium substance P mast cell histamine vasodilation nociceptors pain receptors Davidoff art Copyright 2008 83169b11.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The diagram shows the effect of tissue injury (left side of diagram) that induces the release of prostaglandin, serotonin, bradykinin, and potassium which cause sensitization of the free nerve endings to pain which lowers the threshold to pain. In addition they induce (red arrows) the axon reflex (white arrows) which causes the production and release of substance P from the free nerve endings which cause the release of histamine from the mast cells. The histamine causes vasodilation and exudation into the damaged area. Three of the hallmarks of inflammation are explained in the diagram. Pain, swelling (edema) and hyperemia increased blood flow.
prostaglandin serotonin bradykinin potassium substance P mast cell histamine vasodilation nociceptors pain receptors Davidoff art Copyright 2008 83169b11.8s
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The diagram shows the effect of tissue injury (left side of diagram) that induces the release of prostaglandin, serotonin, bradykinin, and potassium which cause sensitization of the free nerve endings to pain which lowers the threshold to pain. In addition they induce (red arrows) the axon reflex (white arrows) which causes the production and release of substance P from the free nerve endings which cause the release of histamine from the mast cells. The histamine causes vasodilation and exudation into the damaged area. Three of the hallmarks of inflammation are explained in the diagram. Pain, swelling (edema) and hyperemia increased blood flow.
prostaglandin serotonin bradykinin potassium substance P mast cell histamine vasodilation nociceptors pain receptors Davidoff art Copyright 2008 83169b11.8s
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Tissue Injury Axon Reflex and Sensitization
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Tissue Injury Axon Reflex and Sensitization
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Distension and Peritonitis
The CT scan through the abdomen is from a patient with acute cholecytitis. It shows a gallbladder that is distended and is associated with inflammatory exudate surrounding the gallbladder (arrows) and an inflamed area of peritoneum. The pain arises from both the visceral nociceptors due to increased luminal pressure and somatic receptors of the peritoneal lining. The latter pain is aggravated and induced during inspiration, particulalrly when the examining hand puts some pressure in the right upper quadrant (Murphy’s sign), or by pressure from the ultrasound transducer over the visualized gallbladder (sonographic Murphy’s sign).
16157c01s.81 gallbladder edematous wall distended gall bladder edema in the wall fluid in the fat surrounding the gallbladder indurated fat free fluid in Morrison’s pouch acute cholecystitis stones not visible on CT scan pain peritonitis Murphy’s sign inflammation CTscan Courtesy Ashley Davidoff Copyright 2008 All rights reserved
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Distension and Peritonitis
The CT scan through the abdomen is from a patient with acute cholecytitis. It shows a gallbladder that is distended and is associated with inflammatory exudate surrounding the gallbladder (arrows) and an inflamed area of peritoneum. The pain arises from both the visceral nociceptors due to increased luminal pressure and somatic receptors of the peritoneal lining. The latter pain is aggravated and induced during inspiration, particulalrly when the examining hand puts some pressure in the right upper quadrant (Murphy’s sign), or by pressure from the ultrasound transducer over the visualized gallbladder (sonographic Murphy’s sign).
16157c01s.81 gallbladder edematous wall distended gall bladder edema in the wall fluid in the fat surrounding the gallbladder indurated fat free fluid in Morrison’s pouch acute cholecystitis stones not visible on CT scan pain peritonitis Murphy’s sign inflammation CTscan Courtesy Ashley Davidoff Copyright 2008 All rights reserved
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The CT scan through the abdomen is from a patient with acute cholecytitis. It shows a gallbladder that is distended and is associated with inflammatory exudate surrounding the gallbladder (arrows) and an inflamed area of peritoneum. The pain arises from both the visceral nociceptors due to increased luminal pressure and somatic receptors of the peritoneal lining. The latter pain is aggravated and induced during inspiration, particulalrly when the examining hand puts some pressure in the right upper quadrant (Murphy’s sign), or by pressure from the ultrasound transducer over the visualized gallbladder (sonographic Murphy’s sign).
16157c01s.81 gallbladder edematous wall distended gall bladder edema in the wall fluid in the fat surrounding the gallbladder indurated fat free fluid in Morrison’s pouch acute cholecystitis stones not visible on CT scan pain peritonitis Murphy’s sign inflammation CTscan Courtesy Ashley Davidoff Copyright 2008 All rights reserved
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The CT scan through the abdomen is from a patient with acute cholecytitis. It shows a gallbladder that is distended and is associated with inflammatory exudate surrounding the gallbladder (arrows) and an inflamed area of peritoneum. The pain arises from both the visceral nociceptors due to increased luminal pressure and somatic receptors of the peritoneal lining. The latter pain is aggravated and induced during inspiration, particulalrly when the examining hand puts some pressure in the right upper quadrant (Murphy’s sign), or by pressure from the ultrasound transducer over the visualized gallbladder (sonographic Murphy’s sign).
16157c01s.81 gallbladder edematous wall distended gall bladder edema in the wall fluid in the fat surrounding the gallbladder indurated fat free fluid in Morrison’s pouch acute cholecystitis stones not visible on CT scan pain peritonitis Murphy’s sign inflammation CTscan Courtesy Ashley Davidoff Copyright 2008 All rights reserved
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Distension and Peritonitis
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Distension and Peritonitis
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Pneumonia and Pleuritic Pain
The diagram shows an area of pneumonia (yellow) of the right upper lobe that touches the visceral pleura. The visceral pleura is in intimate contact with the parietal pleura and thus both components become inflamed. With normal breathing, these two surfaces rub each other, and in the case of inflammation they rub each other the wrong way, resulting in pleuritic pain. The pain restricts deep breathing in an attempt to “rest” the pleura, but a pleural effusion, commonly a result of pneumonia, would separate the two by creating a neutral zone between them, and thus prevent their physical contact. The concept of a neutral buffer zone is not a new concept in the ancient discipline of biology.
42540c02a01 lung consolidation pleuritic pain pneumonia RUL pneumonic infiltrate pain on inspiration pleura paietal pleura cough Davidoff Art Courtesy Ashley Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Pneumonia and Pleuritic Pain
The diagram shows an area of pneumonia (yellow) of the right upper lobe that touches the visceral pleura. The visceral pleura is in intimate contact with the parietal pleura and thus both components become inflamed. With normal breathing, these two surfaces rub each other, and in the case of inflammation they rub each other the wrong way, resulting in pleuritic pain. The pain restricts deep breathing in an attempt to “rest” the pleura, but a pleural effusion, commonly a result of pneumonia, would separate the two by creating a neutral zone between them, and thus prevent their physical contact. The concept of a neutral buffer zone is not a new concept in the ancient discipline of biology.
42540c02a01 lung consolidation pleuritic pain pneumonia RUL pneumonic infiltrate pain on inspiration pleura paietal pleura cough Davidoff Art Courtesy Ashley Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The diagram shows an area of pneumonia (yellow) of the right upper lobe that touches the visceral pleura. The visceral pleura is in intimate contact with the parietal pleura and thus both components become inflamed. With normal breathing, these two surfaces rub each other, and in the case of inflammation they rub each other the wrong way, resulting in pleuritic pain. The pain restricts deep breathing in an attempt to “rest” the pleura, but a pleural effusion, commonly a result of pneumonia, would separate the two by creating a neutral zone between them, and thus prevent their physical contact. The concept of a neutral buffer zone is not a new concept in the ancient discipline of biology.
42540c02a01 lung consolidation pleuritic pain pneumonia RUL pneumonic infiltrate pain on inspiration pleura paietal pleura cough Davidoff Art Courtesy Ashley Davidoff MD
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The diagram shows an area of pneumonia (yellow) of the right upper lobe that touches the visceral pleura. The visceral pleura is in intimate contact with the parietal pleura and thus both components become inflamed. With normal breathing, these two surfaces rub each other, and in the case of inflammation they rub each other the wrong way, resulting in pleuritic pain. The pain restricts deep breathing in an attempt to “rest” the pleura, but a pleural effusion, commonly a result of pneumonia, would separate the two by creating a neutral zone between them, and thus prevent their physical contact. The concept of a neutral buffer zone is not a new concept in the ancient discipline of biology.
42540c02a01 lung consolidation pleuritic pain pneumonia RUL pneumonic infiltrate pain on inspiration pleura paietal pleura cough Davidoff Art Courtesy Ashley Davidoff MD
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Pneumonia and Pleuritic Pain
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Pneumonia and Pleuritic Pain
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Right UpperLobe Pneumonia
The chest X-ray in A-P and lateral projection show a pneumonia as a dense area in the right upper lobe (a and b). The pneumonia abuts the pleural surface and incites inflammation of the pleura and causes pain. Images c and d show return to normal 4-6 weeks after initiation of treatment after which time both the pneumonia and the pain have resolved.
41819c02 Courtesy Ashley Davidoff MD medical students code chest CXR imaging lung plain film pneumonia radiology resolution
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Right UpperLobe Pneumonia
The chest X-ray in A-P and lateral projection show a pneumonia as a dense area in the right upper lobe (a and b). The pneumonia abuts the pleural surface and incites inflammation of the pleura and causes pain. Images c and d show return to normal 4-6 weeks after initiation of treatment after which time both the pneumonia and the pain have resolved.
41819c02 Courtesy Ashley Davidoff MD medical students code chest CXR imaging lung plain film pneumonia radiology resolution
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
The chest X-ray in A-P and lateral projection show a pneumonia as a dense area in the right upper lobe (a and b). The pneumonia abuts the pleural surface and incites inflammation of the pleura and causes pain. Images c and d show return to normal 4-6 weeks after initiation of treatment after which time both the pneumonia and the pain have resolved.
41819c02 Courtesy Ashley Davidoff MD medical students code chest CXR imaging lung plain film pneumonia radiology resolution
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
The chest X-ray in A-P and lateral projection show a pneumonia as a dense area in the right upper lobe (a and b). The pneumonia abuts the pleural surface and incites inflammation of the pleura and causes pain. Images c and d show return to normal 4-6 weeks after initiation of treatment after which time both the pneumonia and the pain have resolved.
41819c02 Courtesy Ashley Davidoff MD medical students code chest CXR imaging lung plain film pneumonia radiology resolution
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
Right UpperLobe Pneumonia
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
Right UpperLobe Pneumonia
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
This table explores the variety of ways of classifying pain. The left hand column reveals the classification based on functionality, origin, mode of stimulation, pathological causes and relationship of pain to chronicity. As for functionality, it may be adaptive or non adaptive. The pain may originate from somatic or visceral nociceptors or from damaged nerves in which case it is called neuropathic, or it may be psychogenic. The causes are usually via the inflammatory process but may result from any of the diseases listed.
83199b11.8s pain classification adaptive Non Adaptive somatic visceral nociceptive neuropathic psychogenic dysasthetic psychological psychiatric inflammation infection neoplasm ischemia trauma metabolic functional acute chronic duration cause mode of stimulation origin functionality Courtesy Jamie Armstrong PA Table copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
This table explores the variety of ways of classifying pain. The left hand column reveals the classification based on functionality, origin, mode of stimulation, pathological causes and relationship of pain to chronicity. As for functionality, it may be adaptive or non adaptive. The pain may originate from somatic or visceral nociceptors or from damaged nerves in which case it is called neuropathic, or it may be psychogenic. The causes are usually via the inflammatory process but may result from any of the diseases listed.
83199b11.8s pain classification adaptive Non Adaptive somatic visceral nociceptive neuropathic psychogenic dysasthetic psychological psychiatric inflammation infection neoplasm ischemia trauma metabolic functional acute chronic duration cause mode of stimulation origin functionality Courtesy Jamie Armstrong PA Table copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] =>
This table explores the variety of ways of classifying pain. The left hand column reveals the classification based on functionality, origin, mode of stimulation, pathological causes and relationship of pain to chronicity. As for functionality, it may be adaptive or non adaptive. The pain may originate from somatic or visceral nociceptors or from damaged nerves in which case it is called neuropathic, or it may be psychogenic. The causes are usually via the inflammatory process but may result from any of the diseases listed.
83199b11.8s pain classification adaptive Non Adaptive somatic visceral nociceptive neuropathic psychogenic dysasthetic psychological psychiatric inflammation infection neoplasm ischemia trauma metabolic functional acute chronic duration cause mode of stimulation origin functionality Courtesy Jamie Armstrong PA Table copyright 2008
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] =>
This table explores the variety of ways of classifying pain. The left hand column reveals the classification based on functionality, origin, mode of stimulation, pathological causes and relationship of pain to chronicity. As for functionality, it may be adaptive or non adaptive. The pain may originate from somatic or visceral nociceptors or from damaged nerves in which case it is called neuropathic, or it may be psychogenic. The causes are usually via the inflammatory process but may result from any of the diseases listed.
83199b11.8s pain classification adaptive Non Adaptive somatic visceral nociceptive neuropathic psychogenic dysasthetic psychological psychiatric inflammation infection neoplasm ischemia trauma metabolic functional acute chronic duration cause mode of stimulation origin functionality Courtesy Jamie Armstrong PA Table copyright 2008
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
Classification of Pain
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
Classification of Pain
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => Classification of Pain
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => Classification of Pain
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => table
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] => (object value omitted)
[nextElementSibling] => (object value omitted)
[nodeName] => table
[nodeValue] =>
inflammation
infection
neoplasm
mechanical
obstruction
distension
trauma
ischemia
hemorrhage
dissection
rupture
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => table
[baseURI] =>
[textContent] =>
inflammation
infection
neoplasm
mechanical
obstruction
distension
trauma
ischemia
hemorrhage
dissection
rupture
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => rupture
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => rupture
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => dissection
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => dissection
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => hemorrhage
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => hemorrhage
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => ischemia
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => ischemia
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => trauma
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => trauma
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => distension
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => distension
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => obstruction
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => obstruction
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => mechanical
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => mechanical
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 2
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => neoplasm
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => neoplasm
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => infection
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => infection
)
DOMElement Object
(
[schemaTypeInfo] =>
[tagName] => td
[firstElementChild] => (object value omitted)
[lastElementChild] => (object value omitted)
[childElementCount] => 1
[previousElementSibling] =>
[nextElementSibling] =>
[nodeName] => td
[nodeValue] => inflammation
[nodeType] => 1
[parentNode] => (object value omitted)
[childNodes] => (object value omitted)
[firstChild] => (object value omitted)
[lastChild] => (object value omitted)
[previousSibling] => (object value omitted)
[nextSibling] => (object value omitted)
[attributes] => (object value omitted)
[ownerDocument] => (object value omitted)
[namespaceURI] =>
[prefix] =>
[localName] => td
[baseURI] =>
[textContent] => inflammation
)
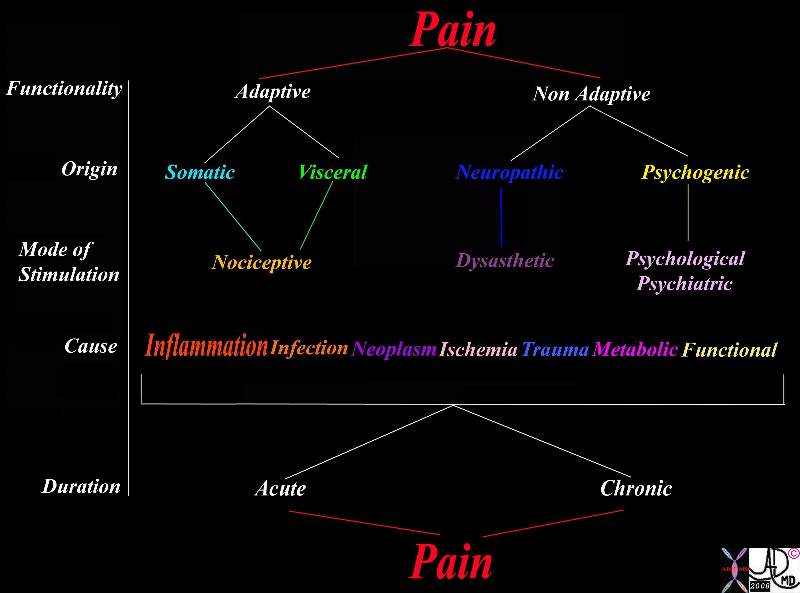 Classification of Pain
Classification of Pain