S
Structural Basis, Diagnosis, and Evaluation
The CommonC Vein Copyright 2008
Authors: Ashley Davidoff, M.D.an; Modern Weng, D.O.
Editor: Pierre d?Hemecourt, M.D.
Definition
Back pain is a disturbing and uncomfortable sensation felt in the lower or upper back. Low back pain may be caused by structural or functional disorders of the lumbar spine, intervertebral discs, nerve roots, spinal cord, muscles or ligaments. The pain may also originate from the bony pelvis or pelvic organs. Sometimes disorders in the upper abdomen can present with back pain such as gallbladder disease, kidney and pancreatic disease. Lastly the skin of the back can also be the cause of back pain.
The clinical result ranges from fleeting pain to debilitating disease and sometimes to life threatening disorders.
The diagnosis requires a careful clinical history that focuses on precipitating factors, duration, onset, character, situation, severity, aggravating relieving, and associated disorders relating to the pain. Imaging may include plain films, CT scan, MRI or bone scan.
Treatment depends on the cause of the back pain and ranges from symptomatic relief with bed rest, analgesics and anti-inflammatory medication through physical therapy, to surgery when indicated.
Background
Low back pain is the second most common reason for physician visits in the United States. Up to 84% of adults have low back pain at some point in their lives. Generalized back pain can have a myriad of etiologies. For most patients, symptoms are self-limited and resolve without any specific treatment. However, for other patients, back pain symptoms are chronic and persistent despite non-specific imaging findings and long-term therapy. Back pain has a substantial impact on lifestyle and quality of life. One US survey found that 72% of those who sought treatment for back pain gave up on exercising or sports-related activities. 60% said they were unable to perform some daily activities, and 46% said they had given up sex because of their back condition. The total costs for the management of low back pain in the United States exceed $100 billion per year. 75% of the total cost is attributable to fewer than 5% of the patients with low back pain. The problem therefore impacts almost all of us in one form or another.
Principles
Structural Principles – The Vertebra
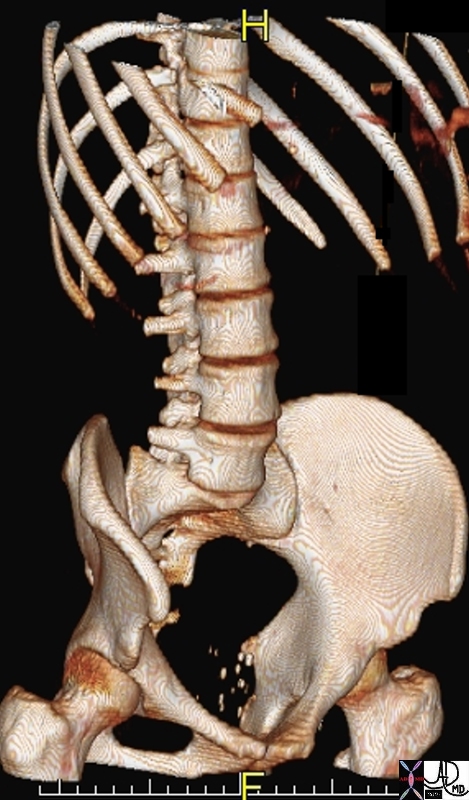
The lumbar vertebra are considered independant building blocks that are connected to vertebra above and below and to the anchoring sacrum that together form a larger unit -the lumbosacral spine. In the larger sense the lumbar spine connects with the thoracic and cervical spine to form the axial skeleton. Via the sacrum and sacroiliac joints the weight of the body is transferred to the lower limbs which help support the weight of the body in the upright position. The lumbar vertebra are built for support and for motion. They support the full weight of the body, and have facets oriented to enable flexion and extension, and side to side motion but they are limited in rotational movement. Diseases of a degenerative nature are more common in the lumbar spine than the thoracic spine because of the increased motion and weight that affetcs the lumbar spine.
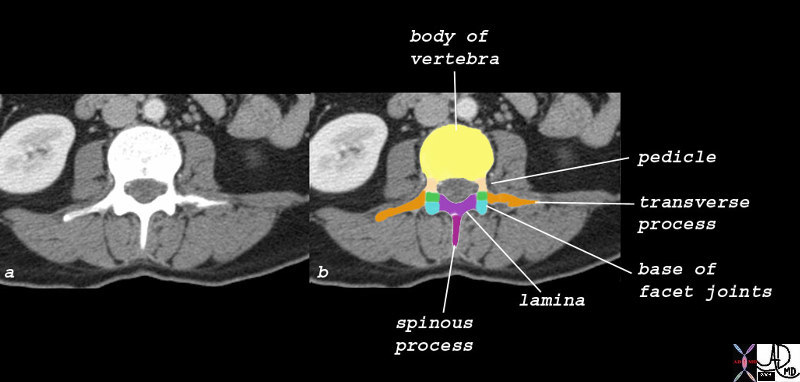
The vertebra consists of two parts: the anterior portion called the vertebral body and the posterior portion called the vertebral or neural arch. The vertebral body is the largest part and is characterized by its cylindrical shape. It forms the anterior border of the spinal canal. The vertebral arch forms the lateral and posterior borders of the spinal canal and consists of 2 pedicles and 2 laminae. Seven further structures arise from the arch. A pair of superior facets, a pair of inferior facets, a pair of transverse processes and a spinous process.
Vertebral Body
The vertebral bodies of the lumbar spine are the largest of the vertebral column. They are wider from side to side than they are from anterior to posterior. They are also slightly thicker anteriorly than they are posteriorly. They usually have concave or straight surfaces superiorly, inferiorly posteriorly and anteriorly. They consist of hard cortical bone externally and less dense cancellous bone internally. The superior and inferior parts of the vertebral body are called the superior and inferior end plates respectively.
Pedicles
The pedicles are short, rounded, and strong bony plates made of thick cortical bone. They connect the posterior aspect of the vertebral body to the lamina enabling the neural canal to be formed around the spinal cord and the cauda equina.
Lamina
The laminae are flattened plates of bone that extend from the pedicles laterally, to join with each other posteriorly and the spinous process forming the posterior components of the neural arch. Its function is to assist protecting the spinal cord and nerves, create a base for the attachment of other bony components of the posterior arch, and to form a base for the attachment of muscles and ligaments.
Facet Joints
The facet joints are situated posterior to the vertebral body and on either side of the vertebra. Thus at the back of the vertebra there are 4 facet joints that contain both cartilage and a synovial lining . The joints are almost vertically oriented providing both strength and rotational ability.
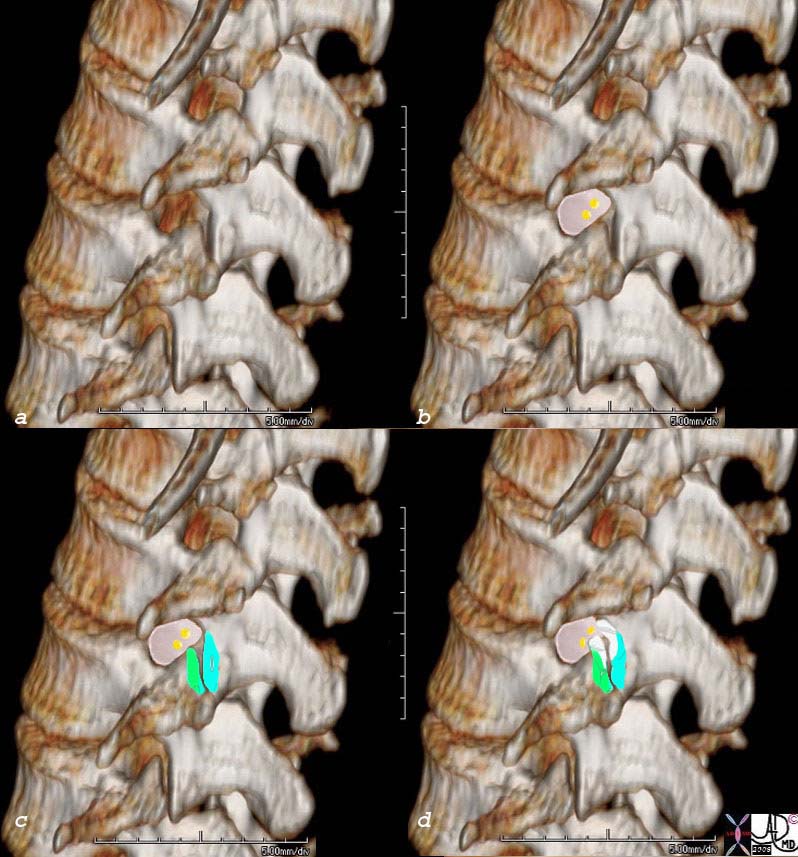
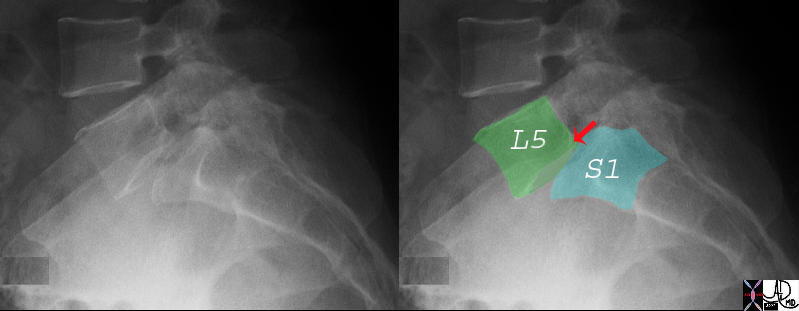
Pars Interarticularis
The pars interarticularis is the part of vertebra that links the superior and inferior articular facets. It is best seen and appreciated in the oblique view of the lumbar spine where the shape of a Scottie dog (Scottish terrier or Aberdeen terrier) can be appreciated.
The pars interarticularis particulalrly of L5 is frequently the site of a stress fracture in young athletes. When this injury is suspected the oblique view of the lumbar spine is extremely helpful and attention to the neck of the Scottie dog is helpful to focus on the anatomical landmark that is affected.
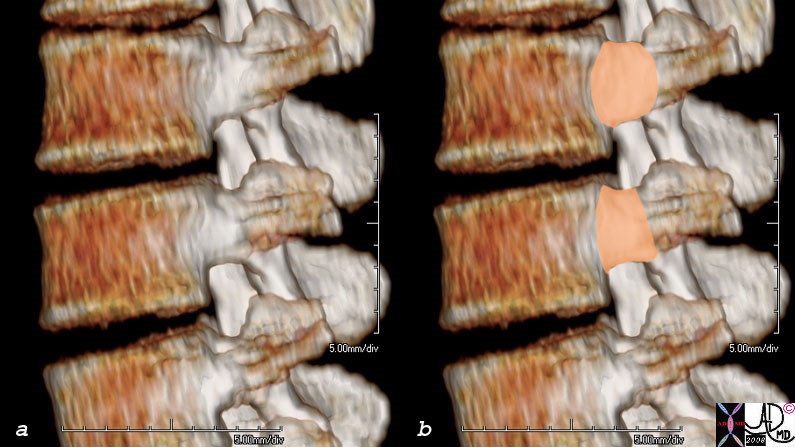
Intervertebral Disc
The intervertebral disc is a fibrocartilagenous structure that lies between the vertebral bodies.
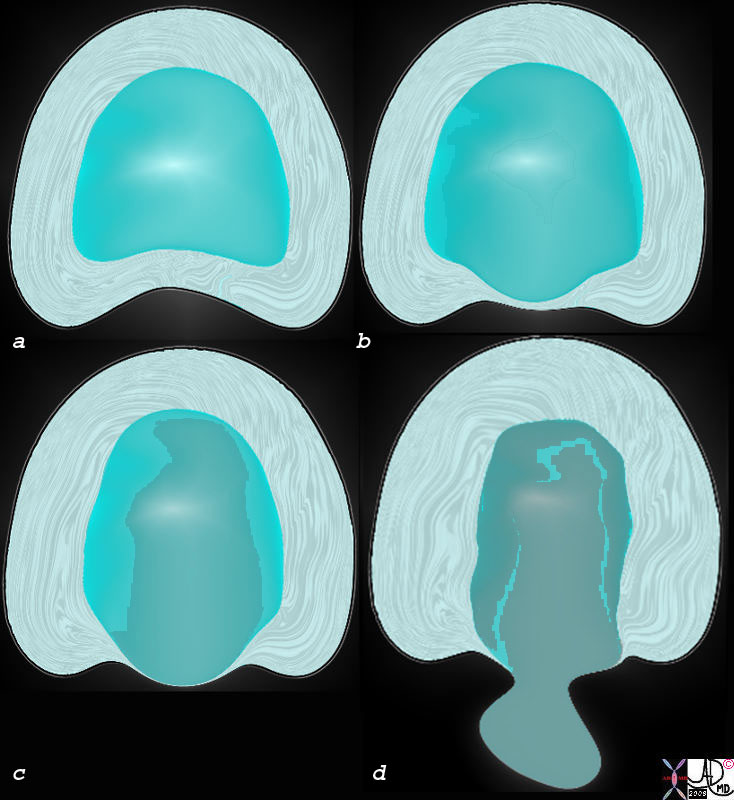
Structurally it consists of a soft inner gelatinous viscoelastic cushion called the nucleus pulposus which is surrounded by a series of fibrous rings collectively forming a tougher surrounding annulus fibrosis.
The nucleus pulposus is nearly 90% water, but also contains complex proteins. It serves to to cushion the stresses between the vertebra as well enabling the movement of the adjacent vertebral bodies in multiple directions.
Aside from enclosing and protecting the nucleus pulposus, the annulus also connects the vertebral bodies and limits the motion between them. The outer fibers of the annulus blend the anterior and posterior longitudinal ligaments of the spine, and are also attached to the bone at the disc margins via Sharpey’s fibers.
The disc has conceptually been compared to a doughnut with a jelly centre. The intervertebral discs make up about one third the length of the spine and represent as a group the largest structure in the body that does not have a direct blood supply. As the discs expand and contract under duress and motion they absorb water and nutrients from their direct environment almost like a sponge.
The overall function of the disc is to act as a shock absorber to reduce the loads on the bony axial skeleton. They compress under stress of weight and spring back when relieved of the stress.The intervertebral disc and facet joints between the vertebra normally allow for a considerable amount of movement including rotation, lateral bending, flexion and extension.
Diseases of the disc include bulging, herniations and ruptures either due to aging and degeneration or due to excessive mechanical forces. As people age, dehydration and degeneration causes the nucleus pulposus to lose its large water content resulting in a decrease in turgor. The loss of turgor is thought to increase the risk of herniated nucleus pulposus.
The Muscles and Ligaments
In addition to the complex bony and cartilagenous components of the vertebra, the ligaments and muscles play an important role in support and stability. The thoracic spine has added support in the form of the ribs and the muscles that link the ribs to each other and consequently stabilise the thoracic spine laterally. The lumbar spine lacks this lateral support and depends solely on the muscles and ligaments for this type of support..
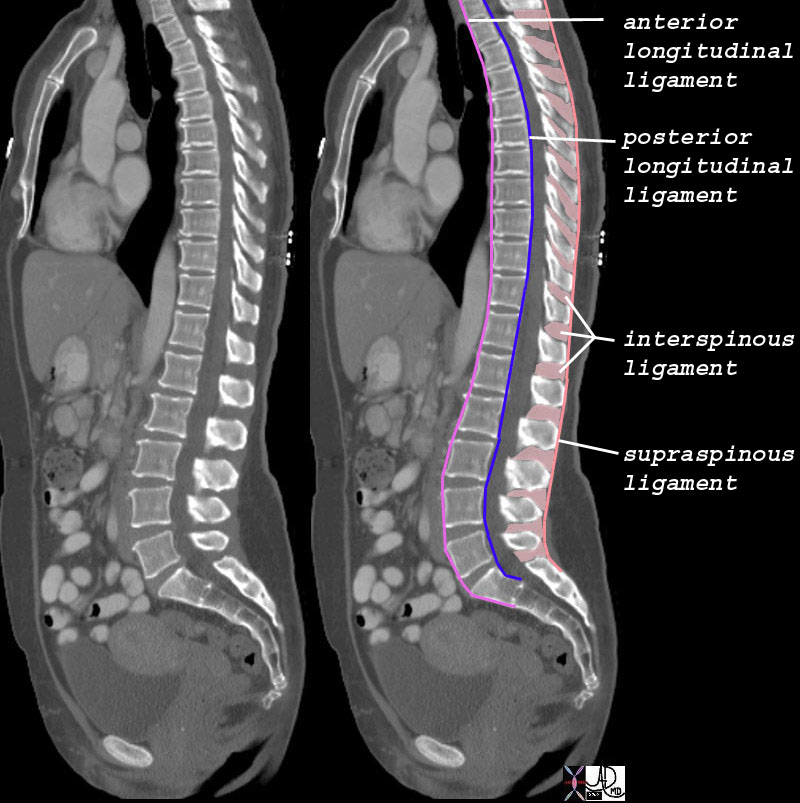
There are 5 major ligaments that support the spine including the anterior longitudinal ligament, posterior longitudinal ligament, interspinous ligament, supraspinous ligament, and the ligamenta flava. The anterior and posterior longitudinal ligaments run vertically along the anterior and posterior aspectsof the vertebral bodies respectively. The posterior ligament begins to narrow at the lumbar region. At L4 and L5, the posterior longitudinal ligament is one-half the width of that at L1. This narrowing produces a weakness in the posterolateral aspect of the intervertebral disc. This weakness makes the lumbar spine more susceptible to disc herniations. It is interesting to note that the spinal cord extends only to the L1 vertebra and thus, the typical disc herniations at L4 and L5 are not at risk of impinging on the spinal cord. However, if there is a severe posterior herniation, this may impinge on the nerves that extend from the base of the spinal cord at L2 (these nerves are also called the cauda equina) which if damaged can cause urine/stool incontinence as well as decreased sensation along the perineum/anus.
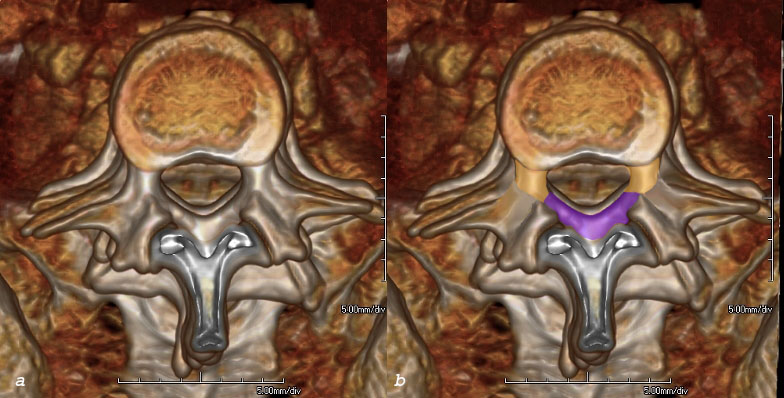
Ligamentum Flavum
The ligamentum flavum is strongest of the vertebral ligaments. The term flavum derives from the Latin word flavum which means yellow and describes the color of the ligament in its natural state. The ligaments are paired, each lying on the inside of the laminae.
Their function is to connect the vertebra, prevent excessive movement and protect the neural elements and the spinal cord.
The Spinal Cord and Canal in the Lumbar Region
The spinal cord connects the brain with the peripheral nervous system. It is protected by the bony spinal column and its length reaches only to about L1 or L2 where it becomes the conus medullaris – the cone shaped tapered end of the spinal cord that has no nerves arising from it .
The nerves for the lumbosacral region hang off the distal spinal cord like the hairs of a horse’s tail . Hence the name cauda equina which is the Latin for horses tail. The nerves extend caudally from the end of the spinal cord, lessening in number as they sequentially exit via the neural foramina to their appropriate segments. At the base of the cauda equina, there are approximately 10 fibre pairs, 3-5 lumbar, 5 sacral, and a single coccygeal nerve.
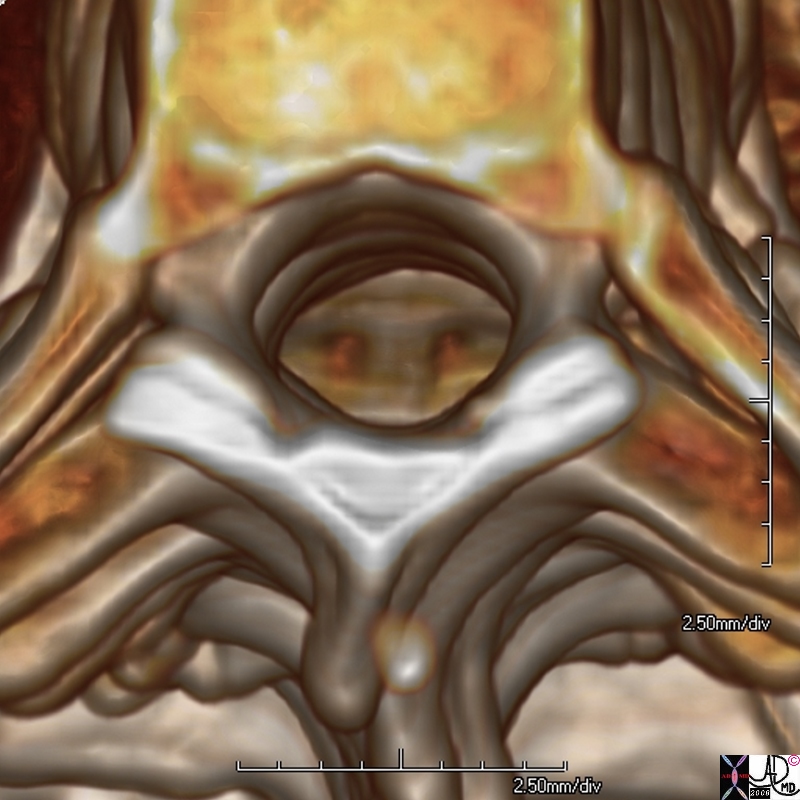
Spinal Canal and its Spaces
The spinal canal is the tubular protective unit that surrounds the spinal cord and nerves. It is formed by the bony and ligamentous components of the vertebra. The bones and ligaments of the spinal column are aligned in such a way to create a canal that provides protection and support for the spinal cord and nerve roots.
Between the ligaments and the periosteum of the bones of the spinal canal and the outer membrane (dura mater) of the spinal cord lies the epidural space (aka extradural or peridural space). It contains small arterioles, venous plexuses, lymphatics, nerve roots, and loose fatty tissue. It is in this space that medication is injected for pain relief.
The duramater ( Latin for “hard mother” ) is the outermost and toughest layer of the spinal cord and nerves. Deep to the dura is another membrane called the arachnoid. (arachnoid is Greek for cobweb) It is a thin avascular membrane which is adherent to the dura. Deep to the arachnoid and intimately attached to the spinal cord is the pia mater (pia is from the Latin pius meaning tender or gentle) which is a thin delicate and vascular membrane. The space between the pia and arachnoid is called the subarachnoid space and it contains the cerebrospinal fluid. It is from this space that fluid is taken for a diagnostic spinal tap, where pressures are measured to evaluate for raised intracranial pressure, and where contrast is injected for myelography.
At the level of the distal end of the spinal cord at L1, the subarachnoid space is a ring of about 2-3mm, while below L2 at the level of the cauda equina it expands to form the more capacious lumbar cistern, and is about 9mm in diameter.
Neural Foramen
The neural foramen or intervertebral foramen is an oval shaped space between two vertebra that houses the spinal nerves and vessels. Each interspace has a pair of foramina. The foramen is bounded anteriorly by the intervertebral disc and posterior aspects of adjoining vertebral bodies, superiorly by the pedicle of the upper vertebra, and inferiorly by the pedicle of the lower vertebra. The posterior border is formed by the facets and joint of the two vertebra. Each neural foramen is thus bounded by three joints.
From the spine a nerve root will exit the intervertebral foramen below its corresponding segment. For example, the L4 nerve root will exit the spinal column between L4 and L5.
· The L1 nerve root supplies motor function to the iliopsoas muscles and sensation on the anterior thigh just below the inguinal ligament. There are no reflexes associated with the L1 nerve root.
· The L2 nerve root supplies motor function to the iliopsoas, adductors, and quadriceps. It also accounts for sensation in the middle of the anterior thigh. There are no reflexes associated with the L2 nerve root.
· The L3 nerve root controls the adductor muscles of the hip as well as the quadriceps. It also accounts for sensation in the anterior thigh just above the knee. There are no reflexes associated with the L3 nerve root.
· The L4 nerve root is responsible for the anterior tibialis muscles and sensation over the patella then extending medially to the medial malleolus. The L4 nerve root is associated with the patella reflex.
· The L5 nerve root controls the extensor hallicus longus and the hamstring muscles. It also accounts for sensation over the proximal lateral aspect of the lower leg just as well as the dorsal aspect of the foot and big toe. There are no reflexes associated with the L5 nerve root.
· The S1 nerve root accounts for motor function in the peroneus longus and brevis muscles as well as the gartrocnemius. It supplies sensation over the lateral malleolus. The S1 nerve root is associated with the achilles reflex.
When the relatively small space of the neural foramen is considered in conjunction with its intimate relationship with the posterior aspects of the intervertebral disc and space, and relationship to the facet joints, it is no wonder that a small space occupying event (disc protrusion, herniation or osteophyte presence) could result in a significant clinical event. The clinical event may be acute or chronic.
Interdependance is a fundamental concept throughout the body, and the spine is no exception. This concept implies that the combination of vertebra to form a new unit (in this case the lumbosacral spine) that is bigger and more powerful than the individual parts. While the bigger unit is more powerful than the individual parts, the bigger unit is only as strong as its individual parts, and continued respect of the role the smaller units play is all imporant. This concept is typified in the spine when a single slippage of one of the parts sometimes only by only a few mms can cause devastating and debilitating symptoms.
Unique features of the Vertebra
Each vertebral body is quite unique and designed with a functional purpose. For instance, the occipital-atlas joint, where the base of the skull meets the first cervical vertebra?also known as the atlas?is specifically intended for flexion and extension. The joint below that, the atlanto-axial joint between C1 and C2 is meant for rotation. The remainder of the upper cervical vertebra motion is rotation, whereas the lower cervical vertebra is designed more for sidebending.
The twelve thoracic vertebra are unique in the sense that, the facet orientation is backward, upward, and lateral. Therefore, based on these facet orientations, the thoracic spine is more conductive to rotation around an axial plane. Whereas the lumbar vertebra have facets that are orientated in a direction that is backward and medial. This orientation of the lumbar spine facets favors and optimizes flexion and extension with respect to the sagittal plane.
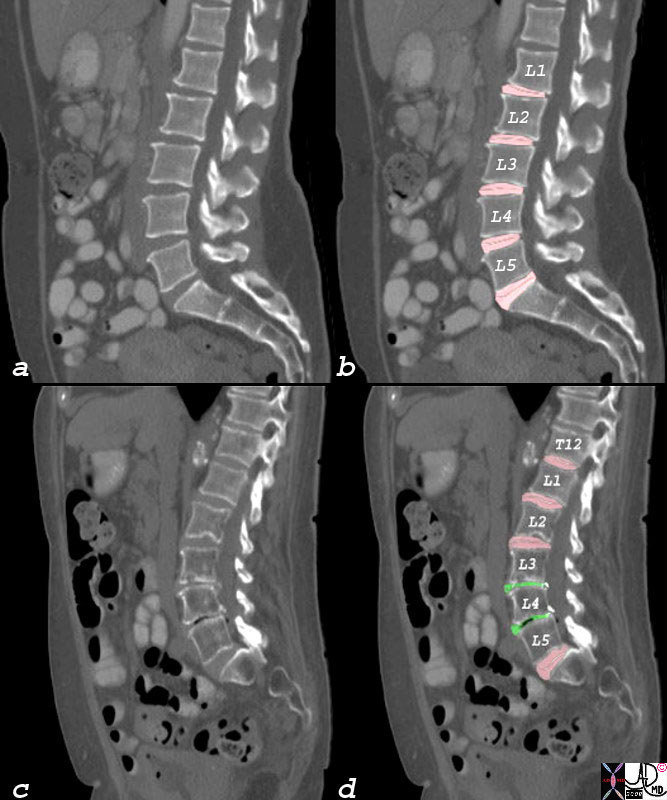
The five lumbar vertebrae are distinguished by their size, facet orientation and large almost rectangular spinous processes. The normal curvature of the lumbar spine is lordotic. The large cross-sectional area of the lumbar vertebral body is designed to sustain longitudinal loads. The L5 vertebra carries the largest amount of weight of any vertebra in the entire spine. The intervertebral discs enlarge progressively from L1 to L5 respective to the increasing weight each has to bear.
Aging
The wear and tear on the spine as people age is universal and nobody is spared. We walk, we stand, sit, kneel, and bend over. We move, we jog, we play sport – and at each turn we depend on the strenghth and integrity of the tissues. The movements around and on the spine are complex and require elasticity pliability and strength. Structures age and get worn out. Elasticity pliability and strength of tissues is lost, dehydration of the disc occurs, and the natural consequences of aging is felt by all the tissues including the back. However the shift of structures by only a few mms in the region of the neural canal as a result of the described degenerating and aging process can have significant consequences.
Space Limitations
Space is an extremely important aspect of the spinal cord and the nerves. The exiting nerve roots negotiate the neural canal which is usually quite capacious and measures approximately 15mm in craniocaudad extent and about 10mm in A-P when viewed in the lateral projection. The nerves and sheaths are relatively small compared to the neural foramen and so the spatial design seems to have latitude.
Disease processes can affect only one of the structural elements described, so that for example isolated disc disease manifest as a herniated disc may result in devastating symptoms. On the other hand a multiplicity of structural components may be abberrant, including disc space narrowing, bulging disc, osteophyte formation, facet joint disease and ligamentous weakening without significant symptoms or signs. The net clinical effect relates to the critical space which the disease occupies together with other factors such as the release of chemical irritants as a result of injury.
Forces
The basic standing position places overall gravitational and longitudunal force on the spine with the greatest weight accomodated by the lumbar spine and more specifically by L5. The centre of gravity of the body is just anterior to the lumbar spine. The upright posture therefore places a continual downward and forward thrust on the lower lumbar spine. The facet joints are therefore under continual stress, with the forces focused on the pars interarticularis. The lordotic shape of the lumbar spine tends to disperse the force so that the other lumbar vertebra assume responsibility to accomodate a share of the force. Flexion and extension create variable and changing compressive forces on the discs, that from a functional point of view serves to disperse pressure, but also creates sponge like negative pressures that help the disc to absorb water and nutrients direct from the immediate environment. The facet joints have forces exerted on them by flexion and extension, side to side motions, and rotational movement. The ligaments and the orientation of the facet joints limit the extent of movement. In the healthy spine the forces are well balanced – but the spine is only as strong as its weakest link.
Interactions
There are three major joints between adjacent vertebra; intervertebral disc space and the two facet joints. They act in concert. When any of these joints is traumatised or degenerates it puts undue stress on the others and they may respond by creating bony butresses to aid stability. These buttresses are called osteophytes. Thus when the disc loses height there is consequently much less support for the facet joints at that particular level, and the joints become subject to increased stress. In addition accelerated wear and tear on the joints might occur as a consequence of unbalanced distribution of forces. The effects of the unbalanced forces puts increased stress on the ligaments and muscles and consequently pain syndromes result from any one of the consequences of a single weak element in the veretebral chain. In addition the natural weakening of the aging bone by osteoporosis diminishes the overall support.
Diseases of the Lumbar Spine
Now that we have a good sense of the structure of the lumbar spine we will review some of the more common diseases that affect the spine, and more specifically those that cause back pain.
The differential diagnosis for back pain can be essentially divided into mechanical versus non-mechanical etiologies.
- Mechanical low back pain:
- Degenerative disc or joint disease
- Spinal stenosis
- Herniated nucleus pulposus, annular tears
- Spondylolysis, spondylolisthesis
- Osteoporotic compression fracture
- Severe kyphosis, scoliosis, or transitional vertebrae
- Musculoskeletal strain or sprain
- Cauda equine syndrome
- Non-mechanical spinal conditions:
- Primary vertebral tumors, multiple myeloma, or metastatic cancer to the spine
- Osteomyelitis, epidural abscess, discitis, or shingles
- Dissecting aortic aneurysm
- Nephrolithiasis, pyelonephritis, or perinephric abscess
- Ankylosing spondylitis, psoriatic spondylitis, Reiter?s syndrome, or Paget?s disease of the bone
Degenerative disc or joint disease (osteoarthritis)
Degenerative joint disease (aka DJD, osteoarthritis, spondylosis, and spinal arthritis) is a group of disorders that are primarily characterised by changes in the joint cartilage caused by wear and tear on intervertebral discs and or the cartilage of the facet joints. As the cartilage changes, there are secondary effects on the surrounding tissues that help characterize the disorder, including joint space narrowing, vaccuum phenomenon, bony irregularity, sclerosis, eburnation of the opposing joint surfaces, subchondral cyst formation, and osteophytes.
The cause of degenerative disc or joint disease is typically an age-related phenomenon commonly associated with overuse. Other risk factors include obesity, female sex, family history, and previous back injuries.
The result of the degeneration is a syndrome in which structural changes, compensatory mechanisms, and low-grade inflammation results in pain in the joints or in the surrounding region. With prolonged DJD, destruction and remodeling of the joint itself will occur. Often osteophytes or bone spurs will be seen as will an irregularity of the joint surface signaling a chronic inflammatory reaction. A variety of specific entities including disc bulge, disc herniation, disc rupture, lumbosacral facet syndrome, and spinal stenosis fall under the umbrella of DJD.
The diagnosis of DJD rests on the combination of the clinical presentation and imaging appearances. Symptoms associated with osteoarthritis in the lower back include stiffness in the morning that resolves later in the day with more activity, tenderness to palpation of the lumbar spine, and decrease flexibility.
Plain x-rays of the lumbar spine will show evidence of spondylosis, osteophyte formation, and decreased intervertebral space but will not be able to characterize changes in the disc. MRI is more able to identify structural changes in the soft tissues.
The most common appearance of degenerative joint disease is disc space narrowing with some osteophytic change. There is often some gas in the joint, usually nitrogen that is sucked into the joint by the vacuum that is caused when the disc losses volume by losing water and shrinks in an air tight space. This phenomenon is called “vacuum phenomenon” Additionally one usually sees some roughening and sclerosis of the surfaces of the joint. More commonly than not the patient with DJD is asymptomatic. The radiological appearance often does not correlate well with the clinical picture. Thus a patient with no symptoms may have significant structural changes and a patient with little structural change on X-ray may have severe symptoms. The MRI has the most specific correlation with acute symptoms since it reflects the aberrant changes in the disc and abnormal disc position in the patient with acute back pain . Thus it is very important to reiterate that it is the combination of the clinical evaluation and the imaging that enables the clinician make an accurate diagnosis.
Many patients can be treated successfully with weight reduction, core and para-spinal muscle strengthening, NSAIDs, as well as lumbar supportive bracing. Epidural corticosteroid or facet joint injections maybe considered for patients with continued back pain despite treatment. Patients that have failed non-operative treatment who continue to have intolerable symptoms of back pain secondary to degeneration may require surgical decompression.
Lumbar spinal stenosis
Lumbar spinal stenosis is defined as a congenital or acquired narrowing of the spinal canal, nerve root canals, or intervertebral foramina due to spondylosis or degenerative disc disease. It usually affects the middle aged and older population and affects from the cervical and lumbar spine. It is uncommon for the thoracic spine to be affected.
The narrowing of the spinal canal is caused by any combination of many degenerative structural changes that affect the spine but the primary process is the degenerative changes in the discs which dehydrate and narrow. This process can cause tilting, slippage, or rotation of vertebral bodies which results in shortening of the spinal column. The changes in stresses also cause any combination of osteophyte formation, facet hypertrophy, bulging disks, and hypertrophy of the ligamentum flavum. The ligamentum flavum may also buckle inward as a result of the loss of height and compress the spinal sac and nerve roots. The ligamenta flava sometimes also calcify or ossify. Degenerative spondylolisthesis or slippage of one vertebra on another caused by loss of ligamentous muscular and bony support can further compromise the canal.
The net result is a a pressure or impingement of the nerve roots prior to their exit form the foramina due to the narrowing. Lumbar spinal stenosis rarely causes pressure or impingement on the spinal cord itself because the spinal cord and conus medullaris end at L1.
The diagnosis of spinal stenosis is based on the combination of clinical presentation and imaging.
Clinically lumbar spinal stenosis may present with classic pseudoclaudication symptoms of leg pain during ambulation that improves with rest. As the name suggests, nerve root entrapment occurs, as there is progressive congenital or acquired narrowing of the spinal canal, nerve root canals, or intervertebral foramen. Sometimes the pain is relieved when the patient bends forward. Other symptoms of spinal stenosis include persistent generalized back pain, numbness in the lower extremities with walking, and radicular pain to the feet.
Imaging is essential to make the diagnosis. Radiographically, tthe diagnosis is most evident on MRI as one can not only directly visualize the disc and soft tissues but also get a relative sense of the bony structural changes. CTscanning is better for the bony elements but CTmyelography is the alternate consideration when MRI is not viable.
Symptoms may be relieved by conservative therapy which includes prolonged sitting and flexion of the lumbar spine. Non-operative treatment involves analgesics, NSAIDs, physical therapy, cardioaerobic conditioning, and epidural corticosteroid injections. For patients with persistent severe pain, a decompressive laminectomy can be considered.
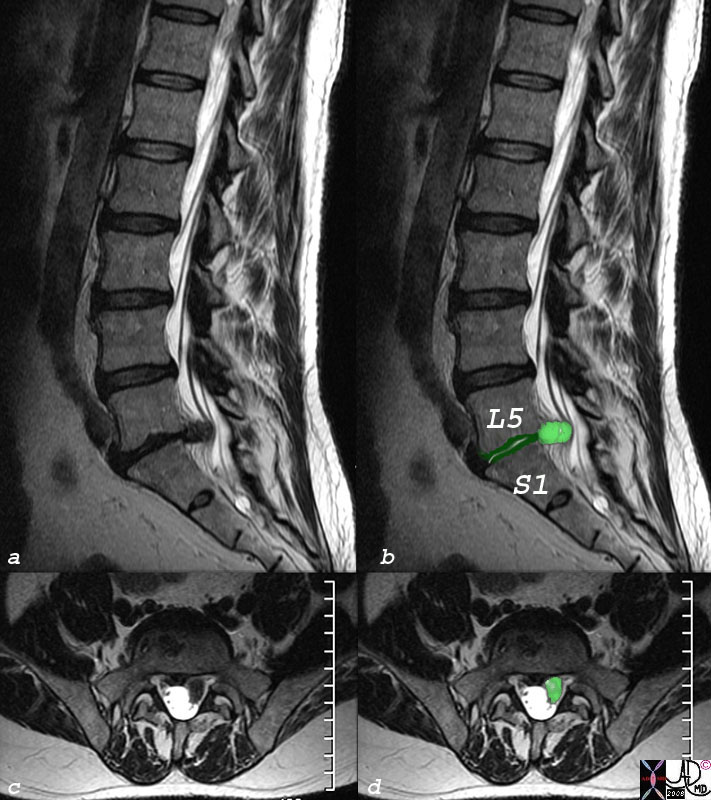
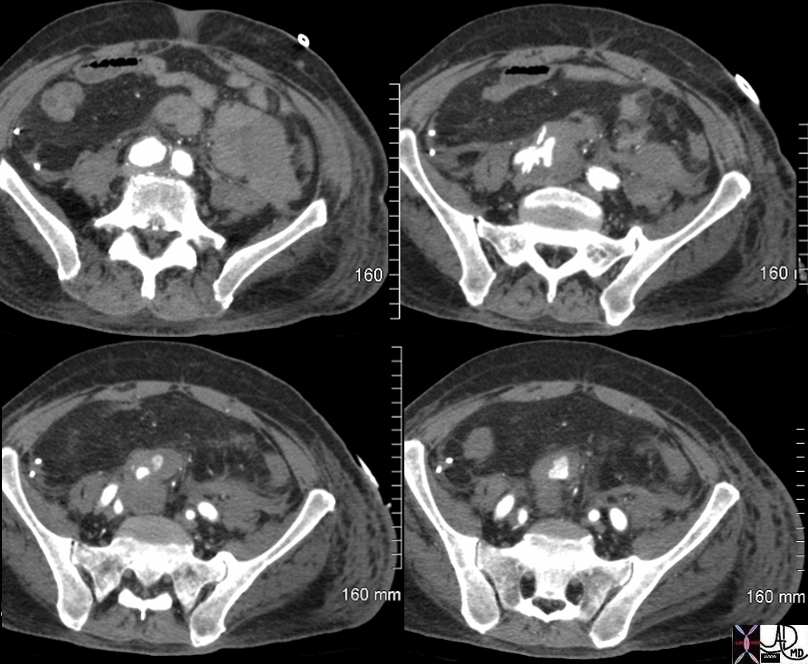
  MRI of Spinal Stenosis MRI of Spinal Stenosis |
| This T2 weighted MRI image is from the same patient above with spinal stenosis, and is used to explain the changes in the transverse views (b,c). The narrowing is commonly caused by facet hypertrophy and ligamentous hypertrophy. On the T2 weighted images the CSF is white and the back of the red arrow points to the normal thecal sac behind the vertebral body seen with the nerves in the sagital plane, while the red arrowhead points to the normal thecal sac and nerves in the transverse plane. At the level of the disc at L3-4 and L4-L5, the thecal sac is obliterated since no white CSF can be identified because it has been squeezed out by the facet and ligament hypertrophy. The base of the green arrow is at the L3-L4 disc space in the sagittal plane and the green arrowhead points to the same level in the axial plane at the level of the spinal stenosis.
73849c01 bone spine ligamentum flava hypertrophy lumbar spine cauda equina impingement on nerves and thecal sac space occupation back pain dx spinal stenosis MRI T2 weighted images Courtesy Ashley Davidoff MD |
Herniated nucleus pulposus, annular tears
A herniated nucleus pulposus (HNP) is a mechanical disorder that results from a displaced intervertebral disc. It is commonly referred to as a ?slipped disc.? It is caused by a tear of the annulus fibrosis which allows for a protrusion of the nucleus pulposus. The resulting mass effect on the nerve roots is responsible for sensory and or motor deficits and pain. The disc protrusion is best diagnosed by MRI, which reflects innate changes in the disc and the mass effect on the nerves and epidural space. CT is an alternate but less sensitive technique while plain film can only reflect narrowing of the intervertebral disc space but cannot visualize the disc.
An HNP or annular tear can occur at any age. There is evidence in the medical literature that suggests that imaging studies may find evidence of an HNP even in patients without lower back symptoms. Therefore it is again important to reiterate that clinical correlation is strongly suggested when attributing lower back pain to a HNP. Symptoms are non-specific but usually relate to flexion of the lumbar spine and typically occur with prolong sitting and bending forward. Patients may also note that symptoms are relieved with laying flat.
At its worse, a HNP may cause radiculopathy?numbness, tingling, and even motor weakness in the lower extremity past the knees. A frank herniation of the lumbar nucleus pulposus may cause impingement to the cauda equina nerves causing urine or stool incontinence. This is a surgical emergency and is known as cauda equina syndrome. HNP causing radiculopathy without symptoms of cauda equina syndrome maybe treated initially with narcotic pain medication, prednisone taper, or a strong NSAIDs (nonsteroidal anti-inflammatory drugs).
Additionally, an epidural corticosteroid injection can be offered for temporary symptomatic relief in some patients. After the acute phase of this condition, gradual progression with physical therapy focusing on lumbar spine strengthening and flexibility is advised. At times a supportive lumbar brace maybe used to help manage the symptoms of an HNP. The natural history of this condition is gradual clinical improvement and return to regular activities in several weeks to even months. However, those with persistent symptoms secondary to HNP that is not responsive to non-operative treatment, diskectomy is considered.
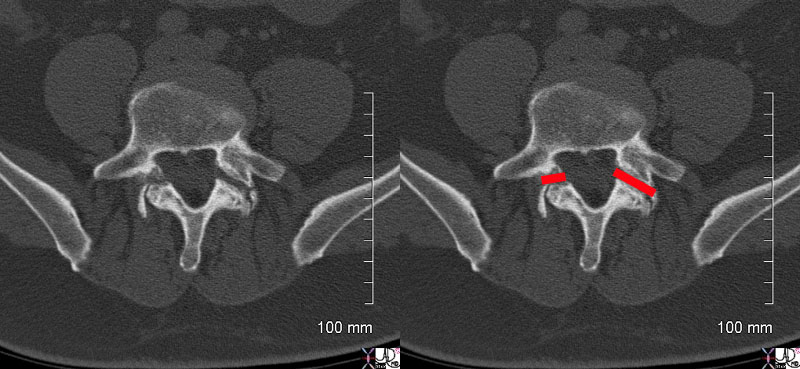
Spondylolysis
Spondylolysis is a non-displaced stress fracture along the pars interarticularis caused by congenital weakness or repetitive trauma tothe pars interarticularis.
In the adolescent athletic population, extension based back pain is especially suspicious for spondylolysis. With more and more children participating in organized athletics, there appears to be an increase prevalence of this condition. Sports such as gymnastics, ballet, figure skating, rowing, and football tend to require repetitive extension of the lumbar spine, and thus, may be a source of increase risk for spondylolysis.
The entity may be complicated by spondylolisthesis which is an anterior slippage or displacement usually of L5 on S1.
The diagnosis is made radiographically using oblique projections of the lumbar spine, and is characterized by a break in the ?collar? on the Scotty dog. If this is negative, and suspicion remains high then a SPECT bone scan should be ordered first followed by a CT scan isolated to the specific area that is positive on bone scan.
The treatment is initially conservative, using rest, analgesia and temporary cessation from athletic activity. Nonsteroidal anti-inflammatory drugs such as ibuprofen are useful . In patients who do not respond to this basic therapy, an anti-lorditic brace for twelve weeks is used, combined with physical therapy emphasizing core and para-spinal musculature strengthening as well as stretching of the hamstring and hip flexor muscles. The patients are usually transitioned into sports with a supportive brace during activity for four to six more weeks.
Spondylolysis comes from the Greek words spondylos, meaning spine or vertebra, and lysis, which means a break or loosening.
- The cause for the slippage or displacement is most commonly spondylolyis and degenerative disease, but also includes congenital isthmic dysplasia, trauma and post operative iatrogenic causes. The bony defect in the pars interarticularis is responsible for the spondylolisthesis in the group of patients with spondylolysis. In degenerative disease a combination of ligamentous injury, facet joint disease, and disc thinning lead to the instability and there may be either forward slippage (anterolisthesis ) or retrolisthesis (posterior listhesis) In the congenital group bony dysplasia of the vertebral arch and or the facets at the lumbosacral junction cause the slippage. Traumatic injury can affect the pars, facets, or ligaments and result in listhesis.Diagnosis is based on imaging and a simple lateral examination of the lumbar spine can document the listhesis. The spondylolysis may be identified on the lateral exam, but oblique views are best for this entity. CTscan and better still CTmyeloraphy are exellent alternatives and do add more information as to the cause of the slippage. MRI offers visualization of the soft tissues.
- Treatment depends on the cause but the back pain is initially treated with conservative methods of pain relief and rest.
- The result of the slippage is anatomical distortion which may cause impingement on the nervees. The clinical consequence ranges from the asymptomatic patient to one with pain , sensory, and or motor dysfunction.
- Spondylolisthesis describes a mechanical abnormality of the vertebral column characterized by slippage of one vertebra on another
- Spondylolisthesis
- Acute Traumatic Injury to the Lumbar SpineAcute compression fracture of the lumbar spine is caused usually by vertical loading forces on the spine such as a fall from a height.
-
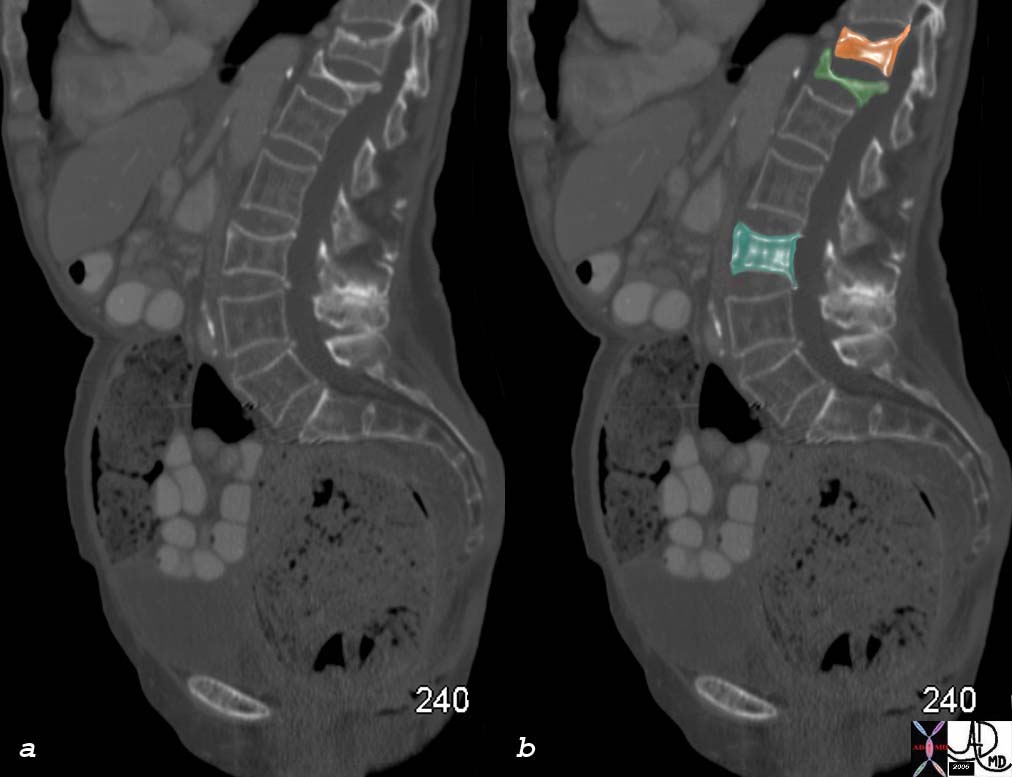
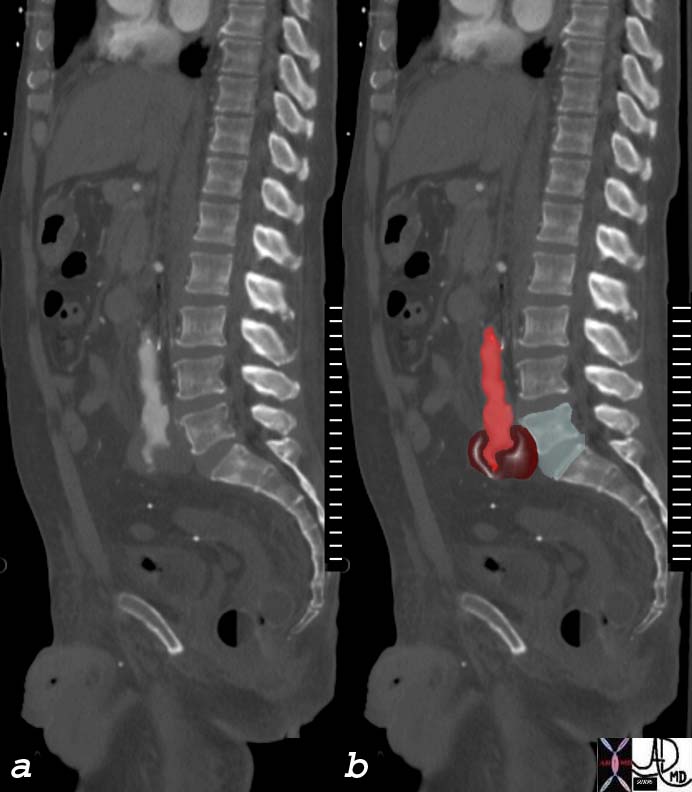
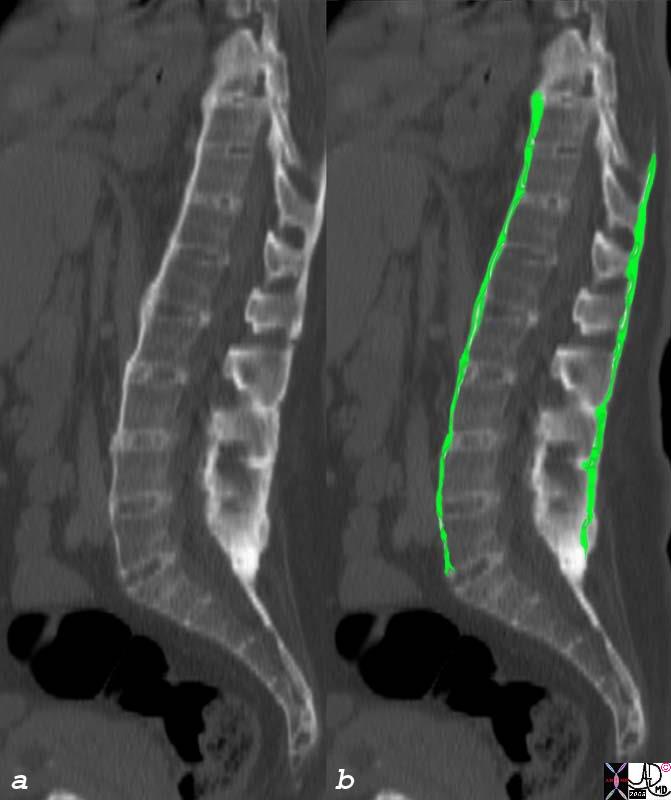
The sagital T2 weighted image of the lumbar spine is from a young patient who sustained a traumatic burst compression fracture (green) of L1 with retropuilsion of the posterior fragment into the thecal sac (white CSF column is obliterated) with impingement on the cauda equina and the conus medullaris. 78652cs lumbar spine trauma burst fracture L1 MRI T2 weighted Courtesy Philips Medical Systems
Musculoskeletal strain or sprain
- The structural result of the osteoporotic compression is a distortion of the vertebral body and change in the distribution of body forces. Clinically pain is the most outstanding feature. It is caused by the bony injury itself but secondary changes in the sacroiliac joints, hips and thoracic spine may cause pain in these areas as well.
- Compression fractures of the lumbar spine are mechanical and traumatic disorders of the vertebral body and are characterized by loss of height and shape deformity of the vertetebral body. They are most commonly caused by bone weakening with normal stresses in conditions of osteoporosis or metastatic bone disease, but in the acute traumatic setting, excessive vertical loading forces on normal bone is the cause of the compression.
- Compression Fractures
The strain is caused when a muscle-tendon unit is stretched or overloaded. A sprain is caused when there is ligamentous or facet capsule injury. Injury is usually caused by forceful contraction, sudden torsion, direct blows, or forceful straightening. These injuries are most commonly seen in athletically related injuries, both in professional athletes whose muscles and ligaments are primed and in the weekend athletes. Physical exam finding are non-specific ranging from extreme lower back pain in all ranges of motion to simply some tenderness to palpation of the para-spinal muscles. The imaging studies and blood work are often normal, though MRI may show edema of the strains or sprains associated with the injured muscles and ligaments.
- Treatment with non steroidal anti-inflammatory drugs (NSAIDs) is effective for symptom pain relief and muscle relaxants for spasm are recommended together with some bed rest and an ice pack.. A common side effect of muscle relaxants is sedation and thus, this class of drug is often given at bedtime to decrease lower back symptoms and aide in sleeping. Lower back physical therapy and cardio aerobic conditioning is also generally recommended for musculoskeletal strain once the patient has passed through the acute phase of increased pain and discomfort. There is anecdotal evidence that spinal manipulation by an osteopathic physician, chiropractor, or a masseuse may provide symptomatic relief.
- The diagnosis often is made based on the clinical history where the pain is acute, and related to a specific forceful or violent strain on the back muscles or ligaments.
- Musculoskeletal strain or sprain is lower back pain without any evidence of systemic, skeletal, joint, or intervertebral disc disease.
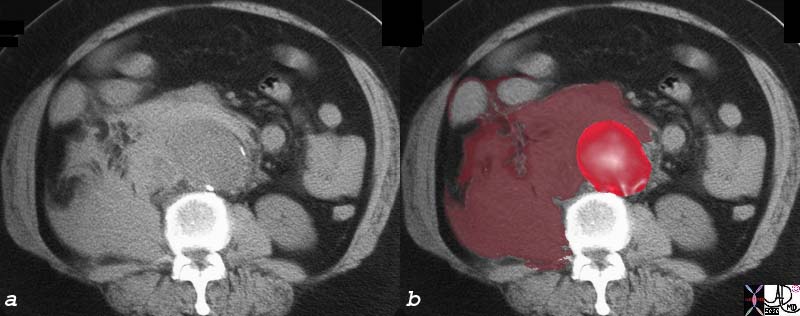
Metastases Metastatic disease to bone is a malignant space occupying abnormality caused by seeding from a systemic artery, retrograde extension through a paravertebral vein, or by direct extension of tumor. Metastases to bone most commonly occurs to those bones with residual red marrow, and thus the spine is a relatively common site. The resulting changes are variable, since the bone responds to the space occupation by either osteoblastic, osteoclastic or mixed mechanisms depending on the nature of the malignancy. The bone however is weakened by the process, and resulting structural changes such as fractures can occur. The periosteum is stretched and invaded and this causes pain, though not all metatstatic disease is associated with pain. Continued growth can result in extension into the spinal canal with consequent neurologic involvement.
The diagnosis is considered in patients with a known malignancy who present with new back pain, or a middle aged or elderly patient who complains of new back pain. More commonly than not, the pain in the latter instance is related to DJD, but it is incumbant on the clinician to exclude metastatic bone disease in this group of patients.
It is reasonable to start with a plain film of the spine that may assist in directing subsequent imaging. If an obvious metastatic lesion s identified, the diagnostic algorithm is directed to identify the primary lesion. Depending on the clinical scenario, imaging may be directed to a bone scan which would identify metastatic pattern of multicentric bone disease, or to MRI which is best able to confirm and characterize metastatic disease.
Treatment depends on the nature of the clinical presentation, disease, and imaging findings but ranges from symptomatic pain relief, to radiation for lesions that have extended into the spinal canal.
Cauda Equina Syndrome
Cauda equina syndrome (CES) is an uncommon emergency clinical syndrome characterised low back pain, saddle sensory disturbances, usually bilateral sciatica, variable motor disturbance and bladder bowel and sexual dysfunction.
It is caused by compression of the cauda equina by a variety of disease processes including degenerative disc disease, trauma, inflammatory diseases (ankylosing spondylitis, sarcoidosis) infections (abscesses) neoplastic disease (lymphoma or metastases) and circulatory disease (inferior vena caval thrombosis or hematoma).
- The result is motor, sensory, or autonomic nerve dysfunction that tends to be bilateral, but can be unilateral involving nerve roots from L1-5 and S1-5 . Treatment is directed to the cause but early decompression is generally indicated. Osteomyelitis is an infection of bone usually caused by staphylococcus aureus. Non pyogenic causes include tuberculosis, fungus, parasitic diseases, and yeasts. The organisms may reach the disc or bone hematogenously with the skin and genitourinary tract often being the primary sources, but bacterial endocarditis, arthritis, and sinusitis also can be primary foci of disease. Sometimes the infection occurs as a result of direct spread from adjacent septic foci such as an infected aortic graft.
- The result include progressive inflammatory and destructive changes in the anterior elements of the spine characteristically affecting both sides of the disc space. Less commonly (5%) the posterior elements are affected. The disease is complicated by abscess formation in the disc space, paravertebral abscess, or epidural abscess. Progressive destruction of the bone can lead to compression. The latter two complications can lead to neurological compromise.
- Osteomyelitis
- The diagnosis is based dominantly on the clinical presentation and the imaging studies confirm structural abnormality but there are no specific findings that will for example differentiate cauda equina syndrome drom disc herniation. it is the severity and extent of the clinical presentation that defines the entity.
- The diagnosis is based on the clinical presentation and imaging findings. Pain is commonly insidious in onset, is progressive, until it is incapacitating without responding to conventional analgesis. Neurological involvement is late. Only half the patients are febrile, leukocytosis is often absent, though the ESR is almost always elevated and one most reliable lab findings.CTscan is sensitive to the bony changes, and will reveal paravertebral soft tissue changes, while MRI is most sensitive to the soft tissue changes and onflammatory exudative changes in the bone and or soft tissues. technetium bone scan shows inflammatory activity but is non specific.Treatment is with antibiotics. Abscesses require drainage by percutaneous via surgical techniques.
- Once the diagnosis is suspected, CTguided aspiration and or biopsy is needed to isolate the organism.
- The plain film of the lumbar spine is often normal in the early phases, but as bony changes ensue the findings become more apparrent.
Aneurysmal DiseaseAneurysmal disease of the aorta or iliac arteries may impinge on the vertebral column and uncomonly will cause back pain. Ruptured aneurysnms however will result in acute severe back pain associated with hypotension resulting in an acute life threatening emergency.
Ankylosisng SpondylitisAnkylosisng Spondylitis is a chronic seronegative inflammatory condition of the articular and paraarticular joints of the spine that is characterized by its progressive ascending involvement of the spine, starting in the sacroiliac joints and lower lumbar spine and progressing to the cervical spine. The inflammatory changes also characteristically involve sites where the joint capsules, ligaments and tendons are attached to the bone and bony ankylosis of the spine results. Associated diseases include peripheral arthritis, iritis, pulmonary disease.The diagnosis is usually made by a combinatoin of clinical, blood tests and imaging studies.During the acute phases the ESR is elevated and 95% of patients exhibit the HLA B27 antigen. Treatment is usually aimed at pain control and decreasing inflammation, with nonsteroidal anti-inflammatory drugs (NSAIDs) most commonly used . Steroids and immunosuppressive agents are sometimes used to reduce the inflammation.
Clinical
Causes and Predisposing Factors
Risk factors for back pain include smoking, obesity, older age, female gender, physically strenuous work, sedentary work, anxiety, and depression. Rarely, acute back pain is a harbinger for a serious systemic illness such as a neoplastic malignancy, aortic aneurysm, abscess formation, or rheumatologic disease.
Lastly, some possible etiologies of generalized back pain can be broadly categorized as:
- Spinal nerve injuries
- Vertebral fractures
- Discogenic pain
- Degenerative joint disease
- Developmental defects
- General contusions and strains
- Neoplasm
- Infection or abscess formation
- Rheumatological disease
- Referred pain (i.e. from an aortic aneurysm, renal stones, hip pathology, etc)
- The word ankylosing comes from the Greek word ankylos, meaning anchoring, or stiffening , while spondylos means vertebra. Spondylitis refers to inflammation of one or more vertebrae
- Radiologically the appearance of the spine is pathognomoni characterized by bony ankylosis. In the early stages, bilateral sacroilitis characterised by indistinctness of the joint, with subchondral erosions on the iliac side. The early changes in the spine are characterized by anterior corner erosions on the vertebral bodies, (Romano lesions) with subsequent bridging between the vertebra, followed by bony ankylosis.
- Clinically the patient is usually a young male who presents with low back pain centered over the sacrum and which may radiate to the buttocks and legs. As the upper spine becomes involved pain ascends into the thoracolumbar area. Flexion becomes difficult .
- The cause of the disease is mostly unknown but 95% of patients with the disease exhibit the HLA B27 marker suggesting a genetic factor. However all patients with HLA B27 do not develop ankylosing spondylitis and and nort all patients with AS have a positive HLA B27. The disease does run in families strengthening the genetic and familial involvement in the etiology of the disease.
The differential diagnosis for back pain can be essentially divided into mechanical versus non-mechanical etiologies.
- Mechanical low back pain:
- Musculoskeletal strain or sprain
- Degenerative disc or joint disease
- Herniated nucleus pulposus, annular tears
- Cauda equine syndrome
- Spinal stenosis
- Osteoporotic compression fracture
- Spondylolysis, spondylolisthesis
- Severe kyphosis, scoliosis, or transitional vertebrae
-
- Non-mechanical spinal conditions:
· Primary vertebral tumors, multiple myeloma, or metastatic cancer to the spine· Dissecting aortic aneurysm· Ankylosing spondylitis, psoriatic spondylitis, Reiter?s syndrome, or Paget?s disease of the bone
- · Nephrolithiasis, pyelonephritis, or perinephric abscess
- · Osteomyelitis, epidural abscess, discitis, or shingles
Clinical Approach to Back Pain –
The clinical approach to the diagnosis of back pain requires careful and insightful questioning. Since back pain is a common problem, it is incumbent to start out with a history that elucidates the character of the pain and defines associated symptoms and diseases. It is all too easy to get an MRI to help with the diagnosis, but the imaging findings as pointed out, frequently have no correlation with the actual disease process, and so it is incumbent to progress with history, clinical examination and lab tests before proceeding to imaging techniques.
As pointed out in the introduction to the pain module series there are elements of pain that need to be elucidated including precipitating factors, duration, onset, character, severity, situation, aggravating, relieving factors and radiation of the pain.
Precipitating Factors
There are a few factors that precipitate injury to the back including the severity of the force, frequency, and direction of the precipitating force that puts strain on the back.
Severity of precipitating force is logically an important factor , so that all severe forces in the primed and non primed back, or in the young or old back, will play a precipitating role. Thus in an MVA or violent athletic injury any part of the complex is subject to injury including muscle, disc, ligament, capsule, or bone. It is also logical that a person who presents with back pain after this type of injury needs urgent diagnostic and therapeutic attention. In the elderly patient or the unprimed non athletic back, even minor injury, twist or turn, or unaccustomed back position, can be sufficient to change the balance of structures by just a few mms to cause pressure on the nerves or even disc herniation. The spring or summer time with renewal of physical activity in the form of gardening or excercise for eaxample after the prolonged inactivity of the winter and with the renewal of physical activity in the form of gardening or excercise can result in the clinical syndrome of back pain. The lifting of heavy objects using the back rather than the legs to take the force are definite precipitating factors that are associated with back injury.
The direction of the force sometimes plays an important role. Prolonged bending over or sitting forward such as might occur in gardening, or prolonged journey where the patient may sit for a long time are often precipitating factors. Flexion of the back puts frontward force on the disc and opens the posterior aspect of the intervertebral space, and predisposes to herniation particulalrly in the weakened disc. Repetitive extension of the back such as occurs in gymnastics, dance, or figure skating is the usual cause of stress fractures of the pars interarticularis of L5 causing spondylolysis and spondylolisthesis.
- Duration
Pain may be hyperacute, (reaching a peak measured in seconds, minutes, to hours), acute (less than 6 weeks), and chronic (greater than 6 weeks.) The hyperacute unrelenting pain that has no precipitating factors, that lasts for hours, herald an urgent situation and require immediate referral to the emergency room. Renal colic with characteristic loin to groin distribution and hematuria is a less urgent example. Confirmation of the diagnosis requires a CTscan without intravenous contrast. The hyperacute pain of a ruptured aneurym is the real emergency and the clue is the presence of hypotension in the elderly patient. In this clinical setting the vascular surgeons should be on board as soon as this diagnosis is suspected clinically and an emergency CTscan without contrast would quickly establish the diagnosis. An aortic dissection with back pain is also a hyperacute presentation, but the back pain tends to be higher and the blood presssure is usually elevated. It is also an emergency but there usually is more time available between diagnosis and treatment as long as there is noclinical suggestion of pericardial involvement. The other examples of relatively spontaneous hyperacute back pain include an acute herniated disc, or an acute compression fracture.
Most the pain syndromes are more insidious and advance over days or a week. DJD, HNP tend to build up over a few days and then last for longer – days to weeks. Spondylolysis, spondylolisthesis, spinal stenosis, and osteomyelitis are also insidious and may last for months.
The onset of back pain has been discussed to some extent in the paragraph above. There are those diseases that present with severe back pain without any provocation. Often these are concerning situations, and include diseases such as renal colic ruptured aneurysms and aortic dissection. There are those that are precipitated acutely by minimal provocation with relatively acute onset and these usually are caused by discogenic diseases. Lastly there are back pain syndromes that have an insidious onset and include slowly progressive DJD, spinal stenosis and osteomyelitis for example.
- Onset
- In general, back pain lasts for 3-6 weeks and more than 80% will resolve by 12 weeks.
Character
In most instances the acute pain tends to be sharp and severe, while chronic pain tends to be dull and deep. Renal colic tends to come in waves of severity . The neuromuscular mechanical pains tend to be continuous and unrelenting. The pain of a ruptured aneurysm is lancinating and severe. The radicular pain has a a correlative distribution of a nerve root.
The pain may be felt in the low back, buttocks or down the legs. It may be unilateral or bilateral, localized or diffuse. Once there is a radicular component flags are raised as to neurological involvement raising the level of clinical concern.
The pain is graded from 1 – 10 with 1 being mild and 10 being the worst . This scale takes into account physical and psychological aspects of the pain. Patients who have the most severe pan in the morning as they get up usually have DJD
Aggravating
Patient positioning often makes the pain worse and sometimes the pain is relieved by position. So flexion in the patient with HNP may make the pain worse. Sometimes lying down, or lying down in a specific position makes the pain worse. The relationship to mionor changes in position suggests how tenious the involved space is where by virtue of a few mms, pain is either aggravated or relieved.
- Severity
- Situation
Relieving
In DJD, the pain is worst in the morning and is relieved as the day wears on. In spinal stenosis the pain is aggravated by walking and relieved by rest. Since this simulates claudication it is called pseudoclaudication. Spinal stenosis is also often also relieved when the patient flexes. HNP on the other hand is often relieved by lying flat where there is relative hyperextension of the spine and hence closing of the posterior space of the intervertebral disc.
The pain is termed radicular pain when it radiates down the legs and usually implies nerve root involvement. This can occur in any of the diseases described , and in all cases raises the clinical concern.
Associated Symptoms
The presence of other sensory or motor disturbance such as parasthesias, tingling, muscle weakness, urinary or fecal incontinence, have similar implications of nerve root involvement and create concern for cauda equina syndrome. Symptoms or signs that suggest a systemic illness such as malaise, weight loss, or fevers are also concerning , and raise concern for malignancy, or osteomyelitis.
In patients over the age of 65, malignancy, compression fractures, spinal stenosis, and aortic aneurysms become more prevalent. Disease specific imaging studies should be order without delay.
- Radiation
Lumbar spinal stenosis may present with classic pseudoclaudication symptoms of leg pain during ambulation that improves with rest. Other symptoms of pseudoclaudication include numbness in the lower extremities with walking and radicular pain to the feet.
Physical Examination
First, a general inspection of the back must be performed with the examiner being cognescent for any evidence of scoliosis, abnormal kyphosis of the thoracic spine, or increased lordosis of the lumbar spine.
Palpate the entire spine to isolate any areas of point tenderness. Then test the lumbar spine range of motion in flexion, extension, sidebending, and rotation to see if any of these movements elicits any discomfort or pain. Unilateral spondylolysis can be isolated by having the patient stand on one leg with extension of the lumbar spine. A positive test is where there is pain ipsilateral to the weight-bearing leg.
In addition, a straight leg test can be used to help confirm any radicular symptoms. This test is performed with the patient lying supine as the examiner raises one leg as far as possible with the knee in extension and the ankle in dorsiflexion. If there are any radicular symptoms down the leg, then the test is considered positive. Furthermore, the examiner needs to check the flexibility of the hip flexor muscles to isolate any hip flexion contractures that may be causing hyperlordosis. Hip joint range of motion should also be examined to determine if the patient?s back symptoms are actually referred pain from any hip pathology.
Finally, a thorough neurological exam should be performed focusing of the L5 and S1 nerve roots, since 98% of clinically relevant disc herniations occur at L4-5 and L5-S1. The L5 nerve root innervates the muscles that dorsiflex the great toe and foot. Thus, it can be tested by having the patient walk on his heels. Similarly, the S1 nerve root innervates the muscles that plantar flex the great toe and foot. Hence, walking on the toes will test for this. There?s also a diminished ankle jerk associated with a S1 nerve compression. The L4 nerve root innervates the quadriceps and can be tested by having the patient do a squat and rise. Patella reflex tend to be diminished with L4 nerve impingement. Lastly, if there is a clinical suspicion for cauda equina syndrome, which is a surgical emergency, a rectal exam to check for rectal tone and post void residuals should be obtained.
Labs
Typically, if a mechanical cause of low back pain is suspected, then no blood work needs to be collected. However, if there is multiple joint involvement and other systemic symptoms, then a rheumatological and infectious cause should be in the differential diagnosis. An initial rheumatological and infectious work-up includes an erythrocyte sedimentation rate (ESR) and a complete blood count (CBC). If there is a clinical suspicion for ankylosing spondylitis, then a HLA B27 should also be added.
Imaging
Up to 90% of patients with back pain in the absence of sciatica or systemic symptoms improve over time and without intervention.
Given the favorable prognosis, imaging studies are infrequently required. Imaging is not necessary during the first 4 to 6 weeks, unless the patient fits any of the following criteria:
Recent trauma
Focal progressive neurological deficit
Unexplained weight loss, fever, or a history of cancer
History of intravenous drug use
Age less than 18 or greater than 50 years old
Osteoporosis or a history of prolonged corticosteroid use
If there are persistent symptoms for greater than 6 weeks without any neurological deficits, then an initial AP and lateral plain radiograph should be obtained targeting the area of discomfort.
Early use of Magnetic resonance imaging (MRI) and computerized tomography (CT) scans that do not fit the above criteria is strongly discouraged. The medical literature has clearly shown that disk herniations, spinal stenosis, or facet arthropathy can occur in asymptomatic patients. Hence, when the patient presents clinically with lower back pain, there is a good chance that the spine pathology seen on MRI or CT have already been there for some time prior to the patient developing symptoms.
In general, MRI is the modality of choice when evaluating any disc, nerve, and ligamentous injury. CT scans are generally better for analyzing any bony pathology. Moreover, MRI and CT scans are more sensitive than plain x-rays at detecting early spinal malignancy and infection. Therefore, MRI and CT scans should be reserved for patients in whom there is a strong clinical suspicion of underlying infection, malignancy, or persistent neurological deficits.
Additionally, SPECT bone scans can be used to isolate the area where a suspected stress fracture, malignancy, infection, or inflammatory arthritis may occur.
Management
Once non-mechanical spinal conditions have been ruled out by a thorough history, physical examination, and diagnostic imaging then the clinician can safely proceed to treat mechanical low back pain. Non-operative treatment of general musculoskeletal strain, degenerative disc/joint disease, herniated discs, and spinal stenosis without neurological deficits are essentially equivalent. Up to 90% of patients with back pain in the absence of sciatica or systemic symptoms improve over time and without intervention.
Initial treatment involves non-steroidal anti-inflammatory drugs (NSAIDs) for acute symptomatic relief and activity modification with gradual progression to physical therapy for abdominal and erector spinae muscle strengthening. Bed rest does not increase the speed of recovery from acute low back pain and may sometimes delay recovery.
For a herniated nucleus pulposus with radicular symptoms, a quick 6-7 day tapering course of an oral corticosteroid may be used to temper severe lower back pain. Narcotic medication may also be occasionally needed for acute severe pain but should be used for only a short period of time. Moreover, epidural corticosteroid injections offer symptomatic relief for selected patients. Incidentally, a corticosteroid epidural injection can also be used for persistent back pain with spinal stenosis. Moreover, persistent back pain associated with degenerative joint disease in the spine may also benefit from a corticosteroid facet joint injection.
Diskectomy is the surgical option for a persistently symptomatic herniated nucleus pulposus that does not respond to non-operative management. Diskectomy produced better pain relief than non-operative management over a period of four years, but it is unclear whether there is any advantage after 10 years. Surgery should only be considered if pain symptoms do not improve after six weeks of treatment as the natural history of herniated disks is often favorable. For spinal stenosis associated with persistent severe pain, a decompressive laminectomy may be necessary.
Interestingly, some patients with chronic low back pain have no radiculopathy or anatomical abnormalities that clearly explain their symptoms. The current medical literature supports aerobic conditioning to reduce pain and improve function in these patients with chronic low back pain.
If the patient has been diagnosed with spondylolysis, treatment involves initial restriction of activities as well as a Boston overlapping bracing which is a hard plastic shell custom molded brace. Patients will also be started on physical therapy emphasizing core strengthening.
Lastly, non-operative treatment of lumbar compression fractures includes pain management, bracing with a thoracic-lumbar-sacral orthosis, and physical therapy. Surgical treatment is needed if there is neurological compromised associated with the compression fracture.
Red Flags
Factors that raise concern include;
Age <20 or greater than 50;
In the younger patient, athletically related injury such as spondylolisthesis is considered whereas in the older patient metastases and osteomyeltis are considered
Unexplained weight loss or fever;
When patient have systemic symptoms, they are often accompanied wit systemic diseases. With weight loss a primary malignancy with metastases to the spine is a consideration, while the patient with fever, osteomyelitis must be considered. In this same category are those patients with a history of i/v drug abuse or alcohol abuse.
Steroid use;
In those patients on steroids, both infections and compression fracture must be considered.
Unremitting pain;
Osteomyelits and metatstases are a cause of unremitting pain.
If the patient presents with saddle distribution of pain with incontinence then cauda equina syndrome is considered and an urgent MRI should be performed along with a surgical consultation. Cauda equina syndrome is a surgical emergency, and it is caused by acute mechanical compression of nerves supplying the lower extremities, bowel, and bladder. If the patient has symptoms of urine or stool incontinence, decrease sensation in the perineum and anus then cauda equine syndrome must be considered.
Patient information
-
- Non-mechanical spinal conditions:
· Primary vertebral tumors, multiple myeloma, or metastatic cancer to the spine· Dissecting aortic aneurysm· Ankylosing spondylitis, psoriatic spondylitis, Reiter?s syndrome, or Paget?s disease of the bone
- · Nephrolithiasis, pyelonephritis, or perinephric abscess
- · Osteomyelitis, epidural abscess, discitis, or shingles
Clinical Approach to Back Pain –
The clinical approach to the diagnosis of back pain requires careful and insightful questioning. Since back pain is a common problem, it is incumbent to start out with a history that elucidates the character of the pain and defines associated symptoms and diseases. It is all too easy to get an MRI to help with the diagnosis, but the imaging findings as pointed out, frequently have no correlation with the actual disease process, and so it is incumbent to progress with history, clinical examination and lab tests before proceeding to imaging techniques.
As pointed out in the introduction to the pain module series there are elements of pain that need to be elucidated including precipitating factors, duration, onset, character, severity, situation, aggravating, relieving factors and radiation of the pain.
Precipitating Factors
There are a few factors that precipitate injury to the back including the severity of the force, frequency, and direction of the precipitating force that puts strain on the back.
Severity of precipitating force is logically an important factor , so that all severe forces in the primed and non primed back, or in the young or old back, will play a precipitating role. Thus in an MVA or violent athletic injury any part of the complex is subject to injury including muscle, disc, ligament, capsule, or bone. It is also logical that a person who presents with back pain after this type of injury needs urgent diagnostic and therapeutic attention. In the elderly patient or the unprimed non athletic back, even minor injury, twist or turn, or unaccustomed back position, can be sufficient to change the balance of structures by just a few mms to cause pressure on the nerves or even disc herniation. The spring or summer time with renewal of physical activity in the form of gardening or excercise for eaxample after the prolonged inactivity of the winter and with the renewal of physical activity in the form of gardening or excercise can result in the clinical syndrome of back pain. The lifting of heavy objects using the back rather than the legs to take the force are definite precipitating factors that are associated with back injury.
The direction of the force sometimes plays an important role. Prolonged bending over or sitting forward such as might occur in gardening, or prolonged journey where the patient may sit for a long time are often precipitating factors. Flexion of the back puts frontward force on the disc and opens the posterior aspect of the intervertebral space, and predisposes to herniation particulalrly in the weakened disc. Repetitive extension of the back such as occurs in gymnastics, dance, or figure skating is the usual cause of stress fractures of the pars interarticularis of L5 causing spondylolysis and spondylolisthesis.
- Duration
Pain may be hyperacute, (reaching a peak measured in seconds, minutes, to hours), acute (less than 6 weeks), and chronic (greater than 6 weeks.) The hyperacute unrelenting pain that has no precipitating factors, that lasts for hours, herald an urgent situation and require immediate referral to the emergency room. Renal colic with characteristic loin to groin distribution and hematuria is a less urgent example. Confirmation of the diagnosis requires a CTscan without intravenous contrast. The hyperacute pain of a ruptured aneurym is the real emergency and the clue is the presence of hypotension in the elderly patient. In this clinical setting the vascular surgeons should be on board as soon as this diagnosis is suspected clinically and an emergency CTscan without contrast would quickly establish the diagnosis. An aortic dissection with back pain is also a hyperacute presentation, but the back pain tends to be higher and the blood presssure is usually elevated. It is also an emergency but there usually is more time available between diagnosis and treatment as long as there is noclinical suggestion of pericardial involvement. The other examples of relatively spontaneous hyperacute back pain include an acute herniated disc, or an acute compression fracture.
Most the pain syndromes are more insidious and advance over days or a week. DJD, HNP tend to build up over a few days and then last for longer – days to weeks. Spondylolysis, spondylolisthesis, spinal stenosis, and osteomyelitis are also insidious and may last for months.
The onset of back pain has been discussed to some extent in the paragraph above. There are those diseases that present with severe back pain without any provocation. Often these are concerning situations, and include diseases such as renal colic ruptured aneurysms and aortic dissection. There are those that are precipitated acutely by minimal provocation with relatively acute onset and these usually are caused by discogenic diseases. Lastly there are back pain syndromes that have an insidious onset and include slowly progressive DJD, spinal stenosis and osteomyelitis for example.
- Onset
- In general, back pain lasts for 3-6 weeks and more than 80% will resolve by 12 weeks.
Character
In most instances the acute pain tends to be sharp and severe, while chronic pain tends to be dull and deep. Renal colic tends to come in waves of severity . The neuromuscular mechanical pains tend to be continuous and unrelenting. The pain of a ruptured aneurysm is lancinating and severe. The radicular pain has a a correlative distribution of a nerve root.
The pain may be felt in the low back, buttocks or down the legs. It may be unilateral or bilateral, localized or diffuse. Once there is a radicular component flags are raised as to neurological involvement raising the level of clinical concern.
The pain is graded from 1 – 10 with 1 being mild and 10 being the worst . This scale takes into account physical and psychological aspects of the pain. Patients who have the most severe pan in the morning as they get up usually have DJD
Aggravating
Patient positioning often makes the pain worse and sometimes the pain is relieved by position. So flexion in the patient with HNP may make the pain worse. Sometimes lying down, or lying down in a specific position makes the pain worse. The relationship to mionor changes in position suggests how tenious the involved space is where by virtue of a few mms, pain is either aggravated or relieved.
- Severity
- Situation
Relieving
In DJD, the pain is worst in the morning and is relieved as the day wears on. In spinal stenosis the pain is aggravated by walking and relieved by rest. Since this simulates claudication it is called pseudoclaudication. Spinal stenosis is also often also relieved when the patient flexes. HNP on the other hand is often relieved by lying flat where there is relative hyperextension of the spine and hence closing of the posterior space of the intervertebral disc.
The pain is termed radicular pain when it radiates down the legs and usually implies nerve root involvement. This can occur in any of the diseases described , and in all cases raises the clinical concern.
Associated Symptoms
The presence of other sensory or motor disturbance such as parasthesias, tingling, muscle weakness, urinary or fecal incontinence, have similar implications of nerve root involvement and create concern for cauda equina syndrome. Symptoms or signs that suggest a systemic illness such as malaise, weight loss, or fevers are also concerning , and raise concern for malignancy, or osteomyelitis.
In patients over the age of 65, malignancy, compression fractures, spinal stenosis, and aortic aneurysms become more prevalent. Disease specific imaging studies should be order without delay.
- Radiation
Lumbar spinal stenosis may present with classic pseudoclaudication symptoms of leg pain during ambulation that improves with rest. Other symptoms of pseudoclaudication include numbness in the lower extremities with walking and radicular pain to the feet.
Physical Examination
First, a general inspection of the back must be performed with the examiner being cognescent for any evidence of scoliosis, abnormal kyphosis of the thoracic spine, or increased lordosis of the lumbar spine.
Palpate the entire spine to isolate any areas of point tenderness. Then test the lumbar spine range of motion in flexion, extension, sidebending, and rotation to see if any of these movements elicits any discomfort or pain. Unilateral spondylolysis can be isolated by having the patient stand on one leg with extension of the lumbar spine. A positive test is where there is pain ipsilateral to the weight-bearing leg.
In addition, a straight leg test can be used to help confirm any radicular symptoms. This test is performed with the patient lying supine as the examiner raises one leg as far as possible with the knee in extension and the ankle in dorsiflexion. If there are any radicular symptoms down the leg, then the test is considered positive. Furthermore, the examiner needs to check the flexibility of the hip flexor muscles to isolate any hip flexion contractures that may be causing hyperlordosis. Hip joint range of motion should also be examined to determine if the patient?s back symptoms are actually referred pain from any hip pathology.
Finally, a thorough neurological exam should be performed focusing of the L5 and S1 nerve roots, since 98% of clinically relevant disc herniations occur at L4-5 and L5-S1. The L5 nerve root innervates the muscles that dorsiflex the great toe and foot. Thus, it can be tested by having the patient walk on his heels. Similarly, the S1 nerve root innervates the muscles that plantar flex the great toe and foot. Hence, walking on the toes will test for this. There?s also a diminished ankle jerk associated with a S1 nerve compression. The L4 nerve root innervates the quadriceps and can be tested by having the patient do a squat and rise. Patella reflex tend to be diminished with L4 nerve impingement. Lastly, if there is a clinical suspicion for cauda equina syndrome, which is a surgical emergency, a rectal exam to check for rectal tone and post void residuals should be obtained.
Labs
Typically, if a mechanical cause of low back pain is suspected, then no blood work needs to be collected. However, if there is multiple joint involvement and other systemic symptoms, then a rheumatological and infectious cause should be in the differential diagnosis. An initial rheumatological and infectious work-up includes an erythrocyte sedimentation rate (ESR) and a complete blood count (CBC). If there is a clinical suspicion for ankylosing spondylitis, then a HLA B27 should also be added.
Imaging
Up to 90% of patients with back pain in the absence of sciatica or systemic symptoms improve over time and without intervention.
Given the favorable prognosis, imaging studies are infrequently required. Imaging is not necessary during the first 4 to 6 weeks, unless the patient fits any of the following criteria:
Recent trauma
Focal progressive neurological deficit
Unexplained weight loss, fever, or a history of cancer
History of intravenous drug use
Age less than 18 or greater than 50 years old
Osteoporosis or a history of prolonged corticosteroid use
If there are persistent symptoms for greater than 6 weeks without any neurological deficits, then an initial AP and lateral plain radiograph should be obtained targeting the area of discomfort.
Early use of Magnetic resonance imaging (MRI) and computerized tomography (CT) scans that do not fit the above criteria is strongly discouraged. The medical literature has clearly shown that disk herniations, spinal stenosis, or facet arthropathy can occur in asymptomatic patients. Hence, when the patient presents clinically with lower back pain, there is a good chance that the spine pathology seen on MRI or CT have already been there for some time prior to the patient developing symptoms.
In general, MRI is the modality of choice when evaluating any disc, nerve, and ligamentous injury. CT scans are generally better for analyzing any bony pathology. Moreover, MRI and CT scans are more sensitive than plain x-rays at detecting early spinal malignancy and infection. Therefore, MRI and CT scans should be reserved for patients in whom there is a strong clinical suspicion of underlying infection, malignancy, or persistent neurological deficits.
Additionally, SPECT bone scans can be used to isolate the area where a suspected stress fracture, malignancy, infection, or inflammatory arthritis may occur.
Management
Once non-mechanical spinal conditions have been ruled out by a thorough history, physical examination, and diagnostic imaging then the clinician can safely proceed to treat mechanical low back pain. Non-operative treatment of general musculoskeletal strain, degenerative disc/joint disease, herniated discs, and spinal stenosis without neurological deficits are essentially equivalent. Up to 90% of patients with back pain in the absence of sciatica or systemic symptoms improve over time and without intervention.
Initial treatment involves non-steroidal anti-inflammatory drugs (NSAIDs) for acute symptomatic relief and activity modification with gradual progression to physical therapy for abdominal and erector spinae muscle strengthening. Bed rest does not increase the speed of recovery from acute low back pain and may sometimes delay recovery.
For a herniated nucleus pulposus with radicular symptoms, a quick 6-7 day tapering course of an oral corticosteroid may be used to temper severe lower back pain. Narcotic medication may also be occasionally needed for acute severe pain but should be used for only a short period of time. Moreover, epidural corticosteroid injections offer symptomatic relief for selected patients. Incidentally, a corticosteroid epidural injection can also be used for persistent back pain with spinal stenosis. Moreover, persistent back pain associated with degenerative joint disease in the spine may also benefit from a corticosteroid facet joint injection.
Diskectomy is the surgical option for a persistently symptomatic herniated nucleus pulposus that does not respond to non-operative management. Diskectomy produced better pain relief than non-operative management over a period of four years, but it is unclear whether there is any advantage after 10 years. Surgery should only be considered if pain symptoms do not improve after six weeks of treatment as the natural history of herniated disks is often favorable. For spinal stenosis associated with persistent severe pain, a decompressive laminectomy may be necessary.
Interestingly, some patients with chronic low back pain have no radiculopathy or anatomical abnormalities that clearly explain their symptoms. The current medical literature supports aerobic conditioning to reduce pain and improve function in these patients with chronic low back pain.
If the patient has been diagnosed with spondylolysis, treatment involves initial restriction of activities as well as a Boston overlapping bracing which is a hard plastic shell custom molded brace. Patients will also be started on physical therapy emphasizing core strengthening.
Lastly, non-operative treatment of lumbar compression fractures includes pain management, bracing with a thoracic-lumbar-sacral orthosis, and physical therapy. Surgical treatment is needed if there is neurological compromised associated with the compression fracture.
Red Flags
Factors that raise concern include;
Age <20 or greater than 50;
In the younger patient, athletically related injury such as spondylolisthesis is considered whereas in the older patient metastases and osteomyeltis are considered
Unexplained weight loss or fever;
When patient have systemic symptoms, they are often accompanied wit systemic diseases. With weight loss a primary malignancy with metastases to the spine is a consideration, while the patient with fever, osteomyelitis must be considered. In this same category are those patients with a history of i/v drug abuse or alcohol abuse.
Steroid use;
In those patients on steroids, both infections and compression fracture must be considered.
Unremitting pain;
Osteomyelits and metatstases are a cause of unremitting pain.
If the patient presents with saddle distribution of pain with incontinence then cauda equina syndrome is considered and an urgent MRI should be performed along with a surgical consultation. Cauda equina syndrome is a surgical emergency, and it is caused by acute mechanical compression of nerves supplying the lower extremities, bowel, and bladder. If the patient has symptoms of urine or stool incontinence, decrease sensation in the perineum and anus then cauda equine syndrome must be considered.
Patient information
Lower back pain is a very common symptom and is the second most common reason for a physician visit in the United States. In fact, it has been estimated that up to 84% of adults have lower back pain at some point in their lives. For most patients, symptoms are self-limited and resolve without any specific radiographic imaging or treatment. Imaging is not necessary during the first 4-6 weeks, unless the patient fits any of the following criteria:
Recent trauma
Focal progressive neurological deficit
Unexplained weight loss, fever, or a history of cancer
History of intravenous drug use
Osteoporosis or a history of prolonged corticosteroid use
Age less than 18 or greater than 50 years old
Emergencies related to lower back pain are rare, but if symptoms of urine/stool incontinence or decreased sensation in the perineum/anus manifest, then an immediate referral to the emergency department is necessary.
References
-
-
- Ankylosing Spondylitis eMedicine Peh CG Wilfred MD MBBS FRCP FRCR MHSM
- Back Pain – Mechanical e Medicine Perina Debra MD
- Back Pain eMedicine Pathophysiology of Chronic Back Pain Wheeler Anthony H MD
- Back Pain Imaging Medscape Finch Philip Technology Insight
- Cauda Equina Syndrome eMedicine Beeson Michal S MD MBA FACP
- Compression Fractures (Lumbar) eMedicine Sherman Andrew L
- Facet Joint Disease eMedicine Lumbosacral facet syndrome Gerard Malanga MD
- Osteomyelitis EMedicine Spinal Infections Vinas Federico C MD
- Spinal Stenosis eMedicine Hsiang John NK MD PhD
- Spinal Stenosis Alexander JT
- Spondylolisthesis eMedicine Irani Zubin MD MBBS
- Sprain and Strain eMedicine Lumbosacral Spine Sprain Strain Injuries Radebold Andrea MD
- Herniated Nucleus Pulposus eMedicine Foster Mark MD
- Intervertebral Disc degeneration Medscape
-
-
- Deyo RA, Weinstein JN. Low back pain. New England J Med. 2001; 344:363.
- Deyo RA. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine. 1987; 12:264.
- Cassidy JD, Carroll LJ, Cote P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine. 1998; 23:1860.
- d?Hemecourt PA, Gerbino PG, Micheli LJ. Back injuries in the young athlete. Clin Sports Med. 2000; 19(4):663.
- Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006; 88 suppl 2:21
- American Academy of Orthopedic Surgeons. Press Release. 2006
- Deyo RA, Loeser JD, Bigos SJ. Herniated lumbar intervertebral disk. Ann Intern Med. 1990; 112:598.
- Deyo RA, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992; 268:760.
- Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002; 137:5
Web References
-
- Back Pain Lumbar Vertebral Compression Mark King
- SpineHealth.com
- PTU.edu Kinesiology
Multiple choice questions
1) All of the following choices require immediate radiographic imaging except:
- A)Recent trauma
- B)Age greater than 50 years old
- C)History of intravenous drug use
- D)History of recent trauma
- E)History HIV/AIDS
2) What percentage of patients with back pain in the absence of sciatica or systemic symptoms improve over time:
- A)5%
- B)25%
- C)50%
- D)75%
- E)90%
3) A 40 year old male comes to clinic with persistent lower back pain for two months. There is no recent trauma or injury. Additionally, the patient denies any history of intravenous drug use or corticosteroid use. Past medical history is unremarkable. Upon review of systems, the patient denies any fever, chills, weight loss or gain, or melena. Which is the initial imaging modality of choice?
- A)MRI
- B)Ultrasound
- C)CT scan
- D)Plain x-rays
- E)SPECT bone scan
4) A 42 year old male presents to clinic with lower back pain. Patient states that the pain occurred when he was picking up a heavy box as he was helping his brother move. The patients symptoms started yesterday and has not really improved. He describes lower back pain going to his left buttock that is consistent in nature and is exacerbated by any movement. The only comfortable position is laying flat in bed. He walks very gingerly secondary to pain. The patient denies any changes in bowel or bladder dysfunction. On exam, he can only flex his lumbar spine about 30 degrees and extend to 10 degrees until he has tremendous discomfort. Which of the follow is not recommended as a treatment option:
- A) Bed rest for 7 days
- B) Naproxen 500mg by mouth twice daily for 10 days
- C) Prednisone taper, 60mg for two days, then 40mg for two days, and then 20mg
for two days.
- D)Vicoden every 4-6 hours as needed for only the first seven days.
5) Which imaging modality is best at the evaluation of any disc, nerve, and ligamentous injury?
- A) CT scan
- B) MRI
- C) Plain x-rays
- D) Ultrasound
- E) SPECT bone scan
6) Which imaging modality is best at the evaluation of any specific bony pathology?
- A) CT scan
- B) MRI
- C) Plain x-rays
- D) Ultrasound
- E) SPECT bone scan
7) A 12 year old gymnast is being evaluated for extension based lower back pain. You suspect spondylolysis and the diagnosis is confirmed via SPECT bone scan and CT. What is the best option for treatment?
- A) No treatment is needed, spondylolysis should heal on its own
- B) The patient should be taken to surgery for a diskectomy
- C)Out of sports, Boston overlapping bracing, physical therapy emphasizing core
Strengthening
- D)Prescribe naproxen twice daily for 14 days
- E)Confirm the diagnosis with an MRI
8) A 44 year old male was diagnosed with low back pain secondary to a herniated nucleus pulposus at the L4-L5 level that appears to be encroaching on the L5 nerve root based on an MRI done 6 months ago. Despite treatment with relative rest, NSAIDs, and physical therapy the patient continues to be symptomatic with flexion based lower back pain. These symptoms come off-and-on, and he?ll occasional flairs of back pain that require an emergency room visit. This has occurred twice over the last three months. He now presents to you on a follow-up visit 3 days after being seen in the emergency room. He has been taking hydrocodone/acetaminophen 5/500mg every 6 hours for pain. Repeat MRI is unchanged from the one done 6 months ago. There are no changes in bowel or bladder habits nor is there any numbness or tingling down his lower extremities. Which of the following treatments is most warranted in this case?
- A)Wean off hydrocodone/acetaminophen, start NSAIDs, and bed rest for 7-10
days
- B)Stop hydrocodone/acetaminophen and start physical therapy with core
strengthening
- C)Continue with hydrocodone/acetaminophen and follow-up in one week
- D)Wean off hydrocodone/acetaminophen, start NSAIDs, activity as tolerated, and refer for possible diskectomy
9) Which of the following symptoms in addition to lower back pain would one strongly suspect cauda equine syndrome?
- A)skin lesions
- B)painful knee joints and motor weakness on exam
- C)numbness and tingling in the toes along with motor weakness on exam
- D)urine or stool incontinence and decrease perineum/anus sensation on exam
- E)proximal muscle weakness
10) When suspecting cauda equine syndrome, which of the follow should be done next?
- A)MRI of the lumbar spine and intravenous steroids
- B)MRI of the lumbar spine and emergent surgical consultation
- C)MRI of the lumbar spine and narcotic pain medications
- D)CT of the lumbar spine and emergent surgical consultation
- E)CT of the lumbar spine and intravenous steroids
11) Which of the following is a mechanical cause of back pain that is deemed a medical emergency
- A)spondylolysis
- B)back pain associated with a herniated nucleus pulposus
- C)cauda equine syndrome
- D)facet arthropathy
- E)scoliosis
12) Risk factors for lower back pain include all of the following except:
- A)male gender
- B)sedentary work
- C)obesity
- D)smoking
- E)older age
13) A 45 year old female comes to see you with lower back pain. Patient states that she noticed lower back symptoms while doing routine household chores yesterday. The patient has not significant past medical history and she does not take any medications. She notes stiffness in her lower back without any numbness or tingling in her lower extremities. She also denies any urine or stool incontinence and motor weakness. Exam is only remarkable for some discomfort with forward flexion. What should be done next?
- A)CT of the lumbar spine
- B)Plain x-rays of the lumbar spine
- C)MRI of the lumbar spine
- D)Check a pregnancy test
- E)Prescribe naproxen
14) The above 45 year old female returns to your clinic 2 months later with continued symptoms of stiffness in her lower back. Symptoms have improved but only slightly, and she complains that her symptoms have affected her activities of daily living. Again she denies any urine/stool incontinence, motor weakness, and numbness/tingling in her legs. What is the next most appropriate course of action?
- A)CT of the lumbar spine
- B)Plain x-rays of the lumbar spine
- C)MRI of the lumbar spine
- D)Check a pregnancy test
- E)Prescribe naproxen
15) In a patient over 65 years of age who present with lower back pain, all of the following become more prevalent except:
- A)Spondylolysis
- B)Malignancy
- C)Compression fractures
- D)Spinal stenosis
- E)Aortic Aneurysms
16) You suspect that a 71 year old female patient has pseudoclaudication secondary to lumbar spinal stenosis. Which of the follow is a classic presentation of pseudoclaudication?
- A) Flexion based lower back pain that worsens with ambulation
- B) Urine or stool incontinence and decrease perineum/anus sensation on exam
- C) Painful knee joints and motor weakness on exam
- D) Leg pain during ambulation that improves with rest
17) All of the following is a non-mechanical cause of lower back pain except:
- A)Nephrolithiasis
- B)Ankylosing spondylitis
- C)Spondylolysis
- D)Multiple myeloma
- E)Dissecting aortic aneurysm
18) All of the following is a mechanical cause of lower back pain except:
- A)Herniated nucleus pulposus
- B)Vertebral compression fracture
- C)Psoriatic spondylitis
- D)Cauda equine syndrome
- E)Severe scoliosis
19) A physical exam finding of extension based lower back pain that is isolated to the ipsilateral weight-bearing leg when the patient stands on that leg with extension of the lumbar spine is indicative of:
- A)Herniated nucleus pulposus
- B)Vertebral compression fracture
- C)Pseudoclaudication
- D)Nephrolithiasis
- E)Spondylolysis
20) 98% of the clinically relevant disc herniations occur at in the following areas:
- A)L2-L3, L3-L4
- B)L4-L5, L5-S1
- C)T12-L1, L1-L2
- D)T9-T10, T11-T12
References
- American Osteopathic Association: Foundations for osteopathic medicine. Baltimore, Williams and Wilkins. 1997.
- Savarese, RG. OMT Review. Second edition. 2000.
- Deyo RA, Weinstein JN. Low back pain. New England J Med. 2001; 344:363.
- Deyo RA. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine. 1987; 12:264.
- Cassidy JD, Carroll LJ, Cote P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine. 1998; 23:1860.
- d?Hemecourt PA, Gerbino PG, Micheli LJ. Back injuries in the young athlete. Clin Sports Med. 2000; 19(4):663.
- Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006; 88 suppl 2:21
- American Academy of Orthopedic Surgeons. Press Release. 2006
- Deyo RA, Loeser JD, Bigos SJ. Herniated lumbar intervertebral disk. Ann Intern Med. 1990; 112:598.
- Deyo RA, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992; 268:760.
- Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002; 137:586.
Answers to the multiple choice questions
1) E
2) E
3) D
4) A
5) B
6) A
7) C
8) D
9) D
10) B
11) C
12) A
13) E
14) B
15) A
16) D
17) C
18) C
19) E
20) B
References
- Lower back pain is a very common symptom and is the second most common reason for a physician visit in the United States. In fact, it has been estimated that up to 84% of adults have lower back pain at some point in their lives. For most patients, symptoms are self-limited and resolve without any specific radiographic imaging or treatment. Imaging is not necessary during the first 4-6 weeks, unless the patient fits any of the following criteria:
Recent trauma
Focal progressive neurological deficit
Unexplained weight loss, fever, or a history of cancer
History of intravenous drug use
Osteoporosis or a history of prolonged corticosteroid use
Age less than 18 or greater than 50 years old
Emergencies related to lower back pain are rare, but if symptoms of urine/stool incontinence or decreased sensation in the perineum/anus manifest, then an immediate referral to the emergency department is necessary.
References
-
-
- Ankylosing Spondylitis eMedicine Peh CG Wilfred MD MBBS FRCP FRCR MHSM
- Back Pain – Mechanical e Medicine Perina Debra MD
- Back Pain eMedicine Pathophysiology of Chronic Back Pain Wheeler Anthony H MD
- Back Pain Imaging Medscape Finch Philip Technology Insight
- Cauda Equina Syndrome eMedicine Beeson Michal S MD MBA FACP
- Compression Fractures (Lumbar) eMedicine Sherman Andrew L
- Facet Joint Disease eMedicine Lumbosacral facet syndrome Gerard Malanga MD
- Osteomyelitis EMedicine Spinal Infections Vinas Federico C MD
- Spinal Stenosis eMedicine Hsiang John NK MD PhD
- Spinal Stenosis Alexander JT
- Spondylolisthesis eMedicine Irani Zubin MD MBBS
- Sprain and Strain eMedicine Lumbosacral Spine Sprain Strain Injuries Radebold Andrea MD
- Herniated Nucleus Pulposus eMedicine Foster Mark MD
- Intervertebral Disc degeneration Medscape
-
-
- Deyo RA, Weinstein JN. Low back pain. New England J Med. 2001; 344:363.
- Deyo RA. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine. 1987; 12:264.
- Cassidy JD, Carroll LJ, Cote P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine. 1998; 23:1860.
- d?Hemecourt PA, Gerbino PG, Micheli LJ. Back injuries in the young athlete. Clin Sports Med. 2000; 19(4):663.
- Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006; 88 suppl 2:21
- American Academy of Orthopedic Surgeons. Press Release. 2006
- Deyo RA, Loeser JD, Bigos SJ. Herniated lumbar intervertebral disk. Ann Intern Med. 1990; 112:598.
- Deyo RA, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992; 268:760.
- Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002; 137:5
Web References
-
- Back Pain Lumbar Vertebral Compression Mark King
- SpineHealth.com
- PTU.edu Kinesiology
Multiple choice questions
1) All of the following choices require immediate radiographic imaging except:
- A)Recent trauma
- B)Age greater than 50 years old
- C)History of intravenous drug use
- D)History of recent trauma
- E)History HIV/AIDS
2) What percentage of patients with back pain in the absence of sciatica or systemic symptoms improve over time:
- A)5%
- B)25%
- C)50%
- D)75%
- E)90%
3) A 40 year old male comes to clinic with persistent lower back pain for two months. There is no recent trauma or injury. Additionally, the patient denies any history of intravenous drug use or corticosteroid use. Past medical history is unremarkable. Upon review of systems, the patient denies any fever, chills, weight loss or gain, or melena. Which is the initial imaging modality of choice?
- A)MRI
- B)Ultrasound
- C)CT scan
- D)Plain x-rays
- E)SPECT bone scan
4) A 42 year old male presents to clinic with lower back pain. Patient states that the pain occurred when he was picking up a heavy box as he was helping his brother move. The patients symptoms started yesterday and has not really improved. He describes lower back pain going to his left buttock that is consistent in nature and is exacerbated by any movement. The only comfortable position is laying flat in bed. He walks very gingerly secondary to pain. The patient denies any changes in bowel or bladder dysfunction. On exam, he can only flex his lumbar spine about 30 degrees and extend to 10 degrees until he has tremendous discomfort. Which of the follow is not recommended as a treatment option:
- A) Bed rest for 7 days
- B) Naproxen 500mg by mouth twice daily for 10 days
- C) Prednisone taper, 60mg for two days, then 40mg for two days, and then 20mg
for two days.
- D)Vicoden every 4-6 hours as needed for only the first seven days.
5) Which imaging modality is best at the evaluation of any disc, nerve, and ligamentous injury?
- A) CT scan
- B) MRI
- C) Plain x-rays
- D) Ultrasound
- E) SPECT bone scan
6) Which imaging modality is best at the evaluation of any specific bony pathology?
- A) CT scan
- B) MRI
- C) Plain x-rays
- D) Ultrasound
- E) SPECT bone scan
7) A 12 year old gymnast is being evaluated for extension based lower back pain. You suspect spondylolysis and the diagnosis is confirmed via SPECT bone scan and CT. What is the best option for treatment?
- A) No treatment is needed, spondylolysis should heal on its own
- B) The patient should be taken to surgery for a diskectomy
- C)Out of sports, Boston overlapping bracing, physical therapy emphasizing core
Strengthening
- D)Prescribe naproxen twice daily for 14 days
- E)Confirm the diagnosis with an MRI
8) A 44 year old male was diagnosed with low back pain secondary to a herniated nucleus pulposus at the L4-L5 level that appears to be encroaching on the L5 nerve root based on an MRI done 6 months ago. Despite treatment with relative rest, NSAIDs, and physical therapy the patient continues to be symptomatic with flexion based lower back pain. These symptoms come off-and-on, and he?ll occasional flairs of back pain that require an emergency room visit. This has occurred twice over the last three months. He now presents to you on a follow-up visit 3 days after being seen in the emergency room. He has been taking hydrocodone/acetaminophen 5/500mg every 6 hours for pain. Repeat MRI is unchanged from the one done 6 months ago. There are no changes in bowel or bladder habits nor is there any numbness or tingling down his lower extremities. Which of the following treatments is most warranted in this case?
- A)Wean off hydrocodone/acetaminophen, start NSAIDs, and bed rest for 7-10
days
- B)Stop hydrocodone/acetaminophen and start physical therapy with core
strengthening
- C)Continue with hydrocodone/acetaminophen and follow-up in one week
- D)Wean off hydrocodone/acetaminophen, start NSAIDs, activity as tolerated, and refer for possible diskectomy
9) Which of the following symptoms in addition to lower back pain would one strongly suspect cauda equine syndrome?
- A)skin lesions
- B)painful knee joints and motor weakness on exam
- C)numbness and tingling in the toes along with motor weakness on exam
- D)urine or stool incontinence and decrease perineum/anus sensation on exam
- E)proximal muscle weakness
10) When suspecting cauda equine syndrome, which of the follow should be done next?
- A)MRI of the lumbar spine and intravenous steroids
- B)MRI of the lumbar spine and emergent surgical consultation
- C)MRI of the lumbar spine and narcotic pain medications
- D)CT of the lumbar spine and emergent surgical consultation
- E)CT of the lumbar spine and intravenous steroids
11) Which of the following is a mechanical cause of back pain that is deemed a medical emergency
- A)spondylolysis
- B)back pain associated with a herniated nucleus pulposus
- C)cauda equine syndrome
- D)facet arthropathy
- E)scoliosis
12) Risk factors for lower back pain include all of the following except:
- A)male gender
- B)sedentary work
- C)obesity
- D)smoking
- E)older age
13) A 45 year old female comes to see you with lower back pain. Patient states that she noticed lower back symptoms while doing routine household chores yesterday. The patient has not significant past medical history and she does not take any medications. She notes stiffness in her lower back without any numbness or tingling in her lower extremities. She also denies any urine or stool incontinence and motor weakness. Exam is only remarkable for some discomfort with forward flexion. What should be done next?
- A)CT of the lumbar spine
- B)Plain x-rays of the lumbar spine
- C)MRI of the lumbar spine
- D)Check a pregnancy test
- E)Prescribe naproxen
14) The above 45 year old female returns to your clinic 2 months later with continued symptoms of stiffness in her lower back. Symptoms have improved but only slightly, and she complains that her symptoms have affected her activities of daily living. Again she denies any urine/stool incontinence, motor weakness, and numbness/tingling in her legs. What is the next most appropriate course of action?
- A)CT of the lumbar spine
- B)Plain x-rays of the lumbar spine
- C)MRI of the lumbar spine
- D)Check a pregnancy test
- E)Prescribe naproxen
15) In a patient over 65 years of age who present with lower back pain, all of the following become more prevalent except:
- A)Spondylolysis
- B)Malignancy
- C)Compression fractures
- D)Spinal stenosis
- E)Aortic Aneurysms
16) You suspect that a 71 year old female patient has pseudoclaudication secondary to lumbar spinal stenosis. Which of the follow is a classic presentation of pseudoclaudication?
- A) Flexion based lower back pain that worsens with ambulation
- B) Urine or stool incontinence and decrease perineum/anus sensation on exam
- C) Painful knee joints and motor weakness on exam
- D) Leg pain during ambulation that improves with rest
17) All of the following is a non-mechanical cause of lower back pain except:
- A)Nephrolithiasis
- B)Ankylosing spondylitis
- C)Spondylolysis
- D)Multiple myeloma
- E)Dissecting aortic aneurysm
18) All of the following is a mechanical cause of lower back pain except:
- A)Herniated nucleus pulposus
- B)Vertebral compression fracture
- C)Psoriatic spondylitis
- D)Cauda equine syndrome
- E)Severe scoliosis
19) A physical exam finding of extension based lower back pain that is isolated to the ipsilateral weight-bearing leg when the patient stands on that leg with extension of the lumbar spine is indicative of:
- A)Herniated nucleus pulposus
- B)Vertebral compression fracture
- C)Pseudoclaudication
- D)Nephrolithiasis
- E)Spondylolysis
20) 98% of the clinically relevant disc herniations occur at in the following areas:
- A)L2-L3, L3-L4
- B)L4-L5, L5-S1
- C)T12-L1, L1-L2
- D)T9-T10, T11-T12
References
- American Osteopathic Association: Foundations for osteopathic medicine. Baltimore, Williams and Wilkins. 1997.
- Savarese, RG. OMT Review. Second edition. 2000.
- Deyo RA, Weinstein JN. Low back pain. New England J Med. 2001; 344:363.
- Deyo RA. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine. 1987; 12:264.
- Cassidy JD, Carroll LJ, Cote P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine. 1998; 23:1860.
- d?Hemecourt PA, Gerbino PG, Micheli LJ. Back injuries in the young athlete. Clin Sports Med. 2000; 19(4):663.
- Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006; 88 suppl 2:21
- American Academy of Orthopedic Surgeons. Press Release. 2006
- Deyo RA, Loeser JD, Bigos SJ. Herniated lumbar intervertebral disk. Ann Intern Med. 1990; 112:598.
- Deyo RA, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992; 268:760.
- Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002; 137:586.
Answers to the multiple choice questions
1) E
2) E
3) D
4) A
5) B
6) A
7) C
8) D
9) D
10) B
11) C
12) A
13) E
14) B
15) A
16) D
17) C
18) C
19) E
20) B