The Common Vein Copyright 2009
Imaging
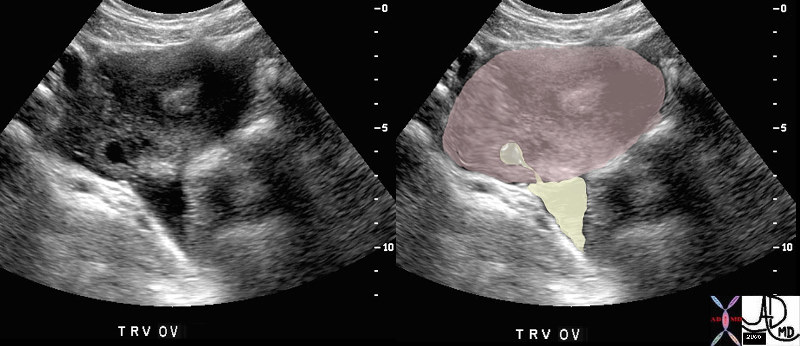 Ruptured Follicle Ruptured Follicle |
| 47025c01 young patient with known ovulation one day earlier ovary Graafian follicle rupture tear drop shape pear shaped ovulation physiology normal anatomy USscan Davidoff MD |
Ovaries
Position – ovarian fossa, bordered laterally/anteriorly by external iliac vessels, posteriorly by ureter and internal iliacs. May be displaced superiorly by adnexal or uterine masses and pregnancy.
Shape – ovoid, approximately 3 x 3 x 2 cm in nulliparous adult. Atrophy after menopause unless taking hormonal therapy. Typical volume around 9ml, increasing to 15ml in multiparous adult.
Imaging
Ultrasound is primary imaging choice. Lack of ionizing radiation to vulnerable germ cells. Ultrasound can identify ovaries in adults, though they may not be seen in up to 20% of post menopausal women. Normal appearance is of low level echogenicity with thin hyperechoic rim.
Normal cycle
In the fertile phase (approx age 14-50 years), there are typically follicles which appear as simple cysts, <10mm. Usually a single follicle enlarges under hormonal influence during first half of cycle (proliferative phase, under estrogen influence), known as the “dominant follicle”. The dominant follicle peaks in size at midcycle (around 20-25mm) before rupturing in response to LH (Leutinizing Hormone) surge and releasing ovum. Thereafter, it is known as the corpus luteum and appears as a cyst with a small complex region (cumulus oophorus) which regresses in size throughout second half of menstrual cycle (secretory phase, under progesterone influence) in the absence of fertilization.
Pathology
Fertility medications – such as clomiphene cause multiple follicles to enlarge and ovulate (hence increased risk of multiple gestations). In severe cases, the ovary is enlarged and totally obscured by functional follicles causing discomfort. This is known as Ovarian Hyperstimulation Syndrome (OHS). The ovary may be more then 20cm in size, and leaky capillaries may cause transudation of fluid and ascites/pleural effusions. During pregnancy, such ascites is worsened due to increased hormonal influence and may cause dangerous fluid shifts.
Functioning cysts
Nonfunctioning cysts – ovarian/paraovarian (Wolffian duct)/adnexal; usually benign; do not change in size
Polycystic ovaries – hyperechoic rim, rounded/enlarger ovary, “string of pearls” = many small follicles in periphery of ovary. Associated with Stein-Leventhal syndrome (increased LH, decreased FSH, diabetes, hirsute)
Complex cysts – hemorrhagic, endometrioma, torsion, abscess, hydro/pyosalpinx, dermoid, malignancy, necrotic fibroid, non GYN (duplication, mesenteric cysts)
Endometriomas
Pelvic Inflammatory Disease
Ovarian Torsion
Neoplasms
Benign – dermoid, serous/mucinous cystadenoma
Malignant – cystadenocarcinoma, endometroid carcinoma
Metastases – breast, GI (Krukenberg)
